0% found this document useful (0 votes)
15 views126 pagesSexually Transmitted Infections
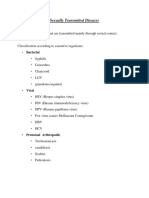
The lecture notes cover sexually transmitted infections (STIs), detailing their causes, modes of transmission, symptoms, diagnosis, and treatment. It categorizes STIs into bacterial, viral, parasitic, and fungal, and discusses risk factors and prevention strategies. Specific STIs such as gonorrhea, trichomoniasis, syphilis, and chancroid are examined in depth, including their pathophysiology and clinical manifestations.
Uploaded by
Richard KaringuriCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
15 views126 pagesSexually Transmitted Infections
The lecture notes cover sexually transmitted infections (STIs), detailing their causes, modes of transmission, symptoms, diagnosis, and treatment. It categorizes STIs into bacterial, viral, parasitic, and fungal, and discusses risk factors and prevention strategies. Specific STIs such as gonorrhea, trichomoniasis, syphilis, and chancroid are examined in depth, including their pathophysiology and clinical manifestations.
Uploaded by
Richard KaringuriCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd