Professional Documents
Culture Documents
Sumup Toxi Os
Uploaded by
Selma MutiaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sumup Toxi Os
Uploaded by
Selma MutiaraCopyright:
Available Formats
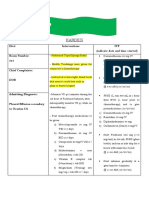
Osteosarcoma MAP (methotrexate, DOXOrubicin,
cISplatin)
ID: 1901 v.4 Endorsed Essential Medicine List
This protocol is based on limited evidence; refer to the evidence section of this protocol for more information.
The treatment of sarcoma is complex and combined modality therapy is common; the involvement of a multidisciplinary team
(MDT) in the initial development and ongoing evaluation of the treatment plan, and the management of the sequelae associated
with treatment is strongly recommended. Patients with sarcoma should be considered for inclusion in a clinical trial. For
details of centres that specialise in sarcoma care and current clinical trials visit the Australasian Sarcoma Study Group (ASSG)
website.
Related pages:
Clinical practice guidelines for the management of adult onset sarcoma
Treatment schedule - Overview
Cycle 1 to 4
Drug Dose Route Day
DOXOrubicin 37.5 mg/m2 IV * 1 and 2
ciSplatin 60 mg/m2 IV infusion ** 1 and 2
Pegfilgrastim 6 mg Subcut 3
Methotrexate 12,000 mg/m2 (maximum IV infusion 22 and 29
20,000 mg)
Calcium folinate (Leucovorin) 15 mg/m2 every 6 hours (for IV bolus 23 and 30
4 doses) ***
Frequency: 35 days
Cycles: 4
Cycle 5 and 6
Drug Dose Route Day
DOXOrubicin 37.5 mg/m2 IV * 1 and 2
Pegfilgrastim 6 mg S/C 3
Methotrexate 12,000 mg/m2 (maximum IV infusion 15 and 22
20,000 mg)
Calcium folinate (leucovorin) 15 mg/m2 every 6 hours (for IV bolus 16 and 23
4 doses) ***
* Various doses and schedules have been used in clinical trials. Alternate regimens administered doxorubicin as a single dose on
D1. Doxorubicin has also been administered as a bolus, a 4 hour infusion and as a continuous infusion over 48 hours
** Cisplatin is only administered for cycles 1 to 4 and has been administered over 2 or 4 hours on day 1 and day 2 or as a
continuous 72 hour infusion (120 mg/m2) on day 1
*** Commence 24 hours after the start of methotrexate infusion. Calcium folinate 15 mg/m2 is given IV for the first 4 doses, then
IV/PO given every 6 hours until methotrexate level is less than 0.1 micromol/L. Calcium folinate rescue doses should be titrated to
methotrexate level and any associated toxicity, see methotrexate toxicity
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 1 of 21
Frequency: 28 days
Cycles: 2
Notes:
In patients older than 40 years of age, consider using cisplatin and doxorubicin without high dose methotrexate.
Drug status: All drugs in this protocol are on the PBS general schedule
Pegfilgrastim is PBS authority
Cost: ~ $2,000
Treatment schedule - Detail
The supportive therapies (e.g. antiemetics, premedications, etc.), infusion times, diluents, volumes and routes of administration, if included, are
listed as defaults. They may vary between institutions and can be substituted to reflect individual institutional policy.
Antiemetics if included in the treatment schedule are based upon recommendations from national and international guidelines. These are
defaults only and may be substituted to reflect individual institutional policy. Select here for recommended doses of alternative antiemetics.
Cycle 1 to 4
Day 1
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
DOXOrubicin 37.5 mg/m2 (IV) over 5 to 15 minutes *
ciSplatin 60 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 2 hours **
Day 2
Dexamethasone 8 mg (PO) 60 minutes before chemotherapy
DOXOrubicin 37.5 mg/m2 (IV) over 5 to 15 minutes *
ciSplatin 60 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 2 hours **
Day 3
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Pegfilgrastim 6 mg (Subcut) inject subcutaneously on day 3 at least 24 hours after
chemotherapy
Day 4
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Day 22
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
Methotrexate 12,000 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 4 hours.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 2 of 21
Day 22
(Maximum 20,000 mg)
Day 23
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Calcium folinate (Leucovorin) 15 mg/m2 (IV bolus) Commence 24 hours after the start of the methotrexate
infusion. Calcium folinate 15 mg/m2 IV is given every 6
hours for the first 4 doses, then 15 mg/m2 IV/PO every
6 hours until methotrexate level is less than 0.1
micromol/L. ***
Day 24 and 25
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Day 29
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
Methotrexate 12,000 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 4 hours.
(Maximum 20,000 mg)
Day 30
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Calcium folinate (Leucovorin) 15 mg/m2 (IV bolus) Commence 24 hours after the start of the methotrexate
infusion. Calcium folinate 15 mg/m2 IV is given every 6
hours for the first 4 doses, then 15 mg/m2 IV/PO every
6 hours until methotrexate level is less than 0.1
micromol/L. ***
Day 31 and 32
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Frequency: 35 days
Cycles: 4
Cycle 5 and 6
Day 1
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
DOXOrubicin 37.5 mg/m2 (IV) over 5 to 15 minutes *
Day 2
Dexamethasone 8 mg (PO) 60 minutes before chemotherapy
DOXOrubicin 37.5 mg/m2 (IV) over 5 to 15 minutes *
Day 3
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 3 of 21
Day 3
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Pegfilgrastim 6 mg (Subcut) inject subcutaneously on day 3 at least 24 hours after
chemotherapy
Day 4
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Day 15
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
Methotrexate 12,000 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 4 hours.
(Maximum 20,000 mg)
Day 16
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Calcium folinate (leucovorin) 15 mg/m2 (IV bolus) Commence 24 hours after the start of the methotrexate
infusion. Calcium folinate 15 mg/m2 IV is given every 6
hours for the first 4 doses, then 15 mg/m2 IV/PO every
6 hours until methotrexate level is less than 0.1
micromol/L. ***
Day 17 and 18
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Day 22
Netupitant 300 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with palonosetron)
Palonosetron 0.5 mg (PO) 60 minutes before chemotherapy (fixed dose
preparation with netupitant)
Dexamethasone 12 mg (PO) 60 minutes before chemotherapy
Methotrexate 12,000 mg/m2 (IV infusion) in 1000 mL sodium chloride 0.9% over 4 hours.
(Maximum 20,000 mg)
Day 23
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
Calcium folinate (leucovorin) 15 mg/m2 (IV bolus) Commence 24 hours after the start of the methotrexate
infusion. Calcium folinate 15 mg/m2 IV is given every 6
hours for the first 4 doses, then 15 mg/m2 IV/PO every
6 hours until methotrexate level is less than 0.1
micromol/L. ***
Day 24 and 25
Dexamethasone 8 mg (PO) ONCE a day (or in divided doses) with or after food.
* Various doses and schedules have been used in clinical trials. Alternate regimens administered doxorubicin as a single dose on
D1. Doxorubicin has also been administered as a bolus, a 4 hour infusion and as a continuous infusion over 48 hours
** Cisplatin is only administered for cycles 1 to 4 and has been administered over 2 or 4 hours on day 1 and day 2 or as a
continuous 72 hour infusion (120 mg/m2) on day 1
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 4 of 21
*** Commence 24 hours after the start of methotrexate infusion. Calcium folinate 15mg/m2 is given IV for the first 4 doses, then
IV/PO given every 6 hours until methotrexate level is less than 0.1 micromol/L. Calcium folinate rescue doses should be titrated to
methotrexate level and any associated toxicity, see methotrexate toxicity
Frequency: 28 days
Cycles: 2
Indications and patient population
Neoadjuvant and adjuvant treatment of localised or metastatic high grade osteosarcoma of an extremity / axial skeleton
(excluding craniofacial sites) - all disease sites amenable to complete surgical resection
age 40 or younger
Clinical information
Venous access Central venous access device (CVAD) is required to administer this treatment.
