Professional Documents
Culture Documents
1.6.2 Abdominal Examination / Palpation: 1 Antenatal Care 1.6 A P - M
1.6.2 Abdominal Examination / Palpation: 1 Antenatal Care 1.6 A P - M
Uploaded by
Manju Thomas0 ratings0% found this document useful (0 votes)
21 views5 pagesOriginal Title
Antenatal
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views5 pages1.6.2 Abdominal Examination / Palpation: 1 Antenatal Care 1.6 A P - M
1.6.2 Abdominal Examination / Palpation: 1 Antenatal Care 1.6 A P - M
Uploaded by
Manju ThomasCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
WOMEN AND NEWBORN HEALTH SERVICE
King Edward Memorial Hospital
DPMS
Ref: 5268
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual Page 1 of 5
CLINICAL GUIDELINES
SECTION B: OBSTETRICS AND MIDWIFERY
1 ANTENATAL CARE
1.6 ANTENATAL PROCEDURES - MATERNAL
Date Issued: J uly 2001 1.6.2 Abdominal Examination / Palpation
Date Revised: September 2012 Section B
Review Date: September 2015 Clinical Guidelines
Authorised by: OGCCU King Edward Memorial Hospital
Review Team: OGCCU Perth Western Australia
Key words: abdominal palpation, pregnancy
1.6.2 ABDOMINAL EXAMINATION / PALPATION
AI MS
Observe the signs of pregnancy and parity
Assess the fetal size and growth
Detect deviations from the normal
Locate the fetal parts to indicate position and presentation
Auscultate the fetal heart
EQUI PMENT
Doptone
Aqueous gel
Non-stretching tape measure
Wedge as required
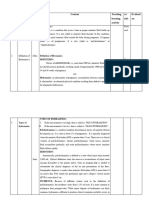
PROCEDURE
ADDITIONAL INFORMATION
1 Preparation
1.1 Perform hand hygiene before and after
patient contact.
See Infection Control Policy, 2.4 Hand
Hygiene.
Ensuring the practitioner has warm hands
may reduce maternal discomfort and risk for
causing contraction of the uterine or
abdominal muscles.
1
1.2 Explain the procedure and gain permission to
proceed.
1.3 Encourage the woman to empty her bladder
prior to the procedure.
A full bladder will make the examination
uncomfortable and can reduce the accuracy
of the fundal height measurement.
1
1.4 Position the woman in the semi recumbent
dorsal position on the bed.
The woman should be encouraged to lie with
her arms by her sides to aid relaxation of the
abdominal muscles.
1
Date Issued: J uly 2001 1.6.2 Abdominal Examination / Palpation
Date Revised: September 2012 Section B
Review Date: September 2015 Clinical Guidelines
Written by:/Authorised by: OGCCU King Edward Memorial Hospital
Review Team: OGCCU Perth Western Australia
DPMS
Ref: 5268
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual Page 5 of 5
PROCEDURE
ADDITIONAL INFORMATION
Consider placing a wedge under the right
buttock if the gravid uterus is of a size likely
to compromise maternal and/or fetal
circulation.
Pelvic tilt prevents occurrence of supine
hypotension resulting from the weight of the
gravid uterus obstructing the inferior vena
cava reducing venous return and hence
cardiac output.
1.5 Ensure the woman is appropriately covered. The womans modesty and privacy is
respected.
2
2 Visual Inspection
2.1 Note the abdominal size. A full bladder, distended colon, or maternal
obesity may effect estimation of fetal size.
1
2.2 Observe the abdominal shape. An abdominal shape that is longer than it is
wide indicates a longitudinal lie. However, a
shape that is low and broad may point to a
transverse lie.
1
The primigravid uterus is ovoid in shape
compared to the multigravid uterus, which is
a rounded shape. Dips and curves in the
uterus may indicate fetal position.
3
2.3 Inspect the abdomen for scars. Presence of scars may indicate previous
abdominal or obstetric surgery.
