Professional Documents
Culture Documents
NCP For Frostbite
Uploaded by
Rommar Romero0 ratings0% found this document useful (0 votes)
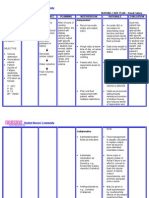
1K views2 pagesThis document discusses the assessment, diagnosis, planning, intervention, rationale, and evaluation for a patient experiencing frostbite. The patient reported not feeling their fingertips. On examination, parts of the patient's skin were turning white, hard, or black. The proposed nursing interventions include rapidly warming the affected area in warm water for 15-30 minutes, teaching the patient about care and prevention of further injury, administering medications to reduce inflammation and prevent infection, and closely monitoring the patient's understanding and skin recovery. The overall goal is to promote healing of the skin and prevent complications from infection or further injury.
Original Description:
Ncp for Frostbite
Original Title
Ncp for Frostbite
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses the assessment, diagnosis, planning, intervention, rationale, and evaluation for a patient experiencing frostbite. The patient reported not feeling their fingertips. On examination, parts of the patient's skin were turning white, hard, or black. The proposed nursing interventions include rapidly warming the affected area in warm water for 15-30 minutes, teaching the patient about care and prevention of further injury, administering medications to reduce inflammation and prevent infection, and closely monitoring the patient's understanding and skin recovery. The overall goal is to promote healing of the skin and prevent complications from infection or further injury.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
1K views2 pagesNCP For Frostbite
Uploaded by
Rommar RomeroThis document discusses the assessment, diagnosis, planning, intervention, rationale, and evaluation for a patient experiencing frostbite. The patient reported not feeling their fingertips. On examination, parts of the patient's skin were turning white, hard, or black. The proposed nursing interventions include rapidly warming the affected area in warm water for 15-30 minutes, teaching the patient about care and prevention of further injury, administering medications to reduce inflammation and prevent infection, and closely monitoring the patient's understanding and skin recovery. The overall goal is to promote healing of the skin and prevent complications from infection or further injury.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
Frostbite
Assessment Diagnosis Planning Intervention Rationale Evaluation
S
Hindi ko
maramdaman
yung dulo ng
mga daliri ko
as verbalized
O:
A part of the
patients
body or skin
is turning
white and
hard or black.
Red, white,
pale or
grayish-
yellow skin
Hard or
waxy-
looking skin
Low body
temperature
Impaired
Skin
Integrity
related to
frost bite as
evidenced
by open
skin lesions
After 3 hours of
nursing
intervention, the
patient will be
able to verbalize
understanding of
cause and
therapeutic
management
regimen and
demonstrate
behaviors to
improve
thermoregulation
Get the patient
to a warm
place and
remove any
wet clothing.
Rapidly warm
the affected
area in water
for 15 to 30
minutes.
Teach the
patient not to
walk on
frostbitten toes
or feet.
Do not rewarm
the skin until
you can keep it
warm.
Gently warm
the area in
warm water
(not hot) or
with wet heat
until the skin
appears red
and warm.
Teach the
patient not use
direct heat
from heating
pads, radiator,
or fires.
Remove
blisters that
contain clear
To promote
thermoregulation
To avoid further
complications
Warming and
then re-
exposing the
frostbitten area
to cold air can
cause worse
damage.
Exposing the
frostbitten area
to direct heat
can cause worse
damage.
To protect skin
or milky fluid
and cover
them with a
topical
antibiotic,
petroleum
jelly, or aloe
vera gel.
Blisters that
contain blood
may not be
removed.
Splint and
elevate the
affected area
and wrap it in
a loose
bandage.
Administer
ibuprofen to
limit
inflammation,
tetanus toxoid
to prevent
tetanus
infection, and
antibiotics
from infections
To prevent or
treat infection.
You might also like
- How to Clean Makeup Brushes Easily in 5 StepsDocument6 pagesHow to Clean Makeup Brushes Easily in 5 StepsNiharika DasNo ratings yet
- Public Playground Safety Handbook: U.S. Consumer Product Safety CommissionDocument60 pagesPublic Playground Safety Handbook: U.S. Consumer Product Safety CommissionpopovicaNo ratings yet
- Assessment of Skin Functions and StructuresDocument65 pagesAssessment of Skin Functions and StructuresVinzii Drt100% (1)
- Impaired Skin DMDocument3 pagesImpaired Skin DMimnotdatsunny100% (1)
- Discharge Plan For CVADocument1 pageDischarge Plan For CVAPhoebe Guevarra100% (2)
- FrostbiteDocument13 pagesFrostbiteRosalyn YuNo ratings yet
- NCP AneurysmDocument4 pagesNCP AneurysmJanielle Christine Monsalud100% (1)
- Headache Nursing CareDocument4 pagesHeadache Nursing CareAnneUXDNo ratings yet
- SITXWHS001 Assessment 1 - Short AnswersDocument13 pagesSITXWHS001 Assessment 1 - Short AnswersNasir BilalNo ratings yet
- Fluid Volume Management Nursing InterventionsDocument5 pagesFluid Volume Management Nursing InterventionsMerrill HansNo ratings yet
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- Learning Objective: at The End of The Exercise Students Shall Be Able ToDocument3 pagesLearning Objective: at The End of The Exercise Students Shall Be Able ToAni Gupta100% (1)
- NCP PancreatitisDocument2 pagesNCP PancreatitisJeanelle GenerosoNo ratings yet
- NCP for Acute Coronary Syndrome AssessmentDocument3 pagesNCP for Acute Coronary Syndrome Assessmentsarahtot67% (3)
- NCP - Fluid RetentionDocument3 pagesNCP - Fluid RetentionMichelle Teodoro100% (1)
- NCP 2 and Soapie 1Document5 pagesNCP 2 and Soapie 1narsD100% (1)
- Decreased Cardiac Output Nursing DiagnosisDocument2 pagesDecreased Cardiac Output Nursing DiagnosisJoehoney BarreraNo ratings yet
- Case: Liver Cirrhosis Assessment:: Nursing InferenceDocument7 pagesCase: Liver Cirrhosis Assessment:: Nursing InferenceLovelyn GanirNo ratings yet
- Rapini DermatopatologíaDocument474 pagesRapini DermatopatologíadrNo ratings yet
- Respiratory Failure NCPDocument1 pageRespiratory Failure NCPkyaw100% (1)
- NCP For AnaphylacticDocument3 pagesNCP For AnaphylacticRommar Romero67% (3)
- Nursing Care Plan for Patient with LymphedemaDocument1 pageNursing Care Plan for Patient with Lymphedemayasira50% (2)
- Science Investigatory ProjectDocument7 pagesScience Investigatory Project카밀카밀No ratings yet
- Semi-Detailed Lesson Plan (Footspa) : Prepared By: Rosemarie A. Ramirez-AmilDocument5 pagesSemi-Detailed Lesson Plan (Footspa) : Prepared By: Rosemarie A. Ramirez-AmilRosemarie RamirezNo ratings yet
- Nursing Care Plan 1 DiagDocument4 pagesNursing Care Plan 1 Diagguysornngam100% (1)
- Multi Noduar Colloid GoiterDocument1 pageMulti Noduar Colloid GoiterVincent John Faller100% (1)
- Improving Comfort with Endotracheal TubeDocument1 pageImproving Comfort with Endotracheal TubeSelwynVillamorPatenteNo ratings yet
- Anti-Diabetic Drug Vildagliptin: Mechanism, Indication, Side Effects and Nursing CareDocument2 pagesAnti-Diabetic Drug Vildagliptin: Mechanism, Indication, Side Effects and Nursing CareChris Denver BancaleNo ratings yet
- A Nursing Care Plan VaDocument3 pagesA Nursing Care Plan VaArianne Paola QuindoyNo ratings yet
- Care Plan ExampleDocument2 pagesCare Plan Exampleincess27100% (1)
- NCP Near DrowningDocument1 pageNCP Near Drowningchristine louise bernardoNo ratings yet
- NCP Risk Infection Papillary Thyroid CADocument2 pagesNCP Risk Infection Papillary Thyroid CAjazvNo ratings yet
- NCP For CTTDocument1 pageNCP For CTTJen Rhae LimNo ratings yet
- Student Nurses’ Community NURSING CARE PLAN – Renal FailureDocument2 pagesStudent Nurses’ Community NURSING CARE PLAN – Renal FailureAldrein GonzalesNo ratings yet
- Orahex Oral SolutionDocument1 pageOrahex Oral SolutionconanmarcNo ratings yet
- 6639burn NCPDocument18 pages6639burn NCPDivina Grace Renon Camba100% (1)
- Aminogen Drug StudyDocument2 pagesAminogen Drug Studymilesmin100% (1)
- Week 10 Drug Card - Hydrochlorothiazide (HCTZ)Document2 pagesWeek 10 Drug Card - Hydrochlorothiazide (HCTZ)RCurry09No ratings yet
- NCPDocument6 pagesNCPKyla Carbonel100% (1)
- Nursing Care Plan for Breast CancerDocument2 pagesNursing Care Plan for Breast CancerMaina BarmanNo ratings yet
- Orientation PhaseDocument3 pagesOrientation Phasekimchi girlNo ratings yet
- NCP Acute PainDocument3 pagesNCP Acute PainDyanne BNo ratings yet
- GlipizideDocument3 pagesGlipizideapi-3797941100% (1)
- Acute Pain Related To Tissue Trauma and InjuryDocument4 pagesAcute Pain Related To Tissue Trauma and Injuryprickybiik50% (2)
- NCP & Drugstudy FormatDocument7 pagesNCP & Drugstudy Formatanonymous89ify100% (1)
- IV Isotonic Fluid Therapy GuideDocument2 pagesIV Isotonic Fluid Therapy GuideFrances Oscar GaviolaNo ratings yet
- NCP Ineffective Breathing GunshotDocument3 pagesNCP Ineffective Breathing GunshotMikko Enoc100% (1)
- Silvadene (Silver Sulfadiazine)Document1 pageSilvadene (Silver Sulfadiazine)ENo ratings yet
- Nursing Care Plan For RabiesDocument1 pageNursing Care Plan For RabiesAngel VillamorNo ratings yet
- NCP PROPER Pain and Decreased Cardiac OutputDocument3 pagesNCP PROPER Pain and Decreased Cardiac OutputErienne Lae Manangan - CadalsoNo ratings yet
- D5LR VS PLRDocument27 pagesD5LR VS PLRgerrilynwayneNo ratings yet
- NCP - Acute Pain Stomach CancerDocument2 pagesNCP - Acute Pain Stomach CancerJohn Michael TaylanNo ratings yet
- Name of DrugDocument6 pagesName of Drug私 シャーロット100% (1)
- Nursing Care Plan Renal FailureDocument2 pagesNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimNo ratings yet
- Cancer Pain ManagementDocument8 pagesCancer Pain ManagementMaryjoy Gabriellee De La Cruz100% (1)
- 66 Drug AnaDocument3 pages66 Drug AnaAlexa RoqueNo ratings yet
- NCP - Fluid Volume DeficitDocument2 pagesNCP - Fluid Volume DeficitPatrice LimNo ratings yet
- ASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoDocument1 pageASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoCherie MayNo ratings yet
- Levothyroxine SodiumDocument3 pagesLevothyroxine Sodiumapi-3797941100% (1)
- Somera Case 1928Document68 pagesSomera Case 1928jrkalbo75% (4)
- TramadolDocument1 pageTramadolAi RouNo ratings yet
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PonceNo ratings yet
- NCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)Document2 pagesNCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)yanny0350% (2)
- Burns and Environmental EmergenciesDocument33 pagesBurns and Environmental EmergenciesmatrixtrinityNo ratings yet
- Heat and Cold ApplicationDocument21 pagesHeat and Cold Applicationbemina jaNo ratings yet
- Causes, Types and Treatment of BurnsDocument5 pagesCauses, Types and Treatment of BurnsPooja ChapdiNo ratings yet
- Philippine Central Islands College: Quarter 4Document9 pagesPhilippine Central Islands College: Quarter 4Quijano, Stephanie L.No ratings yet
- Burn Injury Causes, Types, First Aid & When to Seek Medical HelpDocument19 pagesBurn Injury Causes, Types, First Aid & When to Seek Medical HelpAhmad JoiyaNo ratings yet
- Respiratory Distress SyndromeDocument4 pagesRespiratory Distress SyndromeRommar RomeroNo ratings yet
- EndocrineDocument40 pagesEndocrineRommar RomeroNo ratings yet
- Scope and Limitation On Thesis Patients Satisfaction On Charity WardDocument1 pageScope and Limitation On Thesis Patients Satisfaction On Charity WardRommar RomeroNo ratings yet
- Introduction On Thesis Patients Satisfaction On Charity WardDocument2 pagesIntroduction On Thesis Patients Satisfaction On Charity WardRommar RomeroNo ratings yet
- Classification and Management of Wounds: Warrington DivisionDocument2 pagesClassification and Management of Wounds: Warrington DivisionRoger ChristensenNo ratings yet
- NuDerm Clear Blender Sunfader PIDocument3 pagesNuDerm Clear Blender Sunfader PILynn AGNo ratings yet
- Contact Dermatitis Concept MapDocument1 pageContact Dermatitis Concept MapAlexeve TabalNo ratings yet
- Lime (Citrus Aurantifolia) Peel As Natural Antibacteria For Wound Skin Infection Caused by Staphylococcus AureusDocument4 pagesLime (Citrus Aurantifolia) Peel As Natural Antibacteria For Wound Skin Infection Caused by Staphylococcus AureusExtraordinary MaryNo ratings yet
- Skin Lesion Exam: 4 Key FeaturesDocument2 pagesSkin Lesion Exam: 4 Key FeaturesElrey InocianNo ratings yet
- NHS Continuing Healthcare Checklist: October 2018 (Revised)Document24 pagesNHS Continuing Healthcare Checklist: October 2018 (Revised)Alejandro CardonaNo ratings yet
- Volumizacao Com PreenchedoresDocument18 pagesVolumizacao Com PreenchedoresMichele CarvalhoNo ratings yet
- Cosmetic and Cosmeceutical in Skin Problem PDFDocument13 pagesCosmetic and Cosmeceutical in Skin Problem PDFaman theNo ratings yet
- Bahasa Inggris ArtikelDocument2 pagesBahasa Inggris ArtikelekonurcahyaningrumNo ratings yet
- Case RatesDocument306 pagesCase RatesCyril DaguilNo ratings yet
- My Paper Elsevier Androgenic Alopecia1Document9 pagesMy Paper Elsevier Androgenic Alopecia1David GuerreroNo ratings yet
- Lecture 27 - Histology of The Integumentary System 2Document89 pagesLecture 27 - Histology of The Integumentary System 2spitzmark2030No ratings yet
- Oral Melanotic Macule - An Unusual Occurrence in GingivaDocument4 pagesOral Melanotic Macule - An Unusual Occurrence in GingivaYeni PuspitasariNo ratings yet
- Actinic Keratosis: (Aka Bowen's Disease)Document5 pagesActinic Keratosis: (Aka Bowen's Disease)fadoNo ratings yet
- LHR Full Details - 1.03.21Document38 pagesLHR Full Details - 1.03.21chauhanpriyanshu059No ratings yet
- Nonsurgical Treatments For Infraorbital RejuvenationDocument11 pagesNonsurgical Treatments For Infraorbital RejuvenationHuy Hoàng GiaNo ratings yet
- Annual Report FY 2019 20Document328 pagesAnnual Report FY 2019 20Monil BNo ratings yet
- Sexual HygieneDocument32 pagesSexual Hygienethea medinaNo ratings yet
- The DermaphocytesDocument11 pagesThe DermaphocytescatuiraneljhayyyNo ratings yet
- AkapulkoDocument4 pagesAkapulkoRoland Acob Del Rosario Jr.No ratings yet
- VV Inc's Positioning of Vicks Vaporub as a Rub for Child's Cold in IndiaDocument7 pagesVV Inc's Positioning of Vicks Vaporub as a Rub for Child's Cold in IndiaashukgiriNo ratings yet
- Data of Doctors in TexasDocument54 pagesData of Doctors in TexasAdnanNo ratings yet