Professional Documents
Culture Documents
The Technology Behind Glucose Meters
The Technology Behind Glucose Meters
Uploaded by
wahyuthp43Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Technology Behind Glucose Meters
The Technology Behind Glucose Meters
Uploaded by
wahyuthp43Copyright:
Available Formats
S-10
DIABETES TECHNOLOGY & THERAPEUTICS
Volume 10, Supplement 1, 2008
Mary Ann Liebert, Inc.
DOI: 10.1089/dia.2008.0005
The Technology Behind Glucose Meters: Test Strips
JOACHIM HNES, Dr. rer. nat.,
1
PETER MLLER, Dr. rer. nat.,
1
and NIGEL SURRIDGE, Ph.D.
2
ABSTRACT
Blood glucose meters are the basis for people with diabetes to live a near-normal life avoid-
ing acute and late complications. The main part of the technology behind blood glucose meters
is formed by test strips. This paper tries to give an overview and some insight into the princi-
ples of test strips. They contain enzymes, coenzymes, mediators, and indicators in the form of
a dry layer and convert blood glucose concentration into a signal that is readable by the meter.
Measurement speed, specificity, accuracy, and precision are dominated by test strip chemistry
and design. During the last decades, they have been developed to do the job in 5 s, with less
than 1 L of blood. It is our firm belief that they will be developed further and stay important
for decades to come.
INTRODUCTION
I
NABILITY TO CONTROL their blood sugar levels
is a major challenge for many patients with
diabetes. After decades of development and
use of self-measurement of blood glucose, com-
bined with intensified insulin therapy, the Di-
abetes Control and Complications Trial study
1
has proven that frequent control and proper
regulation of blood glucose are essential for
those with diabetes to live a near normal life
and to avoid late complications. Today, people
with diabetes can choose from a multitude of
blood glucose meters. Every time a measure-
ment is required, a finger (or other site) is
lanced with a small lancing device, and a tiny
blood drop is obtained and then placed onto a
small, single-use test strip. After a few seconds,
the meter displays the result, and the patient
can act accordingly.
Everyone is familiar with blood glucose me-
ters, but what is the technology behind them?
The meter is an electronic device converting
a signal to a digital value, which then is shown
on the display. Electronic memory, communi-
cation with a personal computer, and many
other features are packed into a nicely designed
housing. Handling is generally easy, and me-
ters have become more like nice examples of
consumer electronics. But in a nutshell, the ba-
sic function is that of an ampere meter in the
case of electrochemical measurement or a pho-
tometer for color-forming strips.
The key for accurate measurement of blood
glucose is conversion of the glucose concentra-
tion to a specific signal. This has to be done
from a small drop (typically around 1 L) of
the highly complex blood sample. Continuous
improvements of technology have enabled test
strips to do this difficult job in just 5 s. (For the
1
Roche Diagnostics GmbH, Mannheim, Germany.
2
Roche Diagnostics Operations Inc., Indianapolis, Indiana.
role of meters, see the section Measurement
Methods: Electrochemistry and Photometry.)
Lets have a closer look inside these little
pieces of plastic, and behind such well-de-
signed blood glucose meters.
HISTORY
Self-measurement of blood glucose started
around 1970 with test strips designed for visual
evaluation by the patient. HGT 20-800 or Chem-
strip bG
from Boehringer Mannheim
(Mannheim, Germany) and Ames (Elkhart, IN)
Dextrostix
were typical products in 1975. With
Chemstrip bG, the customer had to place a large
drop of blood (25 L) on top of the chemistry
coating. After a precisely measured time interval
of 1 min, the blood was manually wiped off, and
after a further minute, the color of the chemistry
pad had to be compared with a printed color
scale. Well-trained patients were able to read
blood glucose with sufficient accuracy to man-
age their diabetes successfully. Blood glucose
meters came into use around 1975.
The next revolution came in 1987, when
LifeScan (Milpitas, CA) introduced the One
Touch
system. The test strip was a flat piece
of plastic with a hole covered by a membrane.
The blood drop was placed on the top side of
the membrane. Since the membrane layer did
not separate erythrocytes, the resulting color
was a mixture of red from hemoglobin plus
blue dye from the glucose reaction. Therefore,
visual evaluation was not possible. After 45 s,
the meter measured from the bottom side of the
strip, with two wavelengths being used to com-
pensate for the color of blood.
2
In 19871988,
the first test strip employing an electrochemi-
cal measurement was introduced with the Ex-
acTech
Pen meter (Medisense, Waltham, MA;
now Abbott Diabetes Care, Alameda, CA).
Wiping was unnecessary, and visual evalua-
tion was not applicable, of course. All other
companies reacted and developed non-wipe
systems as well, and wipe strips and visual
evaluation are completely outdated now.
Since the late 1980s, test strip measurements
became faster and faster, and nowadays, 5 s is
state of the art. In parallel, the sample volume
required has decreased (Fig. 1), and the test sys-
tem with the lowest volume currently is
Therasenses [now Abbott Diabetes Cares]
FreeStyle with 0.3 L, introduced in 1999.
The motivation for this development to low
volume was to enable a successful test every
BLOOD GLUCOSE TEST STRIPS S-11
0,01
0,1
1
10
100
1965 1970 1975 1980 1985 1990 1995 2000 2005 2010 2015
Year of Product Launch
B
l
o
o
d
V
o
l
u
m
e
(
L
)
Roche electrochemical
Roche photometric
LifeScan
Abbott
Bayer
New Competitors
Four major players have
lined up between 0.3-1 l
FIG. 1. Overview of sample volume need versus time of product introduction. Test strips have been developed dur-
ing the last decades to work with samples as small as 0.3 L.
time. Furthermore, it enabled shallower lanc-
ing depth to avoid pain. Our feeling is that
this goal has been achieved by all major prod-
ucts at a volume around or below 1 L. Cus-
tomers cannot control lancing to precisely
produce smaller amounts. After lancing, they
either get nothing because lancing depth was
insufficient, or they are easily able to produce
a drop of 1 L or even greater. Such a drop
is necessary to allow easy targeting, espe-
cially when the capillary entrance of a test
strip has to be hit. The lower the volume
gained, the more difficult is the application.
A further reduction of net volume required
would not be advantageous for the customer.
If accompanied by a further miniaturization
of strips and capillaries, it would even make
handling more difficult.
A further development needs to be men-
tioned. In the beginning, visual or photometric
test strips were dosed from the top, and a large
blood drop was placed on the surface. Electro-
chemical strips, in contrast, are filled by con-
tacting the drop with the entrance of a capil-
lary, mostly from an edge of the strip. Even
some current photometric strips like Accu-
Chek
(Roche Diagnostics, Mannheim) Com-
pact use capillary fill. The market has moved
to a certain extent from photometry and top
dosing towards electrochemistry and capillary
fill. This is certainly due to the fact that in cer-
tain circumstances such as professional health-
care environments, it is important to keep
blood away from the main meter housing for
hygienic/safety reasons. Electrochemical test
strips, up to this point, have been better able to
deliver this feature because of the length of con-
ducting leads that can be placed between the
meter and the blood application site of the test
strips. No such severe limitation exists for the
application of photometry in systems to be
used by single individuals, and photometry
may also provide this benefit without the need
to fill a lengthy capillary in novel future itera-
tions of the technology.
