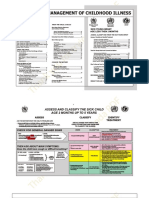
At the start of a sick child (2 months to 5 years) consultation
Ask the mother what the childs problems are. Determine if this is an initial or followup visit for this problem.
�IMCI Case Management
Focused Assessment Danger signs Main Symptoms Nutritional status Immunization status Other problems Classification
Need to Refer
Specific treatment
Home management
Treatment Identify treatment Treat
Counsel & Follow-up Counsel caretakers Follow-up
�Check for general danger signs
Ask: Not able to drink or breastfeed, Vomits everything, Convulsions, or Look: Abnormally sleepy or difficult to awaken
Need to Refer (except in severe dehydration)
�Ask about the main symptoms
Cough or difficulty in breathing Diarrhea Fever Ear problem
�Cough or difficulty in breathing
Ask: For how long? Look: Count RR Chest indrawing Stridor
The child must be calm.
� Any general danger sign or Chest indrawing or Stridor
SEVERE PNEUMONIA OR VERY SEVERE DISEASE
1st dose of antibiotic Vitamin A Breastfeeding/sugar water URGENT REFERRAL
�� Fast breathing 2 12 months old: 50/minute 1 year or older: 40/minute
PNEUMONIA
Antibiotic for 5 days Relieve cough with safe remedy Advise mother on danger signs Follow up in 2 days
�No signs of pneumonia or a very severe disease
NO PNEUMONIA: COUGH OR COLD
If cough 30 days refer to hospital for assessment Relieve cough with safe remedy Advise mother on danger signs Follow up in 5 days if no improvement
�Diarrhea: Classify For dehydration
Persistent diarrhea Blood in the stool
�Classify for dehydration
2 or more of the following:
Abnormally sleepy/difficult to wake Sunken eyes Not able to feed/drinking poorly Skin pinch goes back very slowly
SEVERE DEHYDRATION
Plan C
��Plan C: To treat dehydration quickly
IV fluid: LRS 100 ml/kg body weight (in 6 hrs for infants; 3 hrs for children)
NO
IV treatment within 30 minutes
NO
Oresol/NGT
�Plan C: To treat dehydration quickly
Oresol/NGT
NO
Oresol p.o.
NO
URGENT REFERRAL
�Classify for dehydration
2 of the following:
Restless, irritable Sunken eyes Drinks eagerly, very thirsty Skin pinch goes back slowly
SOME DEHYDRATION
Plan B
�Plan B: Treat some dehydration with ORS
Determine the amount (in ml) of Oresol to be given in 4 hours = weight of the child (in kg) X 75, or if weight is unknown, use this chart.
Age < 4 mos 4-12 mos
Amount
200-400
400-700
�Plan B: Treat some dehydration with ORS
Determine the amount (in ml) of Oresol to be given in 4 hours = weight of the child (in kg) X 75, or if weight is unknown, use this chart.
Age 12 mos-2 yrs 2-5 yrs
Amount
700-900
900-1400
�Plan B: Treat some dehydration with ORS
Show the mother how to give Oresol to the child: frequent sips from a cup If the child vomits, wait for 10 minutes. Then continue, but more slowly. Continue breastfeeding if the child wants to breastfeed. If the child develops puffy eyelids, stop ORS.
�Plan B: Treat some dehydration with ORS
After 4 hours: Reassess the child & classify for dehydration. Select appropriate plan. Begin feeding the child in the health center.
�Classify for dehydration
Not enough signs to classify as SEVERE DEHYDRATION or SOME DEHYDRATION
NO DEHYDRATION
Plan A
�Plan A: Treat diarrhea at home
Give extra fluid.
Up to 2 yrs 50 100 ml after each LBM
2 -4 yrs
100 200 ml after each LBM
Continue feeding. Know when to return.
�Persistent diarrhea: 14 days or more
+ Dehydration=severe persistent diarrhea
Treat dehydration Give Vitamin A Refer to hospital
�Persistent diarrhea: 14 days or more
No dehydration=persistent diarrhea
Advise regarding feeding Give Vitamin A Follow up in 5 days
�Blood in the stool = dysentery
Oral antibiotic for shigella for 5 days Follow up in 2 days
�Fever: (history/temperature 37.5C or above)
Malaria risk?
Measles now or w/in last 3 mos Dengue risk?
�Fever: Ask about malaria risk
Residing in endemic area? OR: Travel & overnight w/in past stay in endemic area, or 6 mos Blood transfusion
�Malaria risk +
Blood smear Ask: Duration of fever? Present everyday? Look: Stiff neck Runny nose Other signs of measles
�Malaria risk + any general danger sign or stiff neck
Very severe febrile disease/malaria
Quinine (under med. supervision) 1st dose of antibiotic, Paracetamol Urgent referral
�Malaria risk +, blood smear + No runny nose, no measles
Malaria
Oral antimalarial Paracetamol Follow up in 2 days > 7 days fever hospital for assessment
�No malaria risk Any general danger sign or stiff neck
Very severe febrile disease
1st dose of antibiotic, Paracetamol Urgent referral
�Measles now or w/in last 3 mos Clouding of cornea or Deep or extensive mouth ulcers
Severe complicated measles
1st dose of antibiotic, Vitamin A Urgent referral
�Measles now or w/in last 3 mos Pus draining from the eye or Mouth ulcers
Measles with eye or Mouth complications
Vitamin A Tetracycline eye ointment Gentian violet Follow up in 2 days
�Measles now or w/in last 3 mos No other signs
Measles
Vitamin A
�If there is Dengue risk
Bleeding gums, nose, in vomitus or stools Black vomitus or stools Persistent abdominal pain Persistent vomiting Skin petechiae Slow capillary refill No signs, but fever > 3 days Tourniquet test
�Slow capillary refill
Indicates poor skin perfusion Press down firmly with your finger on the sternum for 5 seconds and release. (Alternatively you can use the nail bed or soles of the feet.) A normal capillary refill should occur within 2-3 seconds.
�Any of the danger signs or + tourniquet test
Severe Dengue hemorrhagic fever
If skin petechiae, persistent abdominal pain or vomiting, or + tourniquet test only signs, give ORS Any other signs of bleeding Plan C Urgent referral Do not give aspirin
�Ear problem: tender swelling behind ear
Mastoiditis
1st dose of antibiotic Paracetamol for pain Urgent referral
��Ear discharge < 14 days or Ear pain
Acute ear infection
Antibiotic for 5 days Paracetamol for pain Wicking Follow up in 5 days
�Ear discharge for 14 days or more
Chronic ear infection
Wicking Follow up in 5 days
��Visible severe wasting or Edema on both feet or Severe palmar pallor
Severe malnutrition or severe anemia
Vitamin A Urgent referral
�Some palmar pallor or Very low weight for age
Anemia or very low weight for age
Assess for feeding problem Pallor: iron & Mebendazole in children > 2 yrs Wt for age very low: Vitamin A