Professional Documents
Culture Documents
Lab 11 Antianginal
Uploaded by
anaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lab 11 Antianginal
Uploaded by
anaCopyright:
Available Formats
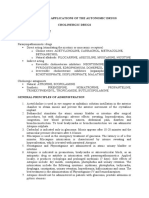
PRACTICAL APPLICATIONS OF THE ANTIANGINAL DRUGS
I. THEORETICAL PART
Antianginal drugs reestablish the balance between the oxygen demand and supply in
the ischemic myocardium, with decreasing the frequency of angina crisis. They act through:
Decreasing the cardiac activity (lower intotropism, chronotropism)
Decreasing the peripheral resistance (vasodilation)
The association of both
Antianginal substances increase the oxygen supply and decrease the myocardial
oxygen consumption, modifying the factors that have an influence upon this consumption:
The stress in the myocardial wall (dependent to the intraventricular pressure,
ventricular radius, wall thickness)
Heart rate
Contractility
CLASSIFICATION
Organic nitrates
• GLYCERYL TRINITRATE (GTN) – NITROGLYCERINE
• ISOSORBIDE DINITRATE (ISDN)
• ISOSORBIDE 5 MONONITRATE (ISMN)
• PENTAERYTHRITYL TETRANITRATE
Other antianginal drugs
• MOLSIDOMIN
• BETA BLOCKERS
• CALCIUM CHANNEL BLOCKERS
• IVABRADIN (inhibitor of the SN)
• RANOLAZINE (inhibitor of the sodium influx)
GENERAL PRINCIPLES OF ADMINISTRATION
1. Nitrates are indicated in coronary diseases (ischemic cardiopathy, AMI) and in heart
failure (only in association with other drugs).
2. In angina pectoris crisis, short acting, sublingual nitrates are administered:
Nitroglycerine 1 tablet or 1 puff. The dose may be repeated after a few minutes. If
there is no relief after the third administration, the patient should see a doctor,
suspecting an AMI.
3. The patient should always have Nitroglycerin available, which can be used also in
prophylaxis, if the patient knows the determing circumstances of an angina crisis
(physical effort, stress).
4. Nitroglycerine for sublingual use expires quickly, after 6 months (do not prescribe
several packages).
5. Nitrates with a long duration of action (oral or transdermic) are prescribed for the
prophylaxis of angina crisis together with beta blockers or calcium channel blockers,
in the daily treatment of ischemic cardiopathy.
6. The transdermic patch with Nitroglycerine should be applied on healthy, dry, hairless
and clean skin. For a better adhesion to the skin, it should be kept pressed with the
palm for several seconds. A patch that has been used, should be never reapplied.
Nitroderm TTS 5 (5 mg/24 hours) releases a dose of 0.2 mg/hour for a contact surface
of 10 cm2.
7. Nitrates can be responsible of hypotension (especially after the first dose or in case of
increasing the dose) and reflex tachycardia, with dizziness and fatigue. Another
adverse effect of nitrates is the tolerance, which appears after a prolonged treatment.
For the prevention, nitrates should be discontinued during the therapy and replaced by
another antianginal drug.
8. Molsidomin is a vasodilator with an antiplatelet effect. It is used as an alternative in
patients with severe headache after nitrates, 2 tab./day.
9. In patients with ischemic cardiopathy, the antianginal treatment should be associated
with an antiplatelet agent (Aspirin 75-100 mg/day, Ticlopidin 2 tab/day) and
sometimes with an antilipemic drug.
10. The administration of Ivabradine or Ranolazine require EKG monitoring.
THE TREATMENT IN AMI
1. Oxygen 4-8 l/min
2. Antianginal treatment
• GTN
• 1 tab/puff sublingual every 5 min, max. 3x
• IV infusion 1-3 mg/h (in left heart failure up to 6 mg/h)
• Beta blockers, in case of GTN failure or tachycardia, but without left heart
failure
• Calcium channel blockers (not dihydropyridines), in case of GTN and beta
blockers failure
3. Antiplatelet agents
• Aspirin
• 150-300 mg p.o. (250 mg IV), continue with 75-100 mg/day, plus
• ADP antagonist (asap, plus 12 months)
• 60 mg Prasugrel or 180 mg Ticagrelor
• 600 mg Clopidogrel in absence of Prasugrel or Ticagrelor
4. Anticoagulants
• In NSTEMI: Fondaparinux or Enoxaparin or UFH
• In STEMI:
• First choice: PCI, plus Enoxaparin or UFH
• Second choice: Streptokynase 1.5 mil. IU in 30-60 min or Alteplase
(expensive) 15 mg bolus IV => 0.75 mg/kg in 30 min => 0.5 mg/kg in
60 min.
