0% found this document useful (0 votes)
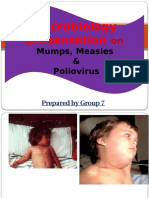
62 views62 pagesMeasles and Related Viral Infections
Uploaded by
asmashk2003Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
62 views62 pagesMeasles and Related Viral Infections
Uploaded by
asmashk2003Copyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd