Professional Documents
Culture Documents
Pressure Indicating Media Loney Knechtel
Uploaded by
rochirrephtto0 ratings0% found this document useful (0 votes)
27 views5 pagesprosto
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentprosto
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views5 pagesPressure Indicating Media Loney Knechtel
Uploaded by
rochirrephttoprosto
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
136 Volume 101 Issue 2
The Journal of Prosthetic Dentistry Looney and Knechtel Arrais et al
study were close to the final DC.
At the 10-minute interval, differ-
ences in DC between light- and auto-
polymerized groups ranged from 3.5%
(Calibra) to 33.9% (RelyX ARC). The
clinical relevance of such differences in
DC deserves consideration, as only a
4% decrease in DC impairs elastic mod-
ulus, hardness, and fracture strength of
composite resins.
25
The relative hard-
ness of composite resins has been pro-
posed as a means of determining the
effectiveness of polymerization when
comparing values of a test group to
those of a control group known to have
been maximally polymerized. It is also
suggested that a ratio of 90% would be
acceptable for a clinical situation.
10
If
such an assumption was extrapolated
to the DC analysis of the current study,
the autopolymerizing modes of prod-
ucts exhibiting PC
A/D
values of approxi-
mately 90% might provide RLA layers
with mechanical properties capable of
resisting the high stress imparted after
cementation of an indirect restora-
tion. Based on these findings, it may
be assumed that RLAs demonstrating
such polymerization characteristics
would perform adequately when light
is completely blocked by the indirect
restoration. However, studies evaluat-
ing the mechanical properties of dual-
polymerized RLAs within the short
period of time following the mixing of
the components may provide further
information.
CONCLUSIONS
Within the limitations of the cur-
rent study, it was concluded that the
dual-polymerizing mode of all RLAs
tested generated higher DC values than
the autopolymerizing mode. However,
R
p
max
and PC
A/D
varied widely among
products. The DC of all products at
10 minutes after initial material mixing
was higher than that at 5 minutes, only
in the autopolymerizing mode. Thus,
the first 2 research hypotheses were val-
idated, while the third hypothesis was
only validated when the resin cements
were allowed to autopolymerize.
REFERENCES
1. Braga RR, Cesar PF, Gonzaga CC. Mechanical
properties of resin cements with different ac-
tivation modes. J Oral Rehabil 2002;29:257-
62.
2. Peutzfeldt A. Dual-cure resin cements: in
vitro wear and effect of quantity of remaining
double bonds, filler volume, and light curing.
Acta Odontol Scand 1995;53:29-34.
3. Santos GC Jr, El-Mowafy O, Rubo JH, Santos
MJ. Hardening of dual-cure resin cements
and a resin composite restorative cured with
QTH and LED curing units. J Can Dent Assoc
2004;70:323-8.
4. Tanoue N, Koishi Y, Atsuta M, Matsumura H.
Properties of dual-curable luting composites
polymerized with single and dual curing
modes. J Oral Rehabil 2003;30:1015-21.
5. Arrais CA, Giannini M, Rueggeberg FA, Pash-
ley DH. Effect of curing mode on microtensile
bond strength to dentin of two dual-cured
adhesive systems in combination with resin
luting cements for indirect restorations. Oper
Dent 2007;32:37-44.
6. Lu H, Mehmood A, Chow A, Powers JM.
Influence of polymerization mode on flexural
properties of esthetic resin luting agents. J
Prosthet Dent 2005;94:549-54.
7. el-Mowafy OM, Rubo MH, el-Badrawy
WA. Hardening of new resin cements
cured through a ceramic inlay. Oper Dent
1999;24:38-44.
8. Hofmann N, Papsthardt G, Hugo B, Klaiber
B. Comparison of photo-activation versus
chemical or dual-curing of resin-based
luting cements regarding flexural strength,
modulus and surface hardness. J Oral Rehabil
2001;28:1022-8.
9. Fonseca RG, Santos JG, Adabo GL. Influence
of activation modes on diametral tensile
strength of dual-curing resin cements. Braz
Oral Res 2005;19:267-71.
10.Johnston WM, Leung RL, Fan PL. A math-
ematical model for post-irradiation hardening
of photoactivated composite resins. Dent
Mater 1985;1:191-4.
11.Blackman R, Barghi N, Duke E. Influence
of ceramic thickness on the polymerization
of light-cured resin cement. J Prosthet Dent
1990;63:295-300.
12.Cardash HS, Baharav H, Pilo R, Ben-Amar A.
The effect of porcelain color on the hardness
of luting composite resin cement. J Prosthet
Dent 1993;69:620-3.
13.Arrais CA, Rueggeberg FA, Waller JL, de Goes
MF, Giannini M. Effect of curing mode on the
polymerization characteristics of dual-cured
resin cement systems. J Dent 2008;36:418-26.
14.Milleding P, Ahlgren F, Wennerberg A,
Ortengren U, Karlsson S. Microhardness and
surface topography of a composite resin
cement after water storage. Int J Prosthodont
1998;11:21-6.
15.Nathanson D. Etched porcelain restorations
for improved esthetics, part II: Onlays. Com-
pendium 1987;8:105-10.
16.Cook WD, Standish PM. Polymerization
kinetics of resin-based restorative materials. J
Biomed Mater Res 1983;17:275-82.
17.Asmussen E. Setting time of composite
restorative resins vs. content of amine,
peroxide, and inhibitor. Acta Odontol Scand
1981;39:291-4.
18.Caughman WF, Chan DC, Rueggeberg FA.
Curing potential of dual-polymerizable resin
cements in simulated clinical situations. J
Prosthet Dent 2001;86:101-6.
19.Anusavice KJ, Hojjatie B. Tensile stress in
glass-ceramic crowns: effect of flaws and ce-
ment voids. Int J Prosthodont 1992;5:351-8.
