Professional Documents
Culture Documents
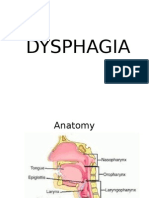
Dysphagia
Uploaded by
Mickola Vorokhta0 ratings0% found this document useful (0 votes)
4 views34 pagesswallowing disorder
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentswallowing disorder
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views34 pagesDysphagia
Uploaded by
Mickola Vorokhtaswallowing disorder
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 34
Dysphagia
Vorokhta Y., MD, PhD
Phases
Neuroanatomy
Motor function Sensory function
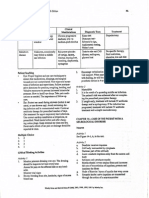
Zone of innervation Nerves Zone of innervation Nerves
Mimic muscles VII Soft palate, oral mucosa, anterior 2/3 V
of the tongue, nasopharynx
Chewing muscles V3 Anterior 2/3 of the tongue VII
The palate (except the palatal Х Posterior 1/3 of the tongue, ІХ
curtain), pharynx (except the oropharynx
pharyngeal muscle), larynx,
esophagus
Palatal curtain V3 Tongue root, larynx Х
The stylopharyngeal muscle ІХ
Muscles of tongue XII
Cervical Muscles V3, VII,
C1-C2
Neuroanatomy
Anatomic region Role
Primary somatosensory, motor Regulation of movements, control and coordination
cortex (ВА 1,2,3,4,6) of the act of swallowing
Cingular gyrus (ВА 24,32) Planning the act of swallowing, choosing a model of
behavior
Orbitofrontal cortex (ВА ?
10,11,12,44,45,47)
Parieto-occipital cortex (ВА Swallowing coordination, sensory processing
7,17,18,40)
Cortex of the temporal lobe pole ?
(ВА 22,38)
Insular cortex Oral phase modulation, processing of afferent information from
taste buds)
capsula interna Tr. corticobulbaris
thalamus Tr.thalamocorticalis, tr. thalamostriaris
Neuroanatomy
Anatomic region Role
Basal ganglia (caudate nucleus, Processing of afferent information
putamen)
Middle peduncles of the tractus pontocerebellares,, fibrae corticopontinae
cerebellum
Brainstem Subcortical center of swallowing, nuclei V, VII, IX, X,
XII FMN
Cerebellum Regulation of coordinated movements, learning and
motor memory of muscles involved in the act of
swallowing
Neurophysiology
Risk factors
• Poor dentition
• Atrophy of the tongue and alveolar ridge
• Diminished taste and smell sensitivity
• Decreased muscle tone
• Increased ligamentous laxity
• Limited laryngeal elevation
Severity
Manifestations
Signs and symptoms of oral or pharyngeal dysphagia include the following:
• Coughing or choking with swallowing
• Difficulty initiating swallowing
• Food sticking in the throat
• Sialorrhea
• Unexplained weight loss
• Change in dietary habits
• Recurrent pneumonia
• Change in voice or speech (wet voice)
• Nasal regurgitation
Signs and symptoms of esophageal dysphagia include the following:
• Sensation of food sticking in the chest or throat
• Change in dietary habits
• Recurrent pneumonia
• Symptoms of gastroesophageal reflux disease (GERD), including heartburn, belching, sour
regurgitation, and water brash
• Other associated factors/symptoms of dysphagia include the following:
• General weakness
• Mental status changes
?
Rosenbek’s Scale
Work-up
• Transnasal esophagoscopy
• Cervical auscultation
• Blood tests: Including thyroid-stimulating hormone, vitamin B-
12, and creatine kinase; may be useful, especially in neurogenic
dysphagia
• Imaging studies: May include videofluoroscopy, computed
tomography (CT) scanning, magnetic resonance imaging (MRI),
and chest radiography
• Endoscopic examination
• Esophageal pH monitoring: The criterion standard for diagnosing
reflux disease
• Pulmonary function tests
Swallowing disorders in Neurological
Diseases
stroke (20-65%)
TBI
tumors
cerebral palsy
iatrogenic dysphagia
Alzheimer's disease, FTD, DTL, vascular dementia
Parkinson's disease
progressive supranuclear palsy
olivopontocerebellar atrophy
Huntington's chorea
Wilson's disease
multiple sclerosis, ALS, Guillain-Barré syndrome
myasthenia
neuroinfections
Iatrogenic dysphagia
• antipsychotics
• corticosteroids
• colchicine
• aminoglycosides
• cholinolytics
• drugs that damage the mucous membranes of the mouth
and pharynx: potassium chloride, NSAIDs, some antibiotics
(doxycycline, tetracycline, biseptol, clindamycin)
• drugs that cause xerostomia (cholinolytics, alpha-blockers,
ACE inhibitors, antihistamines)
• surgery on the head and neck can also cause dysphagia.
Post-stroke dysphagia (PSD or SRD)
in the acute period of a stroke it is noted in 64-
94% of cases, most often - in the first 3-10 days;
in the recovery period - in 23-50% of patients,
and about 11% of patients in the rehabilitation
phase still need tube feeding.
mortality among stroke patients with dysphagia
is 27-37%.
Recovery
TREATMENT
Pharmacologic treatment
• Botulinum toxin type A (BoNT-A)
• Diltiazem
• Cystine-depleting therapy with cysteamine
• Nitrates
Dietary treatment
• Dietary modification is the key component in the general treatment program of
dysphagia. Diets for patients with dysphagia include the following:
• Dysphagia diet 1: Thin liquids (eg, fruit juice, coffee, tea)
• Dysphagia diet 2: Nectar-thick liquids (eg, cream soup, tomato juice)
• Dysphagia diet 3: Honey-thick liquids (ie, liquids that are thickened to a honey
consistency)
• Dysphagia diet 4: Pudding-thick liquids/foods (eg, mashed bananas, cooked cereals,
purees)
• Dysphagia diet 5: Mechanical soft foods (eg, meat loaf, baked beans, casseroles)
• Dysphagia diet 6: Chewy foods (eg, pizza, cheese, bagels)
• Dysphagia diet 7: Foods that fall apart (eg, bread, rice, muffins)
• Dysphagia diet 8: Mixed textures
TREATMENT
Exercise and facilitation techniques
• The following types of exercise can be recommended to patients with dysphagia:
• Indirect (eg, exercises to strengthen swallowing muscles)
• Direct (eg, exercises to be performed while swallowing)
• Facilitation techniques used in the treatment of dysphagia include the following:
• Somatosensory stimulation: In the form of an electrical current applied to the pharynx
• Deep pharyngeal neuromuscular stimulation (DPNS)
• Tactile-thermal stimulation (TTS)
Compensatory techniques
• Maintaining oral feeding often requires compensatory techniques to reduce aspiration
or improve pharyngeal clearance. These include the following:
• Use of the chin-tuck position
• Rotation of the head to the affected side
• Tilting of the head to the strong side
• Lying on one's side or back during swallowing
• Supraglottic swallow
• Bolus-clearing maneuvers
TREATMENT
Enteral feeding
• Nasogastric tube (NGT) feeing
• Oroesophageal tube feeding
• Percutaneous endoscopic gastrostomy (PEG)
Surgery for chronic aspiration
• Medialization: This helps to restore glottic closure and subglottic pressure
during the swallow
• Laryngeal suspension: The larynx is in a relatively protected position under
the tongue base
• Laryngeal closure: This may be performed to close the glottis off, in this
way protecting the airway at the expense of phonation
• Laryngotracheal separation-diversion: This procedure may be done to
separate the airway from the alimentary tract
Vitastim ™
VitaStim software
You might also like
- Lianne Beck, MD Assistant Professor Emory Family MedicineDocument52 pagesLianne Beck, MD Assistant Professor Emory Family MedicineTauqeer IqbalNo ratings yet
- DYSPHAGIADocument47 pagesDYSPHAGIANur Khairah AmalinaNo ratings yet
- UntitledDocument115 pagesUntitledİpek OMURNo ratings yet
- Dysphagia (ENT Posting)Document36 pagesDysphagia (ENT Posting)rajhiniNo ratings yet
- Nur Akbar A. Mini LectureDocument39 pagesNur Akbar A. Mini LectureanafauziahfitriNo ratings yet
- MS NeuroDocument28 pagesMS NeuroFrechel Ann Landingin PedrozoNo ratings yet
- Dysphagia: Dr. Ravi Gadani MS, FmasDocument39 pagesDysphagia: Dr. Ravi Gadani MS, FmasRaviNo ratings yet
- PLENO 1 Kel 5Document60 pagesPLENO 1 Kel 5cecilliacynthiaNo ratings yet