1
2.4 Examine the skin. Hormonal influences in pregnancy can cause
striae gravidarum, hyper-pigmentation,
changes in nails, hair, and the vascular
system.
4
Striae gravidarum caused by physical and
hormonal influences is more common in
younger women, those with higher body
mass indices, and in women carrying larger
babies.
4
Daily massage may prevent stretch
marks, however there is no evidence to
indicate the use of which creams, emollients
and oils prevent occurrence.
5
2.5 Observe for fetal movements.
3 Estimating gestation age
3.1 Palpate of the abdomen by using the
physical landmarks of the xiphisternum, the
umbilicus and the symphysis pubis.
Macrosomia, multiple pregnancy and small
for gestation age may be detected by
palpation and measurement of fundal height.
Current evidence does not indicate that
either the palpation method, or measurement
of fundal height method, is superior to each
other for detection of abnormal fetal growth.
6
If a small for gestational age fetus is
suspected, then confirmation of the
estimated gestational age should be
revisited.
1, 7
Date Issued: J uly 2001 1.6.2 Abdominal Examination / Palpation
Date Revised: September 2012 Section B
Review Date: September 2015 Clinical Guidelines
Written by:/Authorised by: OGCCU King Edward Memorial Hospital
Review Team: OGCCU Perth Western Australia
DPMS
Ref: 5268
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual Page 5 of 5
PROCEDURE
ADDITIONAL INFORMATION
3.2 Measure the fundal height with the tape
measure.
See Clinical Guideline, Section B 1.6.3
Measuring the Fundal Height with a Tape
Measure.
Between 20 to 34 weeks gestation the height
of the uterus correlates closely with
measurements in centimetres, however
obesity has been shown to distort the
accuracy of these measurements
8
4 Palpation Summary
4.1 Fundal Palpation
Both hands are gently placed around the
fundus to determine contours of the fetus.
Aids determination of presentation, whether
cephalic or breech. This will aid diagnosis of
the lie and presentation of the fetus.
1
4.2 Lateral Palpation
Hands are placed at umbilicus level on either
side of the uterus. Gentle pressure is used
with each hand to determine which side
offers the greatest resistance. Walking the
fingers over the abdomen can also locate the
position of the back and distinguish fetal
body parts.
1
Location of the fetal back can help determine
the fetal position.
1
4.3 Pelvic Palpation
Ask the woman to bend her knees slightly
and encourage gentle breathing exercises.
A woman in a relaxed position is less likely to
tense abdominal muscles.
1
To confirm presentation and engagement the
midwife:
faces towards the womans feet
places both hands on either side of
the presenting uterine pole and
palpates gently starting at least 10cm
above the symphysis pubis moving
downwards towards it.
identifies the level and side of the
occiput and sinciput when the
presentation is vertex. In a normal
vertex presentation the head is
flexed and the sinciput will be
palpated at a higher level than the
occiput.
Pawliks manoeuvre should only be used if
necessary to judge size, flexion and mobility
of the head.
1
This will help identify fetal position, degree of
flexion and how many fifths of the presenting
part is palpable above the pelvic brim.
Assess engagement of the presenting part of
the fetus (defined as no more than 2/5ths
palpable above the pelvic brim).
If the head does not engage (3 or more fifths
above the pelvic brim) in a primigravid
woman at term, it may indicate
malpresentation or cephalopelvic
disproportion (CPD).
1
However, non-
engagement is not definitive of CPD. Risk
factors should be discussed with the woman.
Date Issued: J uly 2001 1.6.2 Abdominal Examination / Palpation
Date Revised: September 2012 Section B
Review Date: September 2015 Clinical Guidelines
Written by:/Authorised by: OGCCU King Edward Memorial Hospital
Review Team: OGCCU Perth Western Australia
DPMS
Ref: 5268
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual Page 5 of 5
PROCEDURE
ADDITIONAL INFORMATION
A midwife should notify the Obstetric Team if
a primigravid woman has a high vertex
presentation at term and risk of CPD is
suspected.
