Professional Documents
Culture Documents
Thyroid: Anatomical, Physiological Considerations and Thyroid Dysfunction
Uploaded by
sindhura chillara0 ratings0% found this document useful (0 votes)
12 views60 pagesThyroid anesthesia
Original Title
Thyroid
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThyroid anesthesia
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views60 pagesThyroid: Anatomical, Physiological Considerations and Thyroid Dysfunction
Uploaded by
sindhura chillaraThyroid anesthesia
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 60
THYROID- ANATOMICAL, PHYSIOLOGICAL
CONSIDERATIONS AND THYROID DYSFUNCTION
MODERATOR: Dr. Y. ATCHYUTH,
ASSISTANT PROFESSOR, DEPARTMENT OF
ANAESTHESIOLOGY, RANGARAYA MEDICAL COLLEGE
PRESENTOR: SINDHURA, PG STUDENT
Word THYROID was coined by THOMAS
WHARTON
Gr THYREOS=shield; EDIDOS= from
THYROID ANATOMY
LOCATION: Lower part
of the front and side of
the neck opposite to the
c5,c6,c7 and T1
vertebrae, clasping the
upper part of the trachea
WEIGHT : about 20-25
grams
DIMENSIONS:
lobes: 5*3*2 cms
isthmus: 1.25*1.25 cms
CAPSULE
TRUE CAPSULE: peripheral condensation of fibrous
stroma of the gland
FALSE CAPSULE: splitting of pretracheal fascia, it
attaches to body of hyoid and cricoid cartilage
As laryngeal cartilages move up and
down with swallowing, thyroid also
moves.
Dense venous capsule lies deep to
true capsule, so gland is removed
along with true capsule
RELATIONS OF THE GLAND
Superior Thyroid Artery: A branch
ARTERIAL SUPPLY of external carotid artery. Lies close
to external laryngeal nerve and must
be ligated as close to the gland as
possible
Inferior thyroid artery: a branch
of thyrocervical trunk. Intimately
related to recurrent laryngeal nerve
and ligated as far away from the
gland as possible
Thyroid ima artery(30% cases):
branch of brachiocephalic trunk or
arch of aorta
Accessory thyroid arteries: arises
from tracheal and esophageal
arteries
Blood flow to the gland is 4-
6ml/gm/min. sometimes may reach
1litre/min in large goitres
LYMPHATIC
VENOUS DRAINAGE DRAINAGE
NERVE SUPPLY
Parasympathetic supply- Vagus; recurrent laryngeal
nerve
Sympathetic supply- Superior, middle and inferior
cervical sympathetic ganglia.
PHYSIOLOGY- THYROID HORMONE
SYNTHESIS
1. IODINE TRAP:
Dietary iodine is reduced to iodide in the Gastro
Intestinal tract
It is absorbed into the thyroid gland against the
concentration gradient of 1:5
In thyrotoxicosis, the concentration gradient can be
as high as 1:20
2. OXIDATION AND ORGANIFICATION:
Iodine is oxidized to iodine and is bound to tyrosine
to form monoiodo and di iodo tyrosines by thyroid
peroxidase
3. COUPLING:
Mono iodo tyrosine and di iodo tyrosine coupled
enzymatically by thyroid peroxidase to form either T3 or T4
4. STORAGE:
T3 and T4 are stored after attaching to thyroglobulin protein
as colloid in the gland
5. RELEASE AND RECYCLING:
The release of T3 and T4 through proteolysis from
thyroglobulin and diffusion into the circulation.
The remaining mono iodo and di iodo tyrosines are recycled
for formation of T3 and T4.
THYROID HORMONES
T4: Daily T4 released: 80 to 100mcg/kg
Half life: 7 days
Highly protein bound
T3: 20% secreted by thyroid gland and 80% by extra
thyroidal conversion from T4
biologically active
Half life: 24 to 30 hours
PHYSIOLOGICAL EFFECTS OF THYROID HORMONES
THYROID DYSFUNCTION
HYPERTHYROIDISM
Hyper functioning of the
thyroid gland with
excessive secretion of
active thyroid hormones
Thyrotoxicosis is its
clinical manifestation
when the body tissue is
excessively stimulated
by increased Thyroid
hormones
PATHOPHYSIOLOGY
Increase GI motility, O2 consumption, BMR and heat
production.