- Case Sensory DysphagiaDocument30 pagesCase Sensory DysphagiaPhitsanu SuntornpiyapanNo ratings yet
- Sistem Saraf OtonomDocument31 pagesSistem Saraf OtonomMagista Nugraha100% (1)
- Dysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SDocument64 pagesDysphagia: DR Navin Shukla Associate Professor Department of E.N.T&H.N.SNavin ShuklaNo ratings yet
- Speech Swallowing ImpairmentDocument36 pagesSpeech Swallowing ImpairmentSamer FarhanNo ratings yet
- Dysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalDocument48 pagesDysphagia: DR (Prof.) A B Singh Unit Department of General Surgery Patna Medical College & HospitalAswin Rajasekaran100% (1)
- 3.4. Seminar-The Digestive SystemDocument54 pages3.4. Seminar-The Digestive System6f5d6b5r6tNo ratings yet
- Anatomy and Histology of Mouth - OesophagusDocument70 pagesAnatomy and Histology of Mouth - OesophagusRevila AuliaNo ratings yet
- Dysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Document31 pagesDysphagia: Departemen THT-KL Fakultas Kedokteran Universitas Padjadjaran 2016Sherlyn YeeNo ratings yet
- Palliative Care - Physical AspectsDocument61 pagesPalliative Care - Physical AspectsMars AhlaNo ratings yet
- RESIRATORYDocument121 pagesRESIRATORYpashaNo ratings yet
- Movement Disorders of The Mouth Review of The Common Phenomenologies 2022Document19 pagesMovement Disorders of The Mouth Review of The Common Phenomenologies 2022Gonçalo CabralNo ratings yet
- 1 - Dysphagia and StrokeDocument39 pages1 - Dysphagia and StrokeVeggy Septian Ellitha100% (1)
- DISFAGIA ConcensoDocument9 pagesDISFAGIA Concensolbritez7No ratings yet
- Management of Brain MetastasisDocument69 pagesManagement of Brain MetastasisshokoNo ratings yet
- Tardive Dyskinesia: Chairperson - DR - Denzil A PintoDocument46 pagesTardive Dyskinesia: Chairperson - DR - Denzil A PintodarchanaavigneshNo ratings yet
- Group 7-Plenary 1-GI 2015Document41 pagesGroup 7-Plenary 1-GI 2015Mudita DewiNo ratings yet
- Tiếp Cận Lâm Sàng Trong Chẩn Đoán TMJ - LisaChongDocument97 pagesTiếp Cận Lâm Sàng Trong Chẩn Đoán TMJ - LisaChongKeHuyDietNo ratings yet
- Peripheral Distribution of Cranial Nerves 9,10,11,12Document75 pagesPeripheral Distribution of Cranial Nerves 9,10,11,12Muhammad Bilal IbrahimNo ratings yet
- Neuropharmacology of The ENSDocument34 pagesNeuropharmacology of The ENS120420314No ratings yet
- SGD5 GitDocument59 pagesSGD5 GitMARGARET BLANCHE NICOLASNo ratings yet
- PHPY 303 - GI Lecture #2 - March 14Document25 pagesPHPY 303 - GI Lecture #2 - March 14smhallmobileNo ratings yet
- Vagus Nerve: Vagus Nerve Activities to Relieve Anxiety, Reduce Severe Illness, Relief Depression, Anxiety, Stimulate Vagal Tone, Prevent Inflammation, Trauma, and PTSDFrom EverandVagus Nerve: Vagus Nerve Activities to Relieve Anxiety, Reduce Severe Illness, Relief Depression, Anxiety, Stimulate Vagal Tone, Prevent Inflammation, Trauma, and PTSDRating: 1 out of 5 stars1/5 (1)
- Dysphagia: Muhammad Albahadili MBCHB Cabs HDLMDocument58 pagesDysphagia: Muhammad Albahadili MBCHB Cabs HDLMAli HusseinNo ratings yet
- Neuro CH 14 Study GuideDocument9 pagesNeuro CH 14 Study GuideMichael J MillerNo ratings yet
- Medical Surgical Nursing Review NotesDocument75 pagesMedical Surgical Nursing Review NotesMary Ann Comia RañolaNo ratings yet
- Upper GI Disorders Study GuideDocument10 pagesUpper GI Disorders Study Guidemelpietrowski100% (1)
- Table of 12 Cranials and TractusDocument5 pagesTable of 12 Cranials and TractusjuwitavalenNo ratings yet