Read more about central venous access device line selection
Antiemetics for multi-day Antiemetic therapy should be administered throughout the duration of the chemotherapy
protocols protocol and to cover delayed nausea. The acute and delayed emetic risk of multi-day
chemotherapy protocols will overlap depending on the individual drugs and their sequence of
administration. More or less antiemetic cover may be required.
Ensure that patients also have sufficient antiemetics for breakthrough emesis:
Metoclopramide 10 mg three times a day when necessary (maximum of 30 mg/24 hours, up to
5 days) OR
Prochlorperazine 10 mg PO every 6 hours when necessary.
Read more about preventing antineoplastic induced nausea and vomiting
Cumulative lifetime dose of The total cumulative lifetime dose of doxorubicin is 450 to 500 mg/m2.
doxorubicin Reduce the total cumulative lifetime dose to 400 to 450 mg/m2 if elderly, prior mediastinal
radiation, hypertensive cardiomegaly, concurrent therapy with high dose cyclophosphamide and
some other cytotoxic drugs (e.g. dacarbazine, dactinomycin, etoposide, mitomycin, melphalan,
vincristine and bleomycin).
Baseline clinical assessment, echocardiogram (ECHO) or gated heart pool scan (GHPS) and
electrocardiogram (ECG) evaluation. Patients with normal baseline cardiac function (left
ventricular ejection fraction (LVEF) > 50%) and low risk patients require LVEF monitoring when
greater than 70% of anthracycline threshold is reached or if patient displays symptoms of
cardiac impairment. Post treatment cardiac monitoring is recommended for patients who have
received high levels of total cumulative doses of doxorubicin at the clinicians discretion.
Read more about cardiac toxicity associated with anthracyclines
Hydration Hydration helps to prevent cisplatin-induced nephrotoxicity.
The default regimen is appropriate for patients with normal electrolytes, renal function, fluid
status etc. and should be adjusted according to individual requirements.
Read more about cisplatin hydration regimens
Hydration and urinary Pre-hydration with sodium bicarbonate 8.4% infusion. Urinary pH must be greater than 7 prior to
alkalinisation commencing methotrexate infusion.
(Consider prescribing sodium bicarbonate oral capsules for administration prior to
methotrexate infusion) Sodium bicarbonate 8.4% should continue until the methotrexate level is
equal to or less than 0.1 micromol/L.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 5 of 21
High dose methotrexate Monitoring of methotrexate levels is essential as delayed methotrexate excretion is potentially
an emergency situation. Methotrexate levels to be monitored every 24 hours until level is less
than 0.1 micromol/L.
Methotrexate is renally eliminated. Renal function must be evaluated prior to treatment.
Methotrexate exits slowly from third space compartments (e.g. pleural effusions or ascites),
resulting in a prolonged terminal plasma half-life and unexpected toxicity. In patients with
significant third space accumulations, it is advisable to evacuate the fluid before treatment and
to monitor plasma methotrexate levels.
Glucarpidase is recommended in patients with high dose methotrexate (HDMTX)-induced acute
kidney injury and delayed methotrexate clearance. It can rapidly lower methotrexate levels and
early administration within 48 to 60 hours from the start of the HDMTX infusion is critical, as
life-threatening toxicities may not be preventable beyond this time point.1
Read more about high dose methotrexate-induced toxicity and methotrexate toxicity in
sarcoma.
Methotrexate interactions Avoid administering the following drugs in combination with high dose methotrexate:
ciprofloxacin, NSAIDs, probenecid, proton pump inhibitors (PPIs) (e.g. esomeprazole,
omeprazole, pantoprazole), sulphonamides (e.g. sulfamethoxazole (in Bactrim®, Septrin®)),
penicillins (e.g. piperacillin (in Tazocin®)) and trimethoprim. Severe mucositis may occur if
administered together.
Ototoxicity Ototoxicity may occur with platinum-based therapy; patients should be monitored for signs and
symptoms. Platinum compounds should be used with caution in patients with pre-existing
conditions or risk factors.
Ototoxicity may become more severe in patients being treated with other drugs with
nephrotoxic potential e.g. aminoglycosides.
An audiometry test should be performed if symptoms develop.
Read more about ototoxicity - tinnitus and hearing loss
Peripheral neuropathy Assess prior to each treatment. If a patient experiences grade 2 or greater neuropathy,
cessation of cisplatin is recommended; review by medical officer before commencing
treatment.
Read more about peripheral neuropathy
Link to chemotherapy-induced peripheral neuropathy screening tool
Biosimilar drug Read more about biosimilar drugs on the Biosimilar Awareness Initiative page
Growth factor support G-CSF (short or long-acting) is available on the PBS for chemotherapy induced neutropenia
depending on clinical indication and/or febrile neutropenia risk.
Access the PBS website
FBC at baseline and repeat FBC at baseline and repeat prior to each treatment. EUCs, LFTs and CMP at baseline and
prior to each treatment. regularly throughout treatment as clinically indicated.
EUCs, LFTs and CMP at Methotrexate levels to be monitored every 24 hours until the level is less than 0.1 micromol/L
baseline and regularly MTX
level
Hepatitis B screening and Routine screening for HBsAg and anti-HBc is recommended prior to initiation of treatment.
prophylaxis Prophylaxis should be determined according to individual institutional policy.
Read more about hepatitis B screening and prophylaxis in cancer patients requiring cytotoxic
and/or immunosuppressive therapy
Vaccinations Live vaccines, including BCG, MMR, zoster and varicella vaccines, are contraindicated in cancer
patients receiving immunosuppressive therapy and/or who have poorly controlled malignant
disease.
Refer to the recommended schedule of vaccination for immunocompromised patients, as
outlined in the Australian Immunisation Handbook.
Effects of cancer treatment Cancer treatment can have harmful effects on fertility and this should be discussed with all
on fertility patients of reproductive age prior to commencing treatment.
Read more about the effect of cancer treatment on fertility
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 6 of 21
Dose modifications
Evidence for dose modifications is limited, and the recommendations made on eviQ are intended as a guide only. They are
generally conservative with an emphasis on safety. Any dose modification should be based on clinical judgement, and the
individual patient’s situation including but not limited to treatment intent (curative vs palliative), the antineoplastic regimen
(single versus combination therapy versus chemotherapy versus immunotherapy), biology of the cancer (site, size, mutations,
metastases), other treatment related side effects, additional co-morbidities, performance status and patient preferences. For
more information see dosing considerations & disclaimer .
Dose reductions are complex and may not always follow guidelines for treatment toxicities in other tumour types, therefore
consultation with the patients primary provider should be sought at all times.
