Professional Documents
Culture Documents
Sepsis Induced Cholestasissssssss
Sepsis Induced Cholestasissssssss
Uploaded by
wizardebmCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sepsis Induced Cholestasissssssss
Sepsis Induced Cholestasissssssss
Uploaded by
wizardebmCopyright:
Available Formats
REVIEW
Sepsis-Induced Cholestasis
Nisha Chand and Arun J. Sanyal
J
aundice and hepatic dysfunction frequently accom-
pany a variety of bacterial infections. The relationship
between sepsis and jaundice, particularly in a pediat-
ric population, was reported as early as 1837.
1
Jaundice
may result either directly from bacterial products or as a
consequence of the hosts response to infection. Fre-
quently, both factors contribute to the development of
jaundice. In addition, specic infections that target the
liver may cause jaundice because of the liver injury asso-
ciated with hepatic infection. Although jaundice may be
an isolated abnormality, it is often associated with features
of cholestasis. In critically ill patients, the development of
jaundice and/or cholestasis complicates the clinical pic-
ture and poses a clinical challenge both in diagnostic eval-
uation and in management. In this article, we review the
current concepts about the pathogenesis of jaundice and
cholestasis with infection, their clinical presentation and
diagnostic assessment, and the optimal management of
these clinical problems.
Epidemiologic Considerations
Jaundice is a well-known complication of sepsis or ex-
trabacterial infection. Sepsis and bacterial infection are
responsible for up to 20% of cases of jaundice in patients
of all ages in a community hospital setting.
2
The inci-
dence of jaundice in newborns and early infants varies
between 20% and 60%.
3
There are no data from large-
scale prospective studies on the incidence of hyperbiliru-
binemia in adults with sepsis. Several small retrospective
studies have reported widely varying numbers, from0.6%
to 54%. This variability probably reects both the report-
ing bias and the populations of subjects studied (Table
1).
4,5
Sepsis is more likely to manifest with jaundice in
infants and children than in adults. In this population,
males have a higher incidence of jaundice. However, in
adults, no gender predilection has been reported.
Jaundice has been associated with infections caused by
several organisms including aerobic and anaerobic gram-
negative and gram-positive bacteria. Gram-negative bac-
teria cause most of these cases. The primary site of
infection is most often intraabdominal, but infection of
various other sites such as urinary tract infection, pneu-
monia, endocarditis, and meningitis have been associated
with this complication.
4,6,7
Other specic infections
known to cause jaundice are infections of the hepatobili-
ary tree, clostridial infection, typhoid fever, and legio-
nella.
Although jaundice can occur in isolation in patients
with septicemia, it is frequently associated with other el-
ements of cholestasis. Because the principal clinical man-
ifestation of cholestasis is also jaundice, the published
literature has primarily focused on the syndrome of jaun-
dice, and the exact incidence of cholestasis with jaundice
versus isolated jaundice remains unclear.
Pathophysiology
The pathogenesis of jaundice in systemic infections
is multifactorial. The development of jaundice may
occur from an aberration in the processing of bilirubin
by hepatocytes or from other effects on the liver that
lead to the accumulation of bilirubin in the body. Such
processes include increased bilirubin load from hemo-
lysis, hepatocellular injury, and cholestasis from the
septic state and from various drugs used for the treat-
ment of sepsis. The molecular and biochemical mech-
anisms by which jaundice develops in subjects with
sepsis is best considered in the context of normal bili-
rubin metabolism.
Normal Bilirubin Metabolism
Bilirubin is the end product of the breakdown of the
heme moiety of hemoproteins. In humans, 4 mg of bili-
rubin is formed daily from the degradation of hemopro-
teins, 80% of which is derived from hemoglobin.
8
Unconjugated bilirubin is a highly hydrophobic molecule
and circulates tightly but reversibly bound to albumin in
Abbreviations: AHA, autoimmune hemolytic anemia; BSEP, bile salt export
pump; BSP, tetrabromosulfophthalein; cMOAT, multispecic organic anion trans-
porter; DIC, disseminated intravascular coagulation; IL, interleukin; KCs, Kupffer
cells; LPS, lipopolysaccharide; MRP2, multidrug-resistance-associated protein; NO,
nitric oxide; NTCP, sodium-dependent taurocholate cotransporter; OATP, organic
anion transport protein; RBC, red blood cells; RES, reticuloendothelial system;
SLCT, sulfolithocholyltaurine; TNF, tumor necrosis factor.
From the Division of Gastroenterology, Hepatology and Nutrition, Department
of Internal Medicine, Virginia Commonwealth University Medical Center, Rich-
mond, VA.
Received May 28, 2006; accepted October 16, 2006.
Address reprint requests to: Dr. Arun J. Sanyal, Professor of Medicine, Pharma-
cology and Pathology, Virginia Commonwealth University Medical Center, MCV
Box 980341, Richmond, VA 23298-0341. E-mail: ajsanyal@hsc.vcu.edu; fax:
804-828-4945.
Copyright 2006 by the American Association for the Study of Liver Diseases.
Published online in Wiley InterScience (www.interscience.wiley.com).
DOI 10.1002/hep.21480
Potential conict of interest: Dr. Sanyal received grants from Sano-Aventis and
Debiorision.
230
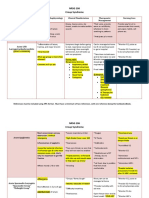
plasma. Figure 1 shows normal bilirubin metabolism at
the hepatocyte. Bilirubin dissociates from albumin at the
sinusoidal, basolateral membranes of hepatocytes and is
taken up inside in a carrier-mediated process that requires
inorganic anions such as Cl
.
6,9,10
Organic anion trans-
port proteins (OATPs) are on the basolateral membranes
of hepatocytes.
11
Their role in bilirubin transport has still
not been directly established, but bilirubin is a presumed
substrate of OATPs.
12
Following uptake into a hepatocyte, bilirubin is
bound by a group of cytosolic proteins (mainly gluta-
thione S-transferases, GST) that prevent its efux
from the cell. Within a hepatocyte, bilirubin is conju-
gated to monoglucuronides and diglucuronides by the
enzyme uridine diphosphate-glucuronosyltrans-
ferase.
13
Conjugation of bilirubin converts it from a
highly hydrophobic molecule to a relatively hydro-
philic molecule that can be excreted into bile.
6,9
Bili-
rubin glucuronides are excreted into bile against a steep
concentration gradient by a canalicular membrane pro-
tein, the canalicular multispecic organic anion trans-
porter (cMOAT), also commonly referred to as the
multidrug-resistance-associated protein (MRP2).
6,9,14
This process is the major driving force of bilirubin
transport and is the rate-limiting step in bilirubin ex-
cretion by the liver.
15
Table 1. Reports of Jaundice and Sepsis
Author (Year) N M/F Age TB/DB (mg %) Alk Phos ALT/AST Agents of Infection Bacteremia Site of Infection Deaths Notes
Bernstein et al.
(1962)
9 8/1 2-8 weeks 12-22/4-7 E. coli (5) 8 UTI (4) 9
Paracolon (2)
P. Aeruginosa (1)
Streptococcus (grp A)
Hall et al. (1963) 11 10/1 15-65 years 2-17/.4-14 5-21 (KA
U/100
mL)
Gr. Diplococci (5) Lungs (11) 2
Hamilton et al. (196) 24 13/11 1 day-13
weeks
3-31/1-16 E. coli (18) 18 Urine (16) 11
A. Aeruginosa (4) Umbilicus (2)
Eye (1)
Kibukamusoke et al.
(1964)
21 21/0 17-65 years 3-27 8-19 (KA
U/100
mL)
8-150/13-150 Lungs (21) 1
Eley et al. (1965) 5 2/3 35-54 years 3-23/8-15 11-26 (KA
U/100
mL)
16-34/24-88
(U/ml)
Str. pyogenes (2) 3 Intraabdominal (4) 1
E. coli (1) UTI (1)
Proteus (1)
Bacteroids (1)
Vermillion et
al.(1969)
7 4/3 18-72 years 5-24/4-16 3-26
(mU/
mL)
1-3 (IU/ml) E. coli (3) 7 Lung (3) 6
Streptococcus (3) Intraabdominal (2)
Pseudomonas (2) Pleural (1)
S. aureus (2)
Miller et al. (1969) 9 1.2-2.5 E. coli (8) Appendicitis (9) 0
Rooney et al. (1971) 22 19/3 1-3 weeks 7-50/1-37 E. coli (14) 19 UTI (9) 0
Proteus (3) CSF (1)
Klebsiella (2) Umbilical (1)
Miller et al. (1976) 30 15/15 15-27 years 2-20 (DB mean
6.78)
mean 128 mean 47.6 S. aureus (4) 11 Pneumonia (9) 13
P. aeruginosa (2) UTI (6)
Paracolon Peritonitis (6)
Klebsiella (6) Soft tissue (4)
Ng et al. (1971) 6 6/0 2-8 weeks 4-33/3-21 20-41 (KA
U/100
mL)
E. coli (5) 4 UTI (6) 0
Paracolon (1)
Borges et al. (1972) 13 8/5 2 months-3
years
3-31/2-14 28-300/50-920
(U/mL)
E. coli (5) UTI (10) 0
Proteus (5) Lung (4)
Streptococcus (2)
Staphlyococcus (2)
Franson et al. (1985) 23 10/13 25-77 years 2-24/2-14 56-1694 23-3300 E. coli (8) 23 Lung (8) 14
Klebsiella (3) Abdominal cavity
(5)
Staphylococcus (6) UTI (4)
Streptococcus (2) IV catheter/graft/
skin (3)
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 231
Disorders of Bilirubin Metabolism During
Systemic Infection
Various mechanisms can lead to hyperbilirubinemia
alone during systemic infection (Table 2). These are dis-
cussed in detail in the following sections.