5. Analgesics
• 3-5 mg IV Morphin, possibly repeat in min.
Preparations
Generic drug Brand name Route of Pharmaceutical
administration dosage form
Glyceryl trinitrate Nitroglicerina sublingual Tab. 0,5 mg
Nitromint sublingual Spray 0,4 mg/puff
Nitroderm(R) transdermic Patch 5mg/24h
TTS 5
Trinitrosan IV Conc. for infusion
5mg/ml
Nitroglicerina apply on skin Ointment 2%,
precordial
Isosorbide dinitrate Isodinit p.o. Tab. 10 mg
Isosorbide mononitrate Olicard p.o. Tab. 40 mg, 60 mg
Pentaerythrityl Pentalong p.o. Tab. 20 mg, 50 mg
tetranitrate
Molsidomin Corvasal p.o. Tab. 2 mg
IV Vials 2 mg/l ml
Ivabradin Bixebra p.o. Tab. 5 mg, 7,5 mg
Ranolazine Ranexa p.o. Tab. 375 mg, 500 mg,
750 mg
PRACTICAL APPLICATIONS OF THE ANTIARRHYTHMIC DRUGS
Antiarrhythmics are drugs which depress the myocardial automatism, conductance and
excitability, administered in the prophylaxis and treatment of cardiac arrhythmias.
CLASSIFICATION
I. Sodium channel blockers
I.A prolong repolarization: QUINIDINE, PROCAINAMIDE, DISOPYRAMIDE
I.B shorten repolarization: LIDOCAINE, TOCAINIDE, MEXILETINE,
PHENYTOIN
I.C little effect on repolarization: FLECAINIDE, PROPAFENONE, MORICIZINE
II. Beta blockers: PROPRANOLOL, ESMOLOL, METOPROLOL, ATENOLOL
III. Potassium channel blockers : AMIODARONE, SOTALOL, BRETYLIUM
IV. Calcium channel blockers: VERAPAMIL, DILTIAZEM
V. Antiarrhythmics that work by other or unknown mechanism: ADENOSINE, DIGOXIN
GENERAL PRINCIPLES OF ADMINISTRATION
1. The antiarrhtythmic should be prescribed only after the arrhythmia was proven on the
EKG/Holter and the risk is superior compared to the side effects of the drug. All
antiarrhythmics have the paradoxal proarrhythmic effect.
2. Before starting the treatment, the patient’s heart function should be evaluated, the
favouring factors for arrhythmias treated (hypokalemia, hypomagnesemia) and
arrhythmogenic drugs administration should be stopped (sympathomimetics, Miofilin,
tricyclic antidepressants).
3. The dose should be individualised, according to the EKG and the response to the
treatment.
4. Most of the antiarrhythmics have a negative inotropic effect and should not be given
in heart failure. Exceptions: Amiodarone, Lidocaine, beta blockers.
5. The pharmacological conversion to sinus rhythm in recurrent atrial fibrillation can be
made outside the hospital by administering a single dose of Propafenone or Flecainide
(„pill-in-the-pocket”).
6. In atrial fibrillation, besides the antiarrhythmic, an anticoagulant treatment should be
administered to prevent a stroke or AMI.
THE EMERGENCY TREATMENT IN ATRIAL FIBRILLATION
• WITH HEART FAILURE
• Amiodarone IV 150-300 mg. If no response:
• Digoxin IV 0.25 mg every 2 hours until reaching the dose of 1.5 mg
• WITHOUT HEART FAILURE
• Beta blocker IV: Esmolol 0.5 mg/kg in one min. => 0.05-0.2 mg/kg/min or
Metoprolol 2.5-5 mg in 2 min. or Propranolol 0.15 mg/kg or
• Verapamil IV 0.075-0.15 mg/kg in 2 min or Diltiazem IV 0.25 mg/kg in 2 min
=> 5-15 mg/h
THE EMERGENCY TREATMENT IN VENTRICULAR TACHYCARDIA
• IN HEMODYNAMICALLY STABLE PATIENT
• First line: Amiodarone
• Second line: Lidocaine IV 1-2 mg/kg or infusion 2-4 mg/min
• Potassium and magnesium
• IN HEMODYNAMICALLY UNSTABLE PATIENT
• Short IV anesthesia and cardioversion
• In cardiorespiratory arrest: cardiopulmonary resuscitation
II. PRACTICAL PART
1. Write a medical prescription to a patient with ischemic cardiopathy. Effort induced
angina pectoris.