Interactions
References & Disclaimer
Cisplatin
Interaction Clinical management
Nephrotoxic drugs (e.g. Additive nephrotoxicity Avoid combination or monitor renal
aminoglycosides, amphotericin, function closely
cisplatin, contrast dye, frusemide,
NSAIDs)
Ototoxic drugs (e.g. aminoglycosides, Additive ototoxicity Avoid combination or perform regular
frusemide, NSAIDs) audiometric testing
Neurotoxic drugs (e.g. vincristine, Additive neurotoxicity Monitor closely for neuropathy if
paclitaxel) combination used
Paclitaxel Administration schedule may influence Minimise toxicity by administering
the development of myelosuppression paclitaxel first in regimens using the
combination
Carbamazepine, phenytoin, valproate Decreased antiepileptic plasma levels Monitor antiepileptic serum levels and
seizure frequency for efficacy; adjust
dosage as appropriate or select
alternative antiepileptic (e.g.
clonazepam, diazepam, lorazepam)
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 7 of 21
Doxorubicin
Interaction Clinical management
Cardiotoxic drugs (eg. bevacizumab, Increased risk of doxorubicin-induced Avoid combination or monitor closely for
calcium channel blockers, propranolol, cardiotoxicity cardiotoxicity
trastuzumab)
Cyclophosphamide Sensitises the heart to the cardiotoxic Monitor closely for cardiotoxicity and
effects of doxorubicin; also, doxorubicin ensure adequate prophylaxis for
may exacerbate cyclophosphamide haemorrhagic cystitis when combination
induced cystitis is used
Glucosamine Reduced efficacy of doxorubicin (due to The clinical effect of glucosamine taken
induction of glucose-regulated stress orally is unknown. Avoid combination or
proteins resulting in decreased monitor for decreased clinical response
expression of topoisomerase II in vitro) to doxorubicin
CYP2D6 inhibitors (e.g. SSRIs (esp. Increased toxicity of doxorubicin Monitor for doxorubicin toxicity
paroxetine), perhexiline, cinacalcet, possible due to reduced clearance
doxepin, flecainide, quinine,
terbinafine)
CYP3A4 inhibitors (e.g. aprepitant, Increased toxicity of doxorubicin Monitor for doxorubicin toxicity
azole antifungals, clarithromycin, possible due to reduced clearance
erythromycin, grapefruit juice, ritonavir
etc.)
CYP3A4 inducers (e.g. carbamazepine, Reduced efficacy of doxorubicin Monitor for decreased clinical response
phenytoin, phenobarbitone, rifampicin, possible due to increased clearance to doxorubicin
St John's wort etc.)
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 8 of 21
Methotrexate
Interaction Clinical management
Ciprofloxacin Increased toxicity of methotrexate Avoid combination or monitor for
possible due to reduced clearance methotrexate toxicity
NSAIDS
Important note: with high-dose
Probenecid methotrexate therapy, many of these
drug combinations are contraindicated
Proton pump inhibitors (e.g.
esomeprazole, omeprazole,
pantoprazole)
Sulphonamides and penicillins (e.g. Increased toxicity of methotrexate Avoid combination or monitor for
sulfamethoxazole (in Bactrim®, possible due to displacement from methotrexate toxicity
Septrin®), piperacillin (in Tazocin®) serum protein binding
etc.)
Trimethoprim Increased toxicity of methotrexate Avoid combination or monitor for
possible due to additive antifolate methotrexate toxicity
activity
Mercaptopurine Increased toxicity of mercaptopurine Avoid combination or monitor for
possible due to reduced clearance mercaptopurine toxicity
Nephrotoxic drugs (e.g. Additive nephrotoxicity Avoid combination or monitor renal
aminoglycosides, amphotericin, function closely
cisplatin, contrast dye, frusemide,
NSAIDs)
Hepatotoxic drugs (e.g. azathioprine, Additive hepatotoxicity Avoid combination or monitor liver
leflunomide, retinoids, sulfasalazine) function closely
Folic acid (e.g. as in multivitamins) Reduced efficacy of methotrexate Avoid combination or monitor for
possible due antagonism of its action decreased clinical response to
Asparaginase (administered methotrexate
immediately prior or concurrently) Note: asparaginase administered shortly
after methotrexate can enhance its
efficacy and reduce its toxicity
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 9 of 21
NK-1 antagonist e.g. aprepitant, fosaprepitant, netupitant
Interaction Clinical management
Dexamethasone Increased effects/toxicity of Reduce dose of antiemetic
dexamethasone due to inhibition of its dexamethasone by approximately 50%
metabolism via CYP3A4 when adding a NK-1 antagonist. For
protocols that already recommend a NK-
1 antagonist, the dose reduction of
antiemetic dexamethasone has already
been taken into account.
If dexamethasone is part of the
chemotherapy protocol, dose reduction
as per the product information is not
routinely recommended in clinical
practice and no additional
dexamethasone is required for
antiemetic cover.
Warfarin Reduced anticoagulant efficacy of INR should be monitored in the 2 week
warfarin due to increased clearance period, particularly at 7 to 10 days
(aprepitant induces CYP2C9). *Note following the administration of
interaction only applicable to aprepitant/ aprepitant/ fosaprepitant
fosaprepitant
Combined oral contraceptive Reduced contraceptive efficacy due to Alternative non-hormonal methods
increased clearance. *Note interaction should be used during and for 1 month
only applicable to aprepitant/ after stopping aprepitant/ fosaprepitant
fosaprepitant
CYP3A4 inducers (e.g. carbamazepine, Reduced efficacy of NK-1 antagonist Avoid combination or monitor for
phenytoin, phenobarbitone, rifampicin, possible due to increased clearance decreased antiemetic effect. Consider
St John’s wort etc.) using an alternative antiemetic regimen
CYP3A4 inhibitors (e.g. azole Increased toxicity of NK-1 antagonist Avoid combination or monitor for
antifungals, clarithromycin, possible due to reduced clearance increased adverse effects of NK-1
erythromycin, grapefruit juice, ritonavir antagonist (e.g. headache, hiccups,
etc.) constipation)
Drugs metabolised by CYP3A4 (e.g. Increased effects/toxicity of these drugs Avoid combination or monitor for
etoposide, imatinib, irinotecan, possible due to inhibition of CYP3A4 by increased toxicity especially with orally
midazolam, paclitaxel, vinblastine, NK-1 antagonist administered drugs
vincristine etc.)
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 10 of 21
General
Interaction Clinical management
Warfarin Antineoplastic agents may alter the Monitor INR regularly and adjust warfarin
anticoagulant effect of warfarin. dosage as appropriate; consider
alternative anticoagulant.
Direct oral anticoagulants (DOACs) e.g. Interaction with both CYP3A4 and P-gp Apixaban: avoid concurrent use with
apixaban, rivaroxaban, dabigatran inhibitors /inducers. strong CYP3A4 and P‑gp inhibitors. If
treating VTE, avoid use with strong
DOAC and antineoplastic levels may CYP3A4 and P‑gp inducers.
both be altered, possibly leading to loss
of efficacy or toxicity (i.e. increased Rivaroxaban: avoid concurrent use with
bleeding). strong CYP3A4 and P‑gp inhibitors.
Dabigatran: avoid combination with
strong P‑gp inducers and inhibitors.
If concurrent use is unavoidable, monitor
closely for efficacy/toxicity of both
drugs.
Digoxin Antineoplastic agents can damage the Monitor digoxin serum levels; adjust
lining of the intestine; affecting the digoxin dosage as appropriate.
absorption of digoxin.
Antiepileptics Both altered antiepileptic and Where concurrent use of an enzyme-
antineoplastic levels may occur, possibly inducing antiepileptic cannot be avoided,
leading to loss of efficacy or toxicity. monitor antiepileptic serum levels for
toxicity, as well as seizure frequency for
efficacy; adjust dosage as appropriate.
Also monitor closely for efficacy of the
antineoplastic therapy.
Antiplatelet agents and NSAIDs Increased risk of bleeding due to Avoid or minimise combination.
treatment related thrombocytopenia. If combination deemed essential, (e.g.
low dose aspirin for ischaemic heart
disease) monitor for signs of bleeding.
Serotonergic drugs, including selective Increased risk of serotonin syndrome Avoid combination.
serotonin reuptake inhibitors (SSRIs with concurrent use of 5-HT3 receptor If combination is clinically warranted,
e.g. paroxetine) and serotonin antagonists (e.g. palonosetron, monitor for signs and symptoms of
noradrenaline reuptake inhibitors ondansetron, granisetron, tropisetron, serotonin syndrome (e.g. confusion,
(SNRIs e.g. venlafaxine) dolasetron, etc.) agitation, tachycardia, hyperreflexia).
