Professional Documents
Culture Documents
BIMC Adult DKA Protocol 2012
BIMC Adult DKA Protocol 2012
Uploaded by
Gavin TexeirraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BIMC Adult DKA Protocol 2012
BIMC Adult DKA Protocol 2012
Uploaded by
Gavin TexeirraCopyright:
Available Formats
BIMC Adult DKA Protocol, Page 1 of 5
BIMC ADULT DIABETIC KETOACIDOSIS (DKA) PROTOCOL
Aim: To establish a protocol for adults with diabetic ketoacidosis.
Rationale: Diabetic ketoacidosis is one of the most serious acute complications of diabetes. Therapy is
time sensitive and should be instituted as soon as possible. Having a unified protocol will allow for rapid
identification of DKA and early initiation of treatment in the emergency department (ED) which can be
continued until resolution of acidosis in the ED or once the patient is admitted to the hospital.
Eligibility: Adults (age18) with DKA are characterized by the triad of hyperglycemia, an anion gap
metabolic acidosis and ketonemia/ketouria.
If adult patients meet the DKA criteria, they should be enrolled in the DKA protocol and categorized
into either mild versus moderate-severe DKA.
DKA Criteria
1. FS 250
2. AG 12
3. Ketonemia/ketouria
DKA Severity
Mild: Venous pH 7.25
Moderate-Severe: Venous pH < 7.25
When patients come from the ED into the hospital and the protocol has already been initiated, the
protocol should be followed to completion. Please complete documentation on ER flow sheet.
Goals:
1.
2.
3.
4.
5.
Glucose level less than 250mg/dL
Anion gap (AG) less than or equal to 12
Volume resuscitation
Electrolyte management
Patient off continuous insulin infusion and back on home regimen or appropriate alternative
Protocol:
A. Once enrolled, all patients should get
1. An assessment for shock status
a. If in shock SBP<90 or MAP<65, intravenous fluid (IVF) resuscitation 20cc/kg wide open
b. If not in shock, IVF NS 1L over 1st hour, then 1L over 1-2hr, and another 1L over 1-2hrs
for goal IVF NS 4L by 5-9 hours
2. Initiation of an insulin drip accordingly for moderate-severe vs. mild DKA
a. moderate-severe: bolus 0.1U/kg and maintenance drip at 0.1 U/kg/hr
b. mild: no bolus and maintenance rate 0.14U/kg/hr
3. Checks of fingerstick glucose (FSG) hourly
4. Check of basic metabolic panel (BMP) every 4 hours
5. Check of initial CBC
6. Correction of potassium and magnesium as follows:
a. K 5.5: observe
b. 4.5 K < 5.5: IV potassium repletion
c. 3.3 K < 4.5: IV and PO potassium repletion
d. K < 3.3: IV and PO potassium repletion + add 40meq of KCL to NS infusion
7. A urinalysis and blood cultures before antibiotics (if indicated)
BIMC Adult DKA Protocol, Page 2 of 5
8. A chest x-ray (if indicated)
9. Blood pressure, heart rate and oxygen saturation monitoring per ED/ICU protocol
10. Supplemental oxygen or mechanical ventilation (if required)
B. If glucose still greater than 250:
1. If FSG decreased by 75-100 over last hour, maintain current insulin infusion rate
2. If FSG decreased by less that 75-100 over last hour, increase insulin drip by 1 unit per hour
3. Continue to check FSG hourly and BMP every four hours
C. If glucose less than/equal to 250, but anion gap is greater than 12:
1. Decrease insulin drip to current rate
2. Initiate D5 NS at 150cc/hr
3. Titrate D5 NS to keep glucose 150-250 mg/dL until acidosis resolves (anion gap 12)
4. Continue to check FSG hourly and BMP every four hours
D. If glucose less than/equal to 250 and anion gap is less than/equal to 12:
1. Test to see that patient can tolerate food
If patient is able to tolerate food:
2. Administer subcutaneous long-acting insulin in one of following doses:
