Professional Documents
Culture Documents
Blood
Uploaded by
Himanshu BandilCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood
Uploaded by
Himanshu BandilCopyright:
Available Formats
Blood
The average adult has about five litres of blood living inside of their body,
coursing through their vessels, delivering essential elements, and removing
harmful wastes. Without blood, the human body would stop working.
Blood is the fluid of life, transporting oxygen from the lungs to body tissue and
carbon dioxide from body tissue to the lungs. Blood is the fluid of growth,
transporting nourishment from digestion and hormones from glands
throughout the body. Blood is the fluid of health, transporting disease fighting
substances to the tissue and waste to the kidneys.
Blood is a bodily fluid in animals that delivers necessary substances such as
nutrients and oxygen to the cells and transports metabolic waste products
away from those same cells.
Because it contains living cells, blood is alive. Red blood cells and white blood
cells are responsible for nourishing and cleansing the body. Since the cells are
alive, they too need nourishment.
Vitamins and Minerals keep the blood healthy. The blood cells have a definite
life cycle, just as all living organisms do. Approximately 55 percent of blood is
plasma, a straw-colored clear liquid. The liquid plasma carries the solid cells
and the platelets which help blood clot. Without blood platelets, you would
bleed to death.
When the human body loses a little bit of blood through a minor wound, the
platelets cause the blood to clot so that the bleeding stops. Because new blood
is always being made inside of your bones, the body can replace the lost blood.
When the human body loses a lot of blood through a major wound, that blood
has to be replaced through a blood transfusion from other people.
But everybody's blood is not the same. There are four different blood types.
Plus, your blood has Rh factors which make it even more unique. Blood
received through a transfusion must match your own. Patients who are
scheduled to have major surgery make autologous blood donations (donations
of their own blood) so that they have a perfect match.
In vertebrates, it is composed of blood cells suspended in blood plasma.
Plasma, which constitutes 55% of blood fluid, is mostly water (92% by
volume),
[1]
and contains dissipated proteins, glucose, mineral ions, hormones,
carbon dioxide (plasma being the main medium for excretory product
transportation), and blood cells themselves. Albumin is the main protein in
plasma, and it functions to regulate the colloidal osmotic pressure of blood.
The blood cells are mainly red blood cells (also called RBCs or erythrocytes)
and white blood cells, including leukocytes and platelets. The most abundant
cells in vertebrate blood are red blood cells. These contain hemoglobin, an
iron-containing protein, which facilitates transportation of oxygen by reversibly
binding to this respiratory gas and greatly increasing its solubility in blood. In
contrast, carbon dioxide is almost entirely transported extracellularly dissolved
in plasma as bicarbonate ion.
Vertebrate blood is bright red when its hemoglobin is oxygenated. Some
animals, such as crustaceans and mollusks, use hemocyanin to carry oxygen,
instead of hemoglobin. Insects and some mollusks use a fluid called
hemolymph instead of blood, the difference being that hemolymph is not
contained in a closed circulatory system. In most insects, this "blood" does not
contain oxygen-carrying molecules such as hemoglobin because their bodies
are small enough for their tracheal system to suffice for supplying oxygen.
Jawed vertebrates have an adaptive immune system, based largely on white
blood cells. White blood cells help to resist infections and parasites. Platelets
are important in the clotting of blood. Arthropods, using hemolymph, have
hemocytes as part of their immune system.
Blood is circulated around the body through blood vessels by the pumping
action of the heart. In animals with lungs, arterial blood carries oxygen from
inhaled air to the tissues of the body, and venous blood carries carbon dioxide,
a waste product of metabolism produced by cells, from the tissues to the lungs
to be exhaled.
Medical terms related to blood often begin with hemo- or hemato from the
Greek word (haima) for "blood". In terms of anatomy and histology, blood is
considered a specialized form of connective tissue, given its origin in the bones
and the presence of potential molecular fibres in the form of fibrinogen.
Blood Types: What's Your Type?
In some ways, every person's blood is the same. But, when analyzed under a
microscope, distinct differences are visible. In the early 20th century, an
Austrian scientist named Karl Landsteiner classified blood according to those
differences. He was awarded the Nobel Prize for his achievements.
Landsteiner observed two distinct chemical molecules present on the surface
of the red blood cells. He labelled one molecule "A" and the other molecule
"B." If the red blood cell had only "A" molecules on it, that blood was called
type A. If the red blood cell had only "B" molecules on it, that blood was called
type B. If the red blood cell had a mixture of both molecules, that blood was
called type AB. If the red blood cell had neither molecule, that blood was called
type O.
If two different blood types are mixed together, the blood cells may begin to
clump together in the blood vessels, causing a potentially fatal situation.
Therefore, it is important that blood types be matched before blood
transfusions take place. In an emergency, type O blood can be given because it
is most likely to be accepted by all blood types. However, there is still a risk
involved.
A person with type A blood can donate blood to a person with type A or type
AB. A person with type B blood can donate blood to a person with type B or
type AB. A person with type AB blood can donate blood to a person with type
AB only. A person with type O blood can donate to anyone.
A person with type A blood can receive blood from a person with type A or
type O. A person with type B blood can receive blood from a person with type
B or type O. A person with type AB blood can receive blood from anyone. A
person with type O blood can receive blood from a person with type O.
Because of these patterns, a person with type O blood is said to be a universal
donor. A person with type AB blood is said to be a universal receiver. In
general, however, it is still best to mix blood of matching types and Rh factors.
Blood Type Inheritance
Possibilities Based on Parents'
Types
PARENTAL COMBINATIONS
Possible Inheritances AB/AB AB/B AB/A AB/O B/B A/B A/A O/B O/A O/O
O no No no no yes yes yes yes yes yes
A yes Yes yes yes no yes yes no yes no
B yes Yes yes yes yes yes no yes no no
AB yes Yes yes no no yes no no no no
Blood Test
A blood test , also known as bloodwork, is a laboratory analysis performed on
a blood sample that is usually extracted from a vein in the arm using a needle,
or via fingerprick. Blood tests
[1]
(also referred to as blood work) are used to
determine physiological and biochemical states, such as disease, mineral
content, drug effectiveness, and organ function. They are also used in drug
tests.