Increased Bilirubin Load/Hemolysis
The development of hemolysis causes an increased bil-
irubin load in septic individuals. In early studies, hemo-
lysis was believed to be the principal mechanism of
jaundice in sepsis.
16
Using light microscopy, Tugswell et
al. found excess iron-containing pigment in the liver of
patients with pneumonia and noted ferritin containing
lysosomes in Kupffer cells.
17
This was believed to be com-
patible with hemolysis and secondary iron overload. Al-
though hemolysis contributes to jaundice in sepsis, it is
unlikely that it is the principal mechanism because the
jaundice results fromconjugated hyperbilirubinemia.
18-20
Table 3 lists various mechanisms of hemolysis in the set-
ting of sepsis.
Hemolysis may occur by multiple mechanisms in the
setting of bacterial infection.
21-22
These may be catego-
rized as mechanisms of hemolysis (1) associated with nor-
mal red cells and (2) related to underlying red cell defects.
The severe forms of many infections from gram-posi-
tive and gram-negative bacteria have been associated with
hemolysis of normal red cells. Of these bacteria, Clostrid-
ium perfringens can give rise to severe, often fatal hemoly-
sis in persons with normal red cells.
23-24
Cl. perfringens
produces phospholipase C, a lecithinase that reacts with
red cell membrane lipoproteins to release lysolecithin,
which, in turn, lyses red cell membranes, producing he-
molysis.
25
In addition, this bacterium also produces pro-
teolytic exotoxins that cause enzymatic dissolution of
membrane proteins.
26
Other infections that commonly
cause hemolysis in normal red cells are malaria and babe-
siosis.
27
Escherichia coli infection periodically may lead to
hemolysis of normal red blood cells (RBCs).
28
Aside from
bacterial infection directly causing hemolysis, multiple
drugs (e.g., penicillin, antimalarial medications, sulfa
medications, or acetaminophen), hypersplenism from in-
fection, portal hypertension, or neoplasmcan increase the
sequestration and phagocytosis of erythrocytes.
21,28
Immunologically mediated red cell injury is another
mechanism by which hemolytic anemia occurs in normal
RBCs of patients with sepsis. Overall, infections account
for about 8% of cases of autoimmune hemolytic anemia
(AHA) and for approximately 27% of such cases in chil-
dren.
22
Immunologically mediated hemolysis may de-
velop by 3 mechanisms: antibody directed to red cell
Fig. 1. Normal bilirubin metabolism. Bilirubin dissociates from al-
bumin at the sinusoidal surface of the hepatocyte and is taken up by the
hepatocyte. Inside the hepatocyte, bilirubin is bound by a group of
cytosolic proteins that prevent its efux from the cell. Bilirubin is then
conjugated to monoglucuronides and diglucuronides by the enzyme
uridine diphosphate-glucuronosyltransferase. Bilirubin glucuronides are
excreted into bile against a steep concentration gradient by a canalicular
membrane protein termed canalicular multispecic organic anion trans-
porter (cMOAT), also commonly referred to as the multidrug-resistance-
associated protein (MRP2). This process is the major driving force of
bilirubin transport and is the rate-limiting step in bilirubin excretion by the
liver.
Table 2. Mechanisms of Hyperbilirubinemia in Sepsis
1. Hemolysis
a. In normal red cells
b. In RBCs with red cell enzyme defects (G6PD)
c. Pathologic changes to RBCs secondary to infection
d. Drug-induced hemolysis
2. Hepatic dysfunction
a. Decreased bilirubin uptake
b. Decreased canalicular transport
c. Decreased clearance of conjugated bilirubin
d. Hepatic ischemia
i. Hypotension
ii. Prolonged Hypoxia
e. Hepatocellular injury (mild reactive hepatitis to overt hepatocellular
necrosis)
3. Cholestasis
Table 3. Mechanisms of Hemolysis in Sepsis
1. Normal RBCs
a. Infections directly causing hemolysis (e.g. Clostridium perfringens)
b. Immunologically mediated red cell injury
1. Cold agglutininassociated hemolytic anemia
a. Mycoplasma pneumoniae
b. Legionella
2. Paroxysmal cold hemoglobinuria
c. Drug-induced hemolysis
d. Transfusion reactions
e. Hypersplenism
2. Underlying red blood cell defects
a. Inherited enzyme deciency
b. Sickle cell disease
c. Hemoglobinopathies
232 CHAND AND SANYAL HEPATOLOGY, January 2007
antigens (IgM or IgG mediated), antigen/antibody com-
plexes, or polyagglutination.
22
IgM antibodies give rise to
intravascular hemolysis, and IgG antibodies give rise to
extravascular hemolysis.
22
Several pathogens, for example, Mycoplasma pneumoniae
and Legionella may cause cold agglutininassociated he-
molytic anemia.
22,25
The cold agglutinins, which are often
IgMs, bind to red cells at lowtemperatures, x complement,
and cause intravascular hemolysis. On the other hand, IgG
antibodies, for example, Donath-Landsteiner antibodies in
paroxysmal cold hemoglobinuria, often cause extravascular
hemolysis. This condition has been associated with upper
respiratory tract infections and a variety of infections that
normally do not lead to sepsis syndrome, for example, syph-
ilis, varicella, Epstein-Barr, measles, and mumps.
22,25,29
He-
molysis and jaundice fromparoxysmal cold hemoglobinuria
may be severe in cold weather.
In individuals with underlying red cell defects, the
threshold for hemolysis is often lower than in normal
individuals. A common defect associated with an in-
creased propensity for hemolysis in a variety of circum-
stances including sepsis is glucose-6-phosphate
dehydrogenase (G-6-PD) deciency.
1
Many types of in-
fections as well as antibiotics can cause hemolytic anemia
in patients with this deciency. G-6-PD is required for
regeneration of nicotinamide adenine dinucleotide dehy-
drogenase (NADPH), which is essential for reducing the
amount of oxygen radicals.
30
In the absence of G-6-PD,
red cell NADPH stores are diminished, thereby lowering
the threshold for oxidant-stress-mediated cell injury. Sep-
sis is often associated with oxidant stress, and this may
induce hemolysis, particularly in those with a lowered
threshold for oxidant-mediated injury.
Microangiopathic hemolytic anemias may be triggeredby
a variety of infections such as Shigella, Campylobacter, and
Aspergillus.
31
Disseminated intravascular coagulation (DIC)
may also cause hemolysis with infections; up to 60% of all
cases of DIC have been attributed to infections, with many
bacterial, viral, fungal, and parasitic pathogens implicated.
25
Drugs are a major cause of hemolysis in patients with
sepsis (Table 4).
31,32
This occurs through a variety of
mechanisms,
34
an apparently major one of which is in-
creased oxidant stress. Finally, hemolysis of nonviable
erythrocytes may occur during massive blood transfu-
sions, resorption of large hematomas, or trauma. These
additional factors are commonly encountered in patients
with sepsis in the ICU.
Hepatocyte Dysfunction as a Cause of
Hyperbilirubinemia
In addition to increased bilirubin load, decreased bili-
rubin uptake, intrahepatic processing, and canalicular ex-
cretion are also important mechanisms of jaundice
associated with infection. This is supported by the mainly
conjugated hyperbilirubinemia that occurs in sepsis.
Many studies have examined the effects of sepsis on the
function of organic anion transporters in the liver. Tetra-
bromosulfophthalein (BSP) is taken up by hepatocytes by
the sodium-independent transport system, the basolateral
OATP.
12
Bilirubin is a presumed substrate for this trans-
porter system.
12
Hepatic uptake of BSP is reported to be
markedly lower in lipopolysaccharide (LPS)-treated ani-
mals. BSP, glutathione, and sulfolithocholyltaurine
(SLCT) are excreted at the canalicular membrane through
MRP2.
12
There is also a decrease in canalicular transport
of glutathione and SLCT, suggesting decreased MRP2
activity. Roelofsen et al. studied the transport of bilirubin
in a rat model of sepsis.
9
In this study, LPS was injected
into rats intravenously to induce endotoxemia. The trans-
port of bilirubin and another organic acid, taurocholate,
were studied 18 hours after the infusion. Sinusoidal up-
take, hepatic content, and canalicular excretion of biliru-
bin were all decreased in endotoxemic rats compared to in
control animals.
9
Also, a 50% decrease in steady-state
elimination of bilirubin was observed in livers exposed to
endotoxin.
6,9
It is unlikely that bilirubin conjugation is substantially
affected by sepsis because more than 60% of the bilirubin
in blood is conjugated.
9
Also, when endotoxin was ad-
ministered to rats, the clearance of conjugated bilirubin
decreased to the same degree that unconjugated bilirubin
did, suggesting that the conjugation of bilirubin was not
contributing to the impairment in bilirubin clearance.
9
This is further supported by the nding that the degree of
bilirubin conjugation in livers exposed to endotoxin was
not substantially different from normal controls.