a. home dose of long acting insulin and meal coverage
b. 0.5-0.8U/kg as daily dose for insulin nave50% long acting & 50% divided in 3 doses
for with-meal short acting insulin (for example: 70kg man to get 0.7*70U/day = 49U/day
~25U Lantus and ~25U/3 = ~8U regular insulin before meals)
3. Discontinue both insulin infusion and D5 NS infusion 1-2 hours after administration of
long-acting insulin
If patient is UNABLE to tolerate food:
4. Continue insulin drip
5. Continue IVF D5 NS fluid
6. Goal FSG 120-180
E. If hypoglycemic (FSG150)
1. If FSG <70
a. Administer 1 ampule of D50
b. Hold insulin drip for 15min and recheck FSG
c. If FSG >100, re-start insulin drip reduced rate ( rate)
d. Goal FSG > 150
2. If FSG 70-150
a. If patient is still has acidosis (AG >12):
i. Switch IVF from D5 NS to D10 NS and start at 150ml/hr
ii. Hold insulin drip for 15min and recheck FSG
iii. If FSG >100, re-start insulin drip reduced rate ( rate)
iv. Goal FSG > 150
b. If patient no longer has acidosis (AG 12):
i. Increase IVF D5 NS rate by 50-150ml/hr
ii. Hold insulin drip for 15min and recheck FSG
iii. If FSG >100, re-start insulin drip reduced rate ( rate)
iv. Goal FSG > 150
BIMC Adult DKA Protocol, Page 3 of 5
BIMC Adult DKA Protocol, Page 4 of 5
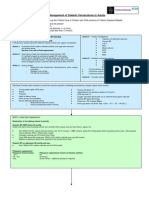
Adult Diabetic Ketoacidosis Treatment Algorithm
* volume expansion is key & must occur simultaneously, see Volume Resuscitation
Acute Phase
250 mg/dL
<250 mg/dL
Did glucose
by 75-100
over last hour?
no
Mild (VBG pH7.25)
Insulin drip 0.14U/kg/hr
Assess acidosis:
AG 12 (or known baseline)
* If next SMA not done, assume still acidotic
yes
yes
1.
IV insulin
by 1 unit/hr
Severe (VBG pH<7.25)
Bolus 0.1U/kg Insulin
and start drip at 0.1U/kg/hr
Check
glucose
Keep IV insulin
at current rate
2.
(If on D5, may need )
3.
IV insulin to
current rate
Start D5NS (or
D5NS) at 150ml/hr
Keep glucose 150-250
until Acidosis resolves
Transition Phase
no
Enter
Transition Phase
Start
Is patient able to eat?
test a few bites of food
no
Maintain IV insulin
& D5 at current rate
until can eat
Check glucose
q1-hour
yes
Feed & Provide SQ insulin
Option #1:
Start home dose of long acting insulin and
meal coverage
Option #2:
Start 0.5-0.8U/kg as daily dose for insulin nave
(50% long acting; 50% subdivided in 3 for
with-meal short acting insulin)
After 1-2 hours: Discontinue IV insulin & D5 infusions
BIMC Adult DKA Protocol, Page 5 of 5
Laboratory Work-Up
Initially (time=0)
Repetition Frequency
Absolute
Blood glucose (fingerstick)
Complete metabolic panel (SMA20
and magnesium)
VBG for pH (mild vs severe DKA)
CBC
Urinalysis, EKG, CXR (DKA trigger)
Lactate (other cause of AG)
Serum/urine ketones
Recommended
HbA1C
Every 1 hour
Every 4 hours (SMA10 with
magnesium and phosphorus)
Every 4 hours until normal
Volume Resuscitation
Patients in shock
SBP<90 or MAP<65
Patients not in shock*
20cc/kg NS wide open
Consider addition of vasopressors
Evaluate for cause other than hypovolemia
1L NS over 1st hour then
1L NS over 1-2 hours then
1L NS over 1-2 hours then
1L NS over 2-4 hours
Should have 4L in by 5-9 hours
* may need to be adjusted for patients with ESRD or CHF
Electrolyte Repletion
Potassium (Patients are most often total body K+ depleted)
K+ 5.5
observe
4.5 K+ < 5.5
IV Potassium repletion
Consider adding 20meq of KCL to NS infusion
IV Potassium repletion
Consider adding 40meq of KCL to NS infusion
IV/PO Potassium repletion
Consider adding 40meq of KCL to NS infusion
Hold insulin and give 20-30meq/hr until >3.3**
3.3 K+ < 4.5
K+ < 3.3
**only if able to recheck K within 1hr in ICU or ER setting via VBG/ABG
Magnesium & Phosphorus: Aggressively replete (goal Mg>1.6, Ph>2.5)
You might also like
- Fitzpatricks Dermatology 9th Edition 3123Document1 pageFitzpatricks Dermatology 9th Edition 3123DennisSujayaNo ratings yet
- UntitledDocument1 pageUntitledZaakira SyedNo ratings yet
- Nursing Fluids and ElectrolytesDocument14 pagesNursing Fluids and Electrolytesaga1028100% (18)
- Guideline of ExtravasationDocument35 pagesGuideline of ExtravasationAura Lorena Rivas Zambrano100% (1)
- 2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes AlgorithmDocument1 page2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes Algorithmms_lezahNo ratings yet
- EPALS Regulations April 2016Document8 pagesEPALS Regulations April 2016Chengyuan ZhangNo ratings yet
- CPAP Cannulaide Pocket GuideDocument2 pagesCPAP Cannulaide Pocket GuidepacsolanoNo ratings yet
- CASP Diagnostic Test Checklist 31.05.13Document6 pagesCASP Diagnostic Test Checklist 31.05.13itho23No ratings yet
- 2015 Neonatal AnesthesiaDocument464 pages2015 Neonatal AnesthesiajulianalaiscNo ratings yet
- Objective Assessment: Hameed LatifDocument16 pagesObjective Assessment: Hameed LatifSyeda Zainab Abbas100% (1)
- Managing Anaphylactic Shock Journal of Modern Pharmacy 2006Document3 pagesManaging Anaphylactic Shock Journal of Modern Pharmacy 2006Saputro AbdiNo ratings yet
- Anaphylaxis Treatment ProcedureDocument4 pagesAnaphylaxis Treatment ProcedureIvy Jorene Roman RodriguezNo ratings yet
- GEA ProtocolsDocument101 pagesGEA Protocolsffbrians100% (1)
- Atls SpineDocument11 pagesAtls SpineRonald David EvansNo ratings yet
- Pediatric Head InjuryDocument9 pagesPediatric Head InjuryAndy WijayaNo ratings yet
- Chest Pain ProtocolDocument4 pagesChest Pain ProtocolArul ShanmugamNo ratings yet
- 2.basic Life SupportDocument7 pages2.basic Life SupportNay ThureinNo ratings yet
- Post Op LaryngospasmDocument2 pagesPost Op Laryngospasmbalab2311No ratings yet
- Intraoperative Fluid ManagementDocument15 pagesIntraoperative Fluid ManagementMirela Marina BlajNo ratings yet
- LaryngospasmDocument3 pagesLaryngospasmbalab2311No ratings yet
- ACLS Study GuideDocument30 pagesACLS Study GuidemmmmzNo ratings yet
- Mechanical Ventilation and Intracranial PressureDocument30 pagesMechanical Ventilation and Intracranial PressureFlavius AnghelNo ratings yet
- CPR Training ModuleDocument22 pagesCPR Training ModuleSunil KbNo ratings yet
- Major Haemorrhage ProtocolsDocument3 pagesMajor Haemorrhage ProtocolsleicesterbugNo ratings yet
- Capnography Reference Handbook: Capnostat Loflo Flotrak Elite AccessoriesDocument40 pagesCapnography Reference Handbook: Capnostat Loflo Flotrak Elite AccessoriesLizzie RamosNo ratings yet
- Basic Life Support: BY Pooja LakshmananDocument35 pagesBasic Life Support: BY Pooja LakshmananJaunita MathewNo ratings yet
- For Best Viewing:: Open in Slide Show Mode Click On IconDocument32 pagesFor Best Viewing:: Open in Slide Show Mode Click On IconSutapa PawarNo ratings yet
- Post Cardiac ArrestDocument2 pagesPost Cardiac ArrestAlthea AlcalaNo ratings yet
- ACLS Online Training Material: Unit One: General ConceptsDocument34 pagesACLS Online Training Material: Unit One: General ConceptsJohn JenjinsNo ratings yet
- Informed Consent For Lasik SurgeryDocument2 pagesInformed Consent For Lasik SurgeryMoerieda RinquestNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Simon JosanNo ratings yet
- Pals Life SaverDocument13 pagesPals Life SaverStephany ZamorasNo ratings yet
- Scape Vs FospeDocument5 pagesScape Vs FospeDr. FarhanNo ratings yet
- IntroductionDocument5 pagesIntroductionFarhan YulmiadiNo ratings yet
- Surgical Cricothyrotomy (Assist)Document5 pagesSurgical Cricothyrotomy (Assist)ydtrgnNo ratings yet