You might also like
- The Crash CartDocument39 pagesThe Crash Cartpramod kumawat100% (1)
- IM On Call (LANGE On Call) PDFDocument738 pagesIM On Call (LANGE On Call) PDFindia2puppy100% (8)
- Pharmacology Viva QuestionsDocument24 pagesPharmacology Viva QuestionsMinhaz Islam100% (1)
- Basic Pharmacology And Drug Calculations [Practice Questions And Answers]From EverandBasic Pharmacology And Drug Calculations [Practice Questions And Answers]Rating: 4 out of 5 stars4/5 (1)
- Antiarrhythmic Drugs Classification (Vaughan Williams)Document8 pagesAntiarrhythmic Drugs Classification (Vaughan Williams)ana100% (1)
- Emergency DrugsDocument47 pagesEmergency DrugsBesimanNo ratings yet
- Anti-Anginal DrugsDocument39 pagesAnti-Anginal Drugspoonam rana100% (1)
- Angina Pectoris & Anti Anginal DrugsDocument46 pagesAngina Pectoris & Anti Anginal DrugsMohammad AliNo ratings yet
- LECTURE 9 Positive InotropicDocument5 pagesLECTURE 9 Positive InotropicanaNo ratings yet
- 06 JunioDocument152 pages06 Juniocristian GamaNo ratings yet
- 25 Address PDF MergedDocument1,744 pages25 Address PDF Mergedsanjay_gawaliNo ratings yet
- ACLS DrugsDocument16 pagesACLS Drugstostc100% (2)
- Drugs Used in Myocardial InfarctionDocument53 pagesDrugs Used in Myocardial InfarctionSandeep KannegantiNo ratings yet
- Pharmacology of The Gastrointestinal Drugs (I)Document12 pagesPharmacology of The Gastrointestinal Drugs (I)anaNo ratings yet
- Price List Pt. Hexpharm Jaya 2020Document3 pagesPrice List Pt. Hexpharm Jaya 2020RetnoSFadhillahNo ratings yet
- On Emergency DrugsDocument25 pagesOn Emergency DrugsBikram Chhetry100% (1)
- ANTI-ARRHYTHMIC DRUGS Veterinary PharmacologyDocument5 pagesANTI-ARRHYTHMIC DRUGS Veterinary PharmacologyljramosNo ratings yet
- Nitrates andDocument61 pagesNitrates andMrunalini DandamudiNo ratings yet
- Pharmacology RevisedDocument59 pagesPharmacology Revisedjohnstockton12100% (1)
- Nitrates Comparison ChartDocument7 pagesNitrates Comparison ChartModi Evana PutriNo ratings yet
- Pharmacology of Antianginal Drugs: Tri Widyawati M. IchwanDocument43 pagesPharmacology of Antianginal Drugs: Tri Widyawati M. IchwanYohanna SinuhajiNo ratings yet
- Drugs 2018 FebDocument143 pagesDrugs 2018 FebTuliNo ratings yet
- Role of Nitrates in Angina: Satabdi Ghosh Phase A Resident Department of Pharmacology, BSMMUDocument17 pagesRole of Nitrates in Angina: Satabdi Ghosh Phase A Resident Department of Pharmacology, BSMMUMehediNo ratings yet
- Supply Chain & Inventory ControlDocument99 pagesSupply Chain & Inventory ControlSUMIT MASKENo ratings yet
- Emergency Drugs GuideDocument8 pagesEmergency Drugs GuideShehnaz SheikhNo ratings yet
- ED Dilution Guide 2018 - Jan 2019Document42 pagesED Dilution Guide 2018 - Jan 2019asyrafrusydi9901No ratings yet
- Emergency Tray PesentationDocument14 pagesEmergency Tray Pesentationgaladimawa2002No ratings yet
- A Drug Study On: EpinephrineDocument16 pagesA Drug Study On: EpinephrineJay Jay JayyiNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument112 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreabctutorNo ratings yet
- Antianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheDocument10 pagesAntianginal Drugs Antianginal Drugs Are Used Primarily To Restore The Balance Between TheMIR SARTAJNo ratings yet
- Cardiac DrugDocument32 pagesCardiac DrugSalim MinjNo ratings yet