In general, 30 years of continuous develop-
ment by many competing companies have led
self-monitoring of blood glucose to an ease of
use that makes it applicable for nearly every-
one.
THE TECHNOLOGY INSIDE STRIPS
Enzymes
All current strips use enzymes as specifiers
for glucose. The enzymes are oxidoreductases,
and oxidize glucose to gluconolactone. Elec-
trons from the glucose are generally then trans-
ferred to the oxidized form of a mediator mol-
ecule, thereby converting it to the reduced
form. (A mediator is usually a small organic or
inorganic chemical capable of existing in both
an oxidized and a reduced form, and generally
reacts quickly to donate or receive electrons.)
This mediator in turn delivers the electrons to
an electrode for electrochemical measurement
or to an indicator molecule, which in turn
forms color. All enzymes use coenzymes (or co-
factors), and additional enzymes may even be
necessary where the overall reaction involves
intermediate steps. Table 1 shows an overview.
The three types of glucose dehydrogenases
(GDHs) are completely different enzymes.
Pyrrolo quinoline quinone (PQQ)-dependent
GDH is also known as glucose dye oxidore-
ductase (GlucDOR). The combination of hexo-
kinase with glucose-6-phosphate dehydroge-
nase, which is the standard reference method
in many laboratories, is not used in current test
strips. The enzyme is responsible for the test
strips sugar specificity, but none of the en-
zymes is completely specific for glucose. Glu-
cose oxidase (GOD) has been described as be-
ing highly specific,
3
but, e.g., mannose is an
interferent although in the low percentage
range. Both 2- and 6-deoxyglucoses react even
at higher rates.
4
PQQ-dependent GDH con-
verts maltose and glucose with similar catalytic
efficiency.
5
Nicotinamide adenine dinucleotide
(NAD)-dependent GDH reacts with xylose,
6
and flavin adenine dinucleotide (FAD)-depen-
dent GDH reacts with maltose, mannose, galac-
tose, and lactose but (like GOD) in the single
digit percentage range only.
7
A high specificity
in enzyme activity tests is a good prerequisite
for using the enzyme in a test strip. However,
high concentrations of enzyme in the formula-
tions can make low side activities a real inter-
ference.
In general, these sugars are not present in the
blood of healthy people or people with dia-
HNES ET AL. S-12
betes. But in the case of some medications or
rare diseases, maltose, xylose, or galactose may
be found, leading to false-positive glucose
readings. It is essential for patients and physi-
cians to carefully read the package insert of test
strips and to avoid using products with the
wrong enzyme system for that special treat-
ment case. On the other hand, it is essential for
the companies to improve specificity even if
sugar nonspecificity is an issue for only a few
patients. Intensive work has been dedicated to
improvement in the specificity of PQQ-depen-
dent GDH. Mutations have been used to reduce
maltose reaction to below 2% of the wild-type
or nonmutated value,
8,9
and product imple-
mentation is in progress. Bayer Healthcare
(Tarrytown, NY) has already changed the en-
zyme of their Ascensia
Microfill
strip prod-
uct from PQQ-dependent GDH to FAD-de-
pendent GDH. GOD also seems to be
advantageous in terms of sugar specificity
since mannose is not used in medications to-
day and deoxy sugars are of academic interest
only, but the natural second substrate of this
enzyme is oxygen. The reduced form of this
substrate is the active oxidant hydrogen per-
oxide. Consequently, nonspecific oxidation of
metabolites and drugs by this hydrogen per-
oxide leads to interferences, e.g., from uric acid
and bilirubin. The alternative for GOD is to use
a non-natural mediator instead of oxygen, but
such a mediator needs to compete with oxygen
for the electrons from glucose. Variations in
oxygen content of the sample, e.g., among ve-
nous, capillary, and arterial blood, then lead to
apparent differences in measured glucose. Al-
titude dependency is a frequent interference
with GOD-based strips, too.
Mediators
The enzyme transfers electrons from glucose
to the oxidized mediator. The reduced media-
tor formed transfers the electrons to a working
electrode, producing a current, or to an indica-
tor, forming color. Ferrocene derivatives and
BLOOD GLUCOSE TEST STRIPS S-13
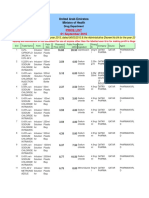
TABLE 1. ENZYME/MEDIATOR SYSTEMS
Additional
Enzyme Coenzyme enzyme Mediator system Indicator Product examples
GOD FAD POD Air oxygen/hydrogen Leuco dye Chemstrip bG,
peroxide One Touch
GOD FAD None Hexacyanoferrate Palladium Accu-Chek
III/hexacyanoferrate II electrode Advantage
GOD FAD None Hexacyanoferrate Carbon electrode One Touch Ultra
III/Hexacyanoferrate II
GDH (GlucDOR) PQQ None Hexacyanoferrate Palladium Accu-Chek
III/hexacyanoferrate II electrode Advantage
(Comfort Curve
strip)
GDH (GlucDOR) PQQ None Quinoneimine/ Phosphomolybdic Accu-Chek
phenylendiamine acid Active, Accu-
Chek Compact,
Accu-Chek Go
GDH (GlucDOR) PQQ None Quinoneimine/ Gold electrode Accu-Chek Aviva
phenylendiamine
GDH (GlucDOR) PQQ None Osmium Electrode FreeStyle
GDH NAD None Phenanthroline quinone Electrode Precision Xtra
GDH FAD None Hexacyanoferrate Palladium Ascensia
III/hexacyanoferrate II electrode Microfill
This is not a complete overview. Other combinations have been used and will be used in the future. Glucose oxi-
dase (GOD) was used first. Glucose dehydrogenase (GDH)/flavin adenine dinucleotide (FAD) is the enzyme most
recently introduced. GlucDOR, glucose dye oxidoreductase; NAD, nicotinamide adenine dinucleotide; POD, peroxi-
dase/ PQQ, pyrrolo quinoline quinone.
Accu-Chek is a trademark of Roche Diagnostics, Ascensia Microfill of Bayer Healthcare, Chemstrip bG of Boehringer
Mannheim, Freestyle and Precision Xtra of Abbott Diabetes Care, and One Touch of LifeScan.
hexacyanoferrate are examples of one-electron
mediators working in this relatively simple
manner. Two-electron mediators, e.g., quinones
are used as well. Phenanthroline quinone is the
mediator in Abbott Diabetes Cares Precision
Xtra
. The same enzyme/mediator system
may sometimes be used for photometric and
electrochemical measurement as is the case for
hexacyanoferrate, which was used as an elec-
trochemical mediator in many products and as
part of the now discontinued Accu-Chek Easy
(Boehringer Mannheim, Indianapolis, IN) pho-
tometric system.
Some mediator systems are more complex
than the simple scheme of Figure 2. The scheme
for GOD/peroxidase (POD) systems working
with atmospheric oxygen is shown in Figure 3.