- Initial Evaluation VertigoDocument8 pagesInitial Evaluation VertigoTanri Hadinata WiranegaraNo ratings yet
- Basic Life SupportDocument25 pagesBasic Life Supportguido pirelaNo ratings yet
- Lesson Plan Human Reproductive SystemDocument2 pagesLesson Plan Human Reproductive SystemGarnis HakimNo ratings yet
- The Neuro Exam: Yes, You Really Do Have To Wake Them Up and Do ThisDocument12 pagesThe Neuro Exam: Yes, You Really Do Have To Wake Them Up and Do ThisDrGasnasNo ratings yet
- Poster 10 PALS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 PALS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- Test Tasks On Pharmacology Module2Document19 pagesTest Tasks On Pharmacology Module2Blessing NwosuNo ratings yet
- Laryngospasm AnesthesiaDocument5 pagesLaryngospasm AnesthesiaLourdes CastilloNo ratings yet
- Initial Assessment and Management: Presented by Fayez Abillama, MDDocument53 pagesInitial Assessment and Management: Presented by Fayez Abillama, MDDaniel GhosseinNo ratings yet
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- Ventricular Fibrillation/ Pulseless Ventricular Tachycardia AlgorithmDocument2 pagesVentricular Fibrillation/ Pulseless Ventricular Tachycardia AlgorithmsafasayedNo ratings yet
- Airway-RSI Pocket CardDocument4 pagesAirway-RSI Pocket CardbellerevolteNo ratings yet
- Cardiac Arrest Vtach and VfibDocument1 pageCardiac Arrest Vtach and VfibBelle A. BasilioNo ratings yet
- Questions FinalDocument3 pagesQuestions FinalKeerthi Chowdary AmaraneniNo ratings yet
- Acls Study Guide 2016 For Pulse 2016Document8 pagesAcls Study Guide 2016 For Pulse 2016eng78ineNo ratings yet
- Truspected Stroke AlgorithmDocument4 pagesTruspected Stroke Algorithmtri wahyunoNo ratings yet
- Galectin ReviewDocument24 pagesGalectin ReviewmaniiiiiiiiNo ratings yet
- Mechanical ThrombectomyDocument58 pagesMechanical Thrombectomyres.uditacharyaNo ratings yet
- ACLS Full LectureDocument47 pagesACLS Full LectureAdhydeva Purusanti100% (3)
- Advanced Cardiovascular Life Support (ACLS)Document2 pagesAdvanced Cardiovascular Life Support (ACLS)Vijay MgNo ratings yet
- Role Play Code BlueDocument2 pagesRole Play Code BlueKrzia TehNo ratings yet
- King Airway: Norcal Ems Training ModuleDocument13 pagesKing Airway: Norcal Ems Training Moduleandrew22No ratings yet
- Pals Pediatric BradycardiaDocument1 pagePals Pediatric BradycardiadarlingcarvajalduqueNo ratings yet
- Traumatic Brain InjuryDocument40 pagesTraumatic Brain InjuryRed DevilNo ratings yet
- Delayed Recovery From AnaesthesiaDocument15 pagesDelayed Recovery From AnaesthesiaSheldon OltonNo ratings yet
- Neonatal ResuscitationDocument7 pagesNeonatal ResuscitationJavier López García100% (1)
- ILS Case Studies COMP 2020.ppsxDocument39 pagesILS Case Studies COMP 2020.ppsxKim Orven KhoNo ratings yet
- IV Drip CalculationsDocument4 pagesIV Drip CalculationsmydewyboyNo ratings yet
- Guidelines For Management of Diabetes MellitusDocument1 pageGuidelines For Management of Diabetes MellitusthapanNo ratings yet
- DKA Protocol TGDocument11 pagesDKA Protocol TGabelNo ratings yet
- Diabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: DiagnosisDocument1 pageDiabetic Ketoacidosis (D.K.A) Beaumont Hospital Protocol: Diagnosislouglee9174100% (1)
- Clinical Pathway StrokeDocument8 pagesClinical Pathway StrokedjizhieeNo ratings yet
- Acute Ischemic Stroke PathwayDocument50 pagesAcute Ischemic Stroke PathwaydjizhieeNo ratings yet
- TocDocument727 pagesTocdjizhiee100% (1)
- Heart Failure Pathway PDFDocument7 pagesHeart Failure Pathway PDFdjizhieeNo ratings yet
- Dka Management of Dka in Adults March 20101Document24 pagesDka Management of Dka in Adults March 20101djizhieeNo ratings yet
