Professional Documents
Culture Documents
Antihypertensives Lect
Uploaded by
Rachna0 ratings0% found this document useful (0 votes)
6 views82 pagesPharmacology Lecture which is based on antihypertensive drugs, it contains the drug mechanisms as well
Original Title
ANTIHYPERTENSIVES LECT
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPharmacology Lecture which is based on antihypertensive drugs, it contains the drug mechanisms as well
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views82 pagesAntihypertensives Lect
Uploaded by
RachnaPharmacology Lecture which is based on antihypertensive drugs, it contains the drug mechanisms as well
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 82
HYPERTENSION
Hypertension
mmHg 140 > mmHg 90 >
****************************************************
Systolic Blood Diastolic Blood
Pressure (SBP) Pressure (DBP)
Types of
Hypertension
Essential Secondary
A disorder of unknown origin affecting the
Secondary to other disease processes
Blood Pressure regulating mechanisms
****************************************************
Environmental
Factors
Stress Na+ Intake Obesity Smoking
Risk factors: Hypertension: 7 classification
1. Age above 55 in Men and 65 in Woman
2. Family History
3. Smoking
4. Diabetes and Dyslipidemia
5. Hypertension
6. Obesity
7. Microalbuminuria
Treatment of Hypertension –
6 compelling Indications:
Heart failure
Coronary artery disease
H/o MI
H/o stroke
Diabetes
Chronic Renal failure
Treatment – Why?
Symptomatic treatment is Mandatory:
Reduce premature cardiovascular morbidity and
mortality and microvascular disease affecting the
brain, kidney and retina.
Hypertension, even asymptomatic needs treatment
major risk factor for stroke, heart failure, renal
disease, peripheral vascular disease, and coronary
artery disease.
Factors inducing HTN include decreased vagal tone,
increased sympathetic tone, increased renin-
angiotensin activity, and excess water retention.
MECHANISMS FOR CONTROLLING B.P
BP = CO x TPR
Cardiac output and peripheral resistance, are
controlled mainly by two overlapping control
mechanisms:
the baroreflexes and
the renin–angiotensin–aldosterone system
√ Most antihypertensive drugs lower blood pressure by
reducing cardiac output and/or decreasing peripheral
resistance
1. Baroreceptors and the sympathetic
nervous system
A fall in blood pressure causes pressure-sensitive
neurons (baroreceptors in the aortic arch and
carotid sinuses) to send fewer impulses to
cardiovascular centers in the spinal cord.
This prompts a reflex response of increased
sympathetic and decreased parasympathetic
output to the heart and vasculature, resulting in
vasoconstriction and increased cardiac output.
These changes result in a compensatory rise in
blood pressure
2. Renin–angiotensin–aldosterone system
Baroreceptors in the kidney respond to reduced arterial
pressure (and to sympathetic stimulation of β1 adrenoceptors)
by releasing the enzyme renin.
Renin converts angiotensinogen to angiotensin I, which is
converted in turn to angiotensin II, in the presence of
angiotensin-converting enzyme (ACE).
Angiotensin II is a potent circulating vasoconstrictor,
constricting both arterioles and veins, resulting in ↑ B.P.
Angiotensin II exerts a preferential vasoconstrictor action on
the efferent arterioles of the renal glomerulus, increasing GFR.
Stimulation of angiotensin II type 1 (AT1) receptors leads to
aldosterone secretion, leading to increased renal sodium
reabsorption and increased blood volume, which contribute to
a further increase in blood pressure.
Pharmacotherapy
Non-drug treatment (Life-style changes)
salt intake (2.5g/d --* 1 g/d)
calorie intake, weight loss
alcohol consumption
physical activity
stress factors
stop smoking,
caffeine intake
2020 International Society of Hypertension Global
Hypertension Practice Guidelines
Pharmacotherapy
Goal of treating hypertension is a systolic B.P < 140 mm
Hg and a diastolic B.P of < 90 mm Hg.
Mild hypertension monotherapy, but most patients
require more than one drug to achieve B.P control.
Recommendation: initiate therapy with a thiazide
diuretic, ACEI, ARB, or calcium channel blocker.
Uncontrolled B.P a second drug should be added,
with the selection based on minimizing the adverse
effects of the combined regimen and achieving goal
blood pressure.
Patients with systolic B.P >160 mm Hg or diastolic B.P
>100 mm Hg should be started on two antihypertensives
simultaneously.
For patients with diabetes, goal B.P = < 140/80 mm Hg.
In patients with chronic kidney disease and
proteinuria, lower goals of < 130/80 mm Hg may be
considered.
Elderly patients less than 150/90 mm Hg.
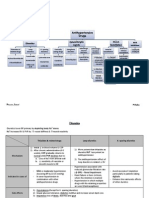
Summary of antihypertensive drugs.
Drugs which lower blood pressure act through three
General Mechanisms:
1. Alter sympathetic activity
2. Relax vascular smooth muscle
3. Alter sodium and water balance
• Treatments for HTN aim to reduce sympathetic tone and
blood volume and/or relax vascular smooth muscle.
Antihypertensive Drugs
Diuretics:
Thiazides: Hydrochlorothiazide, chlorthalidone
High ceiling: Furosemide
K+ sparing: Spironolactone, triamterene and amiloride
MOA: Acts on Kidneys to increase excretion of Na and H2O –
decrease in blood volume – decreased BP
Angiotensin-converting Enzyme (ACE) inhibitors:
Captopril, lisinopril, enalapril, ramipril and fosinopril
MOA: Inhibit synthesis of Angiotensin II – decrease in
peripheral resistance and blood volume
Angiotensin (AII) blockers:
Losartan, candesartan, valsartan and telmisartan
MOA: Blocks binding of Angiotensin II to its receptors
Antihypertensive Drugs
Centrally acting:
Clonidine, methyldopa
MOA: Act on central α2A receptors to decrease sympathetic outflow –
fall in BP
ß-adrenergic blockers:
Non selective: Propranolol (others: nadolol, timolol, pindolol,
labetolol)
Cardioselective: Metoprolol (others: atenolol, esmolol,
betaxolol)
MOA: Bind to beta adrenergic receptors and blocks the activity
ß and α – adrenergic blockers:
Labetolol and carvedilol
α – adrenergic blockers:
Prazosin, terazosin, doxazosin, phenoxybenzamine and
phentolamine
MOA: Blocking of alpha adrenergic receptors in smooth muscles -
vasodilatation
Antihypertensive Drugs
Calcium Channel Blockers (CCB):
Verapamil, diltiazem, nifedipine, felodipine,
amlodipine, nimodipine etc.
MOA: Blocks influx of Ca++ in smooth muscle cells
– relaxation of SMCs – decrease BP
K+ Channel activators:
Diazoxide, minoxidil, and nicorandil
MOA: Leaking of K+ due to opening – hyper
polarization of SMCs – relaxation of SMCs
Vasodilators:
Arteriolar – Hydralazine (also CCBs and K+
channel activators)
Arterio-venular: Sodium Nitroprusside
Angiotensin Converting Enzyme (ACE)
Inhibitors
What is Renin – Angiotensin-
Aldosterone System (RAAS)?
(Physiological Background)
RAAS - Introduction
Renin is a proteolytic enzyme and also called
angiotensinogenase
It is produced by juxtaglomerular cells of kidney
It is secreted in response to:
Decrease in arterial blood pressure
Decrease Na+ in macula densa
Increased sympathetic nerve activity
Renin acts on a plasma protein – Angiotensinogen (a
glycoprotein synthesized and secreted into the
bloodstream by the liver) and cleaves to produce a
decapeptide Angiotensin-I
Angiotensin-I is rapidly converted to
Angiotensin-II (octapeptide) by ACE (present in
luminal surface of vascular endothelium)
Angiotensin-II stimulates Aldosterone secretion
from Adrenal Cortex.
RAAS – actions of Angiotensin-II.
1.Powerful vasoconstrictor, particularly arteriolar – direct
action and release of Adr/NA
Promotes movement of fluid from vascular to
extravascular
promotes Na+ and water reabsorption
It increases myocardial force of contraction (CA++ influx
promotion) and increases heart rate by sympathetic
activity, but reflex bradycardia occurs
2.Aldosterone secretion stimulation – retention of Na++ in
body
Angiotensin-II
What are the chronic ill effects ?
Volume overload and increased T.P.R
Cardiac hypertrophy and remodeling
Coronary vascular damage and remodeling
Hypertension – long standing will cause ventricular
hypertrophy
Myocardial infarction – hypertrophy of non-infarcted
area of ventricles
Renal damage
Risk of increased CV related morbidity and mortality
ACE inhibitors reverse cardiac and vascular
hypertrophy and remodeling
ACE inhibitors
Captopril, lisinopril, enalapril, ramipril and
fosinopril etc.
ACE INHIBITORS
Recommended as first-line treatment of HTN in patients
with a variety of compelling indications, including high
coronary disease risk or history of diabetes, stroke, heart
failure, myocardial infarction, or chronic kidney disease
MOA
lower B.P by ↓PVR without reflexively ↑ CO, HR, or
contractility. (ACEI block conversion of AI to AII and inhibit
breakdown of bradykinin)
ACE is responsible for breakdown of bradykinin.
Bradykinin, is a peptide that ↑ production of nitric oxide
and prostacyclin by blood vessels, potent vasodilators
ACEIs block the enzyme ACE (which cleaves angiotensin I to
form the potent vasoconstrictor angiotensin II)
ACE inhibitors decrease angiotensin II and increase
bradykinin levels.
Vasodilation of both arterioles and veins occurs as a
result of decreased vasoconstriction (from
diminished levels of angiotensin II) and enhanced
vasodilation (from increased bradykinin).
By reducing circulating angiotensin II levels, ACE
inhibitors also decrease the secretion of aldosterone,
resulting in decreased sodium and water retention.