9
Decreased Bile Flow
Cholestasis is the predominant mechanism by which
jaundice develops in sepsis. Extrahepatic cholestasis is
Table 4. Antibiotics Associated with Hemolysis
Immune Complex Mediated
Quinine
Autoantibody Medicated
Sulfonamides
Penicillin
Cephalosporins
Indinivir
Hemolyis in G6PD
Nitrofurantoin
Phenazopyridine
Primaquine
Sulfonamides
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 233
caused by obstruction of the hepatic or common bile duct
and directly impedes the owof bile. This can result from
a primary infection such as cholangitis or can become
secondarily infected. Partial biliary obstruction and ob-
struction as a result of cholelithiasis are more commonly
complicated by infection of the biliary tree, which could
further lead to decreased bile ow.
Sepsis-Associated Cholestasis
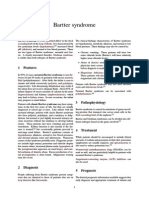
Normal Bile Acid Flow
Before elaborating on the potential mechanisms of
cholestasis in sepsis, it is important to understand the
steps in the formation of bile (Fig. 2). Bile is formed by the
inow of water along osmotic gradients produced by se-
cretion of bile salts into hepatic canaliculi. Bile salts are
the principal solute secreted into this space, and bile ow
is mainly driven by the osmotic forces generated by the
secretion of bile salts into hepatic canaliculi. This is also
known as bile-salt-dependent bile ow, whereas the gen-
eration of bile fromosmotic forces related to other solutes
is known as bile-salt-independent ow.
Bile salts are derived from de novo synthesis in the liver
and fromreabsorption of bile salts fromthe intestine. Bile
acids are transported to the liver following intestinal ab-
sorption. They are taken up by hepatocytes via transport
proteins on the basolateral (sinusoidal) membranes. The
principal mediator of this basolateral transport of bile ac-
ids is the Na-K-ATPase pump, which is ATP dependent
and maintains an inwardly directed sodium gradient. It is
an integral component of the basolateral membrane, and
Na-K-ATPase pumps are found throughout the hepatic
lobule. Sodium-dependent taurocholate cotransporter
(NTCP) is the principal transporter in the uptake of con-
jugated bile salts from plasma into hepatocytes.
35
This
highly efcient pathway results in a high rst-pass clear-
ance of bile salts. The unconjugated bile salt cholate, or-
ganic ion sulfobromophthalein (BSP), and other
lipophilic compounds are primarily transported from
plasma into hepatocytes by sodium-independent trans-
port systems such as organic anion transport proteins
OATP 1, OATP 2, and OATP 3.
35
Bile acids are transported from the basolateral mem-
brane to the canalicular membrane by cytosolic trans-
porter proteins. Transcytosolic transport occurs through
2 main methods: (1) binding to cytosolic proteins and
diffusing to apical domains (mainly conjugated primary
and secondary bile acids) and (2) vesicular trancytosis.
Vesicular transport is responsible for a very small amount
of total bile ow, and the role of this type of transport is
unclear.
The passage of bile salts into biliary canaliculi is the
rate-limiting step in bile formation. This passage is mostly
ATP dependent and occurs against a steep concentration
gradient. There are many ATP-dependent transporters on
the canalicular membrane. Among these are the multi-
drug resistance family and the bile salt export pump
(BSEP). Conjugated bile salts are excreted into bile
through the BSEP. The multiple drug resistance 1 trans-
porter is responsible for transporting hydrophobic or-
ganic cations.
36
Water and inorganic ions enter bile by
diffusion across tight junctions, which provide a barrier
for bile salts, prohibiting the regurgitation of formed bile
into the space of Disse.
Mechanisms and Mediators of Cholestasis Associated
with Infections
The liver has a central role in the regulation of host
defenses. It serves as a source of inammatory mediators
and is a major site of the removal of bacteria and endo-
toxins from systemic circulation.
37-38
Kupffer cells (KCs)
of the liver make up 80%-90% of the xed-tissue macro-
phages of the reticuloendothelial system (RES) and rep-
resent terminally differentiated macrophages. KCs take
up bacteria, particles, and endotoxins (LPS) and are stim-
ulated to release a wide range of products implicated in
liver injury, such as tumor necrosis factor, interleukin 1
and interleukin 6, superoxides, lysosomal enzymes, pro-
coagulants, and platelet-activating factor.
9,39-41
Hepatic injury without biliary obstruction may accom-
pany systemic infection in adults with pneumococcal
pneumonia, streptococcal bacteremia, salmonella infec-
Fig. 2. Normal bile acid ow and bile formation. Bile acids are
transported from the basolateral membrane to the canalicular membrane
by cytosolic transporter proteins. Transcytosolic transport occurs by 2
main methods: (1) binding to cytosolic proteins and diffusion to apical
domains (mainly conjugated primary and secondary bile acids) and (2)
vesicular trancytosis. The passage of bile salts into the biliary canaliculus
is the rate-limiting step in bile formation, which is ATP dependent.
Conjugated bile salts are excreted into bile through the BSEP. The
multiple drug resistance 1 (MDR1) transporter is responsible for trans-
porting hydrophobic organic cations across the canalicular membrane.
The tight junctions between hepatocytes provide a barrier to bile salts,
prohibiting the regurgitation of formed bile into the space of Disse.
234 CHAND AND SANYAL HEPATOLOGY, January 2007
tions (especially typhoid fever), and Escherichia coli bac-
teremia.
42
This can range from mild reactive hepatitis to
overt hepatocellular necrosis that, it has been shown, usu-
ally resolves when the bacteremia is appropriately treated.
Hepatocellular injury is not considered a frequent occur-
rence during extrahepatic bacterial infection. Most stud-
ies that reviewed liver histology in hyperbilirubinemia or
hepatic abnormalities in bacterial infection have noted
very mild to no inammation (see Table 1).
20
The mech-
anism of hepatic injury depends on the underlying infec-
tion, yet most likely there is an unspecied toxin
elaborated by the offending bacteria that ultimately leads
to hepatocellular injury.
20,42
Ischemic liver damage may occur as a consequence of
hypotension or prolonged hypoxia in sepsis. Hepatic
blood ow is depressed in sepsis and nutrient blood ow
to the liver is reduced, which can lead to Kupffer cell
dysfunction and hepatocellular alteration.
43
The lack of
oxygen, mainly to the centrizonal cells and later from
delivery of oxygen-derived free radicals from reperfusion,
leads to hepatocellular damage and thus may result in
centrilobular necrosis of the liver.
4,44,45
Mediation of hep-
atocellular injury via necrosis and/or apoptosis has been
attributed to nitric oxide (NO). This was demonstrated in
septic animal models when inhibition of NO production
gave rise to reductions in both hepatocyte necrosis and
apoptosis.
46
The underlying state of endotoxemia and the prod-
ucts released in response to infection appear to play a
key role in the pathophysiology of the cholestasis of
sepsis. Various effects of this state on the liver that lead
to cholestasis are listed in Table 5. Decreased hepato-
cellular function has been demonstrated to occur early
after the onset of sepsis despite increased cardiac out-
put and hepatic perfusion.
47
This suggests that the hep-
atocellular dysfunction in sepsis may be associated with
the release of proinammatory cytokines such as tumor
necrosis factor alpha (TNF-) or interleukin 6 (IL-
6).
47-48
Various investigations have conrmed the cen-
tral role of endotoxemia in the genesis of cholestasis
associated with sepsis.
41
Direct invasion of the liver by
bacteria is not a major cause of cholestasis or hepatic
injury in most cases of septicemia.
41
Several studies
have shown a quantitative reduction in bile ow within
the isolated perfused livers of rats following LPS or
cytokine administration.
TNF- is a cytokine released by macrophages, endo-
thelial cells, and Kupffer cells and is the primary mediator
of the systemic effects of endotoxins. TNF- has been
implicated in endotoxin-induced cholestasis by the nd-
ing that immunization with anti-TNF- antibodies
blocked endotoxin-associated reduction in bile ow and
bile salt excretion.
49
LPS, TNF-, and interleukins 1
and 6 all have been shown to mediate these effects, giving
rise to cholestasis in the liver.
6,50
Procoagulants released
by activated Kupffer cells induce microvascular thrombo-
sis and have been postulated to cause circulatory distur-
bance, which, in turn, could contribute to endotoxin-
induced hepatic injury.
41
Abnormalities in Bile Acid Formation and Flow
Endotoxemia does not affect bile acid synthesis, cyto-
solic bile acid transport, or the permeability of tight junc-
tions.
51
LPS and cytokines appear to mainly affect
hepatocyte uptake and excretion of bile acids. Table 5 lists
various steps in bile acid transport that possibly are af-
fected in sepsis, thus giving rise to cholestasis. Endotox-
emia decreases the basolateral and canalicular transport of
bile acids (cholate, taurocholate, and chenodeoxycholate)
and organic anions (BSP and the taurine conjugate of
sulfolithocholate).
6,11
It is also postulated that LPS may
stimulate degradation of membrane proteins as well.
50
Several studies have observed endotoxin-induced inhi-
bition of basolateral membrane Na-K-ATPase activ-
ity.
50,52-53
Endotoxin may cause decreased function of
Na-gradient dependent transporters at the basolateral
membrane such as the NTCP.
14,49
It has also been ob-
served that endotoxin affects membrane uidity; this may
be the mechanism involved in reducing Na-K-ATPase
activity after endotoxin administration.
50,54
TNF- and
IL-1 modulate gene expression of transporters NTCP
and BSEP at both the transcriptional and the posttran-
scriptional levels.
12
In a study by Green et al., 16 hours
after intraperitoneal administration of LPS, both protein
expression and functional activity of NTCPs were re-
duced by more than 90%.