For more information link to TGA
Medicines Safety Update
Vaccines Diminished response to vaccines and Live vaccines (e.g. BCG, MMR, zoster and
increased risk of infection with live varicella) are contraindicated in patients
vaccines. on immunosuppressive therapy. Use
with caution in patients on non-
immunosuppressive therapy.
For more information; refer to the
recommended schedule of vaccination
for cancer patients, as outlined in the
Australian Immunisation Handbook
Administration cycles 1 to 4
Day 1 and 2 (cycles 1 to 4)
Approximate treatment time: 4 to 5 hours
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 11 of 21
Safe handling and waste management
Safe administration
General patient assessment prior to each day of treatment.
Peripheral neuropathy assessment tool
Any toxicity grade 2 or greater may require dose reduction, delay or omission of treatment and review by medical officer before
commencing treatment.
Prime IV line(s).
Access port or CVC.
Pre treatment medication
Verify antiemetics taken or administer as prescribed.
Verify dexamethasone taken or administer as prescribed.
Chemotherapy - Time out
Doxorubicin
Administer doxorubicin (vesicant):
over 5 to 15 minutes
via a minibag OR
by IV bolus via a side port of a freely flowing IV infusion
ensure vein is patent and monitor for signs of extravasation throughout administration
flush with ~150 mL of sodium chloride 0.9%
potential for flare reaction during administration of doxorubicin (facial flushing and red streaking along the vein) stop infusion
and exclude extravasation before continuing at a slower rate of infusion.
Although rare, cardiac arrhythmias may occur during or immediately after doxorubicin administration. If sudden onset of dyspnoea,
palpitations or irregular pulse occurs, stop administration immediately and obtain urgent medical officer review.
Cisplatin
Commence prehydration for cisplatin:
administer 10 mmol magnesium sulphate (MgSO4) in 1000 mL sodium chloride 0.9% over 60 minutes
followed by 200 mL of mannitol 20% over 15 minutes
mannitol should be administered via a controlled infusion
mannitol 10% may be used as per institutional policy; there is much variation in the use of mannitol and although there is no
conclusive evidence that mannitol should be used, many sites have used it routinely without renal toxicity. The routine use of
frusemide to increase urine flow is not recommended. Refer to your institutional guidelines and medical orders.
ensure patient has passed urine prior to cisplatin administration as per institutional policy.
Administer cisplatin (irritant):
via IV infusion over 2 hours
flush with 100 mL of sodium chloride 0.9%.
Post hydration:
1000 mL sodium chloride 0.9% over 60 minutes.
Deaccess port or CVC.
Continue safe handling precautions until 7 days after completion of drug(s)
Day 3 (cycles 1 to 4)
Subcutaneous injection
General patient assessment prior to each day of treatment.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 12 of 21
Pegfilgrastim
administer subcutaneously at least 24 hours post chemotherapy.
Day 22 and 29 (cycles 1 to 4)
Safe handling and waste management
Safe administration
General patient assessment prior to each treatment.
Any toxicity grade 2 or greater may require dose reduction, delay or omission of treatment and review by medical officer before
recommencing treatment.
Prime IV line(s).
Access port or CVC.
Pre treatment medication
Verify antiemetics taken or administer as prescribed.
Verify dexamethasone taken or administer as prescribed.
Chemotherapy - Time out
Methotrexate infusion
Prehydration:
administer 100 mL sodium bicarbonate 8.4% in 1000 mL glucose 5% OR sodium chloride 0.9% over 4 hours
continue hydration with sodium bicarbonate 8.4% as prescribed
when urine pH is greater than 7 commence methotrexate
If the urine pH drops below 7 during the methotrexate infusion:
administer stat dose of 100 mL sodium bicarbonate 8.4% over 15 minutes
continue to test all urine for pH, if the pH continues to drop below 7 seek medical review as further doses of sodium bicarbonate
may be required.
Note: A large volume of intravenous fluid is given with this protocol if weight increases by more than 1 kg from baseline or fluid
balance becomes positive by one litre or any other signs of fluid overload are present, review by medical officer (diuretics may be
required)
Administer methotrexate:
via IV infusion over 4 hours
the starting time of the methotrexate infusion must be documented as the leucovorin rescue is to commence exactly 24 hours
after the start of the methotrexate and continue until the methotrexate level is less than 0.1 micromol/L.
flush with ~50 mL of sodium chloride 0.9%
Post methotrexate:
continue hydration with sodium bicarbonate 8.4% until methotrexate level is less than 0.1 micromol/L
continue to monitor all urine pH and fluid input and output
monitor methotrexate concentration every 24 hours until the level is less than 0.1 micromol/L
Read more about methotrexate toxicity
Continue safe handling precautions until 7 days after completion of drug(s)
Day 23 and 30 (cycles 1 to 4)
General patient assessment prior to each day of treatment.
Any toxicity grade 2 or greater may require delay of treatment and review by medical officer before commencing treatment.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 13 of 21
Calcium folinate (Leucovorin)
Commence 24 hours after the start of the methotrexate infusion and repeat every 6 hours until methotrexate level is less than 0.1
micromol/L
administer via IV bolus via the side port of the IV line over 1 to 2 minutes
flush with ~ 50 mL of sodium chloride 0.9%
first 4 doses to be administered IV, then IV/PO every 6 hours until methotrexate level is less than 0.1 micromol/L.
Deaccess port or CVC.
daily weight
monitor pH on all urine output
strict fluid balance input and output
Discharge information
Antiemetics
Antiemetics as prescribed.
Antidiarrhoeals
Antidiarrhoeals as prescribed.
Growth factor support
Arrangements for administration if prescribed.
Patient information
Ensure patient receives patient information sheet.
Administration cycles 5 and 6
Day 1 and 2 (cycles 5 and 6)
Approximate treatment time: 30 to 60 minutes.
Safe handling and waste management
Safe administration
General patient assessment prior to each treatment.
Any toxicity grade 2 or greater may require dose reduction, delay or omission of treatment and review by medical officer before
recommencing treatment.
Prime IV line(s).
Access port or CVC.
Pre treatment medication
Verify antiemetics taken or administer as prescribed.
Verify dexamethasone taken or administer as prescribed.
Chemotherapy - Time out
Doxorubicin
Administer doxorubicin (vesicant):
over 5 to 15 minutes
via a minibag OR
by IV bolus via a side port of a freely flowing IV infusion
ensure vein is patent and monitor for signs of extravasation throughout administration
flush with ~150 mL of sodium chloride 0.9%
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 14 of 21
potential for flare reaction during administration of doxorubicin (facial flushing and red streaking along the vein) stop infusion
and exclude extravasation before continuing at a slower rate of infusion.
Although rare, cardiac arrhythmias may occur during or immediately after doxorubicin administration. If sudden onset of dyspnoea,
palpitations or irregular pulse occurs, stop administration immediately and obtain urgent medical officer review.
Deaccess port or CVC.
Continue safe handling precautions until 7 days after completion of drug(s)
Day 3 (cycles 5 and 6)
Subcutaneous injection
General patient assessment prior to each day of treatment.
Pegfilgrastim
administer subcutaneously at least 24 hours post chemotherapy.
Day 15 and 22 (cycles 5 and 6)
Safe handling and waste management
Safe administration
General patient assessment prior to each treatment.
Any toxicity grade 2 or greater may require dose reduction, delay or omission of treatment and review by medical officer before
recommencing treatment.
Prime IV line(s).
Access port or CVC.
Pre treatment medication
Verify antiemetics taken or administer as prescribed.
