Professional Documents
Culture Documents
Approach To A Child With Hepatosplenomegaly
Approach To A Child With Hepatosplenomegaly
Uploaded by
avi_1388Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Approach To A Child With Hepatosplenomegaly
Approach To A Child With Hepatosplenomegaly
Uploaded by
avi_1388Copyright:
Available Formats
Approach To A Child
With
Hepatosplenomegaly
Dr. Pushpa Raj Sharma
Professor of Child Health
Institute of Medicine
Case History
Eight months, male, from Rupandehi.
Fever with cough and difficulty breathing for
one week, more severe for one day.
Progressive abdominal distension for 4
months.
Repeated pneumonia since 3 months of life
History contd.
Uneventful perinatal period.
Exclusive breast feeding for 3 months.
Repeated treatment with antibiotics since
four months of age for cough and fever.
Gaining weight.
Single child of parent.
Other histories including developmental are
normal
Examination
Wt: 5 Kgs; Length: 64 cms; OFC: 39.5 cm
Apyrexial; R/R: 66/min; P/R: 150/min.
No pallor; no lymphadenopathy; no rash; no
cataract; no specific body odour.
Chest indrawing present; bilateral creps.
Normal heart sounds.
Liver and spleen 5 and 8 cms below costal
margin respectively; non tender; smooth; firm.
no ascitis;
Other system normal
Investigations
Hb: 12.2.g/dL; TLC/DLC: normal; ESR: 20mm/hr.
peripheral film/platelets: normal.
Blood sugar: 79mg/dLSerum
cholesterol:90mg/dL; Liver function: normal
Aldehyde test: negative.
Stool/Urine: normal
HIV:-ve; TORCH: -ve;
USG abdomen: no ascitis, hepatosplenomegaly,
no structural abnormality
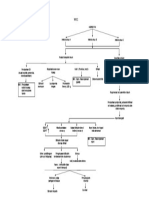
Hepatosplenomegaly: Causes
Infective:
Viral: Hepatotrophic (A,B,C,D,E) and other viruses
(herpes, cytomegalo, Ebstein-Barr, varicella,HIV,
rubella, adeno, entero, arbo.)
Protozoal: malaria, kalazar, amoebic, toxoplasma
Bacterial: sepsis; tuberculosis, brucellosis, syphilis,
Helminths: hydatid, visceral larva migrans
Fungal: histoplasmosis
Hepatosplenomegaly: Causes
Haemopoetic:
Haemolytic: haemolytic disease of newborn
thalassaemia;
Anaemia
Metabolic:
Neiman-Pick, gangliosidosis, Gaucher, fucosidosis,
Wolman, glycogen storage, sialiodosis,
galactosialiodosis, a-mannosidosis.
Hepatosplenomegaly: Causes
Malignancies:
Leukemia, histiocytic syndromes, myeloproliferative
syndromes, lymphomas,
Immunological:
Chronic granulomatous, heriditory neutrophilia, Ommen
syndrome.
Developmental:
Congenital hepatic fibrosis
Congestive:
Hepatic vein obstruction, constrictive pericarditis
This patient
Infective cause that can have lung, liver and
spleen involvement:
Sepsis/other bacterial infection unlikely: normal
blood count, normal immunological reports for
HIV, TORCH, syphilis.
Viral infections unlikely: normal liver function test,
no clinical evidence of congenital infections as:
Neonatal jaundice, retinitis, microcephaly,
hydrocephaly, intracranial infections, osteochondritis,
rash, normal weight and height for age.
This patient
Protozoal unlikely:
Negative blood report (anaemia, jaundice,
pancytopenia), big hepatosplenomegaly.
Haematological unlikely:
Absence of anaemia, jaundice and in the presence
of huge spleenomegaly.
Malignancies unlikely:
Normal blood report, absence of lymphadenopathy
This patient
Immunological unlikely:
Normal liver function, absence of
hypereosinophilia and diarrhoea
Developmental unlikely:
Absence of features of portal hypertension
Congestive unlikely:
Absence of cardiac insufficiency signs,
absence of ascitis.
This patient:
Metabolic Diseases Causing Hepatosplenomegaly
Infantile GM1 gangliodidosis (type 1)
Hepatosplenomegaly at birth, oedema, skin
erruptions, retardation development, seizure
Gauchers:
Features of bone marrow involvement, skeletal
complications
Fucosidosis:
Macroglossia, neurodegenerative features
Wolman disease:
Failure to thrive, steatorrhoea, relentless vomiting
Metabolic Diseases Causing
Hepatosplenomegaly
Glycogen storage Type IV:
Failure to thrive, cardiomyopathy, myopathy
Mucopolysaccharidoses:
Corneal clouding, coarse hair, short stature,
joint stiffness.
Sialidosis and galactodialidosis:
Neonatal sepsis, dysostosis multiplex,
seizures, cherry red spots, mental retardation.
a-mannodidosis:
Psychomotor retardation, dystosis multiplex,
This patient
Neiman-Pick disease :
This could be the likely cause.
Neiman-Pick disease: Two types A and B
Type A: hepatosplenomegaly, moderate
lymphadenopathy, psychomotor retardation.
Type B: splenomegaly first manifestation,
recurrent pneumonias, normal IQ.
You might also like
- Adult Total Body Detox GuideDocument40 pagesAdult Total Body Detox GuideemanvitoriaNo ratings yet
- BD Chaurasia's Human Anatomy, Volume 2 - Lower Limb, Abdoman and Pelvis, 6th Edition PDFDocument472 pagesBD Chaurasia's Human Anatomy, Volume 2 - Lower Limb, Abdoman and Pelvis, 6th Edition PDFYash Salunkhe87% (23)
- RS ARI-Common Cold - PPT 93Document57 pagesRS ARI-Common Cold - PPT 93Dr.P.NatarajanNo ratings yet
- Hematology McqsDocument63 pagesHematology McqsGalaleldin AliNo ratings yet
- Dr-Gerson Suppressed Congressional TestimonyDocument10 pagesDr-Gerson Suppressed Congressional TestimonyJacek Rafał Tatko100% (1)
- Case Study - Nephrotic SyndromeDocument42 pagesCase Study - Nephrotic Syndromefarmasi rsud cilincingNo ratings yet
- Understanding Glomerular Disease: C.M. Yuan Nephrology SVC Walter Reed Army Medical Center Washington, DC 20307Document40 pagesUnderstanding Glomerular Disease: C.M. Yuan Nephrology SVC Walter Reed Army Medical Center Washington, DC 20307mondy199646No ratings yet
- Glomerulonephritis For GPVTSDocument63 pagesGlomerulonephritis For GPVTSSumita MuniandyNo ratings yet
- HepatosplenomegalyDocument10 pagesHepatosplenomegalyนายนภนต์ จันทมณีNo ratings yet
- Nephrotic and Nephritic Syndrome: Med5010 LectureDocument65 pagesNephrotic and Nephritic Syndrome: Med5010 LectureFreeburn Simunchembu100% (1)
- MRCPCH Guide EndoDocument7 pagesMRCPCH Guide EndoRajiv KabadNo ratings yet
- Precocious Puberty With Primary Hypothyroidism Due To Autoimmune ThyroiditisDocument3 pagesPrecocious Puberty With Primary Hypothyroidism Due To Autoimmune ThyroiditisShohel RanaNo ratings yet
- 6 - Inborn Errors of Metabolism - Spring 23Document42 pages6 - Inborn Errors of Metabolism - Spring 23Abdo HaiderNo ratings yet
- 9 Month Old Well-Child Check CC: Abdominal Distention: Michelle Meder, MD Pediatric Resident, PGY-2Document17 pages9 Month Old Well-Child Check CC: Abdominal Distention: Michelle Meder, MD Pediatric Resident, PGY-2Emily EresumaNo ratings yet
- Nephrotic SyndromeDocument49 pagesNephrotic SyndromeAMA237No ratings yet
- Approach To JaundiceDocument36 pagesApproach To JaundiceNandita ChatterjeeNo ratings yet