ACE inhibitors reduce both cardiac preload and
afterload, thereby decreasing cardiac work.
Therapeutic uses
Diabetic nephropathy Like the ARBs, ACEIs slow the
progression of diabetic nephropathy and ↓ albuminuria.
Beneficial effects on renal function may result from ↓
intraglomerular pressures, due to efferent arteriolar
vasodilation.
ACEIs used post myocardial infarction and first-line agents
in the treatment of patients with systolic dysfunction.
Chronic treatment achieves sustained B.P reduction,
regression of left ventricular hypertrophy, and prevention of
ventricular remodeling after a MI.
1st drugs for tx in HF, hypertensive patients with chronic
kidney disease, and patients at increased risk of CAD.
All equally effective in the tx of HTN at equivalent doses.
Adverse effects
Common: dry cough, rash, fever, altered taste,
hypotension and hyperkalemia.
dry cough( 10% of patients) due to increased levels of
bradykinin and substance P, resolves within a few days
of discontinuation.
Angioedema is a rare, due to ↑ bradykinin.
monitor K levels and use potassium supplements and
potassium-sparing diuretics cautiously.
ACE inhibitors can induce fetal malformations and
should not be used by pregnant women.
Effects of various drug classes on the Renin–Angiotensin–
Aldosterone system.
Blue = drug target enzymes; red = drug class.
ANGIOTENSIN II RECEPTOR BLOCKERS
E.g. Losartan, Irbesartan, are alternatives to the ACEIs.
block the AT1 receptors, decreasing the activation of
AT1 receptors by angiotensin II.
ARBs do not increase bradykinin levels.
Used as first-line agents for the tx of HTN especially in
patients with a compelling indication of diabetes, heart
failure, or chronic kidney disease
AE: similar to those of ACEIs, although the risks of
cough and angioedema are significantly decreased.
These agents are also teratogenic and should not be
used by pregnant women.
BRADYKININ
Vasodilation
and vascular
permeability
Sites of action of drugs that interfere with the RAAS
Thiazide diuretics
MOA: Block Na+/Cl- transporter in renal distal convoluted
tubule and decrease blood volume, which ultimately leads to
decreased blood pressure
used as initial drug therapy for hypertension unless CI.
effective in lowering blood pressure by 10–15 mm Hg.
E.g. Hydrochlorothiazide (HCT), lower B.P by increasing
sodium and water excretion.
This causes a decrease in extracellular volume, resulting in a
decrease in cardiac output and renal blood flow
useful in combo therapy with β-blockers, ACE inhibitors,
ARBs, and potassium-sparing diuretics.
Loop diuretics
MOA: Block Na+/K+/2Cl- transporter in renal loop of Henle.
This site accounts for retention of approx. 20 % of filtered
sodium; therefore these are potent diuretics.
Furosemide, torsemide, bumetanide, and ethacrynic acid
act promptly by inhibiting reabsorption of sodium and
chloride
cause decreased renal vascular resistance and increased
renal blood flow.
unlike thiazides, loop diuretics increase the Ca 2+ content of
urine, whereas thiazide diuretics decrease it.
commonly used to manage symptoms of heart failure and
edema.
Potassium-sparing diuretics
MOA: Inhibit sodium absorption by blocking aldosterone
receptor in renal collecting tubule.
oIncrease Na+ and water excretion and ↓ K+ excretion.
Amiloride and triamterene inhibit sodium reabsorption in
the distal tubule by blocking sodium channels. They
interfere with sodium/potassium exchange and reduce
urinary potassium excretion.
Aldosterone antagonists, e.g Spironolactone, have the
additional benefit of diminishing the cardiac remodelling
that occurs in heart failure
Potassium-sparing diuretics are sometimes used in
combination with loop diuretics and thiazides to reduce the
amount of potassium loss induced by these diuretics
β-ADRENOCEPTOR–BLOCKING AGENTS
MOA: Block β1 receptors reduce blood pressure primarily by
decreasing cardiac output.
Also decrease sympathetic outflow from the CNS and inhibit
the release of renin from the kidneys, thus decreasing the
formation of angiotensin II and the secretion of aldosterone.
Prototype = Propranolol acts at both β1 and β2 receptors.
Selective blockers of β1 receptors Metoprolol and Atenolol
The selective β-blockers may be administered cautiously to
hypertensive patients who also have asthma.
The nonselective β-blockers, such as propranolol, are
contraindicated in patients with asthma due to their blockade of
β2-mediated bronchodilation.
use cautiously in the tx of patients with acute heart failure or
peripheral vascular disease
Beta-blockers Mode of action
Competitively block beta receptors in the
heart, peripheral vasculature, bronchi,
pancreas, uterus, kidney, brain and liver.
Beta-blockers reduce heart rate, BP and
cardiac contractility; also depress sinus node
rate and slow conduction through the AV node,
and prolong atrial refractory periods.
Actions of β-adrenoceptor–blocking agents.