Extraction
Venipuncture is useful as it is a minimally invasive way to obtain cells and
extracellular fluid (plasma) from the body for analysis. Since blood flows
throughout the body, acting as a medium for providing oxygen and nutrients,
and drawing waste products back to the excretory systems for disposal, the
state of the bloodstream affects, or is affected by, many medical conditions.
For these reasons, blood tests are the most commonly performed medical
tests.
[2]
If only a few drops of blood are needed, a fingerstick is performed instead of
drawing blood from a vein.
Phlebotomists, laboratory practitioners and nurses are those charged with
patient blood extraction. However, in special circumstances, and emergency
situations, paramedics and physicians sometimes extract blood. Also,
respiratory therapists are trained to extract arterial blood to examine arterial
blood gases.
TYPES OF BLOOD TEST
Biochemical analysis[edit]
A basic metabolic panel measures sodium, potassium, chloride, bicarbonate,
blood urea nitrogen (BUN), magnesium, creatinine, glucose, and sometimes
includes calcium. Blood tests focusing on cholesterol levels can determine LDL
and HDL cholesterol levels, as well as triglyceride levels.
Some blood tests, such as those that measure glucose, cholesterol, or for
determining the existence or lack of STD, require fasting (or no food
consumption) eight to twelve hours prior to the drawing of the blood sample.
For the majority of blood tests, blood is usually obtained from the patient's
vein. However, other specialized blood tests, such as the arterial blood gas,
require blood extracted from an artery. Blood gas analysis of arterial blood is
primarily used to monitor carbon dioxide and oxygen levels related to
pulmonary function, but it is also used to measure blood pH and bicarbonate
levels for certain metabolic conditions.
While the regular glucose test is taken at a certain point in time, the glucose
tolerance test involves repeated testing to determine the rate at which glucose
is processed by the body.
Molecular profiles
Protein electrophoresis (general techniquenot a specific test)
Western blot (general techniquenot a specific test)
Liver function tests
Polymerase chain reaction (DNA). DNA profiling is today possible with
even very small quantities of blood: this is commonly used in forensic
science, but is now also part of the diagnostic process of many disorders.
Northern blot (RNA)
Sexually transmitted diseases
Cellular evaluation
Full blood count (or "complete blood count")
Hematocrit and MCV ("mean corpuscular volume")
Erythrocyte sedimentation rate (ESR)
Cross-matching. Determination of blood type for blood transfusion or
transplants
Blood cultures are commonly taken if infection is suspected. Positive
cultures and resulting sensitivity results are often useful in guiding
medical treatment.
Future Alternatives
Saliva tests
In 2008, scientists announced that the more cost effective saliva testing could
eventually replace some blood tests, as saliva contains 20% of the proteins
found in blood.
Microemulsion
In February 2011 Canadian researchers announced a microchip for blood tests.
Dubbed a microemulsion, a droplet of blood captured inside a layer of another
substance. It can control the exact size and spacing of the droplets. The new
test could improve the efficiency, accuracy and speed of laboratory tests while
also doing it cheaply. The microchip costs $25, whereas the robotic dispensers
currently in use cost around $10,000.
In 2013, Theranos Corporation announced a partnership with Walgreens to
provide blood panels supporting nearly 200 tests, that require only a single
capsule-sized lab vial of blood. Results are available in less than four hours.
Blood is drawn with a finger stick, rather than a needle in the arm. The
diagnostic technology is integrated and cross-calibrated to ensure consistent
results.
SIMBAS
March 2011: A team of researchers from UC Berkeley, DCU and University of
Valparaso have developed lab-on-a-chip that can diagnose diseases within 10
minutes without the use of external tubing and extra components. It is called
Self-powered Integrated Microfluidic Blood Analysis System (SIMBAS). It uses
tiny trenches to separate blood cells from plasma (99 percent of blood cells
were captured during experiments). Researchers used plastic components, to
reduce manufacturing costs.
Functions -
Blood performs many important functions within the body including:
Supply of oxygen to tissues (bound to hemoglobin, which is carried in
red cells).
Supply of nutrients such as glucose, amino acids, and fatty acids
(dissolved in the blood or bound to plasma proteins (e.g., blood lipids).
Removal of waste such as carbon dioxide, urea, and lactic acid.
Immunological functions, including circulation of white blood cells, and
detection of foreign material by antibodies.
Coagulation, which is one part of the body's self-repair mechanism
(blood clotting after an open wound in order to stop bleeding).
Messenger functions, including the transport of hormones and the
signalling of tissue damage.
Regulation of body pH.
Regulation of core body temperature.
Hydraulic functions.
Blood is a constantly circulating fluid providing the body with nutrition, oxygen,
and waste removal. Blood is mostly liquid, with numerous cells and proteins
suspended in it, making blood "thicker" than pure water. The average person
has about 5 liters (more than a gallon) of blood.
A liquid called plasma makes up about half of the content of blood. Plasma
contains proteins that help blood to clot, transport substances through the
blood, and perform other functions. Blood plasma also contains glucose and
other dissolved nutrients.
About half of blood volume is composed of blood cells:
Red blood cells, which carry oxygen to the tissues.
Blood cells, which fight infections.
Platelets, smaller cells that help blood to clot.
Blood is conducted through blood vessels (arteries and veins). Blood is
prevented from clotting in the blood vessels by their smoothness, and the
finely tuned balance of clotting factors.
Blood Conditions -
Hemorrhage (bleeding): Blood leaking out of blood vessels may be
obvious, as from a wound penetrating the skin. Internal bleeding (such
as into the intestines or after a car accident) may not be immediately
apparent.
Hematoma: A collection of blood inside the body tissues. Internal
bleeding often causes a hematoma.
Leukemia: A form of blood cancer, in which white blood cells multiply
abnormally and circulate through the blood. The excessive large
numbers of white cells deposit in the body's tissues, causing damage.
Multiple myeloma: A form of blood cancer of plasma cells similar to
leukemia. Anemia, kidney failure and high blood calcium levels are
common in multiple myeloma.
Lymphoma: A form of blood cancer, in which white blood cells multiply
abnormally inside lymph nodes and other tissues. The enlarging tissues,
and disruption of blood's functions, can eventually cause organ failure.
Anemia: An abnormally low number of red blood cells in the blood.
Fatigue and breathlessness can result, although anemia often causes no
noticeable symptoms.
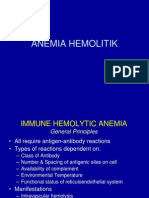
Hemolytic anemia: Anemia caused by rapid bursting of large numbers of
red blood cells (haemolysis). An immune system malfunction is one
cause.
Hemochromatosis: A disorder causing excessive levels of iron in the
blood. The iron deposits in the liver, pancreas and other organs, causing
liver problems and diabetes.
Sickle cell disease: A genetic condition in which red blood cells
periodically lose their proper shape (appearing like sickles, rather than
discs). The deformed blood cells deposit in tissues, causing pain and
organ damage.
Bacteremia: Bacterial infection of the blood. Blood infections are
serious, and often require hospitalization and continuous antibiotic
infusion into the veins.
Malaria: Infection of red blood cells by Plasmodium, a parasite
transmitted by mosquitos. Malaria causes episodic fevers, chills, and
potentially organ damage.
Thrombocytopenia: Abnormally low numbers of platelets in the blood.
Severe thrombocytopenia may lead to bleeding.
Leukopenia: Abnormally low numbers of white blood cells in the blood.
Leukopenia can result in difficulty fighting infections.
Disseminated intravascular coagulation (DIC): An uncontrolled process of
simultaneous bleeding and clotting in very small blood vessels. DIC
usually results from severe infections or cancer.
Hemophilia: An inherited (genetic) deficiency of certain blood clotting
proteins. Frequent or uncontrolled bleeding can result from hemophilia.
Hypercoaguable state: Numerous conditions can result in the blood
being prone to clotting. A heart attack, stroke, or blood clots in the legs
or lungs can result.
Polycythemia: Abnormally high numbers of red blood cells in the blood.
Polycythemia can result from low blood oxygen levels, or may occur as a
cancer-like condition.
Deep venous thrombosis (DVT): A blood clot in a deep vein, usually in
the leg. DVTs are dangerous because they may become dislodged and
travel to the lungs, causing a pulmonary embolism (PE).
Myocardial infarction (MI): Commonly called a heart attack, a myocardial
infarction occurs when a sudden blood clot develops in one of the
coronary arteries, which supply blood to the heart.
Effect of environmental effect on Blood
The effects of environmental and lifestyle factors on blood pressure and
the intermediary role of the sympathetic nervous system.
Essential hypertension is thought to be caused by both genetic and
environmental factors, with varying combinations in different individuals.
Proposed environmental factors include exposure to chronic stress, obesity
alcohol and salt intake, and physical inactivity. The prevalence of hypertension
is related to social factors such as urbanization and education. Several studies,
conducted both experimentally in animals and observationally in people, have
suggested that chronic social conflict is associated with higher blood pressure.
Ambulatory monitoring has shown that most people have their highest
pressures during working hours. Occupational stress can be evaluated as job
strain, which is a combination of high demands at work with low decision
latitude or control. Job strain has been related to coronary heart disease, and a
number of studies have shown that it is also associated with higher ambulatory
blood pressures, both cross-sectionally and prospectively, in men but not in
women. It is likely that environmental and lifestyle facts operate interactively
rather than independently to promote hypertension. There is also extensive
evidence that overactivity of the sympathetic nervous system plays a role in
the development of hypertension, particularly in its early stages. So far it has
not been established why this should occur. There are several possible
environmental origins, however, and all of the lifestyle factors mentioned
above have been shown in at least some studies to operate via the
sympathetic nervous system
Environmental hypertensionology" the effects of
environmental factors on blood pressure in clinical
practice and research.
Blood pressure (BP) is affected by many environmental factors including
ambient temperature, altitude, latitude, noise, and air pollutants. Given their
pervasiveness, it is plausible that such factors may also have an impact on
hypertension prevalence and control rates. Health care providers should be
aware that the environment can play a significant role in altering BP. Although
not among the established modifiable risk factors (e.g. obesity) for
hypertension, reducing exposures when pertinent should be considered to
prevent or control hypertension. The authors provide a concise review of the
evidence linking diverse environmental factors with BP and suggest an
approach for incorporating this knowledge into clinical practice. The authors
propose using the term environmental hypertensionology to refer to the study
of the effects of environmental factors on BP in clinical and research settings.
Hypertension is a common disease and also one of the main risk factors for
coronary heart disease. It is commonly accepted that blood pressure (BP) level
is a function of genetic and environmental factors originating either early in
utero, possibly as a consequence of maternal nutritional conditions, or later
during adult life. Family and twin studies have been used to decompose
genetic and environmental contributions to systolic and diastolic BP variation.
Heritability estimates for systolic BP range from 13% to 82% and for diastolic
BP from less than 1% to 64%, with average levels for both of approximately
50%.'
Genetics Effect on blood -
Large studies (including hundreds of thousands of individuals) identified
genetic factors influencing blood pressure. However, it is unknown whether
the effect of the discovered genetic variants are modified by life-style factors.
Hypertension is a cardiovascular disease in which the blood pressure in the
arteries is elevated. A high blood pressure can be a risk factor for stroke and
heart attack. Blood pressure is defined by two measurements, the systolic and
the diastolic. We talk about hypertension when the systolic blood pressure is
above 140mmHg and/or the diastolic blood pressure is above 90mmHg. The
main organ responsible for the control of the blood pressure is the kidney so
the most causal genes should be expressed in this organ or involved in the
reninangiotensinaldosterone system.
.
Estimation of Enzyme on Blood -
Estimation of blood glucose by Glucose oxidase method -
To understand the importance of measuring blood glucose level.
To understand the principles of enzymatic estimation of glucose.
Glucose is a simple sugar which is a permanent and immediate primary source
of energy to all of the cells in our body. The glucose in blood is obtained from
the food that you eat. This glucose gets absorbed by intestines and distributed
to all of the cells in body through bloodstream and breaks it down for energy.