Increased metabolism leads to :-
- Negative nitrogen balance.
- Lipid depletion.
- Nutritional deficiency.
- Increased O2 consumption
Increase bone and protein turnover, glycogenolysis,
hepatic gluconeogenesis, intestinal glucose absorption,
cholesterol synthesis and degradation
Thyroid Hormones results in positive inotropic and
chromotropic effect by increasing calcium- ATPase and β-
adrenergic receptors amount and sensitivity. This results:-
- Tachycardia
- Increased Cardiac Output and stroke volume.
- Increased adrenergic responsiveness.
- Increased peripheral vasodilation and blood flow.
High BMR → raises body Temperature→ peripheral
vessel dilatation → forces the CO to increase → may lead
to high output failure.
CLINICAL FEATURES:
Symptoms: hyperactivity, weight loss and tremor,
palpitation, anxiety/nervousness, diarrhea, intolerance to
heat, large muscle group weakness, menstrual abnormalities.
Signs: tachycardia ( ↑ sleeping PR), warm moist skin,
irregularly irregular pulse, fine brittle hair, ↑ Cardiac Output,
Ischemic Heart Disease, Heart Failure .
Eye signs: 1. Eyelid retraction.
2. Lid lag sign.
3. Joffroy sign-absence of wrinkling.
4. Mobius sign-difficulty in convergence.
5. Stellwag’s sign-absence of blinking.
TREATMENT
Antithyroid drugs: methimazole or proylthiouracil ( PTU)
interfere with thyroid hormone synthesis. PTU also inhibits the
peripheral conversion of T4 to T3.
Carbimazole: 15-40mg daily till euthyroid & then 5-15mg
PTU:200-400mg daily till euthyroid & then 50-150mg
Methimazole:15-60mg divided every 12hrs.
Although blockage of hormones synthesis is rapid, clinical
improvement occurs after few weeks or months ,because a large
pool of stored hormone continues to be released from thyroid.
S/E: agranulocytosis, hepatotoxicity, vasculitis, teratogenicity.
Iodide: Inhibit hormone release. Effects occur immediately but
short –lived.
Reserved for hyperthyroid patients for surgery, thyroid storm.
Potassium iodide- 3 drops PO every 8 hrly for 10-14 days.
beta adrenergic antagonists: relieve signs and symptoms of
increased adrenergic activity. Propanolol has the added
feature-inhibit conversion of T4 to T3.
Propranolol 40mg BID or nadolol 160mg once daily; higher dose
may be needed
Nadolol and atenolol have a longer duration than
propranolol.
In emergency, pts. can be prepared for surgery in less than 1
hour by IV administration of esmolol. resting heart rate
should be <85-90bpm.
radioactive iodine and subtotal thyroidectomy: other
alternative to medical therapy.
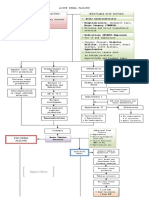
Anesthesia management
Preoperative Assessment
History (hyper/hypo/euthyroidism features, adverse respiratory and CVS
effect due to compression and hormone)
Examination(size, type, retrosternal extension of mass/positive
Pemberton's sign and systemic effect of thyroid hormone)
Investigations including:
Complete Blood Counts
Thyroid Function Tests
Antroposterior or lateral CXR to see retrosternal extension
lateral neck x-ray to see tracheal compression
CT scan
Respiratory function tests
2D ECHO
Preoperative preparation
If elective, patient needs to be rendered euthyroid with drugs
β-blocking drugs- to abolish the clinical manifestation of the
toxic state.
It has very rapid control , operation is possible within a week or
two weeks.
Glucocorticoids –reduce TH release and peripheral conversion of
T4→T3
Iodides started 10-14 days before surgery and proceed until the
day
Lugol’s iodine (for 10 days, 3-5 drops BID) to decrease the
vascularity of the gland.
Benzodiazepine the night before the day of surgery.
Continue antithyroid and B-blockers until the morning of surgery.
Intraoperative management
Allow safe induction and awakening with adequate pain management.
Maintain adequate levels of anaesthesia ( avoid exaggerated sympathetic
response to surgical stimulus).
Barbiturates have antithyroid activity at high doses and is best for
induction
For treatment of hypotension decreased doses of direct-acting
vasopressors such as phenylephrine may be a better choice than
ephedrine, which acts in part by provoking the release of catecholamine.