5 Auscultation
5.1 Locate the fetal heart by identifying the fetal
position and presentation.
Use of a hand held Doppler allows the
woman to hear the fetal heart rate (FHR).
7
5.2 Identify the maternal pulse. The maternal pulse should be identified to
confirm the abdominally detected rate is that
of the fetus, not the woman.
3
5.3 Auscultate the fetal heart rate for one minute
and record in the womans medical record.
The fetal heart rate varies according to
gestational age and activity.
5.4 Report any deviation or irregularity in the
FHR to the medical staff.
A reassuring heart rate is between 110 and
160 beats per minute, with no irregularities.
3
6 Amniotic Fluid Estimation
Assess amniotic fluid volume.
Discuss with the Obstetric Team if an
abnormality is detected.
With oligohydramnios the uterus may feel
small and compact and the fetal parts may
be easily palpated.
It may be associated with renal agenisis or
Potters syndrome, fetal abnormality, and
pre-labour rupture of membranes.
9
With polyhydramnios the uterus may be
larger than expected, the skin may appear
stretched and shiny, and the uterus feels
tense to palpate.
Polyhydramnios may be associated with
oesophageal duodenal atresia, multiple
pregnancy, open neural tube defects,
diabetes mellitus and an anencephalic fetus.
1
7 Documentation
Document the findings on palpation, fetal
activity, and the FHR in the womans medical
records.
REFERENCES
1. Viccars A. Antenatal care. In: Fraser DM, Cooper MA, editors. Myles Textbook for Midwives. 15th ed.
London: Churchill Livingstone; 2009. p. 263-87.
2. Grigg C. Working with with women in pregnancy. In: Pairman S, Pincombe J , Thorogood C, Tracy S,
editors. Midwifery preparation for Practice. Sydney: Churchill Livingstone; 2010. p. 431-68.
3. Baston H. Midwifery Basics. Monitoring fetal wellbeing during routine antenatal care. Practicing
Midwife. 2003;6(4).
Date Issued: J uly 2001 1.6.2 Abdominal Examination / Palpation
Date Revised: September 2012 Section B
Review Date: September 2015 Clinical Guidelines
Written by:/Authorised by: OGCCU King Edward Memorial Hospital
Review Team: OGCCU Perth Western Australia
DPMS
Ref: 5268
All guidelines should be read in conjunction with the Disclaimer at the beginning of this manual Page 5 of 5
4. Tunzi M, Gary R, Grey DO. Common Skin Conditions During Pregnancy. American Family Physician.
2007;75:211-18.
5. Young G, J ewell D. Creams for preventing stretch marks in pregnancy. The Cochrane Database of
Systematic reviews. 2010(2).
6. J aparaj RP, Ho J J , Vallipan J , Sivasangari S. Symphysial fundal height (SFH) measurement in
pregnancy for detecting abnormal fetal growth. The Cochrane Database of Systematic reviews.
2012(7).
7. Campbell S, Lee C. Obstetrics by Ten Teachers. London: Hodder Arnold; 2006.
8. Cunningham FG, Hauth J C, Leveno KJ , et al, editors. Williams Obstetrics. New York: McGraw-Hill;
2005.