Body tries to maintain a constant supply of glucose for your cells by
maintaining a constant blood glucose concentration. The concentration of
glucose in blood, expressed in mg/dl, is defined by the term glycemia. The
value of blood sugar in humans generally ranges from 70 - 100 mg/dl. Blood
sugar levels are regulated by the hormones insulin and glucagon which act
antagonistically. These two hormones are secreted by the islet cells of the
pancreas, and thus are referred to as pancreatic endocrine hormones. When
the blood glucose levels are high, insulin hormone secreted which causing liver
to convert more glucose molecules into glycogen and when the blood glucose
levels are low glucagon secreted and act on liver cells to promote the
breakdown of glycogen to glucose and increases the blood glucose
concentrations. Essentially blood glucose levels determine the time of
secretion of these hormones.
The blood glucose level is easily changed under the influence of some external
and internal factors such as body composition, age, physical activity and sex.
Diabetes is a disease related by the abnormal metabolism of blood sugar and
defective insulin production. So blood sugar levels are an important parameter
for the study of diabetes. The level of glucose circulating in blood at a given
time is called as blood glucose level. The blood glucose level varies at different
time on various part of the day. Hypoglycemia is a possible side effect of
diabetes medications in which blood glucose level drops below 70mg/dl. In
people with diabetes, the body doesn't produce enough insulin or respond to
insulin properly. The result is that sugar builds up in the blood stream,
damaging the body's organs, blood vessels and nerves. This condition in which
too much sugar in the blood stream is called hyperglycemia
ESTIMATION OF ACID PHOSPHATASE ACTIVITY OF BLOOD
SERUM-
The quantitative determination of these enzymes in serum is of interest chiefly
because the acid phosphatase activity of normal blood serum is attributed to
distinct phosphomonoesterases of uncertain physiological significance and the
blood serum of subjects with metastasizing carcinoma of the prostate gland
contains an acid phosphatase with properties corresponding to the enzyme
found by Kutscher and Wolbergs in normal prostate tissue and in seminal fluid.
Invasion of the circulating fluids by carcinomatous prostate tissue liberates
prostate acid phosphatase into the blood where the enzyme can be identified
and the source of the primary tumor so determined.
The general principles underlying the determination of serum alkaline
phosphatases apply also to the determination of serum acid phosphatases.
We have adapted the King and Armstrong method for alkaline phosphatase to
the estimation of serum acid phosphatase activity.
We wish to consider here certain specific conditions which must be satisfied in
adaptations of this kind:
Since serum contains both alkaline and acid phosphatases, the former usually
in great excess, hydrolysis must be conducted under conditions which arc
optimal for acid but completely inhibit alkaline enzymes. This involves a study
of pH-activity relations, particularly of pathological sera containing varying
proportions of both enzymes. The acid phosphatase activity of normal sera is
extremely small. A number of substrate-buffer combinations in varying
concentrations were investigated in order to obtain satisfactory calorimetric
readings without having to hydrolyze too long. After prolonged hydrolysis
significant deviations from linear time-activity relations occur.
GLUCOSE LEVEL IN BLOOD
A glucose meter (or glucometer) is a medical device for determining the
approximate concentration of glucose in the blood. It can also be a strip of
glucose paper dipped into a substance and measured to the glucose chart. It is
a key element of home blood glucose monitoring (HBGM) by people with
diabetes mellitus or hypoglycemia. A small drop of blood, obtained by pricking
the skin with a lancet, is placed on a disposable test strip that the meter reads
and uses to calculate the blood glucose level. The meter then displays the level
in mg/dl or mmol/l.
Since approximately 1980, a primary goal of the management of type 1
diabetes and type 2 diabetes mellitus has been achieving closer-to-normal
levels of glucose in the blood for as much of the time as possible, guided by
HBGM several times a day. The benefits include a reduction in the occurrence
rate and severity of long-term complications from hyperglycemia as well as a
reduction in the short-term, potentially life-threatening complications of
hypoglycemia
Characterstick
There are several key characteristics of glucose meters which may differ from
model to model:
Size: The average size is now approximately the size of the palm of the
hand. They are battery-powered.
Test strips: A consumable element containing chemicals that react with
glucose in the drop of blood is used for each measurement. For some
models this element is a plastic test strip with a small spot impregnated
with glucose oxidase and other components. Each strip is used once and
then discarded. Instead of strips, some models use discs, drums, or
cartridges that contain the consumable material for multiple tests.
Coding: Since test strips may vary from batch to batch, some
models require the user to manually enter in a code found on the
vial of test strips or on a chip that comes with the test strip. By
entering the coding or chip into the glucose meter, the meter will
be calibrated to that batch of test strips. However, if this process
is carried out incorrectly, the meter reading can be up to 4
mmol/L (72 mg/dL) inaccurate. The implications of an incorrectly
coded meter can be serious for patients actively managing their
diabetes. This may place patients at increased risk of
hypoglycemia. Alternatively, some test strips contain the code
information in the strip; others have a microchip in the vial of
strips that can be inserted into the meter. These last two methods
reduce the possibility of user error. One manufacturer has
standardized their test strips around a single code number, so
that, once set, there is no need to further change the code in their
older meters, and in some of their newer meters, there is no way
to change the code.
Volume of blood sample: The size of the drop of blood needed by
different models varies from 0.3 to 1 l. (Older models required larger
blood samples, usually defined as a "hanging drop" from the fingertip.)
Smaller volume requirements reduce the frequency of unproductive
pricks.
Alternative site testing: Smaller drop volumes have enabled "alternate
site testing" pricking the forearms or other less sensitive areas instead
of the fingertips. Although less uncomfortable, readings obtained from
forearm blood lag behind fingertip blood in reflecting rapidly changing
glucose levels in the rest of the body.
Testing times: The times it takes to read a test strip may range from 3 to
60 seconds for different models.
Display: The glucose value in mg/dl or mmol/l is displayed on a digital
display. The preferred measurement unit varies by country: mg/dl are
preferred in the U.S., France, Japan, Israel, and India. mmol/l are used in
Canada, Australia, China and the UK. Germany is the only country where
medical professionals routinely operate in both units of measure. (To
convert mmol/l to mg/dl, multiply by 18. To convert mg/dl to mmol/l,
divide by 18.) Many meters can display either unit of measure; there
have been a couple of published instances
in which someone with
diabetes has been misled into the wrong action by assuming that a
reading in mmol/l was really a very low reading in mg/dl, or the
converse. In general, if a value is presented with a decimal point, it is in
mmol/l, without a decimal it is most likely mg/dl.
Glucose vs. plasma glucose: Glucose levels in plasma (one of the
components of blood) are generally 10%15% higher than glucose
measurements in whole blood (and even more after eating). This
is important because home blood glucose meters measure the
glucose in whole blood while most lab tests measure the glucose
in plasma. Currently, there are many meters on the market that
give results as "plasma equivalent," even though they are
measuring whole blood glucose. The plasma equivalent is
calculated from the whole blood glucose reading using an
equation built into the glucose meter. This allows patients to
easily compare their glucose measurements in a lab test and at
home. It is important for patients and their health care providers
to know whether the meter gives its results as "whole blood
equivalent" or "plasma equivalent." One model measures beta-
hydroxybutyrate in the blood to detect ketoacidosis (ketosis).
Clock/memory: All meters now include a clock that is set by the user for
date and time and a memory for past test results. The memory is an
important aspect of diabetes care, as it enables the person with diabetes
to keep a record of management and look for trends and patterns in
blood glucose levels over days and weeks. Most memory chips can
display an average of recent glucose readings. A known deficiency of all
current meters is that the clock is often not set to the correct time (i.e. -
due to time changes, static electricity, etc...) and therefore has the
potential to misrepresent the time of the past test results making
pattern management difficult.
Data transfer: Many meters now have more sophisticated data
handling capabilities. Many can be downloaded by a cable or
infrared to a computer that has diabetes management software to
display the test results. Some meters allow entry of additional
data throughout the day, such as insulin dose, amounts of
carbohydrates eaten, or exercise. A number of meters have been
combined with other devices, such as insulin injection devices,
PDAs, cellular transmitters
[2]
and even Game Boys.
[3]
A radio link
to an insulin pump allows automatic transfer of glucose readings
to a calculator that assists the wearer in deciding on an
appropriate insulin dose.
TECHNOLOGY
Many glucose meters employ the oxidation of glucose to gluconolactone
catalyzed by glucose oxidase (sometimes known as GOx). Others use a similar
reaction catalysed instead by another enzyme, glucose dehydrogenase (GDH).
This has the advantage of sensitivity over glucose oxidase but is more
susceptible to interfering reactions with other substances.
[13]
The first-generation devices relied on the same colorimetric reaction that is
still used nowadays in glucose test strips for urine. Besides glucose oxidase, the
test kit contains a benzidine derivative, which is oxidized to a blue polymer by
the hydrogen peroxide formed in the oxidation reaction. The disadvantage of
this method was that the test strip had to be developed after a precise interval
(the blood had to be washed away), and the meter needed to be calibrated
frequently.
Most glucometers today use an electrochemical method. Test strips contain a
capillary that sucks up a reproducible amount of blood. The glucose in the
blood reacts with an enzyme electrode containing glucose oxidase (or
dehydrogenase). The enzyme is reoxidized with an excess of a mediator
reagant, such as a ferricyanide ion, a ferrocene derivative or osmium bipyridyl
complex. The mediator in turn is reoxidised by reaction at the electrode,which
generates an electrical current. The total charge passing through the electrode
is proportional to the amount of glucose in the blood that has reacted with the
enzyme. The coulometric method is a technique where the total amount of
charge generated by the glucose oxidation reaction is measured over a period
of time. This is analogous to throwing a ball and measuring the distance it has
covered so as to determine how hard it was thrown. The amperometric
method is used by some meters and measures the electrical current generated
at a specific point in time by the glucose reaction. This is analogous to throwing
a ball and using the speed at which it is travelling at a point in time to estimate
how hard it was thrown. The coulometric method can allow for variable test
times, whereas the test time on a meter using the amperometric method is
always fixed. Both methods give an estimation of the concentration of glucose
in the initial blood sample.
The same principle is used in test strips that have been commercialised for the
detection of diabetic ketoacidosis (DKA). These test strips use a beta-
hydroxybutyrate-dehydrogenase enzyme instead of a glucose oxidising enzyme
and have been used to detect and help treat some of the complications that
can result from prolonged hyperglycaemia.
Blood alcohol sensors using the same approach, but with alcohol
dehydrogenase enzymes, have been tried and patented but have not yet been
successfully commercially developed
LDH BLOOD TEST-
LDH is the short form for the Lactate Dehydrogenase test. This test is typically
used as a measure of tissue damage in an individual. It may be used to
measure acute tissue damage, which has occurred due to a recent illness or
injury. It may also be used to measure chronic tissue damage which has
occurred due to a debilitating and progressive condition. Because of this
function, the LDH test may also be used to measure and detect the rate of
progression of such a condition based on the rate at which the results are
progressing. The LDH blood test is carried out under instruction from a doctor
when there is sufficient evidence to point to cellular or tissue damage. The
level of LDH has to be elevated in order to confirm that there is some sort of
damage in the body. However, the LDH level alone may not be able to pin
point the exact location of the damage or injury. A further test or series of
tests may be ordered to locate the area where the damage has occurred.
There is an LDH iso-enzymes test which may be used for further diagnosis,
along with other tests that can identify the location of cellular damage. After
diagnosis is complete, medical intervention will be decided upon based on the
location and severity of the problem. Further testing of the LDH levels will
continue as treatment progresses to monitor the effects of the treatment. If
the problem continues to worsen, the level of LDH will continue to rise,
whereas if an improvement has occurred it will register a fall. Hemolytic
anemia can be checked for using the LDH test. Hemolytic anemia occurs when
the red blood cells are being broken by a physical barrier, which is an artificial
valve or stent in the body, or by some condition that is causing the blood cells
to be unusually weak.
High LDH levels can be associated with some conditions such as, strokes,
hemolytic anemia, drug abuse, kidney disease, liver disease, mononucleosis,
pancreatic disease, and muscular dystrophy. It is also important to know when
the level of LDH will be elevated naturally. People who undergo strenuous
exercise or have just taken part in a physically demanding activity may have
slightly damaged muscles as the muscles have been strained to a great extent.
This will reflect in a temporary rise in LDH levels, so it is important rest well
prior to any testing.
What does elevated LDH levels mean?