50
Impaired hepatocyte transport function has also been
detected at the canalicular level. Cholyltaurine (CT) and
chenodeoxycholyltaurine (CDCT) are substrates for can-
alicular bile acid transporters.
12
ATP-dependent CT and
CDCT transport was markedly decreased in a rat sepsis
model.
51
This appears to result from down-regulation of
transporters at the canalicular membrane.
6,40,51
Table 5. Mechanisms of Cholestasis of Sepsis
Decreased basolateral transport of bile acids
Inhibition of basolateral membrane Na-K-ATPase activity
Decreased basolateral membrane uidity
Down-regulation of transporters
Decreased NTCP function
Decreased canalicular transport of bile acids
Down-regulation of transporters
Decreased BSEP function
Decreased MRP2 function
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 235
Bile-acid-dependent and -independent ows are re-
duced in septic models compared to in controls.
6,49-50
The
main evidence for this is the inhibition of biliary excretion
of GSH and, to a lesser extent, of HCO
3
after LPS
administration.
6,49
Maximum reduction in bile acid ow
occurs 12-18 hours after endotoxin and/or cytokine ad-
ministration.
6
Clinical Syndromes
The jaundice of sepsis is usually cholestatic and can
occur within a few days of the onset of bacteremia and
may even appear before other clinical features of the un-
derlying infection become apparent.
55
In the absence of
intraabdominal infection, abdominal pain is rare. Simi-
larly, pruritus is not a major manifestation of cholestasis
associated with infection. Hepatomegaly occurs about
half the time.
55
Conjugated hyperbilirubinemia in the
range of 2-10 mg/dL is often seen, although rarely higher
levels can be seen.
19
This is particularly true in those with
postoperative jaundice who also are septic and on TPN.
Serum alkaline phosphatase is usually elevated but rarely
more than 2-3 times above the upper limit of normal.
55
Serum aminotransferase is generally only modestly ele-
vated (Table 6).
55
Specic Clinical Scenarios of Infection and Jaundice
Biliary Tract Disease. Obstruction or infection of
the hepatobiliary tree should be considered a potential
cause of jaundice, especially when a patient presents with
right upper quadrant pain, jaundice, and fever. Cholan-
gitis most commonly occurs secondary to obstruction of
the biliary tract with a gallstone or after biliary interven-
tion. Less commonly, cholangitis may occur after obstruc-
tion from a tumor of the ampulla, bile duct, or pancreas.
Laboratory results will show leukocytosis, conjugated hy-
perbilirubinemia, and elevation of alkaline phosphatase
disproportionate to transaminasemia. Acute cholangitis
has a more severe course than jaundice associated with
extrahepatic infections.
Liver Abscess and Pylephlebitis. Biliary tract disease
is the most common condition associated with liver ab-
scess.
56
This includes infection (cholangitis) that may oc-
cur secondary to choledocholithiasis, biliary stricture, or
malignancy.
57
Another potential cause of pyogenic ab-
scess is spread through the portal vein from an intraab-
dominal primary site to the liver.
58
Almost a third of liver
abscesses are cryptogenic.
59
Patients present with fever,
chills, and weight loss. Abdominal complaints most often
are vague or absent. Up to two thirds of patients have
hepatomegaly. Alkaline phosphatase levels are invariably
elevated, with less frequent elevation of bilirubin and ami-
notransferases. Optimal treatment includes prompt diag-
nosis, percutaneous or surgical drainage of the abscess,
and broad-spectrum enteric antibiotic coverage. Progno-
sis depends on prompt recognition and treatment, with a
cure rate ranging from 80% to 100%.
56
ICU Setting. A patient presenting with jaundice in
the ICU is a frequently encountered problem. Infections,
hemodynamic instability, renal insufciency, hepatotoxic
drugs, multiple blood transfusions, and/or TPN admin-
istration are some of the potential causes of jaundice,
which usually presents 1-2 weeks after onset of the initi-
ating event. Jaundice under these circumstances is usually
of a cholestatic type, with mainly conjugated hyperbiliru-
binemia and only slightly elevated ASTand ALT.
43
When
there is no obvious biliary obstruction; underlying sys-
temic infection is highly likely. Sepsis is the most com-
mon etiology of jaundice and cholestasis in the ICU. This
is especially true in patients who are in an ICU due to
trauma. In a retrospective study by Boekhorst et al., the
development of jaundice in the ICU was shown to have a
poor prognosis.
43
This could be a result of a delay in
diagnosis of the instigating factor. If the underlying pro-
cess is detected and adequately treated in a timely fashion,
the prognosis is usually good.
Gram-Negative Bacterial Infections. Cholestasis is a
known complication of gram-negative bacterial infection,
especially in infants. This syndrome is more frequent in
the neonatal period and may account for as much as a
third of the cases of neonatal jaundice.
22
Most cases of
sepsis associated with cholestatic jaundice have evidence
of gram-negative bacteremia, with Escherichia coli the
more common pathogen.
20,60
Pyelonephritis, peritonitis,
appendicitis, diverticulitis, pneumonia, and meningitis
are types of infections observed to cause jaundice. The
urinary tract is the most common site of infection associ-
ated with this syndrome, especially in the neonatal per-
iod.
60
Liver histology shows intrahepatic cholestasis with
Kupffer cell hyperplasia and little or no evidence of cellu-
lar necrosis. Aside from cholestasis, liver histology reveals
an almost normal hepatic parenchyma.
20
The manifesta-
tions of the underlying infection usually dominate the
presentation.
55
Jaundice and cholestasis are usually revers-
ible and subside completely after resolution of the infec-
tion.
Pneumonia. The male-to-female ratio of patients
who develop jaundice with pneumococcal pneumonia is
Table 6. Liver Test Abnormalities in Sepsis
Conjugated hyperbilirubinemia: total bilirubin ranging from 2 to 10 mg/dL
Elevated alkaline phosphatase: rarely more than 2-3 times upper limit of
normal
Mild elevation of aminotransferases
236 CHAND AND SANYAL HEPATOLOGY, January 2007
10 to 1.
18
Most investigators think that pneumonia-asso-
ciated jaundice is a result of hepatocellular damage.
20
Many patients with pneumonia, with or without jaun-
dice, have abnormalities suggestive of hepatocellular dam-
age.
20
Hepatic necrosis has more commonly been
identied in liver biopsies of patients with pneumo-
nia.
17,60
Liver histology consistently shows patchy necro-
sis and dilated biliary canaliculi with bilirubinostasis.
20
The prognosis is good after complete resolution of the
infection.
Clostridium perfringens. Clostridium perfringens is a
commonly isolated clostridial species that can cause a
wide spectrum of clinical manifestations, from transient
bacteremia to massive red blood cell hemolysis, shock,
and death. Clostridial hemolysis has been described as a
rare complication of septic abortion, gall bladder disease,
and surgical procedures.
61
Severe bacteremia may result in
massive hemolysis, hemoglobinuria, shock, and death.
Clostridium perfringens produces a large variety of toxins
and virulence factors. The alpha toxin, a lecithinase, is
capable of hydrolyzing sphingomyelin and lecithin to
phosphoryl choline and diglyceride.
62
Lysolecithins re-
leased from cell membranes also act as hemolysins. Lyso-
lecithins also produce RBC membrane failure, which
accounts for the profound or fatal hemolytic anemia in
clostridial sepsis.
61
Striking hemoglobinemia and hemo-
globinuria are seen in this condition, and the high plasma
hemoglobin level may produce marked dissociation be-
tween blood hemoglobin and hematocrit levels. Acute
renal failure and hepatic failure usually develop. The
prognosis in this clinical setting is very poor, with more
than half the patients dying even with proper and exten-
sive treatment.
63-64
Therapy consists of high-dose penicil-
lin and surgical debridement.
63
Leptospirosis. Leptospirosis is a zooanthroponosis
transmitted among animals and occasionally from ani-
mals to humans. In the incubation period, the leptospira
organisms disseminate to different organs, especially the
liver, kidneys, muscles, and lungs. Experimental data sug-
gest that after the leptospira gain access to the blood-
stream, they concentrate in the liver, where they
reproduce.
65-66
There are two classical forms of presenta-
tion of leptospirosis, the icteric and anicteric forms. The
icteric form is the less common. A severe presentation of
the disease, occurring in only 5%to 10%of all leptospiral
infections, is known as Weils disease. This is associated
with high fever, severe hepatic function impairment, in-
tense jaundice, renal insufciency, hemorrhagic diathesis,
and cardiovascular compromise. Although serum biliru-
bin may be extremely high, serum aminotransferase and
alkaline phosphatase are only slightly to moderately ele-
vated. The mortality rate for this presentation is high.
Typhoid Fever. Typhoid fever, also known as enteric
fever, is an acute systemic illness caused by Salmonella
typhi. Typhoid fever is an infection that not only causes
jaundice but also induces liver injury.
20,67
Hepatomegaly
occurs in about 30% of patients, and jaundice occurs in
about a third of patients with hepatomegaly. Alkaline
phosphatase is usually 2-3 times the normal level, and
serum aminotransferases rarely are more than 5 times the
upper limits of normal. Rarely, ALT values may be mark-
edly elevated.
20
The diagnosis is made by (1) isolating
salmonellae from the blood or stool and (2) observing a
rise in the titer of the Widal reaction during the course of
the illness. The etiology of the hepatic damage in typhoid
fever is believed to be secondary to the effect of endotox-
in.
68
Previous studies have demonstrated that injection of
Salmonella typhi endotoxin produces focal hepatic necro-
sis. Other studies have suggested that liver injury may
occur by local release of cytotoxins or local inammatory
reactions within reticuloendothelial cells.