20.Rueggeberg FA, Craig RG. Correlation of
parameters used to estimate monomer con-
version in a light-cured composite. J Dent Res
1988;67:932-7.
21.Rueggeberg FA, Hashinger DT, Fairhurst CW.
Calibration of FTIR conversion analysis of
contemporary dental resin composites. Dent
Mater 1990;6:241-9.
22.Ruyter IE. Methacrylate-based polymeric
dental materials: conversion and related
properties. Summary and review. Acta Odon-
tol Scand 1982;40:359-76.
23.Ruyter IE. Unpolymerized surface layers on
sealants. Acta Odontol Scand 1981;39:27-
32.
24.Ruyter IE, Svendsen SA. Remaining methacry-
late groups in composite restorative materials.
Acta Odontol Scand 1978;36:75-82.
25.Ferracane JL, Berge HX, Condon JR. In vitro
aging of dental composites in water--effect
of degree of conversion, filler volume, and
filler/matrix coupling. J Biomed Mater Res
1998;42:465-72.
26.Braga RR, Ferracane JL. Contraction stress
related to degree of conversion and reaction
kinetics. J Dent Res 2002;81:114-8.
27.Barron DJ, Rueggeberg FA, Schuster GS. A
comparison of monomer conversion and
inorganic filler content in visible light-cured
denture resins. Dent Mater 1992;8:274-7.
28.Rueggeberg FA, Caughman WF. The influence
of light exposure on polymerization of dual-
cure resin cements. Oper Dent 1993;18:48-
55.
29.Paul SJ, Leach M, Rueggeberg FA, Pashley
DH. Effect of water content on the physi-
cal properties of model dentine primer and
bonding resins. J Dent 1999;27:209-14.
30.Lee IB, An W, Chang J, Um CM. Influence of
ceramic thickness and curing mode on the po-
lymerization shrinkage kinetics of dual-cured
resin cements. Dent Mater 2008;24:1141-7.
Corresponding author:
Dr Cesar AG Arrais
Department of Operative Dentistry, School of
Dentistry
University of Guarulhos
R. Dr. Nilo Peanha, 81, Predio U 6 Andar
Centro
Guarulho, Sao Paulo
BRAZIL
CEP: 07011-040
Fax: 55-11-64641758
E-mail: cesararrais@yahoo.com.br
Acknowledgment
The authors thank Bisco, Inc, Kerr Corp,
Pentron, Inc, Dentsply Caulk, and 3M ESPE
for providing all restorative materials, and
the Medical College of Georgia School of
Dentistry, Augusta, Ga, for allowing the use of
facilities and providing all required equipment
to perform the study.
Copyright 2009 by the Editorial Council for
The Journal of Prosthetic Dentistry.
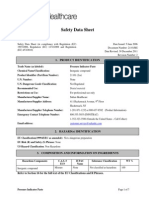
Diagnosing denture problems using
pressure-indicating media
Robert W. Loney, DMD, MS,
a
and Mark E. Knechtel, DDS
b
Faculty of Dentistry, Dalhousie University, Halifax, Nova Scotia
a
Professor and Head, Division of Removable Prosthodontics.
b
Instructor and Head, Division of Comprehensive Care.
Pressure-indicating media have
long been advocated for use in di-
agnosing problems with dentures at
insertion and denture adjustment
appointments.
1-8
Typically, pressure
indicators are used to identify prob-
lems related to impingement, exten-
sion, and/or width of prostheses.
8
Although patient input is useful in
identifying the general location of sore
spots, patients often cannot precisely
pinpoint the location of irritations.
9,10
Therefore, some authors
5,9
advocate
that a denture base should never be
modified without first using media to
identify specific areas requiring ad-
justment.
While primarily used to locate ar-
eas on the denture base that cause
pressure and pain,
8
pressure-indi-
cating media have diverse applica-
tions for identification of a variety of
denture-related problems.
5
Pressure-
indicating media can be nonsetting
and cream-based (Pressure Indicator
Paste; Mizzy, Inc, Cherry Hill, NJ),
nonsetting aerosol powders (Occlude;
Pascal Intl, Inc, Bellevue, Wash),
or media that polymerize (typically
catalyst/base elastomers such as Fit
Checker; GC Corp, Tokyo, Japan).
The purpose of this article is to
provide guidelines for optimal use of
the media, and to identify alternative
applications for consideration in daily
practice.
Pressure-indicating media have more diverse applications than merely the identification of areas on the denture base
that cause mucosal pressure and pain. The purpose of this article is to provide guidelines for optimal use of the media
and to identify alternative uses that could be considered in daily practice. (J Prosthet Dent 2009;101:137-141)
TECHNIQUE
1. Prior to applying media, remove
any obvious spicules or sharp projec-
tions from the denture, to minimize
patient discomfort.
9
2. Evaluate the denture base adap-
tation with pressure-indicating media
prior to occlusal adjustments, as al-
terations in the base adaptation can
alter the occlusal contacts.
3
3. Dry the denture before the ap-
plication of media,
6,9
so that the
material will adhere to the denture
surface. However, leave the oral mu-
cosa moist, so that the paste does not
adhere to it. Instruct patients with a
dry mouth to rinse with water and/or
spray the paste-covered denture with
water prior to placement intraorally.
1
Note that spraying the paste-covered
denture with air-water aerosol is ef-
fective. After removal from the oral
cavity, ensure that the media is not
adhering to tissues and pulling off the
base, creating a false positive for ex-
cessive pressure.
4. Use the correct amount of mate-
rial. For cream types, apply sufficient
material so that the base appears to
be primarily the color of the media,
as too little or too much material will
make interpretation more difficult.
4,5
Use a stiff brush to place pronounced
streaks in the material (Fig. 1).
