100% found this document useful (2 votes)
720 views17 pagesEssential Guide to Intubation Techniques
Intubation involves inserting an endotracheal tube through the mouth or nose into the trachea to maintain an open airway. It is used to provide oxygen, anesthesia, or medication when a patient is experiencing respiratory distress that cannot be treated with less invasive methods. There are different types of intubation based on the tube location and purpose, such as endotracheal intubation through the mouth into the trachea, which is the most common type. Intubation requires specialized training and equipment to properly place and secure the tube. Nurses monitor patients after intubation to ensure proper tube placement and provide care to prevent complications.
Uploaded by
Joan SinghCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
100% found this document useful (2 votes)
720 views17 pagesEssential Guide to Intubation Techniques
Intubation involves inserting an endotracheal tube through the mouth or nose into the trachea to maintain an open airway. It is used to provide oxygen, anesthesia, or medication when a patient is experiencing respiratory distress that cannot be treated with less invasive methods. There are different types of intubation based on the tube location and purpose, such as endotracheal intubation through the mouth into the trachea, which is the most common type. Intubation requires specialized training and equipment to properly place and secure the tube. Nurses monitor patients after intubation to ensure proper tube placement and provide care to prevent complications.
Uploaded by
Joan SinghCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
- Introduction to Intubation: Provides a comprehensive introduction to intubation, highlighting its necessity in emergency care to secure an airway.
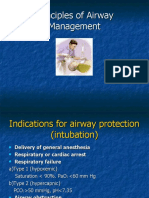
- Purposes of Intubation: Details the various medical reasons for performing intubation, including opening airways and providing oxygen or anesthesia.
- Instruments for Intubation: Lists and describes the primary tools used in the intubation process, such as the laryngoscope and Ambu bag.
- Endotracheal Tube: Focuses on the characteristics and specifications of an endotracheal tube, including its components like the bevel and cuff.
- Common Types of Intubation: Overview of the various intubation methods including nasogastric and fiber optic along with their specific applications.
- Disadvantages of Intubation: Explores potential complications and drawbacks associated with intubation, highlighting risks and recommendations.
- Nursing Care for Patients with Endotracheal Tube: Provides guidelines for nursing care immediately after intubation, focusing on patient monitoring and care techniques.