68
Cholangitis
and biliary stasis are apparently not important in the
pathogenesis of hepatic lesions.
67
The histology of the
livers of patients with typhoid fever shows focal cell ne-
crosis with mononuclear cell inltration and marked
Kupffer cell hyperplasia with mild cholestasis.
20
Typhoid
nodules, aggregations of Kupffer cells, are characteristic of
typhoid fever and are randomly distributed throughout
the hepatic lobule.
68
Follow-up liver biopsies have shown
complete resolution within 2 weeks after control of infec-
tion.
20
Natural History
The presence of jaundice and sepsis or the degree of its
severity does not seem to inuence survival or predict the
overall prognosis of the patient.
20,69
The overall prognosis
depends on the underlying infection. There usually is
complete resolution of hepatic dysfunction and cholesta-
sis if the underlying condition is adequately treated, yet
the outcome may be guarded if detection and treatment
are delayed.
4,6,14,69
Certain causes of jaundice in a criti-
cally ill patient such as acalculous cholecystitis and as-
cending cholangitis have a very poor prognosis.
Histology
The most prominent nding in sepsis is intrahepatic
cholestasis. Histologically, bile is found in the bile cana-
liculi and in hepatocyte cytoplasm(Fig. 3A-C). Bile back-
owinto the perisinusoidal spaces may lead to bile uptake
by Kupffer cells. There may also be some cholestasis-re-
lated parenchymal changes including feathery degenera-
tion of the hepatocyte cytoplasm. Apoptosis when present
appears as rounded bile-tinged apoptotic bodies in the
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 237
hepatic lobule. An increased amount of smooth endoplas-
mic reticulum as a result of cholestasis may lead to hepa-
tocytes having a ground-glass appearance.
Evaluation of Jaundice in an Infected Patient. The
guiding principles in the evaluation of a given patient are
consideration of (1) the differential diagnosis, (2) specic
diagnoses likely to have negatively affect the patient if
missed, and (3) therapeutic options available when a di-
agnosis can be made. Table 7 outlines the recommended
steps for evaluating a patient at risk for sepsis of jaundice.
The outcome of sepsis-associated jaundice is linked to
effective treatment of the sepsis. When jaundice develops
in a patient with an established diagnosis of infection, the
possibility of sepsis-related jaundice is obvious. On the
other hand, a high index of suspicion is often necessary to
diagnose this condition when jaundice is the presenting
manifestation of infection. The presence of hyperbiliru-
binemia and abnormal hepatic parameters may draw at-
tention from assessing a more serious underlying disease
process and lead to an unnecessary search for hepatic or
biliary disease. However, if a septic source is not known,
the possibility of hepatic or biliary infection as the cause of
jaundice should also be considered. There are many spe-
cic entities that require special attention.
Given the common causes of jaundice and the different
circumstances in which it is encountered, a thorough,
systematic approach should be carried out to evaluate the
cause (Table 7). Table 8 lists various etiologies in the
differential diagnosis in this setting. The type of jaundice,
that is, unconjugated versus conjugated and isolated hy-
perbilirubinemia versus jaundice with liver enzyme ab-
normalities, provides valuable clues that should guide
further workups. Unconjugated hyperbilirubinemia
should initiate a search for hemolysis and potential causes
of hemolysis. On the other hand, with a predominantly
cholestatic jaundice, it is imperative to exclude a poten-
tially treatable hepatobiliary cause of sepsis and jaundice.
Imaging studies to evaluate the hepatobiliary tract are
extremely valuable for this purpose. Sonography is rela-
tively inexpensive and can be performed at the bedsides of
critically sick patients. Also, Doppler sonography can ex-
clude vascular occlusion as a cause of jaundice. However,
sonography is not sensitive enough to pick up small ab-
scesses, and a CT scan should be performed when a he-
patic abscess is suspected.
Table 7. Evaluation of Patient at Risk for
Sepsis with Jaundice
1. Assess the type of jaundice
Conjugated versus Unconjugated
Unconjugatedinitiate a search for hemolysis
Conjugated
Search for a hepatobiliary cause
E Imaging studies
US (with or without Doppler)
CT
Isolated jaundice versus jaundice associated with liver enzyme elevation
2. Full workup to evaluate for infection
Complete blood count with differential
Urine analysis
Pan culture
Blood
Urine
Sputum
Catheter tips
Drains
Other potential sources of infection
Imaging
CXR
Further imaging of potential sites of infection (rule out abscess,
hepatobiliary disease, etc.)
Empiric antibiotic coverage: in selected cases, hepatic parameters may
improve within a couple of weeks if they were secondary to infection alone
Fig. 3. Liver biopsies of subjects with cholestasis showing (A) bile
plugs (black arrows), (B) pericholangitis, and (C) intrahepatic inspissated
bile in a subject with TPN-induced cholestasis.
238 CHAND AND SANYAL HEPATOLOGY, January 2007
In patients at risk for sepsis who develop jaundice
without other features of infection, blood cultures,
urine cultures, and a chest X-ray should be obtained as
a minimum workup to exclude sepsis. Also, cultures
should be sent from intravascular catheter tips, drains,
or any other source of potential infection. If an obvious
cause is still not apparent, further aggressive evaluation
for underlying infection or iatrogenic causes should be
sought. There are no controlled data that either vali-
date or refute giving empiric antibiotic coverage to all
patients with jaundice who have not yet shown other
features of infection. Frequently, empiric antibiotic
coverage with a broad-spectrum antibiotic is given to
those who are likely to be unable to tolerate sepsis.
Hepatic parameters, which usually improve within 1-2
weeks of therapy for the underlying infection, should
be followed closely.
Hepatocellular jaundice is diagnosed when hyperbil-
irubinemia is accompanied by high AST and ALT levels
and only modest or no elevation of alkaline phosphatase.
This is usually a result of ischemia, toxins, viral infection,
or iatrogenic injury. Hepatitis viral serology tests should
be done. A Tylenol level may be obtained if this drug has
been used to treat fever associated with infection. Typi-
cally, ALT levels are markedly elevated in such patients.
The passage of biliary sludge may sometimes be associated
with a rapid rise in AST that declines just as rapidly after
passage of the sludge. A hepatobiliary sonogram can be
used to conrmthe presence of sludge. Aliver biopsy does
not usually aid in management of this situation.
Management
The most important part of management is early diag-
nosis and treatment of infection (Table 9). Other addi-
tional steps in management follow.
Correction of Fluid and Electrolyte Imbalances.
Initial management should always include aggressive in-
travascular volume repletion and vasopressive agents if
needed to maintain adequate mean arterial blood pressure
for organ perfusion.
Treatment of Infection. The only effective treatment
of cholestasis of sepsis is the appropriate management of
the underlying infection. Appropriate antibiotic therapy
should be initiated as soon as possible. Septic foci should
be removed or drained. A delay in the diagnosis of infec-
tion and the initiation of antibiotic therapy signicantly
worsens the prognosis.
Enteral Feeding, Enteral feeding may help to resolve
cholestasis. Healthy individuals show a decreased serum
bilirubin with continuous enteral feeding. In infants, cho-
lestasis resolves when enteral feeding is introduced.
70
Ursodeoxycholic Acid. Ursodeoxycholic acid can po-
tentially improve bile ow and bilirubin levels in TPN-
AC- and drug-induced cholestasis. Currently, the clinical
evidence is insufcient to support the use of ursodeoxy-
cholic acid to treat cholestasis from these causes.
71,72
Glycine Administration. Glycine serum concentra-
tions are decreased in sepsis. At a cellular level, glycine
decreases the inux of calcium into Kupffer cells, thereby
reducing the release of TNF. This reduction in TNF may
play a benecial role in treatment of sepsis-associated cho-
lestasis and hepatocellular dysfunction. Yang et al. dem-
onstrated a benecial effect of glycine on hepatocyte
function and integrity in sepsis.
73
After administration of
this nonessential amino acid early after onset of polymi-
crobial sepsis in an animal model, hepatocellular function
markedly improved and the mortality rate decreased from
50% to 0% 10 days after the onset of sepsis.
73
Nitric Oxide Donor Administration. Nitric oxide
(NO) is a paracrine-acting gas enzymatically synthesized
from l-arginine. Cholestasis and endotoxemia have been
Table 9. Management
Treatment of Infection
Antibiotics
Drainage of abscess
Removal of potentially infected drains, IV lines, catheters
Correction of uid and electrolyte imbalances
Early Introduction of enteral feeding
Potential future treatments
Glycine administration
Ursodeoxycholic acid
Nitric oxide donor administration
N-acetyl-L-cyteine (NAC)
Table 8. Differential Diagnosis
Biliary tract disease
Cholecystitis (cholelithiasis/biliary sludge/acalculous)
Cholangitis
Biliary tract obstruction (gallstone, stent obstruction, tumor of the ampulla/
bile duct/pancreas, postbiliary intervention)
Liver disease
Hepatitis
Liver abscess
Hepatic ischemiasecondary to hemodynamic instability
Systemic Infection
Pneumonia
UTI
Bacteremia/septicemia
Other sites of primary infection
Hemolysis
Specic infections
Drugs
Multiple blood transfusions
Hepatotoxic drugs/toxins
Antibiotics
TPN
Tylenol
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 239
shown to cause hepatocyte apoptosis through caspase-
mediated pathways. In vitro studies showthat NOdonors
attenuate hepatic apoptosis via interruption of mitochon-
drial apoptotic signaling through S-nitrosylation of
caspases.