Verify dexamethasone taken or administer as prescribed.
Chemotherapy - Time out
Methotrexate infusion
Prehydration:
administer 100 mL sodium bicarbonate 8.4% in 1000 mL glucose 5% OR sodium chloride 0.9% over 4 hours
continue hydration with sodium bicarbonate 8.4% as prescribed
when urine pH is greater than 7 commence methotrexate
If the urine pH drops below 7 during the methotrexate infusion:
administer stat dose of 100 mL sodium bicarbonate 8.4% over 15 minutes
continue to test all urine for pH, if the pH continues to drop below 7 seek medical review as further doses of sodium bicarbonate
may be required.
Note: A large volume of intravenous fluid is given with this protocol if weight increases by more than 1 kg from baseline or fluid
balance becomes positive by one litre or any other signs of fluid overload are present, review by medical officer (diuretics may be
required)
Administer methotrexate:
via IV infusion over 4 hours
the starting time of the methotrexate infusion must be documented as the leucovorin rescue is to commence exactly 24 hours
after the start of the methotrexate and continue until the methotrexate level is less than 0.1 micromol/L.
flush with ~50 mL of sodium chloride 0.9%
Post methotrexate:
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 15 of 21
continue hydration with sodium bicarbonate 8.4% until methotrexate level is less than 0.1 micromol/L
continue to monitor all urine pH and fluid input and output
monitor methotrexate concentration every 24 hours until the level is less than 0.1 micromol/L
Read more about methotrexate toxicity
Continue safe handling precautions until 7 days after completion of drug(s)
Day 16 and 23 (cycles 5 and 6)
General patient assessment prior to each day of treatment.
Any toxicity grade 2 or greater may require delay of treatment and review by medical officer before commencing treatment.
daily weight
monitor pH on all urine output
strict fluid balance input and output
Calcium folinate (Leucovorin)
Commence 24 hours after the start of the methotrexate infusion and repeat every 6 hours until methotrexate level is less than 0.1
micromol/L
administer via IV bolus via the side port of the IV line over 1 to 2 minutes
flush with ~ 50 mL of sodium chloride 0.9%
first 4 doses to be administered IV, then IV/PO every 6 hours until methotrexate level is less than 0.1 micromol/L.
Deaccess port or CVC.
Discharge information
Antiemetics
Antiemetics as prescribed.
Antidiarrhoeals
Antidiarrhoeals as prescribed.
Growth factor support
Arrangements for administration if prescribed.
Patient information
Ensure patient receives patient information sheet.
Side effects
The side effects listed below are not a complete list of all possible side effects for this treatment. Side effects are categorised into the
approximate onset of presentation and should only be used as a guide.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 16 of 21
Immediate (onset hours to days)
Extravasation, tissue or vein The unintentional instillation or leakage of a drug or substance out of a blood vessel into
injury surrounding tissue. This has the potential to cause damage to affected tissue.
Read more about extravasation management
Headache
Bone pain Bone pain, usually in the lower back or pelvis, associated with colony stimulating factors
(filgrastim, lenograstim, lipegfilgrastim and pegfilgrastim).
Nausea and vomiting Read more about prevention of treatment induced nausea and vomiting
Taste and smell alteration Read more about taste and smell changes
Red-orange discolouration Pink/red/orange discolouration of the urine. This can last for up to 48 hours after some
of urine anthracycline drugs.
Flare reaction Anthracycline flare reaction is caused by a localised allergic reaction. It is characterised by
erythematous vein streaking, urticaria and pruritus which may occur during drug administration
and is often associated with too rapid an infusion. Extravasation must be ruled out if flare
occurs.
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 17 of 21
Early (onset days to weeks)
Neutropenia Abnormally low levels of neutrophils in the blood. This increases the risk of infection. Any fever
or suspicion of infection should be investigated immediately and managed aggressively.
Read more about neutropenia
Thrombocytopenia A reduction in the normal levels of functional platelets, increasing the risk of abnormal bleeding.
Read more about thrombocytopenia
Anorexia Loss of appetite accompanied by decreased food intake.
Read more about anorexia
Skin rash Antineoplastic agents can cause a number of changes in the skin with maculo-papular rash the
most common type of drug-induced skin reaction.
Read more about skin rash
Oral mucositis Erythematous and ulcerative lesions of the gastrointestinal tract (GIT). It commonly develops
following chemotherapy, radiotherapy to the head, neck or oesophagus, and high dose
chemotherapy followed by a blood and marrow transplant (BMT).
Read more about oral mucositis
Diarrhoea Read more about treatment induced diarrhoea
Peripheral neuropathy Typically symmetrical sensory neuropathy, affecting the fingers and toes, sometimes
progressing to the hands and feet. It is associated with several classes of antineoplastic
agents. These include taxanes, platinum-based compounds, vinca alkaloids and some drugs
used to treat multiple myeloma.
Read more about peripheral neuropathy
Fatigue Read more about fatigue
Photosensitivity Increased sensitivity to ultraviolet (UV) light resulting in an exaggerated sunburn-like reaction
accompanied by stinging sensations and urticaria.
Radiation recall Erythematous or inflammatory skin reaction resembling severe sunburn at sites previously
treated with radiotherapy can occur with certain antineoplastic drugs. Symptoms include
vesiculation, desquamation and ulceration of the skin.
Read more about radiation recall
Hypomagnesaemia, Abnormally low levels of magnesium, potassium and calcium in the blood.
hypokalaemia,
hypocalcaemia
Nephrotoxicity Renal dysfunction resulting from damage to the glomeruli, tubules or renal vasculature.
Hepatotoxicity Antineoplastic agents administered either alone or in combination with other drugs and/or
radiation may cause direct or indirect hepatotoxicity. Hepatic dysfunction can alter the
metabolism of some drugs resulting in systemic toxicity.
Ototoxicity Tinnitus and hearing loss may occur due to damage in the inner ear. Tinnitus is usually
reversible, while hearing loss is generally irreversible. Hearing loss is dose-related, cumulative
and may be worse in those with pre-existing hearing problems.
Read more about ototoxicity - tinnitus and hearing loss
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 18 of 21
Late (onset weeks to months)
Anaemia Abnormally low levels of red blood cells (RBCs) or haemoglobin in the blood.
Read more about anaemia
Alopecia Hair loss may occur from all parts of the body. Patients can also experience mild to moderate
discomfort of the hair follicles, and rarely pain as the hair is falling out.
Read more about alopecia
Pulmonary toxicity Pulmonary toxicity may include damage to the lungs, airways, pleura and pulmonary circulation.
Read more about pulmonary toxicity associated with antineoplastic drugs
Nail changes Hyperpigmentation, paronychia, onycholysis, splinter haemorrhage, pyogenic granuloma
formation, subungal haematoma and subungal hyperkeratosis are some of the nail changes
associated with antineoplastic treatment.
Read more about nail toxicities
Cognitive changes (chemo Changes in cognition characterised by memory loss, forgetfulness and feeling vague. This is
fog) also referred to as 'chemo brain' or 'chemo fog'.
Read more about cognitive changes (chemo fog)
Delayed (onset months to years)
Cardiotoxicity Anthracyclines are the most frequently implicated antineoplastic agents associated with
cardiotoxicity, which typically manifests as a reduction in left ventricular ejection fraction
(LVEF), cardiomyopathy, or symptomatic CHF. Anthracycline induced cardiotoxicity has been
categorised into acute, early-onset chronic progressive and late-onset chronic progressive and
is usually not reversible. The risk of clinical cardiotoxicity increases with a number of risk
factors including higher total cumulative doses.