The enzyme LDH or Lactic Acid Dehydrogenase is responsible for creating
energy for the cells in the body. It is found in almost all body tissues and can be
measured by a simple blood test.
Normal LDH levels are generally low and range between 140 IU/liter to 333 IU/
liter. Low LDH levels are usually no cause for concern. However, elevated LDH
levels may indicate cell damage. This damage could be caused by a number of
medical conditions. Some of the elevated LDH level causes include tissue
damage due to trauma or disease, a recent heart attack, disease of the liver or
the kidney or even the lungs, cancer, anemia, HIV, meningitis or encephalitis to
name a few. If a blood test report is positive (a high LDH reading) more medical
tests will be required to determine the actual cause of the cell damage. LDH
tests are also used to monitor a patient's response to chemotherapy or to
evaluate the rate of muscular degeneration or the progress of HIV.
Elevated LDH levels in children also indicate some type of tissue damaged
caused by diseases, trauma or infections. Children suffering from anemia or
cancer need to routinely do an LDH test to monitor their progress and
response to medications.
What are the causes of high and low ldh levels?
Lactate dehydrogenase also known as LDH is an enzyme that is found in nearly
all body tissues. LDH is responsible for creating energy from glucose for cells.
Normal levels of LDH range from 105 and 333 IU/liter. In fact low levels of LDH
indicate that all is normal in the body. In cases where the numbers are radically
low there is still no need to worry. One of the causes of low LDH levels may be
a high intake of vitamin C and this will show up in other blood reports as well.
You should be careful if the LDH levels go over the 333 IU/liter mark. High
levels of LDH can indicate a number of medical conditions such as tissue
damage (due to trauma or disease), hemolytic anemia (an abnormal
breakdown of red blood cells), liver disease, encephalitis, kidney failure, a
recent heart attack, and some types of cancer. An LDH blood test can also
confirm if chemotherapy is working successfully. The test is therefore a regular
part of cancer follow-up care.
Tissue damage is one of the major causes of high LDH levels. Besides this you
could also get a false positive test result due to improper handling of blood test
samples.
What are the Normal LDH levels in blood?
LDH or Lactic Acid Dehydrogenase is an enzyme that is found in almost all
tissue in the body. It is responsible for converting glucose derived from food
into energy. Cells then use this energy in order to function properly. Normal
LDH levels in the blood range from 140 IU/liter to 333 IU/ liter.
You should know that low LDH levels in the blood are not indicative of any
medical problem. At the most a low LDH reading may be a response to a high
intake of vitamin C. It is only when the LDH readings are higher than the
average LDH levels in the blood that there is an indication that there may be
cell damage. High levels of LDH can be due to a number of medical conditions.
Some of these include lung disease, liver disease, kidney failure, anemia, and
some types of cancer, a recent heart attack and tissue degeneration. A blood
test is required to measure LDH levels. If the readings are positive or high,
more medical tests may be necessary in order to get to the cause of the
problem.
Testing the blood for LDH levels also helps assess the efficacy of cancer
treatments such as chemotherapy.
CPK ISOENZYME
What Is a CPK Isoenzymes Test?
Enzymes are complex proteins that facilitate chemical changes in every part of
the body. Your body needs enzymes to function. The CPK isoenzymes test is a
way to measure the levels of an enzyme called creatine phosphokinase (CPK) in
your blood.
CPK can be broken down into three distinct parts:
CPK-1 comes mainly from the brain and lungs
CPK-2 is mainly from the heart
CPK-3 is from skeletal muscle.
When these parts of your body suffer damage due to injury or disease, CPK
isoenzymes can be released into your bloodstream. Checking the levels of
these enzymes in your bloodstream can help doctors identify the areas of your
body that have been damaged.
The CPK isoenzymes test is a simple blood test requiring almost no preparation
and involves minimal risk. The blood sample will be sent to a laboratory for
analysis and your doctor will explain the results to you.
Purpose of CPK Test
A CPK blood test is generally ordered when people go to an emergency room
with symptoms of a heart attack. Your doctor may order a CPK blood test to:
help diagnose a heart attack
investigate chest pain
find out how much heart or muscle tissue has been damaged
The test can also determine whether you carry the gene for muscular
dystrophy. It can detect dermatomyositis (a muscle disease), polymyositis (an
inflammatory disease that affects muscle tissue), and malignant hyperthermia,
an inherited disease that is exacerbated by general anesthesia.
Preparation for the Blood Test
The CPK isoenzymes blood test is performed just like other routine blood tests.
The actual blood analysis takes place in a laboratory. No fasting or special
preparation on the part of the patient is required.
Before scheduling your blood test, it is important to tell your doctor about any
over-the-counter and prescription medications you take. Some substances that
can interfere with the test results are:
drugs that lower cholesterol
steroids
anesthetics
amphotericin B (an antifungal medication)
alcohol
cocaine
Other factors may also interfere with test results, including:
vigorous exercise
prolonged immobility
intramuscular injections
cardiac catheterization
recent surgery
Be sure to discuss these events with your doctor prior to taking the blood test.
How the Blood Test Works
The blood test should take only a few minutes.
Your healthcare provider will use a topical antiseptic to clean a small area of
your arm, usually on the inside of your elbow or on the back of your hand. An
elastic band will then be wrapped around your upper arm to create pressure
and make it easier to access a vein.
A needle will be inserted into your vein and blood drawn into a small vial. You
will probably feel the stick of the needle or a stinging sensation. After the vial is
filled, the elastic band and the needle will be removed. A bandage will be
placed over the puncture site.
The vial will be labeled and sent to a laboratory. Results will be forwarded to
your doctor, who will explain them to you.
In some cases, your doctor may want to repeat the test over several days to
see if your enzyme levels change. Changing levels can help with the diagnosis.
Side Effects
Your arm may feel sore where the needle was inserted and you might have
some mild bruising or throbbing for a short while. You will likely have more
discomfort in rare instances when the healthcare provider has difficulty
accessing a vein.
Most people have no serious or lasting side effects. Rare complications of a
blood test include:
bleeding
lightheadedness
fainting
infection (a risk whenever skin is pierced)
If you experience any of these symptoms, contact your doctor immediately.