- 2022-03-28 - Paediatric Swallowing and Feeding - EdU - Student - OnlineDocument107 pages2022-03-28 - Paediatric Swallowing and Feeding - EdU - Student - Onlineszeho chan100% (1)
- Neurogastroenterology PhysiologyDocument15 pagesNeurogastroenterology PhysiologyTanyaNo ratings yet
- Konsep Perioperatif: SubtitleDocument42 pagesKonsep Perioperatif: SubtitleyuanitaNo ratings yet
- Jurnal Neurogenic Bladder: PembimbingDocument16 pagesJurnal Neurogenic Bladder: PembimbingRamlah AndariasNo ratings yet
- DysfagiaDocument14 pagesDysfagiadrakeironquistNo ratings yet
- Gaggers and Its ManagementDocument58 pagesGaggers and Its ManagementAwani GuptaNo ratings yet
- 2 - Sallowing - 2018Document43 pages2 - Sallowing - 2018suresh herathNo ratings yet
- Special Senses - Oral Cavity Etc.Document18 pagesSpecial Senses - Oral Cavity Etc.Dunkin DonutNo ratings yet
- On Cerebral PalsyDocument18 pagesOn Cerebral Palsyanimol abrahamNo ratings yet
- Nurologic Ass Faculty - 2023 1st Term-1Document29 pagesNurologic Ass Faculty - 2023 1st Term-1cwley64No ratings yet
- Unit 1 Disorders of Upper Gastrointestinal Tract: StructureDocument18 pagesUnit 1 Disorders of Upper Gastrointestinal Tract: StructureShubhendu ChattopadhyayNo ratings yet
- Parkinson's DiseaseDocument16 pagesParkinson's DiseaseNab MughalNo ratings yet
- Nursing Care Plan StrokeDocument3 pagesNursing Care Plan StrokeDawn NavarroNo ratings yet
- PHARM Ven IntroToAnesthesiaDocument22 pagesPHARM Ven IntroToAnesthesiaDhaif dhaifNo ratings yet
- Symptoms Management of Palliative PatientsDocument25 pagesSymptoms Management of Palliative PatientsUtkarsh JhaNo ratings yet
- AUA Pharmacological Treatment of Urinary Incontinence - Committee 8 (2009)Document70 pagesAUA Pharmacological Treatment of Urinary Incontinence - Committee 8 (2009)MaiandrosNo ratings yet
- Nervous System 2Document51 pagesNervous System 2وجد عمرNo ratings yet
- Disfagia Post IctusDocument4 pagesDisfagia Post IctusCarla Inés Muñoz ÑancupilNo ratings yet
- MIKROS-GIT-all PDFDocument106 pagesMIKROS-GIT-all PDFKharisulNo ratings yet
- Medical Surgical Nursing Review NotesDocument75 pagesMedical Surgical Nursing Review Notesstuffednurse92% (146)
- Total Reflexology: The Reflex Points for Physical, Emotional, and Psychological HealingFrom EverandTotal Reflexology: The Reflex Points for Physical, Emotional, and Psychological HealingRating: 2.5 out of 5 stars2.5/5 (2)
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Diagnosis and Treatment of Neurogenic Oropharyngeal DysphagiaFrom EverandDiagnosis and Treatment of Neurogenic Oropharyngeal DysphagiaNo ratings yet
- 10 1002@ana 25083Document56 pages10 1002@ana 25083Mickola VorokhtaNo ratings yet
- Cranial NervesDocument57 pagesCranial NervesMickola VorokhtaNo ratings yet
- Movement DisordersDocument73 pagesMovement DisordersMickola VorokhtaNo ratings yet
- Iatrogenic Neurological Disorders: Vorokhta Y., MD, PHDDocument23 pagesIatrogenic Neurological Disorders: Vorokhta Y., MD, PHDMickola VorokhtaNo ratings yet
- Vorokhta Y., MD, PHDDocument28 pagesVorokhta Y., MD, PHDMickola VorokhtaNo ratings yet
- PNS DisordersDocument14 pagesPNS DisordersMickola VorokhtaNo ratings yet
- Headache & Facial Pain: Vorokhta Y., MD, PHDDocument37 pagesHeadache & Facial Pain: Vorokhta Y., MD, PHDMickola VorokhtaNo ratings yet
- Neurological Complications of Sars-Covid: Vorokhta Yurii. MD, PHDDocument37 pagesNeurological Complications of Sars-Covid: Vorokhta Yurii. MD, PHDMickola VorokhtaNo ratings yet