- Nephrotic SyndromeDocument24 pagesNephrotic SyndromeSamah KhanNo ratings yet
- Clinical Features A) Upper Urinary Tract (Pyelonephritis) :: T:Marwa AL-Headri 1Document16 pagesClinical Features A) Upper Urinary Tract (Pyelonephritis) :: T:Marwa AL-Headri 1abnaltag667No ratings yet
- Pathology of Common Glomerular Syndromes: DR Purushotham KrishnappaDocument34 pagesPathology of Common Glomerular Syndromes: DR Purushotham KrishnappaTarin IslamNo ratings yet
- Nephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassDocument143 pagesNephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassKay BristolNo ratings yet
- Nephrotic and Nephritic Syndrome - 2008Document65 pagesNephrotic and Nephritic Syndrome - 2008rikasusanti101001201No ratings yet
- Investigations in Oral MedicineDocument18 pagesInvestigations in Oral Medicinedr_jamal1983100% (2)
- POLYCYTHEMIADocument14 pagesPOLYCYTHEMIAPrajwal Kumar JhaNo ratings yet
- Anemia JournalDocument8 pagesAnemia JournalAmreen KausarNo ratings yet
- Nephrotic Syndrome: Department of Pediatrics The First Affiliated Hospital Sun Yat-Sen UniversityDocument67 pagesNephrotic Syndrome: Department of Pediatrics The First Affiliated Hospital Sun Yat-Sen UniversityBuwaneka VidanageNo ratings yet
- Content BVDocument88 pagesContent BVMohamed IbrahimNo ratings yet
- Nephrotic SyndromeDocument34 pagesNephrotic SyndromeAnusikta PandaNo ratings yet
- سمنر نسائيهDocument20 pagesسمنر نسائيهsuad aliNo ratings yet
- Hepatomegali in Infant and Children - Pediatrics in Review-2000-Wolf-303-10Document10 pagesHepatomegali in Infant and Children - Pediatrics in Review-2000-Wolf-303-10Reddy LufyanNo ratings yet
- GIT Portal HypertensionDocument24 pagesGIT Portal HypertensionDr.P.NatarajanNo ratings yet
- Change in Urine Color (2Document38 pagesChange in Urine Color (2Mustafa LaithNo ratings yet
- Lecture-Glomerulopathies and Nephrotic SyndromeDocument35 pagesLecture-Glomerulopathies and Nephrotic SyndromeJames StiltonNo ratings yet
- Naga College Foundation, Inc.: Case Study On AnemiaDocument66 pagesNaga College Foundation, Inc.: Case Study On AnemiaAnnie Lou AbrahamNo ratings yet
- Reumato and EndocrineDocument106 pagesReumato and Endocrinehasanatiya41No ratings yet
- 3 Nephrotic SyndromeDocument12 pages3 Nephrotic SyndromeMohamed Na3eemNo ratings yet
- Management of Hyperemesis Gravidarum Francis Ajang Magaji MB, BS, FMCOG (Nig), FWACSDocument13 pagesManagement of Hyperemesis Gravidarum Francis Ajang Magaji MB, BS, FMCOG (Nig), FWACSJunita KosendangNo ratings yet
- Chapter 49Document6 pagesChapter 49Melissa Aina Mohd YusofNo ratings yet
- 1.3 Demam Tifoid Dan Kelainan HeparDocument145 pages1.3 Demam Tifoid Dan Kelainan HeparajikwaNo ratings yet
- Medical Diseases Complicating Pregnancy: by The Name of AllahDocument45 pagesMedical Diseases Complicating Pregnancy: by The Name of Allah'محمد علي' محمد لافيNo ratings yet
- PediaDocument10 pagesPediaKannan KannanNo ratings yet
- SchistosomiasisDocument33 pagesSchistosomiasishendra ari100% (1)
- By DR - Tosif Ahmad TMO-PediatricsDocument27 pagesBy DR - Tosif Ahmad TMO-PediatricskamalNo ratings yet