- Drugs Study Neh Jai2xDocument10 pagesDrugs Study Neh Jai2xjai2xNo ratings yet
- Cad Sihd 2Document67 pagesCad Sihd 2mohammedghassan53No ratings yet
- InotropicsDocument20 pagesInotropicsMalathi VarnaNo ratings yet
- Clinical Cases Pharmacology PDFDocument7 pagesClinical Cases Pharmacology PDFAnkur HazraNo ratings yet
- BretyliumDocument4 pagesBretyliumButchay LumbabNo ratings yet
- Cardiac Medications: 1. Antiplatelet Aggregation Therapy: Antiplatelet Aggregation TherapyDocument14 pagesCardiac Medications: 1. Antiplatelet Aggregation Therapy: Antiplatelet Aggregation TherapyMaria OnofreiNo ratings yet
- Antidotes, Anticholinergics and Antibiotics: Amrit Pokhrel PharmacistDocument21 pagesAntidotes, Anticholinergics and Antibiotics: Amrit Pokhrel PharmacistheenamaharjanNo ratings yet
- Farma StrokeDocument37 pagesFarma StrokeDAHLIANo ratings yet
- Relief of Pain, Inflammation and Rheumatic ConditionsDocument16 pagesRelief of Pain, Inflammation and Rheumatic Conditionsdemolay03No ratings yet
- Antiarrhytmic Talk For ResidenDocument90 pagesAntiarrhytmic Talk For ResidenMusa yohanaNo ratings yet
- Outpatient MedicineDocument190 pagesOutpatient MedicineLikoh TimothyNo ratings yet
- Mosby - Mosby's Drug Reference For Health Professions, 4e-Mosby (2013) - DeletedDocument3 pagesMosby - Mosby's Drug Reference For Health Professions, 4e-Mosby (2013) - DeletedehsanNo ratings yet
- Problem 2Document9 pagesProblem 2Chan Myae NaingNo ratings yet
- Atrial Flutter Medication: Drugs DoseDocument8 pagesAtrial Flutter Medication: Drugs DoseVictoria Castillo TamayoNo ratings yet
- Management Strategy in Hypertensive Crisis The Role of NicardipineDocument38 pagesManagement Strategy in Hypertensive Crisis The Role of Nicardipinezulfikar adiNo ratings yet
- Cardiac DrugsDocument21 pagesCardiac DrugsMona MahfouzNo ratings yet
- OBAT PADA REAKSI HIPERSENSITIVITASDocument59 pagesOBAT PADA REAKSI HIPERSENSITIVITASM Rasya SanimanNo ratings yet
- CardioDocument28 pagesCardioKristine Joy CamusNo ratings yet
- Master Emergency Drugs Before U Practise DR Vishwa Medical CoachingDocument6 pagesMaster Emergency Drugs Before U Practise DR Vishwa Medical Coachingابو عبد الرحمنNo ratings yet
- Atropine: IndicationDocument2 pagesAtropine: IndicationgugicevdzoceNo ratings yet
- Cardiovascular Drugs and Therapies Nitrates Comparison ChartDocument7 pagesCardiovascular Drugs and Therapies Nitrates Comparison ChartArvi J-idNo ratings yet
- ST-Elevation Myocardial Infarction (STEMI) Diagnosis and TreatmentDocument8 pagesST-Elevation Myocardial Infarction (STEMI) Diagnosis and TreatmentamiraNo ratings yet
- Lab 9 RespitatoryDocument3 pagesLab 9 RespitatoryanaNo ratings yet
- Cardiology and endocrine dosesDocument3 pagesCardiology and endocrine dosesSelim TarekNo ratings yet
- AMI Management For 2 ND Year StudentsDocument3 pagesAMI Management For 2 ND Year StudentsShubham TarapureNo ratings yet
- Common Emergency DrugsDocument61 pagesCommon Emergency DrugsFebee Gee100% (1)
- Commonly Used Critical Care Medications: IV Bolus 6 MG, If Conversion To NSR Does Not Occur Within 1-2Document7 pagesCommonly Used Critical Care Medications: IV Bolus 6 MG, If Conversion To NSR Does Not Occur Within 1-2ciptaarynNo ratings yet
- Prescription Writing 1Document10 pagesPrescription Writing 1amaygokhale26802No ratings yet
- 2 2015 Nsaid Analgetik AntipiretikaDocument65 pages2 2015 Nsaid Analgetik AntipiretikasekarNo ratings yet
- Antianginal Drugs Are Used Primarily To Restore The Balance Between The Oxygen SupplyDocument8 pagesAntianginal Drugs Are Used Primarily To Restore The Balance Between The Oxygen SupplyUzma KhanNo ratings yet
- GP RSD KALABAHI drug formularyDocument2 pagesGP RSD KALABAHI drug formularyyosaNo ratings yet
- Cardiac Glycosides and Phosphodiesterase InhibitorsDocument30 pagesCardiac Glycosides and Phosphodiesterase Inhibitorskenneth santosNo ratings yet
- Pertemuan 7 LiyanaDocument36 pagesPertemuan 7 LiyanaLiyana SafitriNo ratings yet
- Infant Care - Practical Course PDFDocument165 pagesInfant Care - Practical Course PDFBogdan MariusNo ratings yet
- Ultrasound 20atlas 20of 20clinical 20casesDocument119 pagesUltrasound 20atlas 20of 20clinical 20casesTimbur IgorNo ratings yet
- Chirurgie PrimaraDocument144 pagesChirurgie PrimaraElena ConstantinNo ratings yet
- Vladimir Fluture-The Path From The Surgical Dream To The Perfect Operation Ebook Final PDFDocument115 pagesVladimir Fluture-The Path From The Surgical Dream To The Perfect Operation Ebook Final PDFAdriana DuțăNo ratings yet
- Infant 20care 202020 PDFDocument226 pagesInfant 20care 202020 PDFRusaneanu Robert-CatalinNo ratings yet
- Infant 20care 202020 PDFDocument226 pagesInfant 20care 202020 PDFRusaneanu Robert-CatalinNo ratings yet
- LAB 8 MGE-drugsDocument2 pagesLAB 8 MGE-drugsanaNo ratings yet
- Lab PharmacoDocument51 pagesLab PharmacoanaNo ratings yet
- The 20human 20body. 20a 20sum 20of 20anthropological 20introductions PDFDocument136 pagesThe 20human 20body. 20a 20sum 20of 20anthropological 20introductions PDFRusaneanu Robert-CatalinNo ratings yet
- Farmaco LectureDocument117 pagesFarmaco LectureanaNo ratings yet
- Lab 7-Practic Aplic.Document5 pagesLab 7-Practic Aplic.anaNo ratings yet
- Infant Care - Practical Course PDFDocument165 pagesInfant Care - Practical Course PDFBogdan MariusNo ratings yet
- Human Anatomy Central Nervous System PDFDocument75 pagesHuman Anatomy Central Nervous System PDFBogdan MariusNo ratings yet
- Practical Applications of The Antihypertensive Drugs I. Theoretical Part ClassificationDocument4 pagesPractical Applications of The Antihypertensive Drugs I. Theoretical Part ClassificationanaNo ratings yet
- Lab 9 RespitatoryDocument3 pagesLab 9 RespitatoryanaNo ratings yet
- The Pharmacology of AntithromboticsDocument14 pagesThe Pharmacology of AntithromboticsanaNo ratings yet
- LAB 12+13 Blood Medic.Document4 pagesLAB 12+13 Blood Medic.anaNo ratings yet
- Human Body and Skeleton Medical VocabularyDocument3 pagesHuman Body and Skeleton Medical VocabularyanaNo ratings yet
- Human Anatomy Central Nervous System PDFDocument75 pagesHuman Anatomy Central Nervous System PDFBogdan MariusNo ratings yet
- Pharmacology of The Gastrointestinal Drugs (Ii) Choleretics, Cholagogues and Other Biliary Secretion ModifiersDocument14 pagesPharmacology of The Gastrointestinal Drugs (Ii) Choleretics, Cholagogues and Other Biliary Secretion ModifiersanaNo ratings yet
- LECTURE 8 AntihypertensiveDocument18 pagesLECTURE 8 AntihypertensiveanaNo ratings yet
- Drugs Acting On The Blood and The Blood-Forming Organs Pharmacology of Antianemic DrugsDocument6 pagesDrugs Acting On The Blood and The Blood-Forming Organs Pharmacology of Antianemic DrugsanaNo ratings yet