This is a very atypical mediator system since
oxygen and hydrogen peroxide are not recy-
cled. Instead, the oxidative power of oxygen is
used in two steps: the first is dependent on glu-
cose, and the second uses the intermediate
formed to oxidize a leuco dye. A clear propor-
tionality of dye formation to glucose should be
the consequence. However, many dyes are also
substrates of GOD,
4
including the one formed
from tetramethyl benzidine. Using glucose,
they can be reduced again to the leuco dye.
With an excess of glucose over oxygen, nearly
no dye is formed. This is the explanation why
an early optical test strip, Chemstrip bG, did
not form significant amounts of color in the first
minute when the test pads were covered by the
sample. This could easily be observed using
aqueous glucose solutions instead of blood.
Only a faint blue borderline at the edge of the
sample drop indicated the reaction in this first
phase. Color formation was only visible after
wiping when oxygen freely diffused into the
layer and competed effectively with the dye for
the electrons from glucose. A further observa-
tion in Chemstrip bG was that hydrogen per-
oxide formed much more color than an equiv-
alent amount of glucose. Taking into account
that GOD uses only -D-glucose, which is two-
thirds of the full glucose concentration, we cal-
culated that the relative yield of dye from glu-
cose (normalized to the dye from hydrogen
peroxide) was between 60% at 1 mM and be-
low 10% at 30 mM. This deviation from clear
stoichiometry of the chemical reaction was em-
pirically built into the test strip formulation
during development. With high and constant
yield, the color at high glucose would have
been much too intensive for precise measure-
ment.
Apart from competition by oxygen, there are
also other reasons that drive the search for new
mediators. These include the basic require-
ments of stability and the ability to react
quickly with typical coenzyme sites (thus al-
lowing fast measurements and high signals), as
well as having low redox potentials that reduce
the cross-reactivity of mediators with other bi-
ological molecules, which can contribute to in-
accuracy. In the case of electrochemical sensors,
a lower redox potential of the mediator also al-
lows the measurement electrode to operate at
lower applied potential, also reducing interfer-
ing reactions and inaccuracy.
Nitrosoanilines are a further example of an
atypical test strip constituent in that they are
not mediators themselves, although they do
address many of the advantages listed
above.
10,11
Rather, they react in situ on the test
strip with glucose, and the enzyme to form a
HNES ET AL. S-14
Glucose Mediator
ox
2 Electrons Electrode
r o t a c i d n I e m y z n E
Glucono-
lactone Mediator
red
Glucose Oxygen
GOD
Glucono-
lactone
Hydrogen
peroxide
Leuco
dye
Glucono-
lactone
POD GOD
Water Dye Glucose
FIG. 2. Scheme of mediator action. The mediator is a
catalyst transferring reduction equivalents from the re-
duced enzyme/coenzyme system to an electrode or to a
color-forming indicator substance.
FIG. 3. Reactions in strips with athmosperic oxygen
mediator and GOD/POD enzymes. This is a very atypi-
cal mediator system since oxygen/hydrogen peroxide is
not recycled. Instead, the oxidative power of oxygen is
used in two steps. Because of the lack of specificity of
GOD, many dyes just formed can be reduced again using
a second molecule of glucose.
species that can act as a mediator. Figure 4
shows the mediator cycle derived from N,N-
bis-(2-hydroxyethyl)-4-hydroximino-cyclo-
hexa-2,5-dienylidene ammonium chloride. The
compound might be called a quinone diimine
oxide. It is in mesomeric equilibrium with the
corresponding C-nitrosoaniline (see Eq. 145 in
Boyer
12
). Unlike N-nitrosoanilines, which are
known to be potent carcinogens, it passed all
tests for mutagenesis and carcinogenesis with-
out positive results. Electrons eventually are
transferred either to an electrode in an electro-
chemical strip or to the indicator in a photo-
metric strip.
Many oxidoreductases accept nitrosoani-
lines for electron transfer, including the GDHs
with FAD and PQQ cofactors and GOD. The
enzymes catalyze a very similar reduction
twice. First they work with a quinone diimine
oxide, then with a quinone diimine. The first
intermediate, a hydroxylamine, is unstable be-
cause of the electron donating power of the p-
amino group and decays to the quinone di-
imine (see the reaction with NAD-dependent
dehydrogenases described below). Thus the
nitrosoaniline is a stable precursor for the
catalytically active and less stable mediator
pair quinone diimine/phenylenediamine. Af-
ter the second enzymatic reduction step, trans-
fer of electrons to a working electrode or to an
indicator like phosphomolybdic acid is a rapid,
nonenzymatic process.
Nitrosoanilines can be reduced by aldehyde
reductases or NAD-dependent alcohol dehy-
drogenases as well since the nitroso group is
isoelectronic with an aldehyde. Reduction
equivalents for this reaction come from NADH,
which in turn is oxidized to NAD. But the
mechanism is a hydride transfer to the nitroso
group, and the product is the quinone diimine
formed by nonenzymatic decay of the primary
reduction product, the aromatic hydroxyl-
amine.
13
This reaction does not produce reduc-
tive equivalents but a new oxidizing species,
and it is not used in glucose test strips.
Electrochemical reactions need a reaction at
the counter electrode to close the current cycle.
In this case we simply use the electrochemical
BLOOD GLUCOSE TEST STRIPS S-15
FIG. 4. The mediator system in Roche photometric strips (R HOCH
2
CH
2
). Many oxidoreductases accept ni-
trosoanilines for electron transfer including the GDHs with FAD and PQQ cofactors and GOD. The resulting re-
duction equivalents can be transferred to a working electrode or to a color-forming indicator substance. In the case
of electrochemical measurement, the current cycle is closed by a reduction at the counter electrode, which is com-
pletely equivalent to the enzymatic reduction.
reduction of nitrosoanilines, which proceeds
in the same way as the enzymatic route. It is
well known that aromatic nitroso compounds
with electron donating substituents are elec-
trochemically reduced in a four-electron reac-
tion to the corresponding anilines.
14
Thus ni-
trosoanilines are used successfully in both
photometric and electrochemical test strips
from Roche.
What is the reason for all those difficult
chemical reactions? Why not select the most
simple mediator reaction of hexacyanoferrate
III/hexacyanoferrate II, which is widely used
in todays products? The mediator reaction is
a potential source of interferences by reducing
agents. Uric acid and bilirubin are endogenous
sources; acetaminophen, dopamine, ascorbic
acid, and many other medications introduce
exogenous reduction equivalents. A simple in-
organic complex like ferricyanide is a redox
mediator without kinetic barriers and reacts
rapidly with all those compounds. We found
that the chemical interferences can be very
much improved using more complex chem-
istry. A mediator of high chemical selectivity is
an advantageous choice like the selection of a
specific enzyme. However, quantitative effects
of interferents are influenced by the properties
of dry chemistry layers and by design of the
measurement chamber and the measurement
method. Appropriate information on remain-
ing interferences can be found in the package
insert of test strips.
Enzyme kinetics
The interaction of enzymes with the sub-
strate glucose and the mediator is not a simple
saturation curve like the well-known
Michaelis-Menten kinetics. GOD and the PQQ-
and FAD-dependent GDH enzymes have only
a single active center. An ordered sequence of
reactions is necessary to transfer the electrons
from glucose to the mediator (Fig. 5).
At high concentrations of glucose, this sub-
strate may enter the active center even when
the coenzyme PQQ is in the reduced form of
PQQH
2
(formed by previous reaction with an-
other glucose molecule). The active center can-
not then accept oxidized mediator until glucose
dissociates again. Thus high concentrations of
substrate lead to inhibition of the desired reac-
tion. The same is true for high concentrations
of mediator binding to the oxidized form of the
enzyme. A detailed study of the interaction of
PQQ-dependent GDH with mediators derived
from nitrosoaniline and several sugars has
been published.
15
The other enzymes have the
same general mechanism. Mediator inhibition
phenomena have been detected with FAD-de-
pendent GDH as well (authors unpublished
data).
NAD-dependent GDH is different. Like in
other NAD-dependent dehydrogenases, both
the coenzyme and the substrate glucose are
bound at the same time near to each other but
in distinct parts of the active center. The mech-
anism does not show substrate or coenzyme in-
hibition. The interaction with the mediator is a
nonenzymatic one. Reductive equivalents are
transferred to mediators by nonenzymatic in-
teraction with the reduced form NADH in the
dissociated state. An inhibition of the enzy-
matic reaction by mediator is not to be expected
and has not been observed.
Dry chemistry layers
Test strips contain enzyme, mediator (or pre-
cursor), indicator, and many additional ingre-
dients in the form of dry layers. A very simple
approach for production is impregnation of a
HNES ET AL. S-16
FIG. 5. Catalytic mechanism of GlucDOR PQQ-dependent GDH. GlucD
OR
ox means that the oxidized coenzyme
PQQ; GlucDOR
red
means that the reduced form of the coenzyme PQQH
2
is bound to the protein scaffold of the en-
zyme.
preformed membrane with a buffered solution
of enzyme and indicator.
2
Screen printing has
been widely used as well.
16
Blade coating is the
method employed by Roche for photometric
strips, and the application is followed by dry-
ing. Usually this is done in continuous run-
through dryers. Short intensive drying is ad-
vantageous to avoid denaturation of enzyme
protein and/or unwanted prereactions of me-
diator and indicator. Many enzymes survive
surprisingly well even if dryer temperatures
reach 70C or 80C, a temperature well above
their melting point. Drying starts with evap-
oration of water from the wet layer holding
temperature far below the temperature of dry-
ing air. Drying ends with the dry hot layer
where the enzyme survives well for a few min-
utes since the liquid environment for denatu-
ration is absent. The critical phase is the time
when temperature rises towards the end of
drying when a little water is present. This
phase can be made as short as a few seconds.
The product of this process is a dry layer, which
then is processed into individual test strips.
Another process called slot-die coating is em-
ployed at Roche for their latest electrochemical
test strip. Here only a selected portion of a pre-
formed test strip base is coated with a thin
stripe of chemistry through a special slot open-
ing in a coating head.
17
Otherwise, the drying
considerations are very similar. A full overview
of the processes used for strip production is
outside the scope of this article.
Dry chemistry uses reactive ingredients that
are able to work in classical wet analytics as well.
However, important differences are obvious
when comparing to laboratory analytical test run-
ning in solution in a cuvette or the like (Table 2).
Mixing is absent in dry chemistry strips,
leading to inhomogeneous distribution of
product through the depth of the layer and in
the sample. The chemical system is open, i.e.,
the layer continuously admits water and glu-
cose from the sample and allows out-diffusion
of soluble ingredients like oxidized and re-
duced mediator, products, and possibly even
enzyme. Conversion of sample glucose is usu-
ally incomplete. An exception to this is the
coulometric method of Therasense FreeStyle.
18
Coulometry measures the total charge in the
capillary volume. This requires good control of
the volume to be analyzed. This means that the
height of the sample layer above the chemistry
layer needs to be held within narrow toler-
ances. Furthermore, a thin capillary space (50
m in the product above) is needed to speed
up the diffusion.
Incomplete conversion seems dangerous to
classic analytic thinking. For instance, how can
conversion speed of enzymes be controlled,
e.g., over cold and hot conditions? The key is
to transfer rate control to diffusion processes
instead of the enzyme/mediator reaction. This
is accomplished by overdosing of enzyme in
the chemistry layer. Once diffusion of glucose
is slower than its enzymatic conversion, even
at low temperature, the high dependency of
enzyme speed on temperature is eliminated.
However, even diffusion is sensitive to tem-
perature with approximately 2% change in
speed for a 1K change in temperature. Most
electrochemical strips show this dependency of
current on temperature. Usually the meter con-
tains a temperature sensor and calculates a glu-
cose value correction based on the estimate of
the temperature outside the meter where the
BLOOD GLUCOSE TEST STRIPS S-17
TABLE 2. A COMPARISON OF DRY CHEMISTRY WITH CONVENTIONAL LAB ANALYTICS
Dry chemistry Lab chemistry
Reagents Dry Wet
Chemistry format Layer Cuvette
Sample application On top of layer Mixing
Chemical system Open (continuous exchange of Closed (no exchange
ingredients with sample after mixing)
during reaction)
Conversion of analyte Partial
a
Full
a
Distribution of product Inhomogeneous Homogeneous
a
Exceptions dependent on analyte and measurement method.
reaction is actually taking place. This correction
falls short in the case of differences between
meter temperature and strip temperature, e.g.,
shortly after a temperature change such as re-
moving a meter from a hot car and testing out-
side (or vice versa). Therefore recommenda-
tions for appropriate waiting times before
testing under dynamic temperature conditions
are given in many meter manuals.
To overcome this inconvenience, Roche re-
cently introduced a novel dual-mode measure-
ment method using electrochemical impedance
in their Accu-Chek Aviva product line.
19
The
impedance measurement is used to determine
the actual temperature of the reaction zone and
correct the standard glucose estimate made by
the more conventional DC amperometric de-
termination.
Roche photometric layers employ a further
method for reduction of temperature influ-
ences. The dye heteropoly blue formed from
the mediator 2,18-phosphomolybdic acid is sol-
uble and diffuses out. This can easily be seen
when a drop of aqueous glucose solution, e.g.,
a control solution, is placed on an Accu-Chek
Active strip. The sample drop becomes green.
This means that yellow mediator-precursor
plus blue dye diffuse into the sample. After a
few seconds, the photometric signal from the
layer is stable, but coloration of the sample in-
creases. Our interpretation is that continued in-
diffusion of glucose (and conversion to dye) is
now compensated by out-diffusion of the dye.
Thus after a short time, a flow equilibrium with
constant dye concentration in the layer is es-
tablished. The temperature dependency of this
flow equilibrium and thus of the photometric
signal is low and needs only a small correction
by the temperature sensor in the meter. As ex-
pected from theory, in-diffusion of glucose and
out-diffusion of blue dye exhibit the same de-
pendency on temperature. Hematocrit depen-
dency is low as well since both diffusion paths
are influenced the same way by the diffusion
blocking effect of erythrocytes.
The compensation of in- and out-diffusion is
an effect that necessarily is present in any layer
when the product of glucose conversion is solu-
ble. This is not a special effect of photometric lay-
ers but applies to the electrochemical world as
well to some extent (Fig. 6). The relevant prod-
uct here is reduced mediator, which needs to be
soluble for diffusing to the electrode. The relation
between reduced mediator lost by diffusion into
the sample and reduced mediator used for oxi-
dation at the electrode is not known, however. A
complete exception is the use of polymer-bound
osmium mediator (TheraSense Freestyle),
18
which cannot diffuse out.
Most test strips today exclude erythrocytes
from entering the reaction layer, with the layer
surface acting as a filter. This is true even for
layers made exclusively from soluble ingredi-
ents. In the few seconds until a typical mea-
HNES ET AL. S-18
Diffusion of Glucose into layer
Diffusion of product(s) into sample
Sample
Chemistry layer
Sample
Chemistry layer
Carrier layer
Transparent
carrier layer
Electrodes
FIG. 6. Schematic cross section through the reactive area of test strips. Amperometric strips and photometric strips
are quite similar. Color formed from the reaction of glucose is observed visually or by means of reflection photome-
try from the side opposite to the sample through the transparent carrier layer in photometric strips (left). Electrode
reactions in amperometric strips (right) occur at the bottom of the chemistry layer opposite to the sample application
side. In either case, the chemistry layers exchange glucose, products, and all soluble ingredients with the sample by
means of diffusion.
surement is finished, complete dissolution and
homogeneous mixing with the sample do not
occur. Clogging by a filter cake of erythrocytes
is avoided by using very thin layers of a few
micrometers. The membrane in the LifeScan
One Touch only partially excluded blood cells.
This caused the necessity of two-wavelength
measurement.
2
Accutrend strips (Roche)
worked with a thick open film. Erythrocytes
were filtered above the chemistry layer using a
glass fiber fleece, which was an extremely rapid
filter. The chemistry layer filled in 0.5 s. How-
ever, the fleece was a volume filter needing
roughly half a millimeter in thickness. Thus
more than 10 L of sample volume was
needed, and this type of product is no longer
state of the art.
MEASUREMENT METHODS:
ELECTROCHEMISTRY AND
PHOTOMETRY
Both methods use similar designs of the de-
tection zone. In both cases, the sample is placed
on top of the layer even if a capillary transports
the sample to the layer from the side. The prod-
uct is observed from the side opposite to the
application of sample (Fig. 6), but the mea-
surement methods are different.
A photometric strip, the Accu-Chek Active,
is shown in Figure 7. Photometric measure-
ment is done by illumination with light. Usu-
ally a narrow wavelength bundle, e.g., from a
light-emitting diode, is used. A part of the dif-
fuse reflection arrives at a photodetector and is
converted to a current. The measurement can
be done with a very fast flash of light. The re-
action product is not changed at all by the mea-
surement, which is purely physical. Accuracy
and precision are clearly dominated by the
strip design in this case. Meter errors contrib-
ute to the system error, but nowadays meters
can be factory calibrated to make this contri-
bution low.
The area of chemistry layer times the neces-
sary thickness of sample over the layer defines
the volume needed since the volume uptake
into the layer is negligible with current thin
layer strips. The formation of color versus
thickness of sample follows a saturation curve,
i.e., only above a certain threshold, color be-
comes independent of sample thickness. The
measurement area is defined by the illumina-
tion area of the optics since the application spot
is usually made larger than the illumination
spot. The theoretical limit to lowering the area
and thus decreasing the necessary volume is
given by granularity of the layer leading to in-
creased variation. This limit is currently at a
sample volume of a few nanoliters (Fig. 8). This
ability is not used currently in any product
since the customer is not able to hit such a small
target area with such a tiny non-visible drop.
Amperometric or colorimetric measure-
ments, in contrast, convert the reaction prod-
uct, i.e., the reduced mediator, to the oxidized
form again. This reaction occurs at the surface
of the electrodes, and diffusion is needed to
transport reduced species to the surface and ox-
idized mediator away from it. The primary
product of the glucose reaction is changed in
this way. In principle, this is a slower process
than the instantaneous observation in photom-
etry; however, the reaction can be finished in a
few seconds or even below a second. Thus the
measurement time is not prolonged signifi-
cantly by comparison. Both electrochemical
and photometric strips have reached 5 s. But
even in the few seconds of applying voltage
and measuring current, the diffusion gradients
of reduced and oxidized mediator are not con-
fined to the few micrometers of the chemistry
layer, but reach out into the sample for those
systems with diffusing reagent components.
Diffusion is limiting the current, thus re-intro-
ducing temperature dependency. Diffusion
through the sample reintroduces hematocrit
dependency, which might have been mitigated
by the layer as described above.
Temperature dependency can be corrected
by the meter as described. Hematocrit depen-
dency can be mitigated by evaluating the pro-
file of current versus time in amperometric
measurements (for example, Accu-Chek Ad-
vantage [Roche, Indianapolis]). Significantly
better compensation of sample hematocrit (as
well as the strip temperature as described
above) is achieved with the addition of AC im-
pedance measurements used in the Accu-Chek
Aviva.
19
Electrochemical measurement quality
is a result of a close cooperation between dry
BLOOD GLUCOSE TEST STRIPS S-19
chemistry and measurement method including
the evaluation algorithm. Sophisticated correc-
tions by the meter are able to improve quality
far beyond the level of simple current mea-
surement. The allowed range (in terms of
hematocrit and temperature) for accurate mea-
surement can be wider than with the built-in
correction of photometric layers. But a word of
HNES ET AL. S-20
FIG. 7. Accu-Chek Active photometric test strip. Measurement is done from the bottom of the strip on the color
comparison field. Three light spots are used to detect for potential underdosing.
Homogeneity Accu-Chek Active film
0
1
2
3
4
5
6
7
0 0,2 0,4 0,6 0,8 1 1,2
detection area [mm]
CV [%]
CV% Sample 100
CV% Sample 250
sample volume [nl] 50 40 30 20 10 0
100 mg/dl
250 mg/dl
FIG. 8. Precision of photometric measurement versus evaluation area with the Accu-Chek Active chemistry layer.
The photometric film was evaluated with a CCD camera. Coefficient of variation (CV) values were calculated from
n 5. The chemistry film enables a precise measurement with 0.1 mm
2
or 316 m316 m area 50 m sample
thickness. This is equivalent to a 5 nl sample requirement.
caution may be allowed: the tolerance for de-
viations caused by temperature and hematocrit
seems to be company-specific. A wide allowed
range may be due to a good correction or to ac-
ceptance of large deviations.
20
The design of electrochemical test strips can
vary significantly, especially in the number of
electrodes used to contact the reagent and
blood sample and in the way in which they are
employed. One of the simplest designs such as
Accu-Chek Advantage
21
uses just two chemi-
cally identical electrodes in a biamperometric
measurement, where the actual potential ap-
plied to the strip is not referenced.
22
A refer-
ence electrode made from silver/silver chlo-
ride can be substituted for one of these two
electrodes to control and stabilize the absolute
potential applied at the measurement (or work-
ing) electrode. Another working electrode can
be added to make a three-electrode strip, as in
the case of LifeScans One Touch Ultra system,
to help safeguard against or compensate for ef-
fects unrelated to glucose concentration (e.g.,
partial filling of the strip or electrochemical re-
actions not derived from glucose). Further elec-
trodes can be added for better ensuring strips
are adequately filled before starting a mea-
surement sequence
23
(Fig. 9).