74,75
Brown et al. showed that NO has a hepato-
protective effect against this liver injury.
76
They showed
that providing NO by administrating molsidomine (a
NO donor) resulted in improved survival in septic rat
models and decreased liver injury and hepatocyte apopto-
sis.
76
N-Acetyl-l-Cysteine. N-acetyl-l-cysteine (NAC) has
been used as a free-radical scavenger, working either as a
direct scavenger or by increasing intracellular stores of
glutathione. Prior administration of NAC allowed an im-
proved cardiac index and lower maximal TNF levels in
endotoxemic dogs compared to controls in a study by
Zhang et al.
77
References
1. Garvin IP. Remarks on pneumonia biliosa. S Med Surg 1837;1:536:544.
2. Whitehead MW, Hainsworth I, Kingham JG. The causes of obvious jaun-
dice in South West Wales: perceptions versus reality. Gut 2001;48:409-
413.
3. Hamilton JR, Sass-Kortsak A. Jaundice associated with severe bacterial
infection in young infants. J Pediatr 1963;63:121-132.
4. Vermillion SE, Gregg JA, Baggenstoss AH, Bartholomew LG. Jaundice
associated with bacteremia. Arch Intern Med 1964;124:611-618.
5. Hawker F. Liver dysfunction in critical illness. Anaesth Intensive Care
1991;19:165-181.
6. Moseley RH. Sepsis and cholestasis. Clin Liver Dis 1999;3:465-475.
7. Neale G, Caughey D, Mollin DL, Booth CC. Effects of intrahepatic and
extrahepatic infection on liver function. Br Med J 1966;1:382-387.
8. Roche SP, Kobos R. Jaundice in the adult patient. Am Fam Physician
2004;69:299-304.
9. Roelofsen H, Van Der Veere C, Ottenhoff R, Schoemaker B, Jansen PL,
Oude Elferink RP. Decreased bilirubin transport in the perfused liver of
endotoxemic rats. Gastroenterology 1994;107:1075-1084.
10. Zucker SD, Storch J, Zeidel L, Gollan JL. Mechanism of the spontaneous
transfer of unconjugated bilirubin between small unilamellar phosphati-
dylcholine vesicles. Biochemistry 1992;31:3184-3192.
11. Moseley R. Sepsis and cholestasis. Clin Liver Dis 2004;8:94.
12. Bolder U, Ton-Nu H-T, Schteingart C, Frick E, Hofmann AF. Hepato-
cyte transport of bile acids and organic anions in endotoxemic rats: Im-
paired uptake and secretion. Gastroenterology 1997;112:214-215.
13. Jansen PL, Mulder GJ, Burchell B, Bock KW. New developments in
glucuronidation research: report of a workshop on glucuronidation, its
role in health and disease. Hepatology 1992;15:532-544.
14. Moseley RH. Sepsis-associated jaundicecomments. Hepatology 1996;
24:969-970.
15. Gerloff T, Steiger B, Hagenbuch B, Madon J, Landmann L, Roth J, et al.
The sister of P-glycoprotein represents the canalicular bile salt export
pump of mammalian liver. J Biol Chem 1998;273:10046-10050.
16. Ng S, Rawston J. Urinary tract infections presenting with jaundice. Arch
Dis Child 1971;46173-176.
17. Tugswell P, Williams O. Jaundice associated with lobar pneumonia. A
clinical, laboratory, and histological study. Q J Med 1977;66:97-118.
18. Zimmerman H, Thomas L. The liver in pneumococcal pneumonia: ob-
servations in 94 cases on liver function and jaundice in pneumonia. J Lab
Clin Med 1950;35:556-567.
19. Franson T, Hierholzer W, LaBrecque D. Frequency and characteristics of
hyperbilirubinemia associated with bacteria. Rev Infect Dis 1985;7:1-9.
20. Zimmerman H. Jaundice due to bacterial infection. Gastroenterology
1979;77:362-374.
21. Scharte M, Fink MP. Red blood cell physiology in critical illness. Crit Care
Med 2003; 31(12 Suppl):S651-S657.
22. Berkowitz FE. Hemolysis and infection: categories and mechanisms of
their interrelationship. Rev Infect Dis 1991;13:1151-1162.
23. Batge B, Filejski W, Kurowski V, Kluter H, Djonlagic H. Clostridial sepsis
with massive intravascular hemolysis: rapid diagnosis and successful treat-
ment. Intensive Care Med 1992;18:488-490.
24. Smith LD. Virulence factors of Clostridium perfringens. Rev Infect Dis
1979;1:254-262.
25. Rosenthal D. Hematologic Manifestations of Infectious Disease. Hema-
tology Basic Principles and Practice. Churchill Livingstone, Inc, 1995:
2162.
26. Beutler E. G6PD deciency. Blood 1994;84:3613-3636.
27. Dhaliwal G, Cornett PA, Tierney LM, Jr. Hemolytic anemia. Am Fam
Physician 2004;69:2599-2606.
28. Shander A. Anemia in the critically ill. Crit Care Clin 2004;20:159-178.
29. Sokol R, Hewitt S. Autoimmune hemolysis: a critical review. Crit Rev
Oncol Hematol 1985;4:125-154.
30. Lindsay K. Nonviral infections of the liver. In: Gitnick G, ed. Principles
and Practice of Gastroenterology and Hepatology. Norwalk, CT: Apple-
ton and Lange, 1994.
31. Dwain L. Thiele. Hepatic dysfunction during systemic infection. In:
Sleisenger and Fordtrans Gastrointestinal and Liver Disease. Philadelphia,
PA: W.B. Saunders Company, 1998.
32. Garratty G. Review: drug-induced immune hemolytic anemiathe last
decade. Immunohematol 2004;20:138-146.
33. Grossjohann B, Eichler P, Greinacher A, Santoso S, Kroll H. Ceftriaxone
causes drug-induced immune thrombocytopenia and hemolytic anemia:
characterization of targets on platelets and red blood cells. Transfusion
2004;44:1033-1040.
34. Arndt PA, Garratty G. The changing spectrum of drug-induced immune
hemolytic anemia. Semin Hematol 2005;42:137-144.
35. Trauner M, et al. Molecular pathogenesis of cholestasis. N Engl J Med
1998;339:1217-1227.
36. Hutchins G, Gollan J. Recent developments in the pathophysiology of
cholestasis. Clin Liver Dis 2004;8:1-26.
37. Beeson P, Brannon E, Warren J. Observations on the sites of removal of
bacteria from the blood in patients with bacterial endocarditis. J Exp Med
1945;81:9-23.
38. Hinshaw L, Reins D, Hill R. Response of isolated liver to endotoxin. Can
J Physiol Pharmacol 1966;44:529-541.
39. Szabo G. Liver in sepsis and systemic inammatory response syndrome.
Clin Liver Dis 2002;6:1045.
40. Roelofsen H, Schoemaker B, Bakker C, Ottenhoff R, Jansen PL, Elferink
RP. Impaired hepatocanalicular organic anion transport in endotoxemic
rats. Am J Physiol 1995;269:G427-G434.
41. Nolan J. Intestinal endotoxins as mediators of hepatic injuryan idea
whose time has come again. Hepatology 1989;10:887-891.
42. Ballas M, Giron J. Reversible hepatitis with Hemophilus inuenzae sepsis.
N Y State J Med 1982;1063-1065.
43. Boekhorst T, Urlus M, Doesburg W, Yap S, Goris R. Etiologic factors of
jaundice in severely ill patients. J Hepatol 1988;7:111-117.
44. Sherlock S. The liver in circulatory failure, diseases of the liver. In: Schiff L,
Schiff ER, eds. Diseases of the Liver. Philadelphia, PA: J.B. Lippincott
Company, 1993.
45. Ledgerwood A. Hepatobiliary complications of sepsis. Heart Lung 1976;
5:621-623.
46. Nadler E, Dickinson E, Beer-Stolz D, Alber SM, Watkins SC, Pratt DW,
et al. Scavenging nitric oxide reduces hepatocellular injury after endotoxin
challenge. AmJ Physiol Gastrointest Liver Physiol 2001;281:G173-G181.
47. Wang P, Ba ZF, Chaudry IH. Hepatocellular dysfunction occurs earlier
than the onset of hyperdynamic circulation during sepsis. Shock 1995;3:
21-26.
48. Wang P, Chaudry IH. Mechanism of hepatocellular dysfunction during
hyperdynamic sepsis. Am J Physiol 1996;270(5 Pt 2):R927-R938.
240 CHAND AND SANYAL HEPATOLOGY, January 2007
49. Whiting J, Green R, Rosenbluth A, Gollan J. Tumor necrosis factor-alpha
decreases hepatocyte bile salt uptake and mediates endotoxin-induced cho-
lestasis. HEPATOLOGY 1995;22:1273-1278.
50. Green R, Beier D, Gollan J. Regulation of hepatocyte bile salt transporters
by endotoxin and inammatory cytokines in rodents. Gastroenterology
1996;111:193-198.
51. Bolder U, Ton-Nu HT, Schteingart CD, Frick E, Hofmann AF. Hepato-
cyte transport of bile acids and organic anions in endotoxemic rats: im-
paired uptake and secretion. Gastroenterology 1997;112:214-225.
52. Moseley RH, Wang W, Takeda H, Lown K, Shick L, Ananthanarayanan
M, et al. Effect of endotoxin on bile acid transport in rat liver: a potential
model for sepsis-associated cholestasis. Am J Physiol 1996;271:G137-
G146.
53. Utili R, Abernathy C, Zimmerman H. Inhibition of Na, K-adeno-
sinetriphosphatase by endotoxin: a possible mechanism for endotoxin-
induced cholestasis. J Infec Dis 1997;136:583-587.
54. Salgia R, Becker J, Sayeed M. Altered membrane uidity in rat hepatocytes
during endotoxic shock. Mol Cell Biochem 1993;121:143-148.
55. Brandorg L, Goldman I. Bacterial and miscellaneous infections of the liver.
In: Hepatology, A Textbook of the Liver. Philadelphia, PA: W.B. Saun-
ders, 1990:1086-1098.
56. Alvarez Perez JA, Gonzalez JJ, Baldonedo RF, Sanz L, Carreno G, Junco A,
et al. Clinical course, treatment, and multivariate analysis of risk factors for
pyogenic liver abscess. Am J Surg 2001;181:177-186.
57. Wong TY, Chiu SI, So MK, Tsang MK, Lai ST, Tse KK, et al. Septic
metastatic endophthalmitis complicating Klebsiella pneumoniae liver ab-
scess in a non-diabetic Chinese man. Hong Kong Med J 2001;7:303-306.
58. Srivastava ED, Mayberry JF. Pyogenic liver abscess: a review of aetiology,
diagnosis and intervention. Dig Dis 1990;8:287-293.
59. Alvarez Perez JA, Baldonedo Cernuda RF, Gonzalez Gonzalez JJ, Sanz AL,
Carreno VG, Garcia BI, et al. [Pyogenic liver abscesses of cryptogenic
origin]. An Med Interna 2001;18:473-478.
60. Bernstein J, Brown AK. Sepsis and jaundice in early infancy. Pediatrics
1962;29:873-882.
61. Terebelo H, McCue R, Lenneville M. Implication of plasma free hemo-
globin in massive clostridial hemolysis. JAMA 1982;248:2028-2029.
62. Becker RC, Giuliani M, Savage RA, Weick JK. Massive hemolysis in
Clostridium perfringens infections. J Surg Oncol 1987;35:13-18.
63. Barrett JP, Whiteside JL, Boardman LA. Fatal clostridial sepsis after spon-
taneous abortion. Obstet Gynecol 2002;99(5 Pt 2):899-901.
64. Chen YM, Lee HC, Chang CM, Chuang YC, Ko WC. Clostridium bac-
teremia: emphasis on the poor prognosis in cirrhotic patients. J Microbiol
Immunol Infect 2001;34:113-118.
65. Carvalho CR, BethlemEP. Pulmonary complications of leptospirosis. Clin
Chest Med 2002;23:469-478.
66. De Brito T, BohmGM, Yasuda PH. Vascular damage in acute experimen-
tal leptospirosis of the guinea-pig. J Pathol 1979;128:177-182.
67. Ramachandran S, Godfrey JJ, Perera MV. Typhoid hepatitis. JAMA1974;
230:236-240.
68. Pramoolsinsap C, Viranuvatti V. Salmonella hepatitis. J Gastroenterol
Hepatol 1998;13:745-750.
69. Pirovino M, Meister F, Rubli E, Karlaganis G. Preserved cytosolic and
synthetic liver function in jaundice of severe extrahepatic infection. Gas-
troenterology 1989;96:1589-1595.
70. Hawker F. Liver dysfunction in critical illness. Anaesth Intensive Care
1991;19:165-181.
71. Duerksen DR, Van Aerde JE, Gramlich L, Meddings JB, Chan G, Thom-
son AB, et al. Intravenous ursodeoxycholic acid reduces cholestasis in par-
enterally fed newborn piglets. Gastroenterology 1996;111:1111-1117.
72. Lazaridis KN, Gores GJ, Lindor KD. Ursodeoxycholic acid mechanisms
of action and clinical use in hepatobiliary disorders. J Hepatol 2001;35:
134-146.
73. Yang S, Koo DJ, Chaudry IH, Wang P. Glycine attenuates hepatocellular
depression during early sepsis and reduces sepsis-induced mortality. Crit
Care Med 2001;29:1201-1206.
74. Li J, Billiar TR, Talanian RV, Kim YM. Nitric oxide reversibly inhibits
seven members of the caspase family via S-nitrosylation. Biochem Biophys
Res Commun 1997;240:419-424.
75. Kim YM, Kim TH, Chung HT, Talanian RV, Yin XM, Billiar TR. Nitric
oxide prevents tumor necrosis factor alpha-induced rat hepatocyte apopto-
sis by the interruption of mitochondrial apoptotic signaling through S-
nitrosylation of caspase-8. HEPATOLOGY 2000;32:770-778.
76. Brown KM, Brems JJ, Moazzam FN, Hartman GG, Gamelli RL, Ding
JW. The nitric oxide donor molsidomine improves survival and reduces
hepatocyte apoptosis in cholestasis and endotoxemia. J Am Coll Surg
2003;197:261-269.
77. Zhang H, Spapen H, Nguyen DN, Benlabed M, Buurman WA, Vincent
JL. Protective effects of N-acetyl-L-cysteine in endotoxemia. Am J Physiol
1994;266:H1746-H1754.
HEPATOLOGY, Vol. 45, No. 1, 2007 CHAND AND SANYAL 241
You might also like
- Vitamin D Deficiency: Epidemiology, Pathophysiology and ManagementDocument61 pagesVitamin D Deficiency: Epidemiology, Pathophysiology and ManagementSalmanNo ratings yet
- Vit D - 2 RevisiDocument36 pagesVit D - 2 RevisijessicaNo ratings yet
- Japanese EncephalitisDocument14 pagesJapanese EncephalitisMuhammad Rafli AkbarNo ratings yet
- Terapi Pencegahan TB Anak: Uk Respirologi Anak Idai Cabang Sumatera SelatanDocument26 pagesTerapi Pencegahan TB Anak: Uk Respirologi Anak Idai Cabang Sumatera SelatanFahrizal FahrizalNo ratings yet
- AB in HematooncoDocument39 pagesAB in HematooncokemalahmadNo ratings yet
- Batuk Kronik BerulangDocument24 pagesBatuk Kronik BerulangHameldo Andika PattinasaranyNo ratings yet
- Ventilasi Mekanik Untuk Neonatus: Dr. R. Adhi Teguh Perma Iskandar Sp.A Divisi Perinatologi FKUI-RSCMDocument52 pagesVentilasi Mekanik Untuk Neonatus: Dr. R. Adhi Teguh Perma Iskandar Sp.A Divisi Perinatologi FKUI-RSCMireneaureliaNo ratings yet
- Kuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)Document17 pagesKuliah: Renjatan Hipovolemi Pada Anak (Hypovolemic Shock in Children)DillaNo ratings yet
- Myelodisplastic SyndromeDocument9 pagesMyelodisplastic SyndromeEni JiantiNo ratings yet
- Childhood ObesityDocument70 pagesChildhood ObesityMedical SuperintendentNo ratings yet
- Sindroma Metabolik Dislipidemia Dan ObesitasDocument45 pagesSindroma Metabolik Dislipidemia Dan ObesitasLaurentius Juan WicaksonoNo ratings yet
- Vitamin D FinalDocument26 pagesVitamin D FinalAoda NmsaNo ratings yet
- Respiratory Support For PneumoniaDocument25 pagesRespiratory Support For Pneumoniamarte robiul saniNo ratings yet
- Atelectasis. Mechanisms, Diagnosis and Management (Peroni, 2000)Document5 pagesAtelectasis. Mechanisms, Diagnosis and Management (Peroni, 2000)Renato Li SoldevillaNo ratings yet
- 10 - Rapidly Progressing GlomerulonephristisDocument26 pages10 - Rapidly Progressing Glomerulonephristisf3er3No ratings yet
- Case AnakDocument28 pagesCase AnakAmorrita Puspita RatuNo ratings yet
- Hurler Syndrome (Biochem Repot)Document5 pagesHurler Syndrome (Biochem Repot)Kristine Abegail CantillerNo ratings yet
- MeningitisDocument20 pagesMeningitisAmalia Tri UtamiNo ratings yet
- Kolestasis AnakDocument5 pagesKolestasis AnakYenny SabriniNo ratings yet
- Ventikular Septal Defect FixDocument18 pagesVentikular Septal Defect FixPutri Sari DewiNo ratings yet
- Larsen Syndrome: - Dr. Kapil R JagtapDocument23 pagesLarsen Syndrome: - Dr. Kapil R JagtapKapil JagtapNo ratings yet
- 1-Fluid Management in Critically Ill Patients - Update Int Med Feb2018Document46 pages1-Fluid Management in Critically Ill Patients - Update Int Med Feb2018ดนุ เกษรศิริNo ratings yet
- Obesity in ChildrenDocument15 pagesObesity in ChildrenJohn ConnorNo ratings yet
- Case Report DifteriDocument20 pagesCase Report DifteriKhodimatur RofiahNo ratings yet
- The Critical Role of Vitamin D in Infants, Children and AdolescentsDocument69 pagesThe Critical Role of Vitamin D in Infants, Children and AdolescentsRose Ann BunyeNo ratings yet
- Neurodermatitis (Lichen Simplex Chronic)Document26 pagesNeurodermatitis (Lichen Simplex Chronic)Yusran Ady FitrahNo ratings yet
- PPT DIARHEA IN CHILDRENDocument31 pagesPPT DIARHEA IN CHILDRENRifka AnisaNo ratings yet
- MalariaDocument23 pagesMalariaIBhe Damianry QritezzNo ratings yet
- Pedsql Module CardioDocument31 pagesPedsql Module CardioRatna100% (1)