9. Crafter H. Problems of pregnancy. In: Fraser DM, Cooper MA, editors. Myles Textbook for Midwives.
15th ed. Sydney: Churchill Livingstone; 2009. p. 333-59.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Amniotic FluidDocument32 pagesAmniotic FluidFahad KhanNo ratings yet
- Amniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfDocument2 pagesAmniotic Fluid Index (AFI) - StatPearls - NCBI BookshelfTarzan SmithNo ratings yet
- MK Polyhydramnios and Oligohydramnios (OBGY)Document14 pagesMK Polyhydramnios and Oligohydramnios (OBGY)Moses Jr KazevuNo ratings yet
- ULTRASOUND Abdomen Normal MeasurementsDocument20 pagesULTRASOUND Abdomen Normal Measurementsadinatop100% (3)
- Assessment of Amniotic Fluid Volume - UpToDateDocument19 pagesAssessment of Amniotic Fluid Volume - UpToDateJUAN FRANCISCO OSORIO PENALOZANo ratings yet
- Aberrant Liquor VolumeDocument37 pagesAberrant Liquor VolumeDoaaNo ratings yet
- Amniotic Fluid Disoder: Muhammad IzzatDocument26 pagesAmniotic Fluid Disoder: Muhammad IzzatcopperNo ratings yet
- Amniotiv Fluid DisorderDocument22 pagesAmniotiv Fluid DisorderLiangkiuwiliu100% (1)
- OligohydramniosDocument9 pagesOligohydramniosDeepika Patidar0% (1)
- Hydramnios NewDocument11 pagesHydramnios NewSpandana DepuruNo ratings yet
- Polyhydramnios & Oligohydramnios: Prepared By: Hamzah Qarawi To: Miss Mahdia KonyDocument37 pagesPolyhydramnios & Oligohydramnios: Prepared By: Hamzah Qarawi To: Miss Mahdia KonyNinaNo ratings yet
- Amniotic FluidDocument34 pagesAmniotic Fluidannu panchalNo ratings yet
- PolyhydramniosDocument2 pagesPolyhydramniosAde Yonata100% (1)
- Care of The Woman With Complications During LaborDocument20 pagesCare of The Woman With Complications During LaborJanelle Cabida SupnadNo ratings yet
- HydramniosDocument31 pagesHydramniosSpandana DepuruNo ratings yet
- OSCE On 14/3/2008: Describe Gynaecoid PelvisDocument82 pagesOSCE On 14/3/2008: Describe Gynaecoid PelvisKahing LiNo ratings yet
- Hydramnios: (Maternal and Child Nursing)Document10 pagesHydramnios: (Maternal and Child Nursing)Angelika AgmataNo ratings yet
- Polyhydramnios & Oligiohydramnios: Prof. Yasmin RaashidDocument11 pagesPolyhydramnios & Oligiohydramnios: Prof. Yasmin RaashidShimmering MoonNo ratings yet
- 18 - Oligohydramnios and PolyhydramniosDocument3 pages18 - Oligohydramnios and PolyhydramniosSu OoNo ratings yet
- Quiz 5 Test BankDocument37 pagesQuiz 5 Test BankOnyeka O AniyedeNo ratings yet
- AnhydramnionDocument3 pagesAnhydramnionNi Wayan Ana PsNo ratings yet
- Questions 5 To 8Document26 pagesQuestions 5 To 8Stefannus Wibisono100% (1)
- 2 PolyhydramniosDocument8 pages2 PolyhydramniosNovhy GanggutNo ratings yet
- Infant of Diabetic MotherDocument17 pagesInfant of Diabetic Motheral_humaira91No ratings yet
- Polyhydramnios (Revised)Document34 pagesPolyhydramnios (Revised)Edward Munyaradzi KutsanziraNo ratings yet
- 29 - Amniotic Fluid Volume DisordersDocument13 pages29 - Amniotic Fluid Volume DisordersAbdelrahman ElsaadawiNo ratings yet
- Management of A Case of Hydramnios and Oligohydramnio1Document12 pagesManagement of A Case of Hydramnios and Oligohydramnio1Easter Soma HageNo ratings yet
- Amniotic FluidDocument5 pagesAmniotic FluidPat Cabanit0% (1)
- CURS 5 Abnormalities of The Umbilical Cord and Amniotic FluidDocument33 pagesCURS 5 Abnormalities of The Umbilical Cord and Amniotic FluidFayad AlmohamedNo ratings yet
- Ward TeachingDocument23 pagesWard Teachingvani reddyNo ratings yet