Analyzing the Results
CPK-1
CPK-1 is found primarily in the brain and lungs. Elevated CPK-1 levels could
indicate:
brain injury, stroke, or bleeding
brain cancer
seizure
pulmonary infarction (death to an area of the lung)
CPK-2
CPK-2 is found in the heart. Elevated levels of CPK-2 can be the result of:
injury to the heart (due to accident)
inflammation of the heart muscle (usually from a virus)
electrical injuries
The presence of high levels of CPK-2 in the blood can also follow heart
defibrillation and open heart surgery. After a heart attack, CPK-2 levels in the
blood rise, but usually fall again within 48 hours.
Congestive heart failure, angina, or pulmonary embolisms generally do not
cause CPK-2 to rise in the bloodstream.
CPK-3
Levels of CPK-3 may rise in the bloodstream if muscles:
are damaged from a crush injury (when a body part has been squeezed
between two heavy objects)
have been immobile for a long period
are damaged by drugs
are inflamed
Other factors that contribute to high levels of CPK-3 include:
muscular dystrophy
muscle trauma (from contact sports, burns, and surgery)
seizures
electromyography (testing of nerves and muscle function)
Results will vary from person to person, depending on specific injuries and
conditions. Your doctor will explain what your specific results mean, and
discuss the most effective form of treatment
Determination of Acid -Glucosidase Activity in Blood
Spots as a Diagnostic Test for Pompe Disease
Pompe disease is an autosomal recessive disorder of glycogen metabolism that
is characterized by a deficiency of the lysosomal acid -glucosidase. Enzyme
replacement therapy for the infantile and juvenile forms of Pompe disease
currently is undergoing clinical trials. Early diagnosis before the onset of
irreversible pathology is thought to be critical for maximum efficacy of current
and proposed therapies. In the absence of a family history, the
presymptomatic detection of these disorders ideally can be achieved through a
newborn-screening program. Currently, the clinical diagnosis of Pompe disease
is confirmed by the virtual absence, in infantile onset, or a marked reduction,
in juvenile and adult onset, of acid -glucosidase activity in muscle biopsies
and cultured fibroblasts. These assays are invasive and not suited to large-scale
screening.
Methods: A sensitive immune-capture enzyme activity assay for the
measurement of acid -glucosidase protein was developed and used to
determine the activity of this enzyme in dried-blood spots from newborn and
adult controls, Pompe-affected individuals, and obligate heterozygotes.
Results: Pompe-affected individuals showed an almost total absence of acid -
glucosidase activity in blood spots. The assay showed a sensitivity and
specificity of 100% for the identification of Pompe-affected individuals.
Conclusions: The determination of acid -glucosidase activity in dried-blood
spots is a useful, noninvasive diagnostic assay for the identification of Pompe
disease. With further validation, this procedure could be adapted for use with
blood spots collected in newborn-screening programs
Relationship between Blood and Finger Print
Due to their immence potential particularly in forensic medicine, the study of
finger print pattern was carried out in relation to various ABO blood groups.
Loops are most common pattern (56.2%), followed by whorls (39.4%) and
arches (4.4%) respectively. Frequency of loops and arches were more in
females compared to males. Frequency of whorls is more in males.
Chi-Square is 15.3145 and P-value <0.001
Loops were of high in O gp (58.8%) & least in AB (50%). Whorls are highest in
AB group (49.4%) & least in O (37.5%). Arches were of high in B (7%) & least in
AB (0.6%).
Loops are highest in O-ves (59.1%) and least in AB-ves (45%). Ulnar loops were
highest in A-ves (57.8%) and least in AB-ves (45%). Radial loops were highest in
O-ves (5.8%) and AB+ves (4.6%) Whorls were of high frequency in ABves
(55%) and least in A-ves (32.1%). Arches were of high frequency in A-ves (10%).
The frequency of finger print pattern in different ABO and Rh blood groups on
all fingers is of the order that loops were of highest frequency followed by
whorls and arches, except on ring fingers, the frequency of whorls is highest.
But in A+ves, thumbs presented high frequency of whorls. In A-ves and AB+ves
the index finger presented high frequency of whorls.
Total finger ridge count and absolute ridge count in different blood groups
were tabulated as follows and analyzed statistically.
Loops are similar in Rh+ & Rh- gp. Arches were slightly more in Rh+ & whorls
were more in Rh-
The general distribution of finger print pattern in different blood groups was of
the same order i.e., high frequency of loops, followed by whorls and arches. In
the present study high frequency of loops was observed in O group (58.8%)
which is consistent with the findings of Hahne .But it differed from the
observations of Herch and Bharadwaja.
who stated that loops were more associated with A group.The frequency of
whorls is highest in AB group (49.4%) which is consistent with the study of
Bharadwaja [2]. But it differed from the study of Prateek [4] who stated that
whorls were associated more with O-ve group.
In the present study, arches were of high frequency in B group and least in AB
group. Loops were of high frequency in O-ves (59.1%) and least in AB-ves
(45%). Thefrequency of whorls ranged from 32.1% (in A-ves) to 55% (in AB-
ves). Arches were of high frequency in A-ves (10%). These observations were
consistent with findings of Prateek [4] who reported high frequency of arches
and low frequency of whorls in A-ves. The distribution of finger print pattern in
different blood groups on all fingers followed the same order in that loops
were of high frequency followed by whorls and arches, except on ring finger
where whorls are of high frequency.
Arches were of high frequency on index finger. But in A+ves, thumbs presented
high frequency of whorls. In A-ves and AB+ves, index finger and ring finger
presented more frequency of whorls. These observations are in consistent with
the findings of Bharadwaj. [2] Highest mean TFRC is observed in AB-ves
(18110.51) and least in B+ves(136.78 53.85). The mean AFRC is highest in
AB+ves (213.8 101) and least in A-ves (181 94.01). These findings differed
from those of Bharadwaj [2], who reported high TFRC (not the mean) in B
group.
Conclusion
There is an association between distribution of finger print pattern and blood
groups. In all blood groups, the frequency of finger print pattern observed is
loops were highest followed by whorls and arches respectively. But loops were
associated more with O group, whorls with AB group and arches with B group.