Avoid:
- Atropine
- Pancuronium
- Halothane
- Ketamine
If hyperthyroid patient with clinically apparent disease
requires emergency surgery :
- Propranolol 0.5mg IV is given ( may be increased ).
- Esmolol (alternative) as a continuous infusion 50-
500mic/kg/min.
- Maintain heart rate below 90bpm.
Use dexametasone 8mg/ hydrocortisone 100 mg to
reduce incidence of airway edema.
Regional anesthesia(SA,EA) may be technique of choice
in hyperthyroid case for non thyroid surgery without
presence of CHF.
Continuous epidural may be preferable to spinal because
of the slower onset of sympathetic nervous system
blockade
Epinephrine should not be added to local anesthetics, as
systemic absorption of this catecholamine could produce
exaggerated circulatory responses
Monitor ECG and patient’s body temperature (for
thyroid storm)
Complications
1. Thyroid Storm :
Acute life threatening exacerbation of hyperthyroidism. Happens intaoperatively or
postoperatively with in 24hr
Manifestations:
Hyperthermia (>40oC)
Tachycardia
CHF
Agitation
Confusion
Dysrhythmias, AF or VT
Severe hypertension
Differential Diagnosis : -
Malignant hyperthermia
Pheochromcytoma
Light anesthesia
Treatment of thyroid storm
PTU 200-400mg PO or via NGT Q6hr.
paracetamal and cold blanket
IV fluids
B-blocker; propranolol 10-40mg PO Q4-6hr /esmolol
infusion until HR<100bpm.
Steroids- hydrocortisone =50-100mg IV -Q6hr
Digoxin for uncontrolled atrial fibrillation and heart failure
Iodide therapy-decrease iodine uptake and thyroid hormone
secretion 250mg PO Or IV Q6hr.
O2 and hemodynamic support
2. Recurrent Laryngeal Nerve (RLN) injury :
-Manifestations of RLN injury:
Unilateral
Asymptomatic unless laryngoscopy done
Bilateral
Usually manifests immediately after extubation.
Laryngeal stridor, acute respiratory distress, vocal cord palsy/adduction,
phonation lost.
Treatment:
Could be temporary or permanent
Re-intubation, paralyzed.
Hydrocortisone 100mg tid.
Wound re-exploration for reversible cause.
If Can not maintain airway do tracheostomy
3. airway obstruction
Vocal cords can collapse together, producing total airway
obstruction during inspiration due to RLN paralysis
If occurs soon after tracheal extubation, despite normal
vocal cord function, suggests tracheomalacia
This reflects a weakening of tracheal rings by chronic
pressure of a goiter
Airway obstruction postoperatively may be due to tracheal
compression by a hematoma
Treatment will be reintubation. If not possible maintain
AirWay with tracheostomy.
4. Hypothyroidism:
Management: TFT on regular bases.
-Thyroxine- 50-200μgm|d.
-10% Cagluconate PO| IV
5 .Hypoparathyroidism & hypocalcaemia:
May be due to:
Trauma to the parathyroid gland,
Devascularization of parathyroid or removal of the gland.
If damage to parathyroid does occur, hypocalcaemia typically
develops 24 to 72 hours postop, but may manifest as early as 1-
3 hours postop
Laryngeal muscles are sensitive to hypocalcaemia. may go
from inspiratory stridor progressing to laryngospasm. Prompt
IV calcium till laryngeal stridor ceases is treatment.
Diagnosis:
Initially asymptomatic
Carpopedal spasm (spasmodic contraction of the muscles of
the hands and feet)
Trousseau’s (carpopedal spasm precipitated by cuff inflation)
Chvostek’s sign (spasm of the facial muscles by tapping the facial
nerve just below the zygomatic bone)
Circumoral paresthesia
Mental status changes
Seizure
QT prolongation or cardiac arrest.
TX:- IV calcium
LARYNGEAL PARALYSIS
ANATOMY OF LARYNX
NERVE SUPPLY OF LARYNX
SENSORY SUPPLY:
Above vocal cords: Internal Laryngeal branch of
superior laryngeal nerve
Below vocal cords: Recurrent laryngeal nerve
MOTOR SUPPLY:
All intrinsic muscles of larynx except cricothyroid
muscle are supplied by recurrent laryngeal nerve
Cricothyroid is supplied by external laryngeal branch
of superior laryngeal nerve.
VOCAL CORD POSITIONS
During respiration, cords are in adduction
During Phonation, cords are in median position
THEORIES ON POSITION OF VOCAL
CORD IN PARALYSIS
SEMON’S LAW: In all progressive organic lesions,
abductor fibres which are phylogenitically newer are
more susceptable and are first to be paralysed.
WAGNER & GROSSMAN HYPOTHESIS: Complete
paralysis of the recurrent laryngeal nerve results in the
vocal cord being in the paramedian position because of
intact cricothyroid muscle, which adducts vocal cord.
When superior laryngeal nerve is also paralysed, the
vocal cord will be in cadaveric position because of loss
of adductive force.
CLASSIFICATION OF LARYNGEAL
PARALYSIS
May be unilateral or bilateral and may involve
1. Recurrent laryngeal nerve
2. Superior laryngeal nerve
3. Both recurrent and superior laryngeal
nerve( combined or complete paralysis)
UNILATERAL RECURRENT
LARYNGEAL NERVE PARALYSIS
Ipsilateral paralysis of CLINICAL
all intrinsic muscles of FEATURES:
larynx except Asymptomatic
cricothyroid change in voice which
Vocol cord assumes a gradually improves by
median or paramedian compensation from the
position and does not other side cord
move laterally on deep TREATMENT:
inspiration
No treatment required
BILATERAL RECURRENT
LARYNGEAL NERVE PARALYSIS
All intrinsic muscles of TREATMENT:
larynx are paralysed In acute stridor,
Vocal cords lie in Tracheostomy is
median or paramedian required
position due to Usually 6 months is an
unopposed action of adequate time to wait
cricothyroid muscles for any spontaneous
CLINICAL recovery
FEATURES: lateralization of vocal
Dysnoea cords can be done
Stridor Type 2 thyroplasty
UNILATERAL SUPERIOR
LARYNGEAL NERVE PARALYSIS
Paralysis of cricothyroid muscle and ipsilateral
anesthesia of larynx above vocal cord
Loss of tension of vocal cord and shortening of vocal
cord
CLINICAL FEATURES:
Weak voice with decreased pitch
Occassional aspiration
TREATMENT:
Medialization laryngoplasty
Modified typr 4 thyroplasty
BILATERAL SUPERIOR LARYNGEAL
NERVE PARALYSIS
Both the cricothyroid muscles are paralysed along with
anaesthesia of upper larynx
CLINICAL FEATURES:
cough
choking fits
weak and husky voice
TREATMENT:
Tracheostomy with a cuffed tube & an oesophageal feeding
tube
Epiglottopexy to close laryngeal inlet to protect lung from
repeated aspirations
COMPLETE UNILATERAL VOCAL
CORD PARALYSIS
Paralysis of all muscles of larynx on one side except
interarytenoid which also receives innervation from opposite
side. Cadaveric position of vocal cord.
CLINICAL FEATURES:
Vocal cord lies in cadaveric position
hoarseness of voice
Aspiration
TREATMENT:
Speech therapy
Medialisation of vocal cord: Thyroplasty type 1, injection of
teflon paste
BILATERAL COMPLETE VOCAL
CORD PARALYSIS
Both cords lie in cadaveric position
Total anesthesia of larynx
CLINICAL FEATURES:
Aphonia
Aspiration, Inability to cough and Bronchopneumonia
TREATMENT:
Tracheostomy
Epiglottopexy
Total laryngectomy
HYPOTHYROIDISM
Hypothyroidism is a condition when the body tissues
are exposed to decreased circulating concentration of
thyroid hormones .
SYMPTOMS SIGNS
Dry coarse skin; cool peripheral
Tiredness, weakness extremities
Dry skin Puffy face, hands, and feet
Cold intolerance (myxoedema)
Diffuse alopecia
Hair loss
Bradycardia
Difficulty concentrating, poor
Carpal tunnel syndrome
memory
Serious cavity effusions
Constipation
Myocardial ischemia or dysrhythmia
Weight gain with poor appetite
Decreased function of respiratory center.
Dyspnea and hoarse voice Decreased cortisol production,
Menorrhagia inappropriate production of ADH
Impaired hearing Hyponatrmeia and Peripheral edema
Elevated TSH/ less T3/ both
Treatment
Patients with severe hypothyroidism, older patients and
patients with CVS disease may have increased sensitivity to
thyroid hormones.