Read more about cardiac toxicity associated with anthracyclines
Evidence
A search of the literature did not find strong evidence to support the use of neoadjuvant or adjuvant MAP in the treatment of
surgically resectable osteosarcoma. Although MAP is used as the standard of care, there are no comparative studies with other
chemotherapy regimens. The expert reference panel supported publication of the protocol on the basis of the information
summarised below. The committee was most strongly influenced by the Intergroup 01332 and EURAMOS-1 trials.3
Is the dose and
Study & Year Supports regimen
Source Comments
Published Use consistent with
the protocol?
Phase III Meyers et al Yes No doxorubicin 75 mg/m2 day 1 cisplatin 120 mg/m2 day 1
trials 20052 protocol 20 weeks duration
(standard of
Bielack et al Yes No same doses but different schedules doxorubicin given as
care)
20153 48 hour infusion, alternative cisplatin administration
as 72 hour infusion
Winkler et al Yes No cisplatin 120 mg/m2day 1, doxorubicin 30 mg/m2 days
19884 1,2
Bacci et al 20005 Yes No methotrexate 8 g/m2 d1,28 cisplatin intra-arterially 120
mg/m2 over 72 hrs d7,34 doxorubicin 60 mg/m2 over 8
hours d9,36
Is the dose and
Date Supports regimen
Guidelines Comments
published/revised Use consistent with
the protocol?
NCCN 2016 Yes no doses
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 19 of 21
Is the dose and
Study & Year Supports regimen
Source Comments
Published Use consistent with
the protocol?
BCCA 2012 Yes No separate protocols cisplatin 100 mg/m2 d1 doxorubicin
75 mg/m2 d1 q3 weekly, methotrexate 8-12 g/m2 d1
leucovorin rescue 25 mg q6h repeating every 1-4 weeks
CCO - N/A - -
Efficacy
Outcome Study No. of patients Control arm Effect
Overall survival Meyers et al2 662 MAP (n=172) 6 yr OS 74%
Bielack et al3 716 MAP (359) 5yr OS 81%
(95% CI:74-86%)
Event free survival Meyers et al2 662 MAP (n=172) 3yr EFS 71%
5yr EFS 64%
Bielack et al3 716 MAP (359) 3yr EFS 74%
Toxicity
A summary of the toxicities associated with this protocol are included in the table below. The most clinically significant toxicities
for this treatment are myelosuppression and febrile neutropaenia.
Grade 3 to 5 toxicity3 Incidence (n=2260)
Neutropaenia 93% (n=238)
Thrombocytopaenia 74% (n=264)
Febrile neutropaenia 54% (n=194)
Infection (neutrophils <1.0 x 109/L) 40% (n=142)
Mucositis 35% (n=112)
Non-neutropaenic infections 24% (n=67)
Hypophosphatemia 14% (n=49)
Neuropathy (motor) 5% (n=16)
Ototoxicity 5% (n=15)
Neuropathy (sensory) 3% (n=9)
References
1 Ramsey, L. B., F. M. Balis, M. M. O'Brien, et al. 2018. "Consensus Guideline for Use of Glucarpidase in Patients with High-
Dose Methotrexate Induced Acute Kidney Injury and Delayed Methotrexate Clearance." Oncologist 23(1):52-61.
2 Meyers, P. A., C. L. Schwartz, M. Krailo, et al. 2005. "Osteosarcoma: a randomized, prospective trial of the addition of
ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate." J Clin Oncol 23(9):2004-2011.
3 Bielack, S. S., S. Smeland, J. S. Whelan, et al. 2015. "Methotrexate, Doxorubicin, and Cisplatin (MAP) Plus Maintenance
Pegylated Interferon Alfa-2b Versus MAP Alone in Patients With Resectable High-Grade Osteosarcoma and Good
Histologic Response to Preoperative MAP: First Results of the EURAMOS-1 Good Response Randomized Controlled Trial."
J Clin Oncol 33(20):2279-2287.
4 Winkler, K., G. Beron, G. Delling, et al. 1988. "Neoadjuvant chemotherapy of osteosarcoma: results of a randomized
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 20 of 21
cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response." J Clin Oncol 6(2):329-337.
5 Bacci, G., S. Ferrari, F. Bertoni, et al. 2000. "Long-term outcome for patients with nonmetastatic osteosarcoma of the
extremity treated at the istituto ortopedico rizzoli according to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: an
updated report." J Clin Oncol 18(24):4016-4027.
History
Version 4
Date Summary of changes
04/09/2020 Biosimilar drug added to clinical information. Version number changed to V.4.
Version 3
Date Summary of changes
08/10/2019 Clinical information updated with PBS expanded indications for GCSF. Drug status updated.
Version 2
Date Summary of changes
31/05/2017 Transferred to new eviQ website. Version number changed to V.2.
Antiemetic change: Netupitant/palonosetron combination has replaced aprepitant and a 5HT3 receptor
antagonist in combination with dexamethasone for all highly emetogenic regimens.
06/06/2017 Approved and published on eviQ. Review in 1 year
15/06/2018 Protocol reviewed by Medical Oncology Reference Committee. No changes. Review 5 years.
25/10/2018 Link added to high dose methotrexate-induced toxicity document in clinical information.
The information contained in this protocol is based on the highest level of available evidence and consensus of the
eviQ reference committee regarding their views of currently accepted approaches to treatment. Any clinician (medical
oncologist, haematologist, radiation oncologist, medical physicist, radiation therapist, pharmacist or nurse) seeking to apply or
consult this protocol is expected to use independent clinical judgement in the context of individual clinical circumstances to
determine any patient's care or treatment. Use is subject to eviQ’s disclaimer available at www.eviQ.org.au
First approved: 6 June 2017
Last reviewed: 15 June 2018
Review due: 30 June 2023
The currency of this information is guaranteed only up until the date of printing, for any updates please check:
https://www.eviq.org.au/p/1901
04 Mar 2021
Osteosarcoma MAP (methotrexate, DOXOrubicin, cISplatin) Page 21 of 21
You might also like
- BFM 2000 Treatment SchemaDocument2 pagesBFM 2000 Treatment SchemaAnonymous 9dVZCnTXSNo ratings yet
- GCC Anti Emetic Guidelines 2003Document2 pagesGCC Anti Emetic Guidelines 2003damondouglasNo ratings yet
- EC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1Document11 pagesEC-DH Epirubicin Cyclophosphamide Followed by Docetaxel With Trastuzumab Protocol V1.1smokkerNo ratings yet
- CALGB Schema FinalDocument1 pageCALGB Schema FinalMohamed MahmoudNo ratings yet
- Bladder Cancer Treatment Regimens: Clinical Trials, Chemotherapy OptionsDocument4 pagesBladder Cancer Treatment Regimens: Clinical Trials, Chemotherapy Optionsc.ramNo ratings yet
- Paclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1Document7 pagesPaclitaxel With EC Adjuvant or Neoadjuvant Protocol V1.1smokkerNo ratings yet