1,3,6,11
5. For polymerizing materials, use
as thin a layer as possible to complete-
ly obscure the underlying denture.
Do not place streaks in elastomeric
materials. Place both types of media
on the intaglio side of the prosthesis
and over the flanges to evaluate for
proper extension or frenal impinge-
ments (Fig. 2). Seat dentures with
polymerization-type materials before
the start of polymerization, so that
the development of increased viscos-
ity will not prevent complete seating
of the denture.
2
6. Insert the denture using mouth
mirrors to retract the commissures,
so that the material is not wiped
away from the denture during inser-
tion. If the entire prosthesis cannot
be placed without touching the lips or
cheeks, evaluate right and left quad-
rants separately,
8
and/or evaluate the
denture base and denture peripheries
separately.
7. When seating the prosthesis
to verify tissue adaptation, use light
pressure initially to ensure patient
comfort.
6
Subsequently, apply firm
pressure in the area of the first molars
or instruct the patient to close with
firm pressure on cotton rolls over the
posterior teeth.
1,3,4,9,11
Do not allow
occlusal contacts, which can cause
tipping of the denture and a change
in the distribution of pressure.
4,7,9,11
8. If manual pressure is used, apply
it as firmly as possible,
4
as increased
pressure tends to increase the flow of
indicator media.
7
Do not apply pres-
138 Volume 101 Issue 2
The Journal of Prosthetic Dentistry
139 February 2009
Looney and Knechtel Looney and Knechtel
3 Areas with streaks remaining in paste have not con-
tacted tissue (N). Areas of paste with no streaks represent
acceptable contact (C). Areas without paste represent
areas of tissue impingement (I).
4 Slight flange overextension in retrozygomal area (ar-
rows) caused displacement of denture during function.
Cream-type media failed to reveal overextension.
5 Undercut areas will cause paste to be wiped off and
will appear to need adjustment. Use caution in these
areas.
6 Use of indicating medium for adjustment of hamular
notch areas is critical, as removal of acrylic resin in incor-
rect areas can result in breach of posterior palatal seal,
resulting in decreased retention.
7 Use indicating medium on nonbearing surfaces of
dentures to disclose problems such as impingement by
coronoid process in lateral excursions. Interferences can
cause both pain and loosening of dentures.
sure on the palatal portion of a max-
illary denture, as functional loading
does not occur in this location.
3
9. Exert pressure perpendicular to
the occlusal plane unless evaluating
the pressure pattern when the den-
ture is moving.
9
Do not move or tip
the denture or allow it to shift when
assessing normal denture base fit.
5
10. To evaluate flange extensions,
stabilize the denture over the occlus-
al surfaces of the teeth to prevent it
from moving while the patient makes
functional movements,
12
or while the
clinician manipulates the cheeks or
lips,
8
to detect overextensions in areas
of the moveable mucosa and frena,
which typically do not displace media
as easily as firmer tissues.
11. To interpret nonsetting pastes,
examine the denture for 3 distinct pat-
terns in the media: areas where streaks
remain, representing areas where
there has been no contact with tis-
sues; areas with paste but no streaks,
where there has been acceptable con-
tact; and areas without paste, which
normally suggest excessive pressure or
impingement (Fig. 3).
3,5,6
12. For polymerizing-type pastes,
areas of excess pressure will appear
as uncovered, or more lightly covered,
with media (Fig. 4). Although nonpo-
lymerizing pastes have been found to
be more accurate in some situations,
2
use media of different thicknesses
7
or
viscosities to identify problem areas
that might not be identified by anoth-
er media (Fig. 4).
13. Use caution when interpret-
ing lack of paste surrounding tissue
undercuts (Fig. 5).
9,11
Note that when
the denture moves over an undercut,
paste will normally be removed from
the denture.
9,13
Adjust the undercut
area only when there are signs or
symptoms of excess pressure or tissue
impingement. Similarly, expect slight-
ly more pressure on primary bearing
areas and do not adjust these areas
unnecessarily.
1,11
14. Note that commonly adjusted
areas of complete dentures include
the incisive papilla,
8
malar process
of the zygoma,
9,13
median palatal
raphe,
14
posterior palatal seal area,
9
hamular notch
8
(Fig. 6), pterygoman-
dibular raphe, mylohyoid ridge,
8,9,12
border of the retromylohyoid space,
8
distobuccal border of the maxillary
9,13
and mandibular
8,9
dentures, bony
prominences
8,14
or spicules, mental
formina,
9
buccal shelves,
9
and frenal
attachments.
8,9
15. Use pressure-indicating media
to detect and adjust other areas on
the oral, rather than the intaglio, sur-
face of a prosthesis. Note that func-
tional impingements of the coronoid
process against the distobuccal sur-
face of the denture
8,9,14
(Fig. 7), bulky
buccal contours
8
(Fig. 8), and teeth
placed too far buccally into the ves-
tibule (Fig. 8) can be identified using
pressure-indicating media.
9
16. Diagnose speech problems,
when possible, with palatograms,
using paste and spray-type pres-
sure-indicating media to diagnose
tongue contact areas on the denture
palate.
14,15
Instruct the patient to re-
peat problematic sounds with the
media covering the palate. Note that
different sounds result in different
contact patterns
15,16
(Fig. 9), which
can be modified by selective removal
from or additions to the palatal con-
tour. Note that the registration of the
tongue contact area on the palate us-
ing paste-type media may sometimes
require numerous repetitions of pho-
netic phrases before the registrations
are easy to interpret.
17. After identifying areas requir-
ing modification, adjust the denture
with an acrylic bur of appropriate size
and shape (H79E, H351E, H261E,
H251E; Brasseler USA, Savannah,
Ga). After adjustment, reapply me-
dia to ensure that the adjustment has
been effective or to determine if other
areas require modification.