- 03 - DR - Dominicus - PELATIHAN DIFTERI SMD 17 Jan 2018 - Diagnosis - SharedDocument54 pages03 - DR - Dominicus - PELATIHAN DIFTERI SMD 17 Jan 2018 - Diagnosis - SharedFebria Valentine AritonangNo ratings yet
- Pituitary Adenomas in Adolescence Diagnostic Approach and Therapeutic Strategy GarofaloDocument48 pagesPituitary Adenomas in Adolescence Diagnostic Approach and Therapeutic Strategy GarofaloClaudia IrimieNo ratings yet
- TB Update 2016Document67 pagesTB Update 2016Nila hermawatiNo ratings yet
- Effect of Ursodeoxycholic Acid On Indirect Hyperbilirubinemia in Neonates Treated With PhototherapyDocument4 pagesEffect of Ursodeoxycholic Acid On Indirect Hyperbilirubinemia in Neonates Treated With PhototherapyEka Satria AnanditaNo ratings yet
- Types of Developmental DisordersDocument60 pagesTypes of Developmental DisordersAnshika ChaudhryNo ratings yet
- TORCH InfectionsDocument37 pagesTORCH InfectionsEylin Halim Rahardjo100% (1)
- Dyspnea in Children - Wahyuni IndawatiDocument20 pagesDyspnea in Children - Wahyuni IndawatiTarmidi MidziNo ratings yet
- Dampak Jangka Panjang StuntingDocument37 pagesDampak Jangka Panjang StuntingFina GisnawatyNo ratings yet
- Neonatal Infection: Julniar M Tasli Herman Bermawi Afifa RamadantiDocument56 pagesNeonatal Infection: Julniar M Tasli Herman Bermawi Afifa RamadantiOtchi Pudtrie WijayaNo ratings yet
- Materi DR. Dr. Ery Olivianto, Sp.A (K)Document39 pagesMateri DR. Dr. Ery Olivianto, Sp.A (K)utamiprakosoNo ratings yet
- Syok Pada AnakDocument28 pagesSyok Pada AnakTaufik Abidin100% (1)
- Hal 74-89 Sirosis Hepar-IsiDocument16 pagesHal 74-89 Sirosis Hepar-IsiMaulia Wisda Era ChresiaNo ratings yet
- Bronkopneumonia Pada Pasien PediatrikDocument5 pagesBronkopneumonia Pada Pasien PediatrikCecilia Evangelista NiluhNo ratings yet
- DEN GU E: DengueDocument53 pagesDEN GU E: Denguerose ONo ratings yet
- Associations Between Screen Time and Lower Psychological WellDocument13 pagesAssociations Between Screen Time and Lower Psychological WellZaid MarwanNo ratings yet
- Dr. Dr. Hesti Lestari, Sp.A (K) Development Monitoring and Stimulation in Preterm InfantDocument28 pagesDr. Dr. Hesti Lestari, Sp.A (K) Development Monitoring and Stimulation in Preterm InfantDennyNo ratings yet
- Case Report Kejang DemamDocument48 pagesCase Report Kejang DemamRahmatNo ratings yet
- NRSG 206 Croup SyndromeDocument3 pagesNRSG 206 Croup SyndromeGirlwithnonameNo ratings yet
- Bartter SyndromeDocument3 pagesBartter SyndromeEnny Andriani100% (1)
- An Eassy On Dengue Fever 1st ChoiceDocument8 pagesAn Eassy On Dengue Fever 1st ChoiceMd Abdullah al Qafi100% (1)
- Ilmu Kesehatan Anak: Judul Materi: Pendekatan Anemia Pada AnakDocument103 pagesIlmu Kesehatan Anak: Judul Materi: Pendekatan Anemia Pada AnakDhanin WitedjaNo ratings yet
- Vit D BDSSDocument58 pagesVit D BDSSIsaiah JohnsonNo ratings yet
- CEBM Levels of EvidenceDocument2 pagesCEBM Levels of EvidenceBellatriix Bonisa MadarjaNo ratings yet
- Children With Henoch Schonlein Purpura 2.0Document13 pagesChildren With Henoch Schonlein Purpura 2.0soniaNo ratings yet
- NBS Law FinalDocument33 pagesNBS Law Finalkissiah Cajetas100% (1)
- Drug EruptionDocument46 pagesDrug EruptionSyahDikaNo ratings yet
- 98692.infecao Sepsisinduced HepatitsDocument12 pages98692.infecao Sepsisinduced HepatitsAndi ZulkarnaeNo ratings yet
- Kolestasis SepsisDocument21 pagesKolestasis SepsisLilik NatasubrataNo ratings yet
- AF SeedingDocument6 pagesAF SeedingdonkeyendutNo ratings yet
- Assessment of Jaundice in The Hospitalized Patient PDFDocument16 pagesAssessment of Jaundice in The Hospitalized Patient PDFlaura canoNo ratings yet
- Nihms-789481 The Molecular Pathogenesis of Cholestasis in SepsisDocument15 pagesNihms-789481 The Molecular Pathogenesis of Cholestasis in SepsisAlexis CarrelNo ratings yet
- Disorders of PancreasDocument17 pagesDisorders of PancreasjonasNo ratings yet
- Gold Standards in Medical FieldDocument8 pagesGold Standards in Medical FieldJyothisankar Radhakrishnan100% (2)
- Ni Hms 267898Document20 pagesNi Hms 267898Thesar WaldiNo ratings yet
- Obstructive Jaundice and Perioperative ManagementsDocument8 pagesObstructive Jaundice and Perioperative ManagementsTri UtomoNo ratings yet
- Abdominal Swelling and Ascites: Global ConsiderationsDocument5 pagesAbdominal Swelling and Ascites: Global ConsiderationsJacob BorongNo ratings yet
- Choledocal CystDocument11 pagesCholedocal CystBilly JonatanNo ratings yet
- Surgical Instruments: March 2015Document122 pagesSurgical Instruments: March 2015Frida RasyidNo ratings yet
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocument47 pagesTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNo ratings yet
- Surgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1Document14 pagesSurgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1miguel cuevasNo ratings yet
- CH 32 Gallbladder and Extrahepatic Biliary SystemDocument33 pagesCH 32 Gallbladder and Extrahepatic Biliary SystemElisha BernabeNo ratings yet
- Cholestatic Liver Disease & Jaundice: Dr. David Minter, D.ODocument79 pagesCholestatic Liver Disease & Jaundice: Dr. David Minter, D.ONabeel ShahzadNo ratings yet
- Bile Duct StrictureDocument12 pagesBile Duct StricturechristianyecyecanNo ratings yet
- General Surgery Long CasesDocument140 pagesGeneral Surgery Long CasesHossain Muhammad91% (11)
- Liver Alterations in Cats - A Literature ReviewDocument39 pagesLiver Alterations in Cats - A Literature ReviewJoanna ChrysanthouNo ratings yet
- Cholangitis and Cholecystitis (DR - Dr. Hery Djagat Purnomo, SpPD-KGEH)Document47 pagesCholangitis and Cholecystitis (DR - Dr. Hery Djagat Purnomo, SpPD-KGEH)Aditya SahidNo ratings yet
- CHolelitiasis, CholesistitisDocument44 pagesCHolelitiasis, CholesistitistrianaamaliaNo ratings yet
- Accuracy of ASGE Criteria For The Prediction of Choledocholithiasis 2016Document6 pagesAccuracy of ASGE Criteria For The Prediction of Choledocholithiasis 2016DannyNo ratings yet
- BMJ Acute PancreatitisDocument8 pagesBMJ Acute PancreatitisMaria M MoldoveanuNo ratings yet
- Clinical Imaging of Liver, Gallbladder, BiliaryDocument93 pagesClinical Imaging of Liver, Gallbladder, Biliaryapi-3856051100% (1)
- 02.gall BladderDocument184 pages02.gall BladderRyam Taif100% (1)
- AFFERENT & EFFERENT SyndromeDocument12 pagesAFFERENT & EFFERENT SyndromeAli Sibra MulluziNo ratings yet
- Causes of Abdominal Pain in Adults - UpToDateDocument13 pagesCauses of Abdominal Pain in Adults - UpToDateAudricNo ratings yet
- Common Bile Duct Stones StrictureDocument48 pagesCommon Bile Duct Stones StrictureSyarif MalawatNo ratings yet
- Liver Funection TestDocument33 pagesLiver Funection TestDjdjjd SiisusNo ratings yet
- Gall Bladder Diseases by - DR Arun Aggarwal GastroenterologistDocument53 pagesGall Bladder Diseases by - DR Arun Aggarwal GastroenterologistDr. Arun Aggarwal GastroenterologistNo ratings yet
- 2010 - Hepatic Resection For Post-Cholecystectomy Bile Duct Injuries - A Literature ReviewDocument8 pages2010 - Hepatic Resection For Post-Cholecystectomy Bile Duct Injuries - A Literature ReviewBattousaih1No ratings yet
- Canine Infectious Diseases PDFDocument149 pagesCanine Infectious Diseases PDFSándor Holdas50% (2)
- Liver Transplant - PedsDocument15 pagesLiver Transplant - Pedsbencleese100% (2)
- Clinical Manifestations and Diagnosis of Acute PancreatitisDocument31 pagesClinical Manifestations and Diagnosis of Acute PancreatitisBrian WilliamNo ratings yet