Therefore, they should be given a small dose of thyroid
hormone initially-25μgm of L thyroxin which is gradually
increased every 2 to 4 weeks ,to a full maintenance dose
during 6-12 wks period .
Younger patients and patients with less severe
hypothyroidism maybe started on slightly higher dose
(50μgm of Lthyroxin) and advanced to a full replacement
dose more quickly
Most pts require 75-100μgm of L_thyroxin daily.
Myxedema
Severe form of hypothyroidism characterized by:-
stupor,
coma,
hypoventilation,
hypothermia,
hypotension and hyponateremia.
Medical emergency with mortality rate of 25-50%.
Sepsis in elderly or exposure to cold may be an initiating event
Management
Intubation and ventilation as needed.
Sodium Levothyroxine: 200-300μgm IV over 10min initially and maintenance
200mg|day IV.
Hydrocortisone -100mg IV ,then 25mg IV Q6hr.
Fluid and electrolyte supplementation
Avoid hypothermia
Anesthesia management
Preoperative Medication:
In uncorrected severe hypothyroidism or myxedema coma
postpone elective surgeries and should be treated with IV
T3 supplementation for emergency surgery
Mild to moderate hypothyroidism may not be absolute
contraindication for urgent surgeries.
Due to its depressant effect- avoid opioids
Cortisol supplementation and aspiration prophylaxis may
be considered
Continue thyroid hormone therapy until morning of
surgery.
Induction of Anesthesia:
Ketamine is preferable drug
If no excessive CVS depression etomidate or thiopental can be used.
During calculating dose of relaxants keep in mind that the coexisting
skeletal muscle weakness.
Maintenance of Anaesthesia:
N2O and supplemental short acting opioids, BZD or Ketamine is best.
Volatiles contraindicated in overtly hypothyroid situation.
Hypothyroidism does not appear to decrease MAC but decrease in CO
speeds rate of induction by inhalational because CMRO2 is
independent of thyroid function.
Reduce MAC if body temperature is <37oC.
Pancronium is best relaxant.
No special consideration about reversals.
IV fluids should contain sodium.
Delay extubation until patient respond appropriately with
accepted body temperature.
postoperatively:
Prolonged postoperative somnolence & inability to wean
earlier, so needs mechanical support.
Avoid postoperative hypothermia & give adequate analgesic.
If patient comes for other surgery having hypothyroidism
Regional Anesthesia is best than GA
THYROID SURGERY UNDER REGIONAL
ANAESTHESIA- CERVICAL PLEXUS BLOCK
DEEP CERVICAL PLEXUS
Patient in supine position, with the head
tilted slightly backward and turned
about 45 degrees to the opposite side
A line drawn from caudal tip of mastoid
to chassaignac’s tubercle(transverse
process of C6) along posterior border
of sternomastoid.
Transverse process of c2, 1.5 cm caudal
mastoid process and 1cm dorsal to line
drawn identified and marked
The transverse processes of
C3,C4,C5 are also palpated and
marked. Distance between each of
them is 1.5 cm
The aim is to block anterior branches
of cervical plexus in the groove of the
transverse process.
The needle is advanced perpendicular
to the skin, medially and slightly
caudally.
After clear bone contact, minimal
withdrawal of the needle, careful
aspiration is done before delivering
drug
SUPERFICIAL
CERVICAL PLEXUS:
The subcutaneous
tissues were infiltrated
in a fan like fashion in
the line of the posterior
border of
sternocleidomastoid
muscle in and around
its midpoint
DOSAGE:
30 ml of 0.75% ropivacaine or 0.25%-0.5% bupivacaine
Of this 10ml for superficial cervical plexus block and
20ml for anesthesia of deep cervical plexus. About 3 to
3.5 ml at each insertion point
THANK YOU
You might also like
- Anesthetic Consideration in Thyroid SurgeryDocument36 pagesAnesthetic Consideration in Thyroid Surgerymaulina13No ratings yet
- A CASE OF MULTINODULAR GOITREDocument27 pagesA CASE OF MULTINODULAR GOITREcnsatish86% (7)
- Anaesthesia and Thyroid DiseaseDocument9 pagesAnaesthesia and Thyroid DiseasedrrksNo ratings yet
- Thyroiddisorders PDFDocument51 pagesThyroiddisorders PDFIslam ShoukryNo ratings yet
- Hypothyroidism, Hyperthyroidism, Thyroid Nodules, and CancerDocument77 pagesHypothyroidism, Hyperthyroidism, Thyroid Nodules, and CancerDann San AntonioNo ratings yet
- Thyroid Lumps11Document15 pagesThyroid Lumps11Tareq SawanNo ratings yet
- Hyperthyroidism 1Document88 pagesHyperthyroidism 1Mamikie Vukeya100% (1)
- DR Ananta Thyroid SlideDocument73 pagesDR Ananta Thyroid SlideRoshan Kumar PanditNo ratings yet
- THYROID LECTURE DR OCAMPO (1) (Autosaved)Document106 pagesTHYROID LECTURE DR OCAMPO (1) (Autosaved)SamNo ratings yet
- Thyroid Storm and Hyperthyroidism - CorePendiumDocument17 pagesThyroid Storm and Hyperthyroidism - CorePendiumSajeewanieNo ratings yet
- Thyroid Gland: Anatomy, Physiology and Disease ManagementDocument127 pagesThyroid Gland: Anatomy, Physiology and Disease ManagementCarla Mae MoraNo ratings yet
- AANA Journal Course: Anesthesia Case Management For ThyroidectomyDocument10 pagesAANA Journal Course: Anesthesia Case Management For ThyroidectomyEzie RiveraNo ratings yet
- Anaesthesia For Thyroid Surgery....Document46 pagesAnaesthesia For Thyroid Surgery....Parvathy R NairNo ratings yet
- Anesthesia management for thyroid surgeryDocument60 pagesAnesthesia management for thyroid surgeryyeabsraNo ratings yet
- Specific Disorders of The Thyroid GlandDocument8 pagesSpecific Disorders of The Thyroid Glandgiselle chloeNo ratings yet
- Thyroid Disease Anesthetic ConsiderationsDocument30 pagesThyroid Disease Anesthetic Considerationssachin10dulkarNo ratings yet
- Thyroid Gland Functions and Disorders ExplainedDocument35 pagesThyroid Gland Functions and Disorders ExplainedEdwin OkonNo ratings yet
- Bahir Dar UniversityDocument23 pagesBahir Dar UniversityĎĵ Žě ĤőpėNo ratings yet
- Hyperthyoidism: Anaesthetic ManagementDocument11 pagesHyperthyoidism: Anaesthetic ManagementerzaraptorNo ratings yet
- Hyperthyroid and HypothyroidDocument61 pagesHyperthyroid and HypothyroidSonia Afika AzizaNo ratings yet
- Pharmacotherapy - Thyroid Disorder PDFDocument63 pagesPharmacotherapy - Thyroid Disorder PDFnadiah100% (3)
- Disorders of The Thyroid and Parathyroid Glands: Ms TeamDocument36 pagesDisorders of The Thyroid and Parathyroid Glands: Ms TeamShy Dela PuertaNo ratings yet
- Lect 5Document26 pagesLect 5eslambasuony98No ratings yet
- Askep GGN ThyroidDocument26 pagesAskep GGN ThyroidTsaalits MuharrorohNo ratings yet
- Hyperthyroid 170715182805Document71 pagesHyperthyroid 170715182805Suryati HusinNo ratings yet
- Diseases of The Thyroid Gland PDFDocument72 pagesDiseases of The Thyroid Gland PDFKay BristolNo ratings yet
- ThyroiditisDocument47 pagesThyroiditisaryanmetkarnewNo ratings yet
- Thyroid DisordersNewDocument47 pagesThyroid DisordersNewTri Octavia SitorusNo ratings yet
- Thyroid DiseasesDocument44 pagesThyroid DiseasesPLDT HOMENo ratings yet
- Thyroid ReportDocument105 pagesThyroid ReportAARVNo ratings yet
- Hyperthyroidism 2011Document30 pagesHyperthyroidism 2011Elyza MagsaysayNo ratings yet
- Assessment and Management of Patients With Endocrine DisordersDocument46 pagesAssessment and Management of Patients With Endocrine Disordersamal100% (1)
- ENDOCRINE AND METABOLISM SYSTEM MODUL I: WEIGHT LOSS CASEDocument28 pagesENDOCRINE AND METABOLISM SYSTEM MODUL I: WEIGHT LOSS CASEsakelengelNo ratings yet
- Thyroid StormDocument16 pagesThyroid StormRaquid MariaNo ratings yet
- Thyroid CrisisDocument34 pagesThyroid CrisisRidyah Ning TyasNo ratings yet
- Hypothalamus-Pituitary-Thyroid Axis: PRESENTERS: DR: Nyangaresi Justine DR: Mitchelle Facilitator: DRDocument31 pagesHypothalamus-Pituitary-Thyroid Axis: PRESENTERS: DR: Nyangaresi Justine DR: Mitchelle Facilitator: DRJustine NyangaresiNo ratings yet
- LO&WO - Endokrin.week4 (Michael G)Document6 pagesLO&WO - Endokrin.week4 (Michael G)Michael GNo ratings yet
- Mbs127 Slide Hyperthyroidism 1Document46 pagesMbs127 Slide Hyperthyroidism 1revita262No ratings yet
- Neck Diseases: Affiliated Hospital Of Jining Medical Colledge Dep.Mammary And Thyroid Surgery Zhu Kunbing 朱坤兵Document61 pagesNeck Diseases: Affiliated Hospital Of Jining Medical Colledge Dep.Mammary And Thyroid Surgery Zhu Kunbing 朱坤兵sanjivdasNo ratings yet
- HYper and Hypo TGDocument43 pagesHYper and Hypo TGRiajoy AsisNo ratings yet
- Thyrotoxicosis & Hypothyroidism by Prof DR NK ChopraDocument52 pagesThyrotoxicosis & Hypothyroidism by Prof DR NK ChopraAbdulsalam DostNo ratings yet
- Thyroid DisorderDocument60 pagesThyroid DisorderThe AbyssinicansNo ratings yet
- Radioactive Iodine Therapy (RAI) for HyperthyroidismDocument6 pagesRadioactive Iodine Therapy (RAI) for HyperthyroidismFirras SalsabilaNo ratings yet
- Bening Disease of Thyroid GlandDocument85 pagesBening Disease of Thyroid GlandKarishma MishraNo ratings yet
- Bahan Tyroid (PA)Document75 pagesBahan Tyroid (PA)Raja FadhilNo ratings yet
- Thyroid StormDocument36 pagesThyroid StormSabrina ShalhoutNo ratings yet
- THYROID DISORDERS GUIDEDocument33 pagesTHYROID DISORDERS GUIDEJanine Dela CruzNo ratings yet
- Thyroid Disease in PregnancyDocument3 pagesThyroid Disease in PregnancyjayinthelongrunNo ratings yet
- Thyro I EctomyDocument9 pagesThyro I EctomySafwan SayedNo ratings yet
- Thyroid Gland DisordersDocument64 pagesThyroid Gland DisordersFaisal RavifNo ratings yet
- Lecture Thyroid GlandDocument54 pagesLecture Thyroid GlandMarinaNo ratings yet
- Thyroid Disease: Dr. Gusti Hariyadi Maulana, MSC, SPPD-KGH Internist-NephrologistDocument30 pagesThyroid Disease: Dr. Gusti Hariyadi Maulana, MSC, SPPD-KGH Internist-NephrologistNurul HikmaNo ratings yet
- Morning ReportDocument31 pagesMorning Reports1882No ratings yet
- MyxedemaDocument3 pagesMyxedemaBobet ReñaNo ratings yet
- SC2 2015 HyperthyroidismDocument38 pagesSC2 2015 HyperthyroidismShafern TanNo ratings yet
- Thyroid Disease GuideDocument65 pagesThyroid Disease GuideIan FordeNo ratings yet
- Therapeutics: Thyroid DisordersDocument24 pagesTherapeutics: Thyroid DisordersSharas FarhadNo ratings yet
- Endocrinology Notes for Medical StudentsFrom EverandEndocrinology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (1)