8
18. For cream-type media, use an
air syringe to blow off as much of the
adjustment debris as possible, then
wipe away
6
any remaining debris in
the cream, prior to reapplying paste
with streaks.
1 Coat denture with enough paste so base is primarily
color of medium, with streaks in paste as on left. Too little
(upper right) or too much (lower right) can make inter-
pretation more difficult.
2 Apply paste well over flange edge onto buccal surface.
Lines of burn-through on flanges often indicate over-
extended or overcontoured areas. Note double line of
burn-through on facet where denture has already been
adjusted.
138 Volume 101 Issue 2
The Journal of Prosthetic Dentistry
139 February 2009
Looney and Knechtel Looney and Knechtel
3 Areas with streaks remaining in paste have not con-
tacted tissue (N). Areas of paste with no streaks represent
acceptable contact (C). Areas without paste represent
areas of tissue impingement (I).
4 Slight flange overextension in retrozygomal area (ar-
rows) caused displacement of denture during function.
Cream-type media failed to reveal overextension.
5 Undercut areas will cause paste to be wiped off and
will appear to need adjustment. Use caution in these
areas.
6 Use of indicating medium for adjustment of hamular
notch areas is critical, as removal of acrylic resin in incor-
rect areas can result in breach of posterior palatal seal,
resulting in decreased retention.
7 Use indicating medium on nonbearing surfaces of
dentures to disclose problems such as impingement by
coronoid process in lateral excursions. Interferences can
cause both pain and loosening of dentures.
sure on the palatal portion of a max-
illary denture, as functional loading
does not occur in this location.
3
9. Exert pressure perpendicular to
the occlusal plane unless evaluating
the pressure pattern when the den-
ture is moving.
9
Do not move or tip
the denture or allow it to shift when
assessing normal denture base fit.
5
10. To evaluate flange extensions,
stabilize the denture over the occlus-
al surfaces of the teeth to prevent it
from moving while the patient makes
functional movements,
12
or while the
clinician manipulates the cheeks or
lips,
8
to detect overextensions in areas
of the moveable mucosa and frena,
which typically do not displace media
as easily as firmer tissues.
11. To interpret nonsetting pastes,
examine the denture for 3 distinct pat-
terns in the media: areas where streaks
remain, representing areas where
there has been no contact with tis-
sues; areas with paste but no streaks,
where there has been acceptable con-
tact; and areas without paste, which
normally suggest excessive pressure or
impingement (Fig. 3).
3,5,6
12. For polymerizing-type pastes,
areas of excess pressure will appear
as uncovered, or more lightly covered,
with media (Fig. 4). Although nonpo-
lymerizing pastes have been found to
be more accurate in some situations,
2
use media of different thicknesses
7
or
viscosities to identify problem areas
that might not be identified by anoth-
er media (Fig. 4).
13. Use caution when interpret-
ing lack of paste surrounding tissue
undercuts (Fig. 5).
9,11
Note that when
the denture moves over an undercut,
paste will normally be removed from
the denture.
9,13
Adjust the undercut
area only when there are signs or
symptoms of excess pressure or tissue
impingement. Similarly, expect slight-
ly more pressure on primary bearing
areas and do not adjust these areas
unnecessarily.
1,11
14. Note that commonly adjusted
areas of complete dentures include
the incisive papilla,
8
malar process
of the zygoma,
9,13
median palatal
raphe,
14
posterior palatal seal area,
9
hamular notch
8
(Fig. 6), pterygoman-
dibular raphe, mylohyoid ridge,
8,9,12
border of the retromylohyoid space,
8
distobuccal border of the maxillary
9,13
and mandibular
8,9
dentures, bony
prominences
8,14
or spicules, mental
formina,
9
buccal shelves,
9
and frenal
attachments.
8,9
15. Use pressure-indicating media
to detect and adjust other areas on
the oral, rather than the intaglio, sur-
face of a prosthesis. Note that func-
tional impingements of the coronoid
process against the distobuccal sur-
face of the denture
8,9,14
(Fig. 7), bulky
buccal contours
8
(Fig. 8), and teeth
placed too far buccally into the ves-
tibule (Fig. 8) can be identified using
pressure-indicating media.
9
16. Diagnose speech problems,
when possible, with palatograms,
using paste and spray-type pres-
sure-indicating media to diagnose
tongue contact areas on the denture
palate.
14,15
Instruct the patient to re-
peat problematic sounds with the
media covering the palate. Note that
different sounds result in different
contact patterns
15,16
(Fig. 9), which
can be modified by selective removal
from or additions to the palatal con-
tour. Note that the registration of the
tongue contact area on the palate us-
ing paste-type media may sometimes
require numerous repetitions of pho-
netic phrases before the registrations
are easy to interpret.
17. After identifying areas requir-
ing modification, adjust the denture
with an acrylic bur of appropriate size
and shape (H79E, H351E, H261E,
H251E; Brasseler USA, Savannah,
Ga). After adjustment, reapply me-
dia to ensure that the adjustment has
been effective or to determine if other
areas require modification.
8
18. For cream-type media, use an
air syringe to blow off as much of the
adjustment debris as possible, then
wipe away
6
any remaining debris in
the cream, prior to reapplying paste
with streaks.
1 Coat denture with enough paste so base is primarily
color of medium, with streaks in paste as on left. Too little
(upper right) or too much (lower right) can make inter-
pretation more difficult.
2 Apply paste well over flange edge onto buccal surface.
Lines of burn-through on flanges often indicate over-
extended or overcontoured areas. Note double line of
burn-through on facet where denture has already been
adjusted.
140 Volume 101 Issue 2
The Journal of Prosthetic Dentistry
141 February 2009
Looney and Knechtel Looney and Knechtel
nies a pressure spot, do not ask the
patient if the adjustment has made a
problem better, as the most likely re-
sponse will be yes. Rather, ask an un-
biased question, such as, How does
that feel? Then, if the patient states
that the problem feels better, ask
the patient to rate the improvement in
terms of a percentage.