In any case, for amperometric measurements
(as opposed to coulometric), the measured cur-
rent and hence glucose estimation are propor-
tional to the working electrode area in the test
strip. Thus normal production tolerance and
accuracy issues define a lower limit to the prac-
tical size of the electrode, and hence to the sam-
ple size. However, recent advances in electrode
forming by laser ablation techniques
24
have
been employed in several systems, including
Accu-Chek Aviva and Bayer Contour. These
advanced techniques are able to produce elec-
trodes of highly precise dimensions, which
promises overall reduction of size and thus
sample volume. The sample volume is also
practically limited in the third dimension by
the ability to reproducibly control sample
chamber heights above the working elec-
trode(s), and hence avoid imprecision. As pre-
viously mentioned, the TheraSense FreeStyle
product currently uses the smallest sample
layer thickness above the electrodes of ap-
proximately 50 m.
In a nutshell, the differences between the two
measurement methods are the following:
Photometric layers are building blocks.
They can be cut and mounted as required by
the product design. In contact with sample,
they produce a signal needing only little pro-
cessing. Dependent on the optics, volumes
down to a few nanoliters can be measured
with state of the art layers. However, the
sample has to be placed just on top of the op-
tics, or a capillary is necessary for hygienic
sample transport.
Electrochemical measurement cells are sys-
tems where electrode area and capillary
thickness have a profound influence on the
signal in addition to the chemistry layer.
Measurement method and evaluation algo-
rithm strongly add to measurement quality.
Downsizing of volume to the nanoliter range
would likely require the construction of new
measurement cells and may need a revolu-
tion? in production methods. An advantage
to this point has been hygiene, specifically in
environments where a meter is used by more
than one individual.
ACCURACY AND PRECISION
State of the art systems nowadays achieve a
precision of 23% coefficient of variation (23
mg/dL SD below 100 mg/dL) and a deviation
within 5% (5 mg/dL below 100 mg/dL) of
the lab reference. More than 95% of all data
usually are within 15% as compared to the
reference. The medical need for accuracy was
described for many years by the Clarke error
grid.
25
A system error of 15% (15 mg/dL
below 100 mg/dL) completely fulfills this need.
In the hypoglycemic region, the tolerance for
positive bias is narrow, but above 60 mg/dL,
dry chemistry systems perform better than
needed. A newer error grid was proposed in
2000.
26
The tolerances in the hypoglycemic re-
gion are wider here. Generally, self-monitoring
systems perform fully within these require-
ments (Fig. 10).
With this in mind, improvements in accuracy
and precision may seem to be unnecessary. In
fact, most customers assume that accuracy ful-
BLOOD GLUCOSE TEST STRIPS S-21
HNES ET AL. S-22
0
50
100
150
200
250
300
350
400
450
500
0 50 100 150 200 250 300 350 400 450 500
Reference (Glucose, Hexokinase, mg/dL)
M
e
a
s
u
r
e
m
e
n
t
s
(
G
l
u
c
o
s
e
,
A
C
C
P
c
o
r
r
e
c
t
e
d
C
o
d
e
s
,
m
g
/
d
L
)
A
A
B
B
C
C
D D
E
E
FIG. 9.
FIG. 10.
fills the medical needs for managing their dis-
ease, and the Diabetes Control and Complica-
tions Trial study
1
supports that view. However,
there is much scientific debate around accu-
racy, including errors made by customers as
opposed to well-trained lab personal (see, for
example, Nichols
27
). The American Diabetes
Association
28
asks for improved systems with
a system error within 5%. Are new technol-
ogy and improved product development able
to fulfill this extreme or at least a more mod-
erate improvement? Lets have a closer look to
a less well-known source of errors, the lab ref-
erence. In 1999, we did an evaluation of the
Roche Glucotrend system versus the definitive
method using isotope dilution
29
(Fig. 11).
Glucotrend showed a system error (the
range for 95% of values) of just below 10%
versus the gas chromatography/isotope di-
lution mass spectrometry definitive method.
Usually, method comparisons versus the con-
ventional hexokinase reference method show
higher values with a mean of 13%. Appar-
ently there is a significant error contribution of
the conventional reference. The use of a perfect
reference system would improve accuracy to
10% without changes in the self-monitoring
system. Improving to 5% versus the conven-
tional reference would be hopeless, however,
since the error of the hexokinase method ver-
sus the definitive method was found to be
above 5% (data not shown). Improvements
clearly are completely excluded if the system
would have to match arbitrarily selected refer-
ences where ease of use and cost of the refer-
ence system are important and reference sys-
tems change from time to time.
27
The
experiment above is a snapshot only where
both the reference and customer systems were
well controlled. Handling errors in sample
preparation for the lab and in the use of self-
monitoring seem to be a much larger error con-
tribution than the apparent errors in this com-
parison. Our learning from many years of
in-house and external method comparisons is
that a reference needs to be controlled with
the same care as the self-monitoring system.
The situation is further exacerbated by the
fact that clinically obtained reference values are
sometimes derived from venous plasma sam-
ples as opposed to reference values derived
from capillary fingerstick sources. The known
physiological differences between these two
sample types for individuals not at glucose ho-
meostasis render more accurate strips even less
worthwhile if results are compared only to ve-
nous samples. Finally, the use of alternate sites
(arm, etc.) to glucose testing might be men-
tioned here. Again, equivalent glucose concen-
trations are observed only at glucose homeo-
stasis plus rapid capillary circulation. A perfect
glucose test strip certainly cannot compensate
for the potential errors in sample acquisition.
Our feeling is that accuracy improvements
should be worked on in the field of sample ac-
quisition and handling both in the reference
method and in the test strip system. Automa-
tized highly integrated spot monitoring sys-
tems are expected to show a high value here
because of error avoidance, although they are
originally intended for maximizing ease of use.
THE FUTURE
What does the future hold for self-monitor-
ing of blood glucose, and for test strips in par-
ticular? The rate of type 1 diabetes incidence,
which represents the majority of those that
need to monitor their blood glucose, is in-
creasing worldwide, although not nearly as fast
as type 2 diabetes, where monitoring is more
controversial. Nevertheless, there is some med-
ical consensus that those individuals with
noninsulin-dependent, type 2 diabetes should
still be testing at higher rates than currently
practiced even in the United States,
30
especially
those needing insulin therapy. A cure for dia-
BLOOD GLUCOSE TEST STRIPS S-23
FIG. 9. Accu-Chek Aviva electrochemical test strip. Two electrodes are used for the measurement. Further elec-
trodes are used for safety features.
FIG. 10. Method comparison of a test strip system with the hexokinase reference showing the Clarke error grid
25
zones AE. Data points represent pairs of glucose values using the Accu-Chek Compact Plus system and the hexo-
kinase reference method. Samples for both were obtained from the same fingerstick.
betes that would eliminate all need for moni-
toring is hoped for, but practically seems far
off. The closest we have come to a cure so far
is pancreas transplantation and islet cell trans-
plantation, which suffer from a lack of organ
availability and also bring with them the side
effects of continuous immune suppression. Ad-
ditionally, despite much initial optimism,
transplanted islet cells offer only transient mit-
igation of the disease.
Assuming the need for testing blood glucose
will exist for the next few decades, what might
be the alternatives to test strips or their equiv-
alents? Noninvasive measurement of blood
glucose has been the focus of intensive efforts
for the last 20 years or so. A wide variety of ap-
proaches have been assessed, but none has
overcome the fundamental issues. These are
that the observation would need to focus on a
volume where glucose is comparable to the
blood value and the general absence of specific
signals from glucose. When glucose levels are
measured from outside the body, there is no
property of glucose that has a unique interac-
tion with any part of the electromagnetic spec-
trum, making an accurate determination of this
molecule extraordinarily difficult.
Continuous monitoring, while still invasive,
has been proposed as an alternative to spot
monitoring. Improvements in accuracy clearly
would be needed to make the method accept-
able as a basis for insulin dosing. The devices
are still rather cumbersome, and even if re-
duced in size, all require an indwelling sensor
HNES ET AL. S-24
FIG. 11. Method comparison of Glucotrend versus the definitive isotope dilution method. Samples for data pairs
were taken from fingersticks (like in Fig. 10). The data demonstrate that the Glucotrend system is capable of a sys-
tem error (the range for 95% of values) of just below 10% versus the gas chromatography/isotope dilution mass
spectrometry (GC-IDMS) definitive method.
of some type that must be changed periodi-
cally. There are, indeed, medically valid use
cases where such high data density will yield
valuable metabolic insights and enable better
therapy optimization. We have no doubt that
these devices will take their appropriate place
in the arsenal available to patients and health-
care professionals, but we believe that higher
cost and more difficult handling will limit their
broad acceptance. However, potential benefits
are arguably not so much on the lines of inva-
siveness as they are on data density. We main-
tain that there are perhaps an equal number of
medical use cases where less dense and less in-
convenient, spot monitoring data will be suffi-
cient for the task at hand. In fact, Roche has re-
cently launched an episodic testing aid in the
form of the Accu-Chek 360 View data visual-
ization tool, which allows patients to chart a
special spot testing regimen of seven tests per
day for 3 days so that with their doctor they
can gain very useful information about their
disease and behavior.
31
The convenience and cost-effectiveness of in-
dividual blood glucose tests seem to justify their
continued existence for many years to come, and
this is particularly likely in the light of devel-
oping nations with less sophisticated infrastruc-
ture for healthcare delivery. Cost pressure on
developed healthcare systems acts in the same
direction. How will test strips and blood glucose
meters evolve? In the past, ease of use was im-
proved by the race for speed and low sample
volume. These parameters have reached mean-
ingful lower limits. However, ease of use and
the concurrent avoidance of handling errors re-
main important. As we continue to see the in-
troduction of the more convenient integrated
systems that incorporate the test elements in
drums, spools, or cartridges, even ease waste
disposal, and eventually might work in a fully
automated mode, it seems likely that the role of
strip technology in the market place will only be
extended. However, they will be even more hid-
den inside the system than today.
REFERENCES
1. The effect of intensive treatment of diabetes on the
development and progression of long-term compli-
cations in insulin-dependent diabetes mellitus. The
Diabetes Control and Complications Trial Research
Group. N Engl J Med 1993;329:977986.
2. Phillips R, McGarraugh G, Jurik F, Underwood R:
Minimum procedure system for the determination of
analytes. US Patent 4,935,346. June 19, 1990.
3. Keilin B, Hartree EF: Specificity of glucose oxidase.
Biochem J 1952;50:331341.
4. Leskovac V, Trivic S, Wohlfahrt G, Kandrac J, Pericin
D: Glucose oxidase from Aspergillus niger: the mech-
anism of action with molecular oxygen, quinones, and
one-electron acceptors. Int J Biochem Cell Biol 2005;
37:731750.
5. Olsthoorn AJJ, Duine JA: On the mechanism and
specificity of soluble, quinoprotein glucose dehydro-
genase in the oxidation of aldose sugars. Biochemistry
1998;37:1385413861.
6. Pauly HE, Pfleiderer G: D-Glucose dehydrogenase
from Bacillus megaterium. Hoppe Seylers Z Physiol
Chem 1976;356:16131623.
7. Tsujimura S, Kojima S, Kano K, Ikeda T, Sato M, Sanada
H, Omura H: Novel FAD-dependent glucose dehydro-
genase for a dioxygen-insensitive glucose biosensor.
Biosci Biotechnol Biochem 2006;70:654659.
8. Kratzsch P, Schmuck R, Bunk D, Shao Z, Thym D,
Knappe W: Variants of soluble pyrroloquinoline qui-
none-dependent glucose dehydrogenase. WO Patent
Application 2002/34919 A1. May 2, 2002.
9. Boenitz-Dulat M, Laggerbauer J, Schmuck R, Kratzsch
P, Knappe W: Genetically engineered pyrroloquino-
line quinone-dependent glucose dehydrogenase com-
prising an amino acid insertion. WO Patent Applica-
tion 2006/008132 A1. January 26, 2006.
10. Hoenes J: Colorimetric assay by enzymatic oxidation
in the presence of an aromatic nitroso or oxime com-
pound. US Patent 5,206,147. April 27, 1993.
11. Hoenes J, Schaeffler J: Method and sensor electrode sys-
tem for the electrochemical determination of an analyte
or an oxidoreductase as well as the use of suitable com-
pounds therefor. US Patent 5,122,244. June 16, 1992.
12. Boyer JH: Formation of the nitroso group and its re-
actions. In: Feuer H, ed. The Chemistry of the Nitro
and Nitroso Group. New York: Interscience Publish-
ers, 1969:258.
13. Kovar J, Plocek J: Investigation of the arylnitroso re-
ductase activity of pig liver aldehyde reductase.
Biochem J 1986;235:537543.
14. Fry AJ: The electrochemistry of nitro, nitroso, and re-
lated compounds. In: Patay S, ed. The Chemistry of
Amino, Nitroso, Nitro and Related Groups, Supple-
ment F2. New York: Wiley, 1996:846847.
15. Becker O: Die Glucose-Dye-Oxidoreduktase in der
klinischen Diagnostik: Kinetische Charakterisierung
und Thermostabilitt des Wildtyps sowie zweier
Mutanten des Enzyms aus Acinetobacter Calcoaceti-
cus [Ph.D. thesis]. Kaiserslautern, Germany: Univer-
sity of Kaiserslautern, 2005.
16. Hill HAO, Higgins IJ, McCann JM, Davis G, Treidl
BL, Birket NN, Plotkin EV, Zwanziger R: Printed elec-
trodes. European Patent 0351891B1. January 24, 1990.
BLOOD GLUCOSE TEST STRIPS S-25
17. Burke DW, Marquant M, Zapf U, Fritz M, Mosoiu D,
Wilsey C: Reagent stripe for test strip. US Patent Ap-
plication 20050016844A1. January 27, 2005.
18. Feldman BJ, Heller A, Heller E, Mao F, Vivolo JA, Fun-
derburk JV, Colman FC, Krishnan R: Small volume in
vitro analyte sensor with diffusible or non-leachable
redox mediator. US Patent 6,299,757. October 9, 2001.
19. Beaty TA, Kuhn LS, Svetnik V, Burke DW: Meter and
method of using the meter for determining the con-
centration of a component of a fluid. US Patent
6,645,368. November 11, 2003.
20. Kuhn LS, Burke DW, Henning Groll H, Celentano M,
Surridge N: Impedance techniques in blood glucose
biosensors: Accu-Chek Aviva. Poster presented at the
Biocrossroads Indiana Biosensor Symposium, Indi-
anapolis, IN, April 6, 2005.
21. Hill B: Accu-Chek
Advantage: electrochemistry for di-
abetes management. Curr Separations 2005;21(2):4548.
22. Kuhn L: Biosensors: blockbuster or bomb? Elec-
trochem Soc Interface 1998;7(4):2631.
23. Ikeda S, Yoshioka T, Nankai S, Tsutsumi H, Baba H,
Tokuno Y, Miyazaki S: Biosensor, and a method and a
device for quantifying a substrate in a sample liquid us-
ing the same. US Patent 5,582,697. December 10, 1996.
24. Bhullar RS, Diebold ER, Hill BS, Surridge NA,
Walling DP: Method of making a biosensor. US Patent
7,073,246. July 11, 2006.
25. Clarke WL, Cox D, Gonder-Frederick LA, Carter W,
Pohl SL: Evaluating clinical accuracy of systems for
self-monitoring of blood glucose. Diabetes Care
1987;10:622628.
26. Parkes JL, Slatin SL, Pardo S, Ginsberg BH: A new
consensus error grid to evaluate the clinical signifi-
cance of inaccuracies in the measurement of blood
glucose. Diabetes Care 2000;23:11431148.
27. Nichols JH: What is accuracy and how close must the
agreement be? Diabetes Technol Ther 2005;7:558562.
28. American Diabetes Association: Self-monitoring of
blood glucose. Diabetes Care 1994;17:8186.
29. Schumann G, Bttner J: Determination of glucose in
reference materials by isotope dilution-mass spec-
trometry. Fresenius J Anal Chem 1988;330:424425.
30. Bergenstal J, Gavin JR 3
rd
; Global Consensus Confer-
ence on Glucose Monitoring Panel: The role of self-
monitoring of blood glucose in the care of people with
diabetes: report of a global consensus conference. Am
J Med 2005;118(Suppl 9A):1S6S.
31. Childs B, Laan R: Development of a novel bG analy-
sis system for episodic bG monitoring in persons with
Type 2 diabetes. Poster 0427-P presented at the Amer-
ican Diabetes Association 67
th
Scientific Session,
Chicago, IL, 2007.
Address reprint requests to:
Dr. Joachim Hnes
Roche Diagnostics GmbH
Sandhofer Strae 116
68305 Mannheim, Germany
E-mail: joachim.hoenes@roche.com
HNES ET AL. S-26
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- NUTRITION EXPERT SCREENING ANSWERS-updatedDocument13 pagesNUTRITION EXPERT SCREENING ANSWERS-updatedatonymutembeiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Past Papers:BiochemistryDocument5 pagesPast Papers:BiochemistryMalavikaNNo ratings yet
- Assignment 1 - Food ChemistryDocument44 pagesAssignment 1 - Food ChemistryQuoc Khanh100% (2)
- Physioex Lab Report: Pre-Lab Quiz ResultsDocument3 pagesPhysioex Lab Report: Pre-Lab Quiz ResultsNicole de Leon0% (1)
- Handy Health Guide To DiabetesDocument49 pagesHandy Health Guide To DiabetesDiabetes Care100% (1)
- Breathing and Gas ExchangeDocument21 pagesBreathing and Gas ExchangeAnna DixonNo ratings yet
- Solution Manual For Human Biology 16th Edition Sylvia Mader Michael WindelspechtDocument36 pagesSolution Manual For Human Biology 16th Edition Sylvia Mader Michael Windelspechtoverspinmeetklac40100% (48)
- 03 Chemistry (25-Shift1)Document7 pages03 Chemistry (25-Shift1)abhiNo ratings yet
- Understanding Feed Analysis TerminologyDocument5 pagesUnderstanding Feed Analysis Terminologyamamùra maamarNo ratings yet
- Chapter I: Food Components: CarbohydrateDocument14 pagesChapter I: Food Components: CarbohydrateJaylina MabulayNo ratings yet
- Hydrolysis of StarchDocument5 pagesHydrolysis of StarchJann Russ EsmeraldaNo ratings yet
- UNIT4 Expt1Document6 pagesUNIT4 Expt1Christian Franco RuizNo ratings yet
- Sharad Pratap Singh's Answer To Is It Necessary To Memorise The Name of The Organic Reactions For JEE or Is The Mechanism and Reagents Enough - QuoraDocument7 pagesSharad Pratap Singh's Answer To Is It Necessary To Memorise The Name of The Organic Reactions For JEE or Is The Mechanism and Reagents Enough - QuorasumitNo ratings yet
- Midterm NutriDocument66 pagesMidterm NutriMaye ArugayNo ratings yet
- Review Article: Pullulanase: Role in Starch Hydrolysis and Potential Industrial ApplicationsDocument15 pagesReview Article: Pullulanase: Role in Starch Hydrolysis and Potential Industrial Applicationsbogdan marianNo ratings yet
- Experiment 3Document6 pagesExperiment 3lechupajarilloNo ratings yet
- Ig ScienceSingleAward TRPDocument71 pagesIg ScienceSingleAward TRPzunairaNo ratings yet
- पञ्चकर्म Part ADocument100 pagesपञ्चकर्म Part AAnil DasNo ratings yet
- K-YBGL Validation ReportDocument5 pagesK-YBGL Validation ReportThu HuyềnNo ratings yet
- Unit 2 - PFD - NumericalsDocument3 pagesUnit 2 - PFD - Numericalssannu986No ratings yet
- Ebook Eliminate Cancers Favorite Building Block Ty Bollinger TTAC PDFDocument32 pagesEbook Eliminate Cancers Favorite Building Block Ty Bollinger TTAC PDFmilanmanijakNo ratings yet
- Whole 4th Year SyllabusDocument161 pagesWhole 4th Year SyllabusPravesh NiraulaNo ratings yet
- Healthy Living Event Proposal 2013 Group 3Document7 pagesHealthy Living Event Proposal 2013 Group 3api-235001675No ratings yet
- What Is Organic Compound?Document3 pagesWhat Is Organic Compound?Mark Joseph LatadeNo ratings yet
- Bulking For MesomorphsDocument41 pagesBulking For MesomorphsSixp8ck100% (2)
- MOH Medicines Price List For Official Use As On 1st of Sep 2016Document579 pagesMOH Medicines Price List For Official Use As On 1st of Sep 2016Sajitha SujeeshNo ratings yet
- In Plant 2Document76 pagesIn Plant 2Nirban SahaNo ratings yet
- Chapter 10-Integration of MetabolismDocument4 pagesChapter 10-Integration of MetabolismJenelyn Lanang DiariosNo ratings yet
- Cmcchapter23 100613135130 Phpapp02 PDFDocument104 pagesCmcchapter23 100613135130 Phpapp02 PDFRicki HanNo ratings yet
- (DD13 14) Bio PhysioDocument587 pages(DD13 14) Bio PhysiominiarNo ratings yet