- MusaedAlsayadi (GynaecologmcqsDr. Farouk Haseeb)Document65 pagesMusaedAlsayadi (GynaecologmcqsDr. Farouk Haseeb)a7332773No ratings yet
- Steroids HormonesDocument15 pagesSteroids HormonesZain Ul Abdin Mughal100% (1)
- Commonly Used Lab Values at A Glance Chem 7 1Document9 pagesCommonly Used Lab Values at A Glance Chem 7 1annatw100% (10)
- Cover Letter DDocument1 pageCover Letter DDebela NanessoNo ratings yet
- Embryology (3) Development of The Male Reproductive OrgansDocument13 pagesEmbryology (3) Development of The Male Reproductive OrgansNazmul Hossain TayonNo ratings yet
- 30-20-DX-489-76 Atellica Menu US FINALDocument2 pages30-20-DX-489-76 Atellica Menu US FINALoctavio omar villegasNo ratings yet
- DM 1 ManagementDocument11 pagesDM 1 ManagementsamNo ratings yet
- 1068 5615 2 PBDocument8 pages1068 5615 2 PBVicky AndriNo ratings yet
- Pathophysiology of Bipolar DisorderDocument1 pagePathophysiology of Bipolar DisorderbeshyNo ratings yet
- 1) The Amount of Plasma Proteins ( P.P.) Is Near ToDocument35 pages1) The Amount of Plasma Proteins ( P.P.) Is Near TobmhshNo ratings yet
- Ch.12 Getting the measure of hormones講義Document7 pagesCh.12 Getting the measure of hormones講義邱小瀧No ratings yet
- Introduction To Hematology-1Document44 pagesIntroduction To Hematology-1Sri DurgaNo ratings yet
- Turners Syndrome: Sonika Shimon Prasad S160232Document20 pagesTurners Syndrome: Sonika Shimon Prasad S160232Ivy DanNo ratings yet
- 08 Chemical MessengersDocument29 pages08 Chemical MessengersMelody GarciaNo ratings yet
- Healing Codes: Grigori GrabovoiDocument47 pagesHealing Codes: Grigori GrabovoiPanther MelchizedekNo ratings yet
- Pathophysiology of Acute Renal FailureDocument2 pagesPathophysiology of Acute Renal Failureminangsung minangnengNo ratings yet
- Essentials of Human PhysiologyDocument552 pagesEssentials of Human PhysiologyTapan Kumar Pal100% (4)
- Case Analysis 4 GERDDocument12 pagesCase Analysis 4 GERDCJ100% (1)
- BCCS03 Ref. 1002100 Spintrol B N Lot. 1827NDocument2 pagesBCCS03 Ref. 1002100 Spintrol B N Lot. 1827Namor kermayaNo ratings yet
- What's A Normal Menstrual PeriodDocument3 pagesWhat's A Normal Menstrual Periodpankaj kararNo ratings yet
- DrugsDocument20 pagesDrugsLee Won100% (1)
- 14 - Lipid Lowering DrugsDocument19 pages14 - Lipid Lowering DrugsAttekah MohammedNo ratings yet
- Effect of Cocoyam Colocasia Esculenta Unripe Plantain Musa Paradisiaca or Their Combination On Glycated Hemoglobin Lipogenic Enzymes and LipidDocument8 pagesEffect of Cocoyam Colocasia Esculenta Unripe Plantain Musa Paradisiaca or Their Combination On Glycated Hemoglobin Lipogenic Enzymes and LipidGoummeli6 SocratesNo ratings yet
- Calcium and Phosphate Hormones: Vitamin D, Parathyroid Hormone, and Fibroblast Growth Factor 23Document11 pagesCalcium and Phosphate Hormones: Vitamin D, Parathyroid Hormone, and Fibroblast Growth Factor 23Handyka Vb GNo ratings yet
- Download ebook Endocrine Secrets Pdf full chapter pdfDocument67 pagesDownload ebook Endocrine Secrets Pdf full chapter pdfjason.green261100% (23)
- SUBICART-GC - PLUS SruthiDocument2 pagesSUBICART-GC - PLUS Sruthiari aranNo ratings yet
- DLL g7 Health Eating DisordersDocument4 pagesDLL g7 Health Eating DisordersivonneNo ratings yet
- Analisis Hematologi Monyet Ekor PanjangDocument148 pagesAnalisis Hematologi Monyet Ekor PanjangIrfan Rian SaputraNo ratings yet
- Alopecia Areata PresentationDocument12 pagesAlopecia Areata Presentationpcjoy2100% (1)
- Drug Tests User Guide NEWDocument16 pagesDrug Tests User Guide NEWzxcv1ingrNo ratings yet