Therapeutic uses
in hypertensive patients with concomitant heart
disease, such as supraventricular tachyarrhythmia (for
example, atrial fibrillation), previous myocardial
infarction, angina pectoris, and chronic heart failure.
Pharmacokinetics
Propranolol undergoes extensive and highly variable
first-pass metabolism.
Oral β-blockers may take several weeks to develop
their full effects.
Esmolol, metoprolol, and propranolol are available in
intravenous formulations.
Adverse effects
Common: Nausea, diarrhoea, bronchospasm, cold
extremities, may cause bradycardia, hypotension, and CNS
side effects such as fatigue, lethargy, and insomnia.
may decrease libido and cause erectile dysfunction,
which can severely reduce patient compliance.
Alterations in serum lipid patterns: Non cardioselective
β-blockers disturb lipid metabolism, decreasing high-
density lipoprotein cholesterol and increasing triglycerides.
Drug withdrawal: Abrupt withdrawal may induce angina,
myocardial infarction, and even sudden death in patients
with ischemic heart disease. Therefore, these drugs must
be tapered over a few weeks in patients with hypertension
and ischemic heart disease.
α-/β-ADRENOCEPTOR–BLOCKING
AGENTS
Labetalol and Carvedilol block α1, β1, and β2
receptors.
Carvedilol, although an effective antihypertensive,
is mainly used in the treatment of heart failure.
Carvedilol, as well as metoprolol and bisoprolol
have been shown to reduce morbidity and
mortality associated with heart failure.
Labetalol is used in the management of
gestational hypertension and hypertensive
emergencies.
α-ADRENOCEPTOR–BLOCKING AGENTS
Prazosin, Doxazosin, and Terazosin produce a
selective block of α1 adrenoceptors in arterioles and venules.
They prevent sympathetic vasoconstriction.
They decrease PVR and lower arterial B.P by causing
relaxation of both arterial and venous smooth muscle.
cause only minimal changes in CO, renal blood flow, & GFR.
Are more effective when used in combo with other agents,
such as a β blocker and a diuretic, than when used alone.
primarily used in men with concurrent HTN & BPH.
a precipitous drop in standing blood pressure develops in
some patients shortly after the first dose is absorbed, thus
the first dose should be small and should be administered at
bedtime
CENTRALLY ACTING ADRENERGIC DRUGS
1. Clonidine acts centrally at alpha2 adrenoceptors in the
medulla of the brain and at imidazoline receptors.
Reduces sympathetic and increases parasympathetic tone,
resulting in blood pressure lowering and bradycardia.
This leads to reduced TPR and decreased B.P.
used primarily for the tx of HTN that has not responded
adequately to treatment with two or more drugs.
PK: absorbed well after oral admin. and excreted by kidney.
Also available in a transdermal patch.
AE: sedation, dry mouth, and constipation.
Rebound hypertension occurs following abrupt withdrawal of
clonidine. The drug should, therefore, be withdrawn slowly if
discontinuation is required.
2. Methyldopa
Methyldopa is a centrally acting alpha2 adrenoceptor agonist
that is converted to methylnorepinephrine centrally to
diminish adrenergic outflow from the CNS (sympathetic tone)
It lowers blood pressure chiefly by reducing peripheral
vascular resistance, with a variable reduction in heart rate
and cardiac output.
The most common side effects of methyldopa are sedation
and drowsiness.
Its use is limited due to adverse effects and the need for
multiple daily doses.
It is mainly used for management of hypertension in
pregnancy, where it has a record of safety.
RENIN INHIBITOR
Inhibits enzyme activity of renin Aliskiren
Aliskiren directly inhibits renin and, thus, acts earlier in
the RAAS than ACEIs or ARBs .
Reduces angiotensin I and II and aldosterone.
It lowers blood pressure about as effectively as ARBs,
ACE inhibitors, and thiazides.
should not be routinely combined with an ACEI or ARB.
AE: can cause diarrhea, especially at higher doses, and
can also cause cough and angioedema, but probably less
often than ACE inhibitors.
Contraindicated during pregnancy.
metabolized by CYP 3A4 and is subject to many DIs
Therapeutic uses
as an initial therapy or as add-on therapy.
useful in the treatment of hypertensive patients who also
have asthma, diabetes, and/or PVD, because unlike β-
blockers, they do not adversely affect these conditions.
Hypertension (all drugs), Angina (all
drugs),Antiarrhythmics- atrial fibrillation(verapamil,
diltiazem)
Pharmacokinetics
Most of these agents have short half-lives (3 to 8 hours)
following an oral dose.
SR preps are available and permit once-daily dosing.
Amlodipine has a very long half-life and does not require a
sustained-release formulation.
Calcium Channel Blockers
MOA: block the inward movement of calcium by binding to
L-type calcium channels in the heart and in smooth muscle of
the coronary and peripheral arteriolar vasculature. This
causes vascular smooth muscle to relax, dilating mainly
arterioles.
Divided into three chemical classes, each with different
pharmacokinetic properties and clinical indications.
