Professional Documents
Culture Documents
Ethical Dilemmas
Uploaded by
Deborah Chemutai0 ratings0% found this document useful (0 votes)
11 views19 pagesCopyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views19 pagesEthical Dilemmas
Uploaded by
Deborah ChemutaiCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 19
A situation in which an individual feels compelled to
make a choice between two or more actions that he or
she can reasonably and morally justify, or when
evidence or an arguments are inconclusive, is called
an ethical dilemma (Beauchamp&Childress,2001;McConnell,2002).
One action must be chosen because performing both
actions would be impossible.
Ethical Dilemmas are usually described in terms of
right or wrong, duty or obligation, rights or
responsibilities, and good or bad. Ethical dilemmas
are commonly identified by the question,” What
should be done?”
Most dilemmas can be identified according to the
following classifications:
• Dilemmas of Beneficence-dilemma that involve
deciding what is good as opposed to what its harmful.
• Dilemmas of autonomy- those that involve deciding
what course of action maximize the patient's right of
self determination.
• Dilemmas of justice- dilemmas that involve dividing
limited health care resources fairly
• Dilemmas of fidelity- those that are involve
honoring promises
• Dilemmas of non maleficence- dilemmas that
involve the avoidance of harm
• Dilemmas of confidentiality- those that involve
respecting privileged information
• Dilemmas of veracity- dilemmas that involve
telling or concealing the truth
Growing awareness of ethical problems has occurred
largely because of (a) social and technological
changes and (b) conflicting loyalties and obligations.
Social changes, such as the women’s movement. The
large number of people without health insurance, the
high cost of health care.
Technology creates new issues that did not exist in
earlier times. Before monitors, respirators, and
parenteral feedings, there was no question about
whether to ‘’ allow’’ an 800- gram premature infant
to die.
Before organ transplantation , death did not require a
legal definition that might still permit viable tissues
to be removed and given to other living persons.
Advances in the ability to decode and control the
growth of tissues through gene manipulation present
new potential ethical dilemmas related to cloning
organisms and altering the course of hereditary
disease and biological characteristics. Today, with
treatment that can prolong and enhance biologic life,
these questions arise: should we do what we know we
can?
Health workers experience conflicts among their
loyalties and obligations to clients, families, primary
care providers, employing institutions. Client needs
may conflict with institutional policies, primary care
provider preferences, needs of the client’s family, or
even laws of the state. However, it is not always easy
to determine which action best serves the client’s
needs.
Responsible ethical reasoning is rational and
systematic. It should be based on ethical principles
and codes rather than on emotions, intuition, fixed
policies, or precedent that is, an earlier similar
occurrence).
Two decision – making models
1- Thompson and Thompson (1985)
Review the situation to determine health problems,
decision needs, ethical components, and key
individuals.
Gather additional information to clarify the situation
Identify the ethical issues in the situation.
Define personal and professional moral positions.
Identify moral positions of key individuals involved
Identify value conflicts, if any
Determine who should make the decision
Identify range of actions with anticipated outcomes.
Decide on a course of action and carry it out.
Evaluate / review results of decision / action.
2- Cassells and Redman (1989)
Identify the moral aspects of care
Gather relevant facts related to a moral issue.
Clarify and apply personal values
Understand ethical theories and principles
Utilize competent interdisciplinary resources
Propose alternative actions.
Apply codes of ethics to help guide actions
Choose and implement resolutive action.
Participate actively in resolving the issue
Apply state and federal laws governing practice.
Evaluate the resolutive action taken
A good decision is one that is in the client’s best
interest and at the same time preserves the integrity
of all involved. Health workers have ethical
obligations to their clients, to the agency that
employs them, and to primary care providers.
Therefore, midwives must weigh competing factors
when making ethical decisions.
Maximize the client’s well – being
Balance the client’s need for autonomy with family
member’s responsibilities for the client’s well – being
Support each family member and enhance the
family support system.
Carry out hospital policies.
