100% found this document useful (7 votes)
7K views3 pagesSLE Pathophysiology
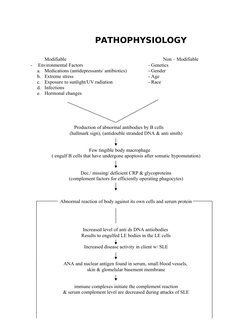
This document summarizes the pathophysiology of systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). It notes that SLE is characterized by the production of abnormal antibodies that can attack the body's own cells and proteins. This leads to immune complex formation and complement activation, resulting in tissue damage. RA is described as an abnormal immune response against antigens in the joints, leading to inflammation and the formation of pannus tissue that can erode and destroy cartilage and immobilize joints.
Uploaded by
Ranela Kwinkee Pastor SalazarCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOC, PDF, TXT or read online on Scribd
100% found this document useful (7 votes)
7K views3 pagesSLE Pathophysiology
This document summarizes the pathophysiology of systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). It notes that SLE is characterized by the production of abnormal antibodies that can attack the body's own cells and proteins. This leads to immune complex formation and complement activation, resulting in tissue damage. RA is described as an abnormal immune response against antigens in the joints, leading to inflammation and the formation of pannus tissue that can erode and destroy cartilage and immobilize joints.
Uploaded by
Ranela Kwinkee Pastor SalazarCopyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOC, PDF, TXT or read online on Scribd
- Pathophysiology: Discusses various factors influencing pathophysiology, including modifiable environmental factors and non-modifiable genetic factors, alongside abnormal immune responses.