- Acute Lymphoblastic Leukemia Treatment RegimensDocument4 pagesAcute Lymphoblastic Leukemia Treatment Regimensnur-aisyahkNo ratings yet
- Regimen for paediatric ALL risk groupsDocument5 pagesRegimen for paediatric ALL risk groupsGlobal cancerNo ratings yet
- Drugs Name References Dose Prescription Dose InformationDocument2 pagesDrugs Name References Dose Prescription Dose InformationSanithaaaNo ratings yet
- Jpho 2019 02 07 Resham Jpho-18-291r sdc1Document1 pageJpho 2019 02 07 Resham Jpho-18-291r sdc1Naman KhalidNo ratings yet
- Kardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313Document2 pagesKardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313kuro hanabusaNo ratings yet
- Peptic Ulcer Disease: Treatment of Peptic UlcersDocument2 pagesPeptic Ulcer Disease: Treatment of Peptic UlcersKenneth NuñezNo ratings yet
- Endometrialcarcinoma r0416 7941Document2 pagesEndometrialcarcinoma r0416 7941crisibarra911No ratings yet
- Vejiga. CtaDocument11 pagesVejiga. CtaIsabel Gago CastilloNo ratings yet
- Total XVDocument8 pagesTotal XVMohammed HaiderNo ratings yet
- Primary Therapy-Chronic Smoldering: ContinuedDocument2 pagesPrimary Therapy-Chronic Smoldering: ContinuedYuliana Eka RusdiyantiNo ratings yet
- Breast Cancer RegimensDocument6 pagesBreast Cancer RegimensMohammad Arwan HamdaniNo ratings yet
- Commonly Used Premedication Regimens for Chemo and Monoclonal AntibodiesDocument2 pagesCommonly Used Premedication Regimens for Chemo and Monoclonal AntibodiesnurulNo ratings yet
- Premedikasi Dan Cinv: (Chemotherapy Induced Nausea and Vomiting)Document22 pagesPremedikasi Dan Cinv: (Chemotherapy Induced Nausea and Vomiting)Yulian 53No ratings yet
- Paclitaxel Trastuzumab Breast Cancer ProtocolDocument9 pagesPaclitaxel Trastuzumab Breast Cancer ProtocolsmokkerNo ratings yet
- EDP Mitotane Protocol V1.0Document8 pagesEDP Mitotane Protocol V1.0Andrei BuruianăNo ratings yet
- Id 397 TeicoplaninDocument2 pagesId 397 TeicoplaninStacey WoodsNo ratings yet
- Doxorubicin (Conventional) : Drug Information - UpToDateDocument55 pagesDoxorubicin (Conventional) : Drug Information - UpToDateramangNo ratings yet
- Paclitaxel With Dose Dense EC Adjuvant or Neo-Adjuvant Protocol V1.0Document7 pagesPaclitaxel With Dose Dense EC Adjuvant or Neo-Adjuvant Protocol V1.0smokkerNo ratings yet
- Tranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data SheetDocument18 pagesTranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data SheetHatim DziauddinNo ratings yet
- R-Codox M: Patients With Good Performance StatusDocument6 pagesR-Codox M: Patients With Good Performance StatusALEXANDER AVILANo ratings yet
- Breast Cancer Doxorubicin & Cyclophosphamide (AC)Document12 pagesBreast Cancer Doxorubicin & Cyclophosphamide (AC)Rawabi SalehNo ratings yet
- Tranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data SheetDocument19 pagesTranexamic Acid Injection 500 MG/ 5 ML Ampoule New Zealand Data Sheetkashif akhtarNo ratings yet
- Squamous Cell Cancers: Primary Systemic Therapy + Concurrent RadiotherapyDocument5 pagesSquamous Cell Cancers: Primary Systemic Therapy + Concurrent RadiotherapyArjun Singh ChoudharyNo ratings yet
- Temozolomide Protocol for GlioblastomaDocument4 pagesTemozolomide Protocol for GlioblastomaSyed Touseef AhmedNo ratings yet
- Acute Leukemia ProtocolDocument13 pagesAcute Leukemia ProtocolBol Dhalbeny MalualNo ratings yet
- Doxorubicin and Ifosfamide Sarcoma Protocol V1.0Document8 pagesDoxorubicin and Ifosfamide Sarcoma Protocol V1.0Joseph TrevinoNo ratings yet
- LYRICE ProtocolDocument6 pagesLYRICE ProtocolInas UthmanNo ratings yet
- Castration-Recurrent Prostate Cancer First-Line Therapy: No Visceral MetastasesDocument2 pagesCastration-Recurrent Prostate Cancer First-Line Therapy: No Visceral Metastasesalberto cabelloNo ratings yet
- Gigfolfiri ProtocolDocument6 pagesGigfolfiri ProtocolNurfarah BilqisNo ratings yet
- Lab 11 AntianginalDocument4 pagesLab 11 AntianginalanaNo ratings yet
- Regimen Kanker RektumDocument8 pagesRegimen Kanker RektumNurul Kamilah SadliNo ratings yet
- Brain Cancer Treatment Regimens (Part 1 of 5)Document5 pagesBrain Cancer Treatment Regimens (Part 1 of 5)Rubana Reaz TanaNo ratings yet
- Docetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolDocument14 pagesDocetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolsmokkerNo ratings yet
- Dexamethasone (RX) : Dosing & UsesDocument4 pagesDexamethasone (RX) : Dosing & UsesFauzi GanihNo ratings yet
- Pre-Operative Orders Post-Op Orders (Ga)Document3 pagesPre-Operative Orders Post-Op Orders (Ga)Alissandra OcampoNo ratings yet
- NICU Dose Card05Document2 pagesNICU Dose Card05Mohamed Abo SeifNo ratings yet
- Lichen PlanusDocument3 pagesLichen PlanusAna PaunescuNo ratings yet
- Protocol Chimioterapie Leucemii Acute Limfoblastice (LALDocument6 pagesProtocol Chimioterapie Leucemii Acute Limfoblastice (LALMonicaNo ratings yet
- L 51 R Hypercvad R MaDocument7 pagesL 51 R Hypercvad R MaMohamed MahmoudNo ratings yet
- Non-Hodgkin Lymphoma (NHL)Document11 pagesNon-Hodgkin Lymphoma (NHL)archanaNo ratings yet
- NEW ZEALAND DATA SHEET FOR DEXAMETHASONE SODIUM PHOSPHATEDocument15 pagesNEW ZEALAND DATA SHEET FOR DEXAMETHASONE SODIUM PHOSPHATEIsti IzzuddinNo ratings yet
- Delayed Intensification I therapy for Down syndrome patientsDocument1 pageDelayed Intensification I therapy for Down syndrome patientsRitush MadanNo ratings yet
- Indonesian Protocol for Acute Lymphoblastic Leukemia (ALL) 2013Document9 pagesIndonesian Protocol for Acute Lymphoblastic Leukemia (ALL) 2013syongebob100% (1)
- TCHP-Docetaxel Carboplatin Trastuzumab Pertuzumab Neoadjuvant Adjuvant Protocol V2.2Document21 pagesTCHP-Docetaxel Carboplatin Trastuzumab Pertuzumab Neoadjuvant Adjuvant Protocol V2.2smokkerNo ratings yet
- EC-D With HP Epirubicin Cyclophosphamide Followed by Docetaxel Trastuzumab Pertuzumab Neo-Adjuvant and Adjuvant Protocol V2.1Document20 pagesEC-D With HP Epirubicin Cyclophosphamide Followed by Docetaxel Trastuzumab Pertuzumab Neo-Adjuvant and Adjuvant Protocol V2.1smokkerNo ratings yet
- Chemotherapy protocols for trophoblastic neoplasiaDocument3 pagesChemotherapy protocols for trophoblastic neoplasiaImam Hakim SuryonoNo ratings yet
- Protocol Outline Remission Induction (6-7 Weeks)Document3 pagesProtocol Outline Remission Induction (6-7 Weeks)Mohammed HaiderNo ratings yet
- Neoadjuvant or Adjuvant Therapy for Breast Cancer Using DOCEtaxel, CARBOplatin, and TrastuzumabDocument6 pagesNeoadjuvant or Adjuvant Therapy for Breast Cancer Using DOCEtaxel, CARBOplatin, and TrastuzumabMohammed GazoNo ratings yet