- HepatosplenomegalyDocument49 pagesHepatosplenomegalyTarun SinghNo ratings yet
- 235-Article Text-483-1-10-20160818Document8 pages235-Article Text-483-1-10-20160818YandiNo ratings yet
- NCM 109 Maternal Lecture Lesson: CausesDocument2 pagesNCM 109 Maternal Lecture Lesson: CausesJanelle ArcillaNo ratings yet
- Neonatal JaundiceDocument5 pagesNeonatal JaundiceLana LocoNo ratings yet
- Acute EncephalopathyDocument4 pagesAcute Encephalopathymadimadi11No ratings yet
- 22 - Proteinuria and HematuriaDocument73 pages22 - Proteinuria and HematuriaArsalan NadeemNo ratings yet
- Acute GlomerulonephritisDocument24 pagesAcute GlomerulonephritisNipul MondolNo ratings yet
- Acute Post-Streptococcal GlomerulonephritisDocument27 pagesAcute Post-Streptococcal GlomerulonephritisAlokh Saha RajNo ratings yet
- Fever of Unknown Origin (FUO)Document55 pagesFever of Unknown Origin (FUO)mohamed hanyNo ratings yet
- Acute GlomerulonephritisDocument6 pagesAcute GlomerulonephritisAnsu MaliyakalNo ratings yet
- GlomerulonephritisDocument35 pagesGlomerulonephritisapi-19916399No ratings yet
- Anak 1Document4 pagesAnak 1Vega HapsariNo ratings yet
- Hypertension Due To Renal Artery Stenosis: Case ReportDocument6 pagesHypertension Due To Renal Artery Stenosis: Case ReportSabhina AnseliaNo ratings yet
- 2Document5 pages2Manthan PatelNo ratings yet
- Chapter 308Document10 pagesChapter 308Lemuel LinoNo ratings yet
- Hemolyticuremicsyndrome 141212190757 Conversion Gate01Document22 pagesHemolyticuremicsyndrome 141212190757 Conversion Gate01Ramses GamingNo ratings yet
- Acute Glomerulonephritis By: Dr. Oyebode Ayodel.A. On 1 June, 2018Document18 pagesAcute Glomerulonephritis By: Dr. Oyebode Ayodel.A. On 1 June, 2018anon_648030566No ratings yet
- Obg PPT 1Document27 pagesObg PPT 1yash myatraNo ratings yet
- Alert Medical Series: USMLE Alert I, II, IIIFrom EverandAlert Medical Series: USMLE Alert I, II, IIIRating: 2 out of 5 stars2/5 (1)
- CNS Seizures in ChildhoodDocument42 pagesCNS Seizures in ChildhoodDr.P.NatarajanNo ratings yet
- Endocrinology Adreno Genital SyndromeDocument29 pagesEndocrinology Adreno Genital SyndromeDr.P.NatarajanNo ratings yet
- Cns Neurological ExaminationDocument26 pagesCns Neurological ExaminationDr.P.NatarajanNo ratings yet
- GIT Examination of AbdomenDocument63 pagesGIT Examination of AbdomenDr.P.NatarajanNo ratings yet
- GIT Viral Hepatitis in Children - PPT 93Document22 pagesGIT Viral Hepatitis in Children - PPT 93Dr.P.NatarajanNo ratings yet
- GIT Portal HypertensionDocument24 pagesGIT Portal HypertensionDr.P.NatarajanNo ratings yet
- Rs Wheeze in ChildrenDocument44 pagesRs Wheeze in ChildrenDr.P.NatarajanNo ratings yet
- GIT Cirrhosis Liver in ChildrenDocument37 pagesGIT Cirrhosis Liver in ChildrenDr.P.NatarajanNo ratings yet
- Rs PleurisyDocument32 pagesRs PleurisyDr.P.NatarajanNo ratings yet
- Rs Foreign Body AspirationDocument50 pagesRs Foreign Body AspirationDr.P.NatarajanNo ratings yet
- Lect. 12 Digestive SystemDocument74 pagesLect. 12 Digestive Systemflex gyNo ratings yet
- Evaluation of Ascites and Its Etiology Using Ultrasonography JRD 119 PDFDocument4 pagesEvaluation of Ascites and Its Etiology Using Ultrasonography JRD 119 PDFEstu Paramadina PratamaNo ratings yet
- Gross Anatomy & Histology of Liver: Prepared By: Anish Dhakal (Aryan) MBBS Student Patan Academy of Health SciencesDocument21 pagesGross Anatomy & Histology of Liver: Prepared By: Anish Dhakal (Aryan) MBBS Student Patan Academy of Health SciencesAjeng TunjungputriNo ratings yet
- TEST - Cancer-ParasiteDocument41 pagesTEST - Cancer-ParasiteRazvan Andrei Valcu100% (2)
- IJ - HCC Non Resectable Lenvima WebinarDocument19 pagesIJ - HCC Non Resectable Lenvima WebinarIndah JamtaniNo ratings yet
- Colecistitis LitiasicaDocument25 pagesColecistitis LitiasicaLuis Adolfo Ramos CastilloNo ratings yet
- IJSO Biology Module - 3Document207 pagesIJSO Biology Module - 3Ikhbaat Atiqur RehmanNo ratings yet
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocument47 pagesTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNo ratings yet
- Usd 12345Document1 pageUsd 12345Msadir KhanNo ratings yet
- 2 5640374391406816Document26 pages2 5640374391406816sillypoloNo ratings yet
- 2 Histology of The Liver, Gallbladder, and Pancreas - 2Document11 pages2 Histology of The Liver, Gallbladder, and Pancreas - 2Linh PhanNo ratings yet
- S.NO. Topic KEY Stem of The Option 1 Option 2 Option 3 Option 4Document12 pagesS.NO. Topic KEY Stem of The Option 1 Option 2 Option 3 Option 4Prosanta Kr BhattacharjeeNo ratings yet
- Stages of Alcohol-Related Liver DiseaseDocument11 pagesStages of Alcohol-Related Liver DiseaseAF KoasNo ratings yet
- WOC HepatitisDocument1 pageWOC Hepatitisdestri wulandariNo ratings yet
- Left Lateral Liver SegmentectomyDocument7 pagesLeft Lateral Liver SegmentectomyTeja Laksana NukanaNo ratings yet
- Digestive System AnatomyDocument8 pagesDigestive System AnatomyBrittany Lei MaquirayaNo ratings yet
- Pig AnatomyDocument13 pagesPig AnatomyNatasia TanaumaNo ratings yet
- Lesson Plan - Anatomy of LiverDocument5 pagesLesson Plan - Anatomy of LiverDelphy VargheseNo ratings yet
- A Guide To The Management of Tuberculosis in Patients With Chronic Liver DiseaseDocument12 pagesA Guide To The Management of Tuberculosis in Patients With Chronic Liver DiseaseMeldaNo ratings yet
- GASTRO Terminology & GlossaryDocument13 pagesGASTRO Terminology & GlossaryEugenia Lopez Delgado100% (1)
- Healthy Liver Diet To Lower SGPT & SGOT LevelsDocument1 pageHealthy Liver Diet To Lower SGPT & SGOT LevelsMari PagxNo ratings yet
- Anatomy & Physiology: Essentials ofDocument83 pagesAnatomy & Physiology: Essentials ofHaina Shaine Bacolor100% (1)
- S4 Mock 1 2006 Biology P1Document8 pagesS4 Mock 1 2006 Biology P1cyber sec100% (1)
- Edexcel IGCSE Biology Revision NotesDocument56 pagesEdexcel IGCSE Biology Revision Notespepepepepepe30% (1)
- Copper ToxicityDocument7 pagesCopper ToxicityberlianNo ratings yet
- Jaundice Overview: Bilirubin Red Blood Cells Hemoglobin Molecule Liver Bile MetabolismDocument6 pagesJaundice Overview: Bilirubin Red Blood Cells Hemoglobin Molecule Liver Bile MetabolismManoj GargNo ratings yet
- CT Features of Extrahepatic Arterioportal Fistula in Two CatsDocument4 pagesCT Features of Extrahepatic Arterioportal Fistula in Two CatsVennaOktaviaAnggrainiNo ratings yet