5
Note that the
patient should rate the improvement
in comfort at close to 100% when the
adjustment is complete, and, if the
patient does not, further adjustment
is most likely warranted.
5
SUMMARY
Use of an indicating medium is one
of several strategies that clinicians can
employ for improving diagnosis and
correction of denture-related prob-
lems. Denture adjustments are more
accurate and effective when made
using an indicating medium. The
authors recommend that the use of
pressure-indicating media for adjust-
ing dentures should become routine.
REFERENCES
1. Carr AB, McGivney GP, Brown DT. Mc-
Crackens removable partial prosthodontics.
11th ed. St. Louis: Mosby; 2004. p. 363-72.
2. Firtell DN, Arnett WS, Holmes JB. Pressure
indicators for removable prosthodontics. J
Prosthet Dent 1985;54:226-9.
3. Greenwood AH, Firtell DN. Pressure
indicators-a useful diagnostic aid. Quintes-
sence Int 1985;16:531-3.
4. Jankelson B. Adjustment of dentures at time
of insertion and alterations to compen-
sate for tissue change. J Am Dent Assoc
1962;64:521-31.
5. Loney R. Diagnosing denture pain:
principles and practice. J Can Dent Assoc
2006;72:137-41.
6. Phoenix RD, Cagna DR, DeFreest CF, Stew-
art KL. Stewarts clinical removable partial
prosthodontics. 3rd ed. Chicago: Quintes-
sence; 2003. p. 431-7.
7. Stevenson-Moore P, Daly CH, Smith DE.
Indicator pastes: their behavior and use. J
Prosthet Dent 1979;41:258-65.
8. Zarb GA, Bolender CL, Eckert SE, Fenton
AH, Jacob, RF, Mericske-Stern R. Prost-
hodontic treatment for edentulous patients:
complete dentures and implant-supported
prostheses. 12th ed. St. Louis: Mosby; 2003.
p. 402-26.
9. Levin B. Impressions for complete dentures.
Chicago: Quintessence: 1984. p. 162-80.
10.Yeoman LR, Beyak BL. Patients ability to
localize adjustment sites on the mandibular
denture. J Prosthet Dent 1995;73:542-7.
11.Renner RP, Boucher LJ. Removable partial
dentures. Chicago: Quintessence; 1987. p.
335-45.
12.Boucher LJ. Insertion adjustment of denture
base surface contacting the mylohyoid ridge.
J Prosthet Dent 1992;67:900-1.
13.Rodegerdts CR. The relationship of pres-
sure spots in complete denture impressions
with mucosal irritations. J Prosthet Dent
1964;14:1040-9.
14.Grant AA, Heath JR, McCord JF. Complete
prosthodontics: problems, diagnosis and
management. London: Wolfe: 1994. p.
33-87.
15.Farley DW, Jones JD, Cronin RJ. Palatogram
assessment of maxillary complete dentures. J
Prosthodont 1998;7:84-90.
16.Kong HJ, Hansen CA. Customizing palatal
contours of a denture to improve speech in-
telligibility. J Prosthet Dent 2008;99:243-8.
Corresponding author:
Dr Robert W. Loney
Division of Removable Prosthodontics
Department of Dental Clinical Sciences
Faculty of Dentistry, Dalhousie University
5981 University Ave
Halifax, NS B3H 1W2
CANADA
Fax: 902-494-1662
E-mail: robert.loney@dal.ca
Copyright 2009 by the Editorial Council for
The Journal of Prosthetic Dentistry.
19. For elastomeric media, mark
the exposed areas of the denture us-
ing a dampened tip of a disinfected
red or blue pencil, so that the area re-
mains indicated, should the polymer-
ized elastomer catch the bur and tear
or pull away from the denture.
20. Adjustment is complete when
the area being evaluated has a rela-
tively even pattern of contact (Fig. 10;
compare with Fig. 3). Note that it is
often not possible to achieve perfect
adaptation of the base.
9
If interpre-
tation of the indicating media is dif-
ficult, avoid adjustment until signs or
symptoms appear, so as not to over-
adjust the denture.
6,9
21. When discomfort accompa-
8 A, External contours of dentures can be evaluated with media. Bulky gingival contours around teeth have no
paste. B, After functional movements, bulky flanges have no paste. Thin these areas, if patient has problems with
loosening or discomfort.
9 A, Contour of palate can affect phonetics. Palatogram represents correct pattern for S sounds with minimal
loss of pressure media behind central incisors. B, Palatogram represents correct pattern for T, D, N, J, and
Ch sounds. Addition of wax or removal of palatal base material can be performed to modify contact areas and
improve phonetics.
10 Well-adjusted denture base. Areas of tissue inflammation that do not correlate to areas of
burn-through are most likely caused by tilting of dentures, possibly due to occlusal problems.
A B
A B
Noteworthy Abstracts of the Current Literature
Single-tooth replacement in the anterior maxilla by means of immediate implantation
and provisionalization: A review
De Rouck T, Collys K, Cosyn J.
Int J Oral Maxillofac Implants 2008;23:897-904.
Objectives: The objective of this study was to assess to what extent the outcome of immediate implantation and pro-
visionalization for replacing single maxillary teeth in the esthetic zone is favorable and predictable from biologic and
esthetic points of view.
Material and Methods: An electronic search (MEDLINE and Cochrane Oral Health Group Specialized Trials Register)
and a manual search were performed to detect studies concerning maxillary single-tooth replacements by means of
dental implants immediately placed into fresh extraction sockets and provisionalized within the first 24 hours. Only
full-text reports on clinical studies published in English up to June 2006 were included. Case reports and reviews on
the topic of interest were excluded.