- Sleep Disorders: Vorokhta Y., MD, PHDDocument34 pagesSleep Disorders: Vorokhta Y., MD, PHDMickola VorokhtaNo ratings yet
- CPRDocument45 pagesCPRJames Elwood DoyolaNo ratings yet
- FDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Document32 pagesFDP Form 7 - 20% Component of The IRA Utilization 20% Component of The Ira Utilization For The First Quarter, Cy 2017Juna Majistad CrismundoNo ratings yet
- Barangay Peace and Order and Public Safety PlanDocument3 pagesBarangay Peace and Order and Public Safety PlanPeter Fritz Boholst100% (1)
- FeverDocument2 pagesFeverMuhammad Jefri LukmanNo ratings yet
- What Is RCM and RBIDocument2 pagesWhat Is RCM and RBIChihiya Fitria Nurhayati0% (1)
- Quizizz: DM Bronze Recap (Final)Document10 pagesQuizizz: DM Bronze Recap (Final)Mahika ManeshNo ratings yet
- Biological Molecules 2 QPDocument12 pagesBiological Molecules 2 QPApdiweli AliNo ratings yet
- Physical Science - 11 - Q1 - 13 - Use of The Other Ingredients in Cleaning Agents 08082020Document18 pagesPhysical Science - 11 - Q1 - 13 - Use of The Other Ingredients in Cleaning Agents 08082020gwynceNo ratings yet
- Visa Application FAQ-SummerDocument8 pagesVisa Application FAQ-SummerCaioAndradeNo ratings yet
- Reflection PaperDocument27 pagesReflection PaperBon Ryan LeonardoNo ratings yet
- Proposal For The BoosterDocument5 pagesProposal For The BoosterraziNo ratings yet
- Ejsr Vol 97 Issue 1 159 171Document171 pagesEjsr Vol 97 Issue 1 159 171Raja ChandruNo ratings yet
- Evaluation Tool (Competency Based) - NonescostDocument35 pagesEvaluation Tool (Competency Based) - NonescostFroilan GuilleranNo ratings yet
- Trastorno de AdaptacionDocument11 pagesTrastorno de AdaptacionEduardo AguilarNo ratings yet
- Routes of Drug AdministrationDocument24 pagesRoutes of Drug Administrationmftaganas100% (1)
- Max Bupa Claim Form NewDocument9 pagesMax Bupa Claim Form NewViral ShuklaNo ratings yet
- Review Jurnal Varicella - Dewi Manik Aulia Fadli - 16700096Document26 pagesReview Jurnal Varicella - Dewi Manik Aulia Fadli - 16700096Lia FadliNo ratings yet
- Fistula in AnoDocument17 pagesFistula in Anoapi-216828341No ratings yet
- User's Manual: M200A Syringe PumpDocument44 pagesUser's Manual: M200A Syringe PumpGandavaa Enkhee50% (4)
- BAYBAY AwardsDocument63 pagesBAYBAY AwardsClennil Palmes SustraidoNo ratings yet
- Quiz BukasDocument3 pagesQuiz BukasDYRAH GRACE COPAUSNo ratings yet
- Prof Nik Marzuki Data PDFDocument3 pagesProf Nik Marzuki Data PDFsue labanNo ratings yet
- 3GN18CV402 Internship ReportDocument29 pages3GN18CV402 Internship ReportHP PAVILION100% (1)
- Blood Cancer Analysis by A.G.Sureshbabu ShenoyDocument4 pagesBlood Cancer Analysis by A.G.Sureshbabu Shenoysaptarishis astrologyNo ratings yet
- "Nisi Dominus Frustra" College of Nursing & Allied Health Sciences Maasin City, Southern LeyteDocument2 pages"Nisi Dominus Frustra" College of Nursing & Allied Health Sciences Maasin City, Southern Leytecoosa liquorsNo ratings yet
- VACCP Template Checklist - SafetyCultureDocument7 pagesVACCP Template Checklist - SafetyCulturepattysaborio520No ratings yet
- Vulture ConservationDocument14 pagesVulture ConservationSaba Parvin Haque100% (2)
- The Gittinger Assessment SystemDocument19 pagesThe Gittinger Assessment SystemeheymanNo ratings yet
- P CLS14 Powertec Compact Leg Sled ManualDocument15 pagesP CLS14 Powertec Compact Leg Sled ManualElizabeth GuzmanNo ratings yet
- Table Saw Safety FinalDocument24 pagesTable Saw Safety Finalvolatileyasser100% (1)