Protect other client’s well – being
Protect the standards of care.
The health professional may feel torn between
obligations to the client, the family, and the
employer. What is in the client’s best interest may be
contrary to the health professional personal belief
system. In settings in which ethical issues arise
frequently, doctors should establish support systems
such as team conferences and use of counseling
professionals to allow expression of their feelings.
Active decisions-ethical decisions and moral
judgments that lead directly to actions and bring
about changes
Passive decisions- decisions that deny , delay, or
avoid action and maintain the status quo by denying
or shifting responsibility to avoid changes
• Programmed decisions- decisions that use precedents,
established guidelines, procedures, and rules to resolve
anticipated, routine, expected types of moral dilemmas
• Non-programmed decisions- decisions that require a unique
response to complex and unexpected moral dilemmas.
Process for resolving ethical problems:
recognition of ethical dilemma
Gathering relevant factual information
Clarify the personal context of the ethical dilemma
Identify and clarify the ethical concept
Construct and evaluate arguments for each issue.
Take action. (Make decision)
Ethical decision making is a skill that can be learned,
based on understanding of underlying ethical
principles, ethical theories or systems, a decision
making model, and the ICM of Ethics.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ART 14 OutlineDocument15 pagesART 14 Outlinesan_leonoraNo ratings yet
- Egyptian Zodiac SignsDocument4 pagesEgyptian Zodiac SignslordsifmorNo ratings yet
- Bahasa Inggris Fakultas Hukum Semester 1Document54 pagesBahasa Inggris Fakultas Hukum Semester 1Pandji Purnawarman83% (6)
- TAMP BriefingDocument17 pagesTAMP Briefingdragon 999999100% (1)
- 178 - 6 - Fun For Flyers On-Line Resources - 2017, 4th - 241pDocument241 pages178 - 6 - Fun For Flyers On-Line Resources - 2017, 4th - 241pNguyen HuyenNo ratings yet
- Drank SauceDocument1 pageDrank SauceUnikkatil FORCENo ratings yet
- A Collection of Facsimiles From Examples of Historic or Artistic Book-Binding, Illustrating The History of Binding As A Branch of The Decorative Arts - GettyDocument252 pagesA Collection of Facsimiles From Examples of Historic or Artistic Book-Binding, Illustrating The History of Binding As A Branch of The Decorative Arts - GettyRic So100% (1)
- FM 415 - Quiz #1Document4 pagesFM 415 - Quiz #1Rose Gwenn VillanuevaNo ratings yet
- Youth Ministry Handbook 06 PDFDocument301 pagesYouth Ministry Handbook 06 PDFDaphneNo ratings yet
- DKA Uganda August 2023Document35 pagesDKA Uganda August 2023Deborah ChemutaiNo ratings yet
- FUMSA GA Concept Draft JONATHANDocument7 pagesFUMSA GA Concept Draft JONATHANDeborah ChemutaiNo ratings yet
- Year 3 Courses - Semester I & 2 - MBCHBDocument14 pagesYear 3 Courses - Semester I & 2 - MBCHBDeborah ChemutaiNo ratings yet
- First Aid Training Wagagai Company 2011Document153 pagesFirst Aid Training Wagagai Company 2011Deborah ChemutaiNo ratings yet
- Doctor Patient Relationship Muk March 2021Document28 pagesDoctor Patient Relationship Muk March 2021Deborah Chemutai100% (1)
- Gene Expression - May 7 2021 MakCHS (Compatibility Mode)Document20 pagesGene Expression - May 7 2021 MakCHS (Compatibility Mode)Deborah ChemutaiNo ratings yet