Results: Eleven studies were selected. Based on a qualitative data analysis, implant survival and even management of
papilla levels seem predictable following immediate implantation and provisionalization. However, maintaining the
midfacial gingival margin may be more problematic, since postextraction bone remodeling and therefore marginal
gingival changes will occur irrespective of the timing of the placement of an implant. The long-term impact of this
remodeling is currently unclear and needs to be elucidated in future research.
Conclusion: The clinician is recommended to be reserved when considering immediate implant placement and pro-
visionalization for replacing single maxillary teeth in the anterior zone. At the very least, a number of guidelines and
prerequisites need to be taken into consideration.
Reprinted with permission of Quintessence Publishing.
140 Volume 101 Issue 2
The Journal of Prosthetic Dentistry
141 February 2009
Looney and Knechtel Looney and Knechtel
nies a pressure spot, do not ask the
patient if the adjustment has made a
problem better, as the most likely re-
sponse will be yes. Rather, ask an un-
biased question, such as, How does
that feel? Then, if the patient states
that the problem feels better, ask
the patient to rate the improvement in
terms of a percentage.
5
Note that the
patient should rate the improvement
in comfort at close to 100% when the
adjustment is complete, and, if the
patient does not, further adjustment
is most likely warranted.
5
SUMMARY
Use of an indicating medium is one
of several strategies that clinicians can
employ for improving diagnosis and
correction of denture-related prob-
lems. Denture adjustments are more
accurate and effective when made
using an indicating medium. The
authors recommend that the use of
pressure-indicating media for adjust-
ing dentures should become routine.
REFERENCES
1. Carr AB, McGivney GP, Brown DT. Mc-
Crackens removable partial prosthodontics.
11th ed. St. Louis: Mosby; 2004. p. 363-72.
2. Firtell DN, Arnett WS, Holmes JB. Pressure
indicators for removable prosthodontics. J
Prosthet Dent 1985;54:226-9.
3. Greenwood AH, Firtell DN. Pressure
indicators-a useful diagnostic aid. Quintes-
sence Int 1985;16:531-3.
4. Jankelson B. Adjustment of dentures at time
of insertion and alterations to compen-
sate for tissue change. J Am Dent Assoc
1962;64:521-31.
5. Loney R. Diagnosing denture pain:
principles and practice. J Can Dent Assoc
2006;72:137-41.
6. Phoenix RD, Cagna DR, DeFreest CF, Stew-
art KL. Stewarts clinical removable partial
prosthodontics. 3rd ed. Chicago: Quintes-
sence; 2003. p. 431-7.
7. Stevenson-Moore P, Daly CH, Smith DE.
Indicator pastes: their behavior and use. J
Prosthet Dent 1979;41:258-65.
8. Zarb GA, Bolender CL, Eckert SE, Fenton
AH, Jacob, RF, Mericske-Stern R. Prost-
hodontic treatment for edentulous patients:
complete dentures and implant-supported
prostheses. 12th ed. St. Louis: Mosby; 2003.
p. 402-26.
9. Levin B. Impressions for complete dentures.
Chicago: Quintessence: 1984. p. 162-80.
10.Yeoman LR, Beyak BL. Patients ability to
localize adjustment sites on the mandibular
denture. J Prosthet Dent 1995;73:542-7.
11.Renner RP, Boucher LJ. Removable partial
dentures. Chicago: Quintessence; 1987. p.
335-45.
12.Boucher LJ. Insertion adjustment of denture
base surface contacting the mylohyoid ridge.
J Prosthet Dent 1992;67:900-1.
13.Rodegerdts CR. The relationship of pres-
sure spots in complete denture impressions
with mucosal irritations. J Prosthet Dent
1964;14:1040-9.
14.Grant AA, Heath JR, McCord JF. Complete
prosthodontics: problems, diagnosis and
management. London: Wolfe: 1994. p.
33-87.
15.Farley DW, Jones JD, Cronin RJ. Palatogram
assessment of maxillary complete dentures. J
Prosthodont 1998;7:84-90.
16.Kong HJ, Hansen CA. Customizing palatal
contours of a denture to improve speech in-
telligibility. J Prosthet Dent 2008;99:243-8.
Corresponding author:
Dr Robert W. Loney
Division of Removable Prosthodontics
Department of Dental Clinical Sciences
Faculty of Dentistry, Dalhousie University
5981 University Ave
Halifax, NS B3H 1W2
CANADA
Fax: 902-494-1662
E-mail: robert.loney@dal.ca
Copyright 2009 by the Editorial Council for
The Journal of Prosthetic Dentistry.
19. For elastomeric media, mark
the exposed areas of the denture us-
ing a dampened tip of a disinfected
red or blue pencil, so that the area re-
mains indicated, should the polymer-
ized elastomer catch the bur and tear
or pull away from the denture.
20. Adjustment is complete when
the area being evaluated has a rela-
tively even pattern of contact (Fig. 10;
compare with Fig. 3). Note that it is
often not possible to achieve perfect
adaptation of the base.
9
If interpre-
tation of the indicating media is dif-
ficult, avoid adjustment until signs or
symptoms appear, so as not to over-
adjust the denture.
6,9
21. When discomfort accompa-
8 A, External contours of dentures can be evaluated with media. Bulky gingival contours around teeth have no
paste. B, After functional movements, bulky flanges have no paste. Thin these areas, if patient has problems with
loosening or discomfort.
9 A, Contour of palate can affect phonetics. Palatogram represents correct pattern for S sounds with minimal
loss of pressure media behind central incisors. B, Palatogram represents correct pattern for T, D, N, J, and
Ch sounds. Addition of wax or removal of palatal base material can be performed to modify contact areas and
improve phonetics.