- Dka Guidelines - 2012Document4 pagesDka Guidelines - 2012djizhieeNo ratings yet
- Penatalaksanaan Cedera Muskuloskeletal: Kuncahyo Kamal Arifin, DR, SpotDocument68 pagesPenatalaksanaan Cedera Muskuloskeletal: Kuncahyo Kamal Arifin, DR, SpotdjizhieeNo ratings yet
- Travel Medicine and Tourism - Jontari Hutagulung S. KPDocument112 pagesTravel Medicine and Tourism - Jontari Hutagulung S. KPdjizhiee100% (1)
- FORM - (FMLA) FAMILY HealthDocument3 pagesFORM - (FMLA) FAMILY HealthRavi SankarNo ratings yet
- Anemia in PregnancyDocument14 pagesAnemia in PregnancyWern Ching Lee50% (2)
- AripiprazolDocument12 pagesAripiprazolGabriel LemosNo ratings yet
- Third Year Paper 2020 - 1999 by DENTOWESOMEDocument60 pagesThird Year Paper 2020 - 1999 by DENTOWESOMENeeraja VeerisettyNo ratings yet
- Fleas ParasitologyDocument54 pagesFleas Parasitologyhuyenthanh1807No ratings yet
- Azmi - Uji Antibakteri Daun SingkongDocument10 pagesAzmi - Uji Antibakteri Daun SingkongimaNo ratings yet
- QuestionsDocument61 pagesQuestionsTop MusicNo ratings yet
- German Measles RubellaDocument4 pagesGerman Measles Rubellaklinik mandiriNo ratings yet
- Christine P. SalimbagatDocument2 pagesChristine P. SalimbagatChristine Pialan SalimbagatNo ratings yet
- Complement-Dependent Cytotoxicity (CDC) To Detect Anti-HLA Antibodies Old But GoldDocument6 pagesComplement-Dependent Cytotoxicity (CDC) To Detect Anti-HLA Antibodies Old But Goldhoangphuong08101992No ratings yet
- Cordia Viral MeningitisDocument7 pagesCordia Viral MeningitisAyuagung Chandra Maha DewiNo ratings yet
- DRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesDocument3 pagesDRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesManuel BetancurNo ratings yet
- BDS Examiners Panel List 2013Document391 pagesBDS Examiners Panel List 2013Suman KashyapNo ratings yet
- Multicultural Nursing Care of Patients - NWS1665191866 - NRSE 4570 - Care Plan - 1Document4 pagesMulticultural Nursing Care of Patients - NWS1665191866 - NRSE 4570 - Care Plan - 1Carlos I. RomeroNo ratings yet
- Endodontic Treatment With 3mix-MpDocument7 pagesEndodontic Treatment With 3mix-MpSergio Llufire MendozaNo ratings yet
- Difference Between Humoral and Cell Mediated Immunity: September 2017Document9 pagesDifference Between Humoral and Cell Mediated Immunity: September 2017Nitish SharmaNo ratings yet
- Instructions For Use of Polytech Breast Implants Manual (Multilingual)Document88 pagesInstructions For Use of Polytech Breast Implants Manual (Multilingual)Mark RothenbergNo ratings yet
- Chest X-Ray (CXR) Interpretation 2Document30 pagesChest X-Ray (CXR) Interpretation 2NaveedNo ratings yet
- Shyla Genslak Nursing Resume Sept 2014 With Clinical ExperienceDocument4 pagesShyla Genslak Nursing Resume Sept 2014 With Clinical Experienceapi-259585170No ratings yet
- Skill Lab SpecificationsDocument17 pagesSkill Lab Specificationssrboghe651665No ratings yet
- Improve The Efficiency of The Yaskawa Motoman mh5 Robot ForDocument9 pagesImprove The Efficiency of The Yaskawa Motoman mh5 Robot Fornicolas casanovaNo ratings yet
- Treating HomestasisDocument49 pagesTreating HomestasisFahadNo ratings yet
- Doh DC 2018-0142Document2 pagesDoh DC 2018-0142vanceNo ratings yet
- LK 2015 Dislokasi SendiDocument5 pagesLK 2015 Dislokasi SendiTriaditya KresnaNo ratings yet
- Ust-Fms 2A-Med 1 Shift A.Y. 2016-2017: Yellow GreenDocument6 pagesUst-Fms 2A-Med 1 Shift A.Y. 2016-2017: Yellow GreenNathaniel CamangonNo ratings yet
- Lecture 1 Cell Injury Adpation and DeathDocument39 pagesLecture 1 Cell Injury Adpation and Deathyat yat szeNo ratings yet