Thumbs presented high frequency of whorls in A+ves. Index and ring fingers
were associated with high frequency of whorls in A-ves and AB+ves. So
prediction of blood group to some extent may be possible with the study of
finger print pattern which may be of great value in forensic medicine, but
influence regional variations, gender and genetic factors should not be
overlooked.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Rationalizati ON: Prefinal Practical ExamDocument22 pagesRationalizati ON: Prefinal Practical ExamOsannah Irish InsongNo ratings yet
- Fundamentals of Anatomy and Physiology 11Th Edition Martini Test Bank Full Chapter PDFDocument48 pagesFundamentals of Anatomy and Physiology 11Th Edition Martini Test Bank Full Chapter PDFDaisyHillyowek100% (13)
- AP Biology-Tissue Types ChartDocument1 pageAP Biology-Tissue Types ChartJeannie WilliamsNo ratings yet
- Measures For Industrial PeaceDocument24 pagesMeasures For Industrial PeaceHimanshu BandilNo ratings yet
- Exit Form - PaytmDocument2 pagesExit Form - PaytmHimanshu BandilNo ratings yet
- Measures For Industrial PeaceDocument24 pagesMeasures For Industrial PeaceHimanshu BandilNo ratings yet
- Iocl - Applied CBSE NET 2014 - 28/12/14 NMDC - 17/05/15 Aai - NpcilDocument1 pageIocl - Applied CBSE NET 2014 - 28/12/14 NMDC - 17/05/15 Aai - NpcilHimanshu BandilNo ratings yet
- Exam PatternDocument1 pageExam PatternHimanshu BandilNo ratings yet
- ShivaniDocument2 pagesShivaniHimanshu BandilNo ratings yet
- ExamDocument1 pageExamHimanshu BandilNo ratings yet
- Blue Print: Customer Action - (Queries, FAQ), (Customer Get Their Answer)Document1 pageBlue Print: Customer Action - (Queries, FAQ), (Customer Get Their Answer)Himanshu BandilNo ratings yet
- Book Review Key Concept in HRDDocument5 pagesBook Review Key Concept in HRDHimanshu BandilNo ratings yet
- Vaishali Restaurant Service MGMTDocument6 pagesVaishali Restaurant Service MGMTHimanshu BandilNo ratings yet
- Cross MatchingDocument2 pagesCross MatchingHimanshu_0No ratings yet
- Anemia HemolitikDocument20 pagesAnemia HemolitikRandy GipsonNo ratings yet
- 01 Introduction To HistologyDocument60 pages01 Introduction To HistologyMartha Orendu Oche AttahNo ratings yet
- The Influence of Thyroid Function On The Coagulation Systemand Its Clinical ConsequencesDocument12 pagesThe Influence of Thyroid Function On The Coagulation Systemand Its Clinical ConsequencesTamara Silva FabresNo ratings yet
- Routine Bio-Chemistry: Blood Sugar RandomDocument2 pagesRoutine Bio-Chemistry: Blood Sugar RandomFarhan haiderNo ratings yet
- Beurer BC 08 Blood Pressure MonitorDocument76 pagesBeurer BC 08 Blood Pressure MonitormihaiylaNo ratings yet
- Perioperative Fluid Management in Pediatrics: By: Karim Kamal, MDDocument33 pagesPerioperative Fluid Management in Pediatrics: By: Karim Kamal, MDMohammed AKNo ratings yet
- Bleeding Time PDFDocument25 pagesBleeding Time PDFKhaled ZatariNo ratings yet
- HDB - Tropical Haematology and Blood Transfusion Laboratory NotesDocument78 pagesHDB - Tropical Haematology and Blood Transfusion Laboratory NotesAbdul AleemNo ratings yet
- Blood Gases: Arterial VenousDocument11 pagesBlood Gases: Arterial VenousDerper WatsonNo ratings yet
- ABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFDocument31 pagesABO - RH - Blood - Grouping Guidance - Manucal - 26 - 03 - 2013 PDFLalrinchhanaNo ratings yet
- Platelet-Rich Plasma: Clinical Applications in DentistryDocument4 pagesPlatelet-Rich Plasma: Clinical Applications in DentistryVijithNo ratings yet
- Connective TissueDocument20 pagesConnective TissueWadabi100% (1)
- Exercise No. 7Document21 pagesExercise No. 7John MelbyNo ratings yet
- Transfusion Medicine in Exotic Pets: Marla Lichtenberger, DVM, DACVECCDocument8 pagesTransfusion Medicine in Exotic Pets: Marla Lichtenberger, DVM, DACVECCAlice HellerNo ratings yet
- Clotting Factors Blood Liver Prothrombin TimeDocument2 pagesClotting Factors Blood Liver Prothrombin TimeArindah Dinar SafitriNo ratings yet
- Hemoglobin and HematocritDocument9 pagesHemoglobin and HematocritLovely B. AlipatNo ratings yet
- Blood CoagulationDocument10 pagesBlood CoagulationgauravkokraNo ratings yet
- Connective TissueDocument5 pagesConnective TissueJanjan Garces100% (1)
- MUST To KNOW in HematologyDocument44 pagesMUST To KNOW in HematologyJan Joseph YbañezNo ratings yet
- PD 4 WJ SBJ UE7 XAASH4 U KZDocument11 pagesPD 4 WJ SBJ UE7 XAASH4 U KZPrincy GuptaNo ratings yet
- Hematology PreliminariesDocument7 pagesHematology PreliminariesRomie SolacitoNo ratings yet
- Anaphy Tissues ReviewerDocument9 pagesAnaphy Tissues ReviewerleyluuuuuhNo ratings yet
- IBO 2015 Theory 1 (EN)Document59 pagesIBO 2015 Theory 1 (EN)tilzit7777No ratings yet
- Wound Healing: Biology Presentation by AbbyDocument8 pagesWound Healing: Biology Presentation by AbbyRaymundus Deaven GoanaNo ratings yet
- DIPASREE - ROYCHOWDHURYAnomalous Secondary Growth in Boerhaavia Stem2020!04!03Anomalous Secondary Growth in Boerhaavia StemDocument2 pagesDIPASREE - ROYCHOWDHURYAnomalous Secondary Growth in Boerhaavia Stem2020!04!03Anomalous Secondary Growth in Boerhaavia StemAkshay KannanNo ratings yet
- Module 9Document3 pagesModule 9Gia Joy B. PardeNo ratings yet