10 Well-adjusted denture base. Areas of tissue inflammation that do not correlate to areas of
burn-through are most likely caused by tilting of dentures, possibly due to occlusal problems.
A B
A B
Noteworthy Abstracts of the Current Literature
Single-tooth replacement in the anterior maxilla by means of immediate implantation
and provisionalization: A review
De Rouck T, Collys K, Cosyn J.
Int J Oral Maxillofac Implants 2008;23:897-904.
Objectives: The objective of this study was to assess to what extent the outcome of immediate implantation and pro-
visionalization for replacing single maxillary teeth in the esthetic zone is favorable and predictable from biologic and
esthetic points of view.
Material and Methods: An electronic search (MEDLINE and Cochrane Oral Health Group Specialized Trials Register)
and a manual search were performed to detect studies concerning maxillary single-tooth replacements by means of
dental implants immediately placed into fresh extraction sockets and provisionalized within the first 24 hours. Only
full-text reports on clinical studies published in English up to June 2006 were included. Case reports and reviews on
the topic of interest were excluded.
Results: Eleven studies were selected. Based on a qualitative data analysis, implant survival and even management of
papilla levels seem predictable following immediate implantation and provisionalization. However, maintaining the
midfacial gingival margin may be more problematic, since postextraction bone remodeling and therefore marginal
gingival changes will occur irrespective of the timing of the placement of an implant. The long-term impact of this
remodeling is currently unclear and needs to be elucidated in future research.
Conclusion: The clinician is recommended to be reserved when considering immediate implant placement and pro-
visionalization for replacing single maxillary teeth in the anterior zone. At the very least, a number of guidelines and
prerequisites need to be taken into consideration.
Reprinted with permission of Quintessence Publishing.
You might also like
- A Large Rhinolith and Importance of Nasal Endoscopy: A Case ReportDocument3 pagesA Large Rhinolith and Importance of Nasal Endoscopy: A Case ReportIOSRjournalNo ratings yet
- Oral Leukoplakia Management Using Diode Laser A Case Report (Chaudri DKK, 2019)Document3 pagesOral Leukoplakia Management Using Diode Laser A Case Report (Chaudri DKK, 2019)Rani PutriNo ratings yet
- Nanocrystallinae Hap From Egg ShellDocument4 pagesNanocrystallinae Hap From Egg Shellcollin samuelNo ratings yet
- Management of Alveolar Ridge ResorptionDocument29 pagesManagement of Alveolar Ridge Resorptionفواز نميرNo ratings yet
- Impression techniques for RPDDocument29 pagesImpression techniques for RPDمؤمل رياض سعد كاظمNo ratings yet
- Polishing and TrimmingDocument9 pagesPolishing and TrimmingKimberly RodilNo ratings yet
- Cantor and Curtis ClassificationDocument4 pagesCantor and Curtis ClassificationMuhammad AwaisNo ratings yet
- Record BlocksDocument59 pagesRecord BlocksahmedNo ratings yet
- Maxillofacial Prosthesis materials comparisonDocument52 pagesMaxillofacial Prosthesis materials comparisonShipra SinghNo ratings yet
- Provisional Restoration: in Fixed ProsthodonticsDocument48 pagesProvisional Restoration: in Fixed ProsthodonticsAhmed Hassan ElFananNo ratings yet
- Complete Denture Cast Preparation GuideDocument18 pagesComplete Denture Cast Preparation Guidefitsum100% (1)
- Infection Control in Fixed Prosthodontics: Prepared & Presented byDocument57 pagesInfection Control in Fixed Prosthodontics: Prepared & Presented byaloooooooshNo ratings yet
- Bruxism and Prostho TreatmentDocument10 pagesBruxism and Prostho Treatmentdorasani99No ratings yet
- Relining and RebasingDocument5 pagesRelining and RebasingMarwaAmerNo ratings yet
- Complete Denture Impression 101Document3 pagesComplete Denture Impression 101DentalLearningNo ratings yet
- Type I: Luting Agents That Include Permanent and Temporary Cements. Type II: Restorative Applications. Type III: Liner or Base ApplicationsDocument5 pagesType I: Luting Agents That Include Permanent and Temporary Cements. Type II: Restorative Applications. Type III: Liner or Base ApplicationsSony RajbhandariNo ratings yet
- Root Completion Times for Primary and Permanent TeethDocument35 pagesRoot Completion Times for Primary and Permanent TeethFaizan Ahmed50% (2)
- Gypsum Products Gypsum Products Gypsum Products Gypsum Products Gypsum ProductsDocument16 pagesGypsum Products Gypsum Products Gypsum Products Gypsum Products Gypsum ProductsZHAREIGHNEILE C. MAMOLO100% (1)
- Anterior Deprogramming Device Fabrication Using A Thermoplastic Material PDFDocument3 pagesAnterior Deprogramming Device Fabrication Using A Thermoplastic Material PDFruli nurul amanNo ratings yet
- Overdenture 140503222227 Phpapp01Document107 pagesOverdenture 140503222227 Phpapp01TatsamYadavNo ratings yet
- Prosthodontic Stents: March 2019Document28 pagesProsthodontic Stents: March 2019Ahmad WahabNo ratings yet
- Gingival Tissue RetractionDocument11 pagesGingival Tissue RetractionNaghman ZuberiNo ratings yet