- See Full Prescribing Information For Complete Boxed WarningDocument53 pagesSee Full Prescribing Information For Complete Boxed WarningMohammed shamiul ShahidNo ratings yet
- T-All 1Document9 pagesT-All 1Mobin Ur Rehman KhanNo ratings yet
- Amoxicillin 250 MG Capsules-Summary of Product CharacteristicsDocument65 pagesAmoxicillin 250 MG Capsules-Summary of Product CharacteristicsBrown and Burk UK Ltd100% (1)
- Prescription Writing 1Document10 pagesPrescription Writing 1amaygokhale26802No ratings yet
- Pharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamFrom EverandPharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamRating: 5 out of 5 stars5/5 (1)
- Jama 2017 11469Document10 pagesJama 2017 11469Selma MutiaraNo ratings yet
- JTD 04 06 562Document7 pagesJTD 04 06 562Selma MutiaraNo ratings yet
- Clinical Relevance of Folinic Acid Over Rescue AFTER HFMTXDocument6 pagesClinical Relevance of Folinic Acid Over Rescue AFTER HFMTXSelma MutiaraNo ratings yet
- Supp Mdu526 Mdu526suppDocument37 pagesSupp Mdu526 Mdu526suppSelma MutiaraNo ratings yet
- High-Dose Methotrexate-Induced Nephrotoxicity in Patients With OsteosarcomaDocument11 pagesHigh-Dose Methotrexate-Induced Nephrotoxicity in Patients With Osteosarcomaadkhiatul muslihatinNo ratings yet
- Hyper-Alkalinization Without Hyper-Hydration For The Prevention HDMTX Acute NefrotoxicDocument5 pagesHyper-Alkalinization Without Hyper-Hydration For The Prevention HDMTX Acute NefrotoxicSelma MutiaraNo ratings yet
- Ambulatory High-Dose Methotrexate Administration Among Pediatric Osteosarcoma Patients in An Urban, Underserved Setting Is Feasible, Safe, and Cost-EffectiveDocument4 pagesAmbulatory High-Dose Methotrexate Administration Among Pediatric Osteosarcoma Patients in An Urban, Underserved Setting Is Feasible, Safe, and Cost-EffectiveSelma MutiaraNo ratings yet
- Toxicity HDMTX OsDocument9 pagesToxicity HDMTX OsSelma MutiaraNo ratings yet
- High-Dose Methotrexate And:or Leucovorin Rescue For The Treatment of Children With Lymphoblastic Malignancies - Do We Really Know Why, When and How?Document8 pagesHigh-Dose Methotrexate And:or Leucovorin Rescue For The Treatment of Children With Lymphoblastic Malignancies - Do We Really Know Why, When and How?Selma MutiaraNo ratings yet
- Dengue: BIKO Penyakit Dalam 2016Document42 pagesDengue: BIKO Penyakit Dalam 2016Melinda MarianniNo ratings yet
- Laporan Jaga IGD 24 Juni 2019Document16 pagesLaporan Jaga IGD 24 Juni 2019Selma MutiaraNo ratings yet
- Diagnosis and Management of Acute StrokeDocument74 pagesDiagnosis and Management of Acute StrokeDonnaBells Hermo Labaniego100% (2)
- Tambahan Refkas BSDocument18 pagesTambahan Refkas BSSelma MutiaraNo ratings yet
- EBM-Internal Med Students-FinalDocument29 pagesEBM-Internal Med Students-FinalSelma MutiaraNo ratings yet
- FIX BOOK Reading Treatment FractureDocument52 pagesFIX BOOK Reading Treatment FractureSelma MutiaraNo ratings yet
- Viral Skin Infections Caused by Herpesviridae and PoxviridaeDocument55 pagesViral Skin Infections Caused by Herpesviridae and PoxviridaeGita RizkiNo ratings yet
- Medical Ethics - Bioethical PrinciplesDocument2 pagesMedical Ethics - Bioethical PrinciplesApril AramNo ratings yet
- APPLY TAFE NSW COURSESDocument4 pagesAPPLY TAFE NSW COURSESiltiNo ratings yet
- 21 CFR Part 111, Dietary Supplement CGMP - Background, Development, Content, Comparison To Drug CGMP, and The FutureDocument9 pages21 CFR Part 111, Dietary Supplement CGMP - Background, Development, Content, Comparison To Drug CGMP, and The Futuremelimaulani-1No ratings yet
- Beatriz Echeverri ResumeDocument1 pageBeatriz Echeverri Resumeapi-436063355No ratings yet
- NMI Board Nursing Licensure RequirementsDocument2 pagesNMI Board Nursing Licensure RequirementsCassandraNo ratings yet
- James Andretich Resume #2Document2 pagesJames Andretich Resume #2Abbey DavisNo ratings yet
- DiphtheriaDocument18 pagesDiphtheriaShishir ShresthaNo ratings yet
- Tongue Tie 2016Document6 pagesTongue Tie 2016drchiNo ratings yet
- Microwave Effects on Human TissuesDocument4 pagesMicrowave Effects on Human TissuesLazlo SecretNo ratings yet
- 713-Article Text-2302-1-10-20180613Document9 pages713-Article Text-2302-1-10-20180613nareNo ratings yet
- Advantages: Bigger SavingsDocument2 pagesAdvantages: Bigger SavingsGerwin Inca BualoyNo ratings yet
- Domestic Violence BrochureDocument2 pagesDomestic Violence Brochureapi-546372896No ratings yet
- How To Detach Unwanted PeopleDocument4 pagesHow To Detach Unwanted PeopleDevanshi Mohan100% (1)
- Entendimiento de Los Datos DisponiblesDocument10 pagesEntendimiento de Los Datos DisponiblesJose Miguel González PeraltaNo ratings yet
- Lifting and Handling of Casualty HandoutsDocument6 pagesLifting and Handling of Casualty HandoutsIvy Jorene Roman RodriguezNo ratings yet
- Electroplating IndustryDocument5 pagesElectroplating IndustryRangasamyNo ratings yet
- IOP Final PDFDocument132 pagesIOP Final PDFLaiba SiddiquiNo ratings yet
- Fact Sheet 11 - DebriefingDocument3 pagesFact Sheet 11 - Debriefingkhushi.avatharaNo ratings yet
- Housekeeping For Grades 7 and 8Document38 pagesHousekeeping For Grades 7 and 8melvin ariasNo ratings yet
- Bulletin 161015 (PDF Edition)Document128 pagesBulletin 161015 (PDF Edition)Darrell BrownNo ratings yet
- Pathology of The Respiratory SystemDocument57 pagesPathology of The Respiratory SystemAngelic khanNo ratings yet
- CBT Pragmatic ApproachDocument10 pagesCBT Pragmatic ApproachMikey StanleyNo ratings yet
- Cover Letter - Meghan L. ShalvoyDocument1 pageCover Letter - Meghan L. ShalvoyMeghan Equality ShalvoyNo ratings yet
- Violent Video GamesDocument7 pagesViolent Video Gamesapi-356126032No ratings yet
- Affirmations For Gratitude: P N Gautam - @theseekerofwisdom - Manifestation CoachDocument5 pagesAffirmations For Gratitude: P N Gautam - @theseekerofwisdom - Manifestation CoachKartikeyNo ratings yet
- Jaundice-Review of Clinical Features, Differential Diagnosis and RemediesDocument13 pagesJaundice-Review of Clinical Features, Differential Diagnosis and RemediesDr-Dalya ShakirNo ratings yet
- Essay 3 Acid Rain KraynyayaDocument9 pagesEssay 3 Acid Rain Kraynyayaapi-512016052No ratings yet
- Instruction and Information Sheet For SF 180, Request Pertaining To Military RecordsDocument3 pagesInstruction and Information Sheet For SF 180, Request Pertaining To Military RecordsAnthony Bonafide Dakush100% (1)
- MCL Agnes Q4Document12 pagesMCL Agnes Q4Luqman Hakim Bin As'ariNo ratings yet