- Dialog Medic PacientDocument4 pagesDialog Medic PacientanaNo ratings yet
- Pulmonary Pharmacology Anticoughing AgentsDocument10 pagesPulmonary Pharmacology Anticoughing AgentsanaNo ratings yet
- Laporan Apotik Ugd Stok OpnameDocument26 pagesLaporan Apotik Ugd Stok OpnameIndSara 07No ratings yet
- PRICELIST JANUARI 2022 (AutoRecovered)Document26 pagesPRICELIST JANUARI 2022 (AutoRecovered)taufanmjNo ratings yet
- Antitussives & MucolyticsDocument50 pagesAntitussives & MucolyticsSaha DirllahNo ratings yet
- Bogash 1963Document5 pagesBogash 1963wahyu santikaNo ratings yet
- Ejercicio 1. Unidad 1 ReadingDocument5 pagesEjercicio 1. Unidad 1 ReadingLenNo ratings yet
- Transes Fundamentals of PharmacologyDocument4 pagesTranses Fundamentals of PharmacologyCHINGCHONG SLAYERNo ratings yet
- Pharmacology Assignment - Medicines and MealsDocument15 pagesPharmacology Assignment - Medicines and MealsFarhat JahanNo ratings yet
- Dosage FormDocument5 pagesDosage Formqbn9vx7t9jNo ratings yet
- Laporan Perencanaan Perbekalan FarmasiDocument11 pagesLaporan Perencanaan Perbekalan FarmasikarinaNo ratings yet
- warfarin (Coumadin) - UW Medicine Anticoagulation Services Https Sites - Uw.edu Anticoag Drugs WarfarinDocument12 pageswarfarin (Coumadin) - UW Medicine Anticoagulation Services Https Sites - Uw.edu Anticoag Drugs Warfarintl drNo ratings yet
- Basic principles of pharmacology classification and drug administrationDocument4 pagesBasic principles of pharmacology classification and drug administrationJayla MarieNo ratings yet
- Copaxone - Ms Drug StudyDocument1 pageCopaxone - Ms Drug StudygraceNo ratings yet
- Injeksi & Oplosan ObatDocument16 pagesInjeksi & Oplosan ObatFebriani RatnaNo ratings yet
- 3.one Compartment Open ModelDocument15 pages3.one Compartment Open ModelSAM KNo ratings yet
- Dangerous DrugsDocument9 pagesDangerous DrugsEarvin Recel GuidangenNo ratings yet
- Sympathomimetics Physical MCQDocument4 pagesSympathomimetics Physical MCQMohamed MoustafaNo ratings yet
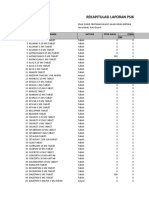
- Rekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFDocument9 pagesRekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFlarasNo ratings yet
- Websitecompanies NewDocument33 pagesWebsitecompanies NewRajiv JulakantiNo ratings yet
- LED-Face-Mask-Consultation-Form - 2Document2 pagesLED-Face-Mask-Consultation-Form - 2Hanan AnsariNo ratings yet
- List Signals Discussed Prac September 2012 - en Till 31-07-2023Document62 pagesList Signals Discussed Prac September 2012 - en Till 31-07-2023Amany HagageNo ratings yet
- @jeeneetprep PGMEE Test SeriesDocument410 pages@jeeneetprep PGMEE Test SeriesL.ABHISHEK KUMARNo ratings yet
- Autocoids 1Document9 pagesAutocoids 1Rutwik YNo ratings yet
- Active Ingredients: Benzocaine, Bismuth Subgallate, Zinc Oxide, MentholDocument2 pagesActive Ingredients: Benzocaine, Bismuth Subgallate, Zinc Oxide, MentholHellcroZNo ratings yet
- Biovion Pharma Product List January 2021Document4 pagesBiovion Pharma Product List January 2021syedsajjadaliNo ratings yet
- Pharmexil - All MixedDocument14 pagesPharmexil - All MixedLisa RayNo ratings yet
- Principles of Drug TherapyDocument8 pagesPrinciples of Drug TherapySNo ratings yet




![Basic Pharmacology And Drug Calculations [Practice Questions And Answers]](https://imgv2-2-f.scribdassets.com/img/word_document/475660044/149x198/2c7fc45015/1691161640?v=1)