- Year 1 Semester 1 - 2021 Timetable Final VersionDocument12 pagesYear 1 Semester 1 - 2021 Timetable Final VersionDeborah ChemutaiNo ratings yet
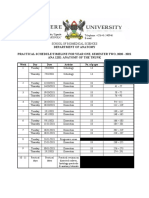
- Practical Timeline SEM II TRUNK-0Document1 pagePractical Timeline SEM II TRUNK-0Deborah ChemutaiNo ratings yet
- Exam 4KEY - 2016Document13 pagesExam 4KEY - 2016Deborah ChemutaiNo ratings yet
- District: Palisa District: S/N School Specific Findings RecommendationsDocument2 pagesDistrict: Palisa District: S/N School Specific Findings RecommendationsDeborah ChemutaiNo ratings yet
- 35148753Document134 pages35148753Deborah ChemutaiNo ratings yet
- Transcription Is A Cellular Process During Which RNA Is SynthesizedDocument7 pagesTranscription Is A Cellular Process During Which RNA Is SynthesizedDeborah ChemutaiNo ratings yet
- accenture案例研究Document7 pagesaccenture案例研究ubcaaufngNo ratings yet
- AnghieDocument106 pagesAnghieArchishaNo ratings yet
- Bachelor of Arts (A.B.) Major in Legal Management Subjectcode Description Units First Year / First SemesterDocument2 pagesBachelor of Arts (A.B.) Major in Legal Management Subjectcode Description Units First Year / First SemesterJunmark CarbonelNo ratings yet
- Invoice 4383450Document1 pageInvoice 4383450Rachit GoyalNo ratings yet
- Form C3.1 Single Work Permit Change in Employer Application For Recruiting Temping AgentsDocument5 pagesForm C3.1 Single Work Permit Change in Employer Application For Recruiting Temping AgentsPG Venkatesh YadavNo ratings yet
- Preparing Adjusting EntriesDocument6 pagesPreparing Adjusting EntriesRey ArellanoNo ratings yet
- Sidang Ilahi Elohim Dalam Mazmur 82:1: Marthin Steven Lumingkewas & Firman PanjaitanDocument25 pagesSidang Ilahi Elohim Dalam Mazmur 82:1: Marthin Steven Lumingkewas & Firman PanjaitanDoni MarpaungNo ratings yet
- Flat FileDocument1 pageFlat FileEr Sundeep RachakondaNo ratings yet
- Modal Verbs: Bill Likes To Show Off. Form Sentences Using The Present PerfectDocument2 pagesModal Verbs: Bill Likes To Show Off. Form Sentences Using The Present PerfectEvaNo ratings yet
- Economics DifferencesDocument5 pagesEconomics DifferencesAyappaNo ratings yet
- The Hindu - Education - Careers - Study Plan For UPSCDocument2 pagesThe Hindu - Education - Careers - Study Plan For UPSCbrijesh113No ratings yet
- Kahama CVDocument3 pagesKahama CVpcfan church100% (2)
- The Little Match Girl Short StoryDocument2 pagesThe Little Match Girl Short StoryTin AcidreNo ratings yet
- PPM Executive Development Program 2021Document12 pagesPPM Executive Development Program 2021ahadiyat jayaNo ratings yet
- Invoice 23001479Document1 pageInvoice 23001479Laxman AdhikariNo ratings yet
- "It's Still The Customer First": Kush Shah, ChairmanDocument28 pages"It's Still The Customer First": Kush Shah, ChairmanAnurag SrivastavaNo ratings yet
- Pres en Tors CourtDocument6 pagesPres en Tors CourtJess BrighamNo ratings yet
- Lay Dominicans Inquirers Pamphlet - Downloadable Color-1Document8 pagesLay Dominicans Inquirers Pamphlet - Downloadable Color-1Enrico CorellaNo ratings yet
- Simex Entry of Illegal Items May 26, 2022Document3 pagesSimex Entry of Illegal Items May 26, 2022Maritime Pulis Gensan MarprstaNo ratings yet
- From Tasting To DigestDocument7 pagesFrom Tasting To Digestlalitarani_05No ratings yet
- Walk Bridges - Raffles PlaceDocument10 pagesWalk Bridges - Raffles PlaceSovereignAdNo ratings yet