1. Diphenylalkylamines:
Verapamil : is the least selective of any calcium channel
blocker and has significant effects on both cardiac and
vascular smooth muscle cells.
It is also used to treat angina and SVT and to prevent
migraine and cluster headaches.
Mode of Action
Block inward current of Calcium into cells in vascular
smooth muscle, myocardium and cardiac conducting system
via L-type calcium channels.
Act on coronary arteriolar smooth muscle to reduce
vascular resistance and myocardial oxygen requirements,
relieving angina symptoms.
Dihydropyridines act mainly on arteriolar smooth muscle to
reduce peripheral vascular resistance and BP. They have
minimal effect on myocardial cells.
Non-dihydropyridines: Diltiazem and Verapamil act on
cardiac and arteriolar smooth muscle. They reduce cardiac
contractility, heart rate and conduction, with verapamil
having the greater effect. Diltiazem has a greater effect on
arteriolar smooth muscle than verapamil.
2. Benzothiazepines:
Diltiazem : affects both cardiac and vascular smooth
muscle cells, but it has a less pronounced negative inotropic
effect on the heart compared to that of verapamil. Diltiazem
has a favorable side effect profile.
3. Dihydropyridines:
Nifedipine, Amlodipine Felodipine, Nicardipine.
act mainly on arteriolar smooth muscle (vascular calcium
channels) to reduce peripheral vascular resistance and BP.
Their affinity for vascular calcium channels rather than for
calcium channels in the heart, makes them particularly
beneficial in treating hypertension.
All differ in their PK, approved uses, and DIs.
Adverse effects
First-degree atrioventricular block and constipation are
common dose dependent side effects of Verapamil.
Verapamil and diltiazem should be avoided in patients with
heart failure or with atrioventricular block due to their
negative inotropic (force of cardiac muscle contraction) and
dromotropic (velocity of conduction) effects.
Dizziness, headache, and a feeling of fatigue caused by a
decrease in blood pressure are more frequent with
dihydropyridines.
Peripheral edema is another commonly reported side
effect.
Nifedipine and other dihydropyridines may cause gingival
hyperplasia.
Reflex tachycardia ("-dipine"s)
DIRECT-ACTING VASODILATORS
Hydralazine and Minoxidil are direct-acting smooth
muscle relaxants.
Hydralazine : Causes nitric oxide release, ↓ TPR via
arteriolar dilation.
Minoxidil : metabolite opens Potassium channels in
vascular smooth muscle causing hyperpolarization of smooth
muscle, results in arteriolar vasodilation.
Decreased arterial resistance and mean arterial blood
pressure elicit compensatory responses reflex stimulation
of heart, resulting in the competing reflexes of increased
myocardial contractility, heart rate, and oxygen
consumption.
also ↑ plasma renin conc, resulting in NA &H 2O retention.
HYDRALAZINE
Predominantly an arteriolar vasodilator with little effect on
venous smooth muscle
Arteriolar vasodilation results in reflex sympathetic stimulation,
leading to tachycardia and fluid retention.
Increases cGMP and this will lead to smooth muscle relaxation.
Also reduces the afterload and has a greater effect to dilate the
arterial
Uses
Severe HTN and congestive heart failure
First line htn in pregnancy with methyldopa.
Why is hydralazine co-administered with beta blocker?
oTo prevent reflex tachycardia.
These actions may prompt angina pectoris, myocardial
infarction, or cardiac failure in predisposed individuals.
Hydralazine is mostly admin in combo with a β-blocker,
such as propranolol, metoprolol, or atenolol (to balance the
reflex tachycardia) and a diuretic (to decrease sodium
retention).
Together, the three drugs decrease cardiac output, plasma
volume, and peripheral vascular resistance.
Indication: B.P in pregnancy induced hypertension.
AE: headache, nausea, anorexia, palpitations, sweating,
and flushing, lupus erythematosus-like syndrome.
Tx with Minoxidil causes hypertrichosis (the growth of
body hair), thus Topical minoxidil (as Rogaine) is used to
treat male pattern baldness.
one person’s toxicity another person’s therapy.
Includes the oral vasodilators, hydralazine and minoxidil, which are used for long-term
outpatient therapy of hypertension; the parenteral vasodilators, nitroprusside, diazoxide,
and fenoldopam, which are used to treat hypertensive emergencies; the calcium channel
blockers, which are used in both circumstances; and the nitrates, used mainly in angina
Sodium Nitroprusside
Powerful vasodilator: releases nitric oxide.
↓ TPR via dilation of both arterioles and venules.
Use: hypertensive emergencies (DOC used IV)
The action occurs as a result of activation of guanylyl
cyclase, either via release of nitric oxide or by direct
stimulation of the enzyme.
The result is increased intracellular cGMP, which relaxes
vascular smooth muscle.
metabolized rapidly (half-life of minutes) and requires
continuous infusion to maintain its hypotensive action.
Adverse effects: All are due release of cyanides
(thiocyanate) – palpitation, pain abdomen, disorientation,
psychosis, weakness and lactic acidosis.
DIAZOXIDE
Diazoxide is an effective and relatively long-acting
parenterally administered arteriolar dilator that is
occasionally used to treat hypertensive emergencies.
prevents vascular smooth muscle contraction by
opening potassium channels and causing powerful
vasodilation.
FENOLDOPAM
Fenoldopam is a peripheral arteriolar dilator used for
hypertensive emergencies and postoperative
hypertension.
It acts primarily as an agonist of dopamine D 1 receptors,
resulting in dilation of peripheral arteries and natriuresis
HYPERTENSIVE EMERGENCY
rare but life-threatening situation characterized by severe
elevations in blood pressure (systolic >180 mm Hg or
diastolic >120 mm Hg) with evidence of impending or
progressive target organ damage (for example, stroke,
myocardial infarction).
B.P should be lowered by about 25%, maintaining diastolic
blood pressure at no less than 100–110 mm Hg.
Parenteral meds lower B.P rapidly (within a few hours)&
achieve reasonable B.P control, then use oral meds over
several weeks smoother long-term mgx of HTN.
Most commonly used: Sodium Nitroprusside.
Other parenteral drugs include fenoldopam, nitroglycerin,
labetalol, CCBs, diazoxide, and hydralazine.
hydralazine 5 mg bolus intravenously over 5 minutes and
repeated every 10 minutes up to a maximum of 20 mg, followed
by intravenous infusion of hydralazine
OR
labetalol (100 mg per 20 mL); initial dose of 20–40 mg given
intravenously over 1–2 minutes and repeated at intervals of 5–
10 minutes until 200 mg have been given.
Alternatively, labetalol may be given as a continuous
intravenous infusion at a rate of 2 mg per minute
Once the BP is stabilised, the patient should be changed to oral
treatment for maintenance.
RESISTANT HYPERTENSION
defined as blood pressure that remains elevated
(above goal) despite administration of an optimal three-
drug regimen that includes a diuretic.
The most common causes of resistant hypertension
are poor compliance, excessive ethanol intake,
concomitant conditions (diabetes, obesity, sleep apnea,
hyperaldosteronism, high salt intake, and/or metabolic
syndrome), concomitant medications
(sympathomimetics, nonsteroidal anti-inflammatory
drugs, or antidepressant medications), insufficient dose
and/or drugs, and use of drugs with similar mechanisms
of action.
COMBINATION THERAPY
Combination therapy with separate agents or a fixed-dose
combination pill may lower blood pressure more quickly
with minimal adverse effects.
A variety of combination formulations of the various
pharmacologic classes are available to increase ease of
patient adherence to treatment regimens that require
multiple medications to achieve the blood pressure goal.
You might also like
- Antihypertensive Drugs Lecture-1Document94 pagesAntihypertensive Drugs Lecture-1onyeukwudaniel12No ratings yet
- Pharmacology NotesDocument6 pagesPharmacology NotesHarsh PawarNo ratings yet
- Antihypetensive DrugsDocument64 pagesAntihypetensive DrugsParsa EbrahimpourNo ratings yet
- Cardiovascular Drugs - IODocument18 pagesCardiovascular Drugs - IOJoël N PaulNo ratings yet
- 11A Drugs Acting On The Cardiovascular SystemDocument85 pages11A Drugs Acting On The Cardiovascular SystemJaps De la CruzNo ratings yet
- HypertensionDocument54 pagesHypertensionBadri KarkiNo ratings yet
- HYPERTENSIONDocument10 pagesHYPERTENSIONChelsea Faith SarandiNo ratings yet
- Hypertension An OverviewDocument214 pagesHypertension An OverviewdkhandkeNo ratings yet
- Anti Hypertensive DrugsDocument46 pagesAnti Hypertensive DrugsShabaka KashataNo ratings yet
- Integrated Therapeutics IiiDocument160 pagesIntegrated Therapeutics IiiSalahadinNo ratings yet
- HYPERTENSIONDocument5 pagesHYPERTENSIONRajesh RamanNo ratings yet
- Hipertensi: DR M. Arman Nasution SPPDDocument101 pagesHipertensi: DR M. Arman Nasution SPPDDian PuspaNo ratings yet
- CVS & Hypolipidemic Drugs-NursingDocument71 pagesCVS & Hypolipidemic Drugs-NursingManikanta Guptha100% (1)
- Lec 22 ANTIHYPERTENSIVE - 2Document22 pagesLec 22 ANTIHYPERTENSIVE - 2Abdul MananNo ratings yet
- Ishac M2 Cardio Antihypertensives 2010Document16 pagesIshac M2 Cardio Antihypertensives 2010Franchesca LugoNo ratings yet
- 6 HypertensionDocument95 pages6 HypertensionZeleke temechewNo ratings yet
- Cardiovascular Drugs Part OneDocument115 pagesCardiovascular Drugs Part Oneelias adugnaNo ratings yet
- Antihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityDocument71 pagesAntihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityMoonAIRNo ratings yet
- General Internal Medicine Hour: HypertensionDocument33 pagesGeneral Internal Medicine Hour: HypertensionRadley Jed C. PelagioNo ratings yet
- Anti Hypertensive ThesisDocument85 pagesAnti Hypertensive Thesiskartik369No ratings yet
- Anti HypretensivesDocument18 pagesAnti HypretensivesLeena AlateeqNo ratings yet
- Anti HypretensivesDocument18 pagesAnti HypretensivesLeena AlateeqNo ratings yet
- Hypertension TejaDocument64 pagesHypertension TejaAnushka MaheshwariNo ratings yet
- Hypertension PDFDocument57 pagesHypertension PDFrahul m dNo ratings yet
- Hypertension OutlineDocument14 pagesHypertension OutlineMaria CayacoNo ratings yet
- PCOL - Chapter 11 - Anti Hypertensive AgentsDocument3 pagesPCOL - Chapter 11 - Anti Hypertensive AgentsCharles BayogNo ratings yet
- Lec 6 Anti-Hypertensive DrugsDocument31 pagesLec 6 Anti-Hypertensive Drugsph211333No ratings yet
- Drugs Used To Treat Cardiovascular Diseases: HypertensionDocument35 pagesDrugs Used To Treat Cardiovascular Diseases: HypertensionAyro Business CenterNo ratings yet
- HypertensionDocument10 pagesHypertensionaa zzNo ratings yet
- Pharmacology of Hypertension: Zebenay B. (B. Pharm, Msc. in Pharmacology)Document74 pagesPharmacology of Hypertension: Zebenay B. (B. Pharm, Msc. in Pharmacology)Gudisa KufoNo ratings yet
- 1 Drugs For HypertensionDocument62 pages1 Drugs For HypertensionSaniNo ratings yet
- HypertensionDocument12 pagesHypertensionDr. PARMINDER NAINNo ratings yet
- Drugs For Hypertension 2023Document19 pagesDrugs For Hypertension 2023aguilarjanicaNo ratings yet
- Oleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Document40 pagesOleh: Bagian Ilmu Penyakit Dalam FK Universitas Sultan Agung Semarang 2012Mbenk NjoeNo ratings yet
- 1 Antihypertensive DrugsDocument14 pages1 Antihypertensive DrugsReda SoNo ratings yet
- Antihypertensive DrugsDocument78 pagesAntihypertensive DrugsOsannah Irish InsongNo ratings yet
- HTNDocument54 pagesHTNapi-232466940No ratings yet
- Hypertension 2021Document60 pagesHypertension 2021mospala285No ratings yet
- Pharma Notes 17-18Document4 pagesPharma Notes 17-18flixiexpressNo ratings yet
- Hypertension: Margaret Xaira R. Mercado RNDocument36 pagesHypertension: Margaret Xaira R. Mercado RNMargaret Xaira Rubio MercadoNo ratings yet
- HypertensionDocument6 pagesHypertensionMatthew Michael100% (1)
- Anti Hypertensive DrugsDocument13 pagesAnti Hypertensive DrugsbajaocNo ratings yet
- Antihypertensives Cardiovascular PharmacologyDocument52 pagesAntihypertensives Cardiovascular PharmacologyAlan LealNo ratings yet
- 5 HypertensionDocument8 pages5 Hypertensioniraqeana100100No ratings yet
- Antihypertensive DrugsDocument7 pagesAntihypertensive Drugshamadadodo7No ratings yet
- HipertensiDocument37 pagesHipertensiIrna Purwanti RahayuNo ratings yet
- HYPERTENSION LiyanaDocument33 pagesHYPERTENSION LiyanaLiyana SafitriNo ratings yet
- Drugs Targeting The Renin-Angiotensin - Aldosterone SystemDocument24 pagesDrugs Targeting The Renin-Angiotensin - Aldosterone SystemAriel OlshevskyNo ratings yet
- Drugs Acting On Cardiovascular System-FinalsDocument125 pagesDrugs Acting On Cardiovascular System-FinalsPrincess C. SultanNo ratings yet
- Hypertension: 1-Hypertension Is Defined As (BP)Document37 pagesHypertension: 1-Hypertension Is Defined As (BP)hussein alnasryNo ratings yet
- Overview:: (Apresoline) (Loniten)Document31 pagesOverview:: (Apresoline) (Loniten)TaikoNo ratings yet
- Drugs Affecting The Cardiovascular SystemDocument70 pagesDrugs Affecting The Cardiovascular SystemRayne Bonifacio100% (2)
- Hipertensi - Interna - Dr. MuzakkirDocument43 pagesHipertensi - Interna - Dr. MuzakkirFarnida JamhalNo ratings yet
- Kuliah Hipertensi KMB1 2018Document43 pagesKuliah Hipertensi KMB1 2018Ainu RamadhaniNo ratings yet
- Genxraver Girl Interrupted Usmle Step 2 Notes PDFDocument259 pagesGenxraver Girl Interrupted Usmle Step 2 Notes PDFughbuzzoffNo ratings yet
- High Blood Pressure: Natural Self-help for Hypertension, including 60 recipesFrom EverandHigh Blood Pressure: Natural Self-help for Hypertension, including 60 recipesNo ratings yet
- The High Blood Pressure Diet Natural Foods that will Lower your Blood Pressure within Weeks!From EverandThe High Blood Pressure Diet Natural Foods that will Lower your Blood Pressure within Weeks!No ratings yet
- 6.3 Neuro Case PresDocument25 pages6.3 Neuro Case PresJane StarkNo ratings yet
- Pharmacology Semi FinalsDocument269 pagesPharmacology Semi FinalsTrishaNo ratings yet
- K51 - Anestesi Pada CV System (Anastesi)Document77 pagesK51 - Anestesi Pada CV System (Anastesi)Dwi Meutia IndriatiNo ratings yet
- DigoxinDocument6 pagesDigoxinSEIYADU IBRAHIM KNo ratings yet
- 2017 Blood Pressure Guideline SlidesDocument98 pages2017 Blood Pressure Guideline Slidesrusu_alexandra_4No ratings yet
- Pcol MidtermsDocument25 pagesPcol MidtermsnoyaNo ratings yet
- Pharmacology Mnemonics (Part 01) by M IhtishamDocument32 pagesPharmacology Mnemonics (Part 01) by M Ihtishammuhammad ihtisham ul hassan100% (1)
- Cardiovascular Drugs - WsDocument45 pagesCardiovascular Drugs - WsCowox Post PartumNo ratings yet
- Diabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000Document7 pagesDiabetes and Hypertension Physiopathology and Therapeutics: Journal of Human Hypertension May 2000chandra9000No ratings yet
- Nursing Responsibilities in Administering Cardiovascular DrugsDocument76 pagesNursing Responsibilities in Administering Cardiovascular DrugsNikka Moreen Dagdag80% (5)
- Hypertension Management RecommendationDocument32 pagesHypertension Management RecommendationSomnath Das GuptaNo ratings yet
- Recent Trends in The Pharmacotherapy of Angina Pectoris: ArticleDocument14 pagesRecent Trends in The Pharmacotherapy of Angina Pectoris: ArticleLarysuka DenysukaNo ratings yet
- The Crash CartDocument39 pagesThe Crash Cartpramod kumawat100% (1)
- Pharmacology-Part 1.Document90 pagesPharmacology-Part 1.Hain YoloNo ratings yet
- Prefix Suffix MnemonicsDocument4 pagesPrefix Suffix MnemonicsAubrey BellezaNo ratings yet
- Drug Class Overviews Calcium Channel Blockers Clinical PharmacologyDocument11 pagesDrug Class Overviews Calcium Channel Blockers Clinical Pharmacologynino dzaganiaNo ratings yet
- EpilatDocument2 pagesEpilatmahgadNo ratings yet
- Acls Drugs FlashcardsDocument4 pagesAcls Drugs FlashcardsLisaNo ratings yet
- Thyroid Storm - UpToDateDocument21 pagesThyroid Storm - UpToDateJENNYLA HAZEL SICLOTNo ratings yet
- Pharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Document23 pagesPharmacology Assignment No.02: Submitted By: Submitted To: Nandraj Ma'am Areeba Shafiq Roll No. 1817007Nandraj123100% (1)
- Anti HypertensivesDocument23 pagesAnti HypertensivesLeena AlateeqNo ratings yet
- Amlong-5 AMLONG-10: When You Must Not Take ItDocument5 pagesAmlong-5 AMLONG-10: When You Must Not Take ItBhanu Rekha RupanaguntlaNo ratings yet
- Isman Firdaus, DR, SP - JP (K), FIHA: QualificationDocument38 pagesIsman Firdaus, DR, SP - JP (K), FIHA: QualificationGhinna Septhiana PratiwiNo ratings yet
- Mineral, Vitamin, and Herbal SupplementsDocument18 pagesMineral, Vitamin, and Herbal SupplementsismailcemNo ratings yet
- 4 Calcium Channel BlockersDocument16 pages4 Calcium Channel BlockersIman SaksoukNo ratings yet
- Hipertensi: Dr. Jamaluddin, M.Kes, SP - JPDocument82 pagesHipertensi: Dr. Jamaluddin, M.Kes, SP - JPRahmawati HamudiNo ratings yet
- Hipertensi UrgensiDocument26 pagesHipertensi UrgensidiegoNo ratings yet
- DR AZAM'S Notes in Anesthesiology CARDIOVASCULAR - SYSTEM PDFDocument624 pagesDR AZAM'S Notes in Anesthesiology CARDIOVASCULAR - SYSTEM PDFjayadi100% (4)
- Drugs Used in AnginaDocument24 pagesDrugs Used in AnginaChandra ShinodaNo ratings yet
- Sympathomimetics Drugs REVIEWDocument9 pagesSympathomimetics Drugs REVIEWLyca SalardaNo ratings yet