- Impression Procedures in CD - KIRTI SHARMADocument42 pagesImpression Procedures in CD - KIRTI SHARMAKirti SharmaNo ratings yet
- My 3rd Seminar - DentinDocument25 pagesMy 3rd Seminar - DentinJon YorkNo ratings yet
- GENERAL PRINCIPLES OF SHADE SELECTION LDDocument3 pagesGENERAL PRINCIPLES OF SHADE SELECTION LDrasagna reddyNo ratings yet
- Relining and Rebasing Complete DenturesDocument28 pagesRelining and Rebasing Complete DenturesAan Mi'dad100% (1)
- Clasp DesignDocument11 pagesClasp DesignBibek RajNo ratings yet
- Arrangement of TeethDocument65 pagesArrangement of TeethIbrahim Ramadan Eltorky100% (1)
- Anatomical Landmarks - PCPDocument14 pagesAnatomical Landmarks - PCPSara Sultana0% (1)
- Recent Advances in DentistryDocument2 pagesRecent Advances in DentistrySudarsan SangeethaNo ratings yet
- Prostho (Compelte Denture) FINAL ANSWERSDocument95 pagesProstho (Compelte Denture) FINAL ANSWERSahead1234No ratings yet
- Dental WaxesDocument32 pagesDental Waxesjohn mwambuNo ratings yet
- Horizontal Posts PDFDocument6 pagesHorizontal Posts PDFaishwarya singhNo ratings yet
- Articulating PapersDocument48 pagesArticulating PapersMayank MalraNo ratings yet
- Wax Pattern Construction TechniquesDocument34 pagesWax Pattern Construction TechniquesMariam SherifNo ratings yet
- Implant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDocument7 pagesImplant Systems: Dr. Unjum Bashir, Dr. Manas Gupta, Dr. Ravish AhujaDr FarhatNo ratings yet
- 2012 Gingival RetractionDocument16 pages2012 Gingival RetractionMaria Mercedes LeivaNo ratings yet
- Complete Denture JourneyDocument30 pagesComplete Denture JourneysapnaNo ratings yet
- 5 - Calcium Hydroxide Vs Mineral Trioxide Aggregates For Partial Pulpotomy of Permanent Molars With Deep Caries PDFDocument6 pages5 - Calcium Hydroxide Vs Mineral Trioxide Aggregates For Partial Pulpotomy of Permanent Molars With Deep Caries PDFAbdul Rahman AlmishhdanyNo ratings yet
- Balanced Occlu HandoutDocument9 pagesBalanced Occlu HandoutMostafa FayadNo ratings yet
- Precision Attachments (2) PRDocument23 pagesPrecision Attachments (2) PRpriyaNo ratings yet
- Psychological factors for denture patientsDocument7 pagesPsychological factors for denture patientsPrateek MishraNo ratings yet
- Use of Polyethylene Ribbon To Create A Provisional Fixed Partial DentureDocument4 pagesUse of Polyethylene Ribbon To Create A Provisional Fixed Partial DentureAhmed AbdulazeezNo ratings yet
- Relining and Rebasing in Complete Dentures: Indian Dental AcademyDocument59 pagesRelining and Rebasing in Complete Dentures: Indian Dental AcademyNajeeb UllahNo ratings yet
- Preprosthetic Surgical ProceduresDocument57 pagesPreprosthetic Surgical ProceduresDentist Here100% (1)
- Posterior Palatal Seal ProsthoDocument64 pagesPosterior Palatal Seal ProsthoAmit BhargavNo ratings yet
- Components FPDDocument91 pagesComponents FPDKashish08No ratings yet
- Section 019 EstheticsDocument10 pagesSection 019 EstheticsMohammed LafiNo ratings yet
- A Review On Posterior Palatal SealDocument6 pagesA Review On Posterior Palatal SealTanmay Srivastava100% (1)
- A Hollow Bulb ObturatorDocument6 pagesA Hollow Bulb ObturatorrekabiNo ratings yet
- FINAL EXAM 2. Restorative Essay Questions and AnswersDocument15 pagesFINAL EXAM 2. Restorative Essay Questions and AnswerspaigenottNo ratings yet
- Recent Advances in Provisional RestorationsDocument6 pagesRecent Advances in Provisional RestorationsAngelia PratiwiNo ratings yet
- Checking and Verification of Crowns and Fixed ProsthesesDocument5 pagesChecking and Verification of Crowns and Fixed Prostheseskhaled alahmadNo ratings yet
- Applied Anatomy Related To Complete Denture-Maxilla MandibleDocument57 pagesApplied Anatomy Related To Complete Denture-Maxilla MandibleRen Jye ChongNo ratings yet
- Basic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionFrom EverandBasic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionNo ratings yet
- Fixed Orthodontic Appliances: A Practical GuideFrom EverandFixed Orthodontic Appliances: A Practical GuideRating: 1 out of 5 stars1/5 (1)
- Essential Tissue Healing of the Face and NeckFrom EverandEssential Tissue Healing of the Face and NeckRating: 5 out of 5 stars5/5 (2)
- MTA Sebagai Alternatif PSADocument7 pagesMTA Sebagai Alternatif PSArochirrephttoNo ratings yet
- Model Core Program Paper DentalDocument30 pagesModel Core Program Paper DentalrochirrephttoNo ratings yet
- Waterforlife PDFDocument44 pagesWaterforlife PDFhaseebNo ratings yet
- The Effect of Varying Diagnostic Thresholds Upon Clinical Caries Data For A Low Prevalence GroupDocument6 pagesThe Effect of Varying Diagnostic Thresholds Upon Clinical Caries Data For A Low Prevalence GrouprochirrephttoNo ratings yet
- Save Water SaveDocument2 pagesSave Water SaverochirrephttoNo ratings yet
- ProstoDocument7 pagesProstorochirrephttoNo ratings yet
- Pressure Indicator PasteDocument7 pagesPressure Indicator PasterochirrephttoNo ratings yet
- Anemia PeriodontitisDocument8 pagesAnemia PeriodontitisrochirrephttoNo ratings yet
- Pressure Indicator PasteDocument7 pagesPressure Indicator PasterochirrephttoNo ratings yet
- Pressure Indicator PasteDocument7 pagesPressure Indicator PasterochirrephttoNo ratings yet