Professional Documents
Culture Documents
Migraine
Migraine
Uploaded by
jagdish_vankarCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Migraine
Migraine
Uploaded by
jagdish_vankarCopyright:
Available Formats
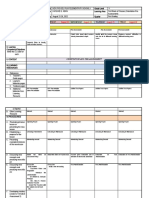
Quick Reference: GUIDELINE FOR PRIMARY CARE
MANAGEMENT OF HEADACHE IN ADULTS
July 2012
Red flags:
Emergent (address immediately)
Thunderclap onset
Fever and meningismus
Papilloedema (+focal signs or reduced LOC)
Acute glaucoma
Urgent (address hours to days)
Temporal arteritis
Papilloedema (NO focal signs or reduced LOC)
Relevant systemic illness
Elderly: new headache with cognitive change
Yes
Refer and/or investigate
Possible indicators of secondary headache:
Unexplained focal signs
Atypical headaches
Unusual headache precipitants
Onset after age 50
Aggravation by neck movement; abnormal
neck exam. Consider cervicogenic headache.
Jaw symptoms; abnormal jaw exam. Consider
temporomandibular disorder.
No
Headache with 2 or more of:
Nausea
Light sensitivity
Interference with activities
Migraine
Yes
Practice points:
Migraine historically under diagnosed
Consider migraine diagnosis for
recurring sinus headache
Bilateral headache
Nonpulsating pain
Mild to moderate pain
Not worsened by activity
No
Ergots, triptans, combination
analgesics or codeine/other
opioids 10 days a month
OR
Acetaminophen or NSAIDs 15
days a month
Manage
No
Headache w/o nausea and 2 or
more of:
Medication overuse:
Assess
Tension-type
Headache
Yes
Educate patient
Consider prophylactic
medication
Provide an eective acute med
for severe attacks with
limitations on frequency of use
Gradual withdrawal if opioid, or
combination analgesic with
opioid or barbituate
Abrupt (or gradual) withdrawal
if acetaminophen, NSAIDs or
triptan
All of:
All of:
Unilateral headache (always same side)
Continuous
Dramatically responsive to
indomethacin
Headache continuous since onset
Acute medication (Table 1)
Monitor for medication overuse
Prophylactic medication (Table 1), if
headache:
> 3 days/month and acute
meds not eective
OR
> 8 days/month (risk of overuse)
OR
Disability despite acute meds
Behavioural management
Headache diary: record frequency,
intensity, triggers and medication
Adjust lifestyle factors: reduce
caeine, ensure regular exercise, avoid
irregular and/or inadequate sleep or
meals
Stress management: relaxation
training, CBT, pacing activity, biofeedback
Tensiontype headache
Acute medication (Table 2)
Monitor for medication overuse
Prophylactic medication if disability
despite acute meds (Table 2)
Uncommon headache syndromes
Frequent headache
Severe
Brief < 3 hours per attack
Unilateral (always same side)
Ipsilateral eye redness, tearing
and/or restlessness during attacks
Migraine
Cluster headache or another
trigeminal autonomic cephalalgia
Yes
Management primarily pharmacological
Acute medication (Table 3)
Prophylactic medication (Table 3)
Early specialist referral recommended
Yes
Hemicrania continua
specialist referral
Yes
New daily persistent headache
specialist referral
The above recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care
for specic clinical circumstances. They should be used as an adjunct to sound clinical decision making.
You might also like
- Unit 3 Progress TestDocument6 pagesUnit 3 Progress Testnowpat2No ratings yet
- Administrative Behavior:: Meaning, Functions, Domains and TypesDocument12 pagesAdministrative Behavior:: Meaning, Functions, Domains and TypesCatherine AbabonNo ratings yet
- Migraine LeafletDocument6 pagesMigraine LeafletEliza Sitinjak100% (1)
- Voice and Participation in The Modern Workplace Challenges and ProspectsDocument17 pagesVoice and Participation in The Modern Workplace Challenges and Prospectsjcalleja1716100% (1)
- HeadacheDocument16 pagesHeadacheBagoes Ario BimoNo ratings yet
- Migraine and You: An Educational Guide For Migraine Headache SufferersDocument23 pagesMigraine and You: An Educational Guide For Migraine Headache SufferersagelsantosNo ratings yet
- Migraine FlowchartDocument2 pagesMigraine FlowchartKemunto OnchwariNo ratings yet
- Headache SummaryDocument3 pagesHeadache Summaryhameedsabah36No ratings yet
- Headache: An Overview: Danish Ejaz BhattiDocument43 pagesHeadache: An Overview: Danish Ejaz BhattiPGHCNo ratings yet
- Depressive DisordersDocument7 pagesDepressive DisordersEllen JulianNo ratings yet
- Tension Type HeadacheDocument18 pagesTension Type HeadacheRiris SihotangNo ratings yet
- Neuro Dr. RehabDocument142 pagesNeuro Dr. RehabMohammed Saad NabhanNo ratings yet
- Journal Reading Syaraf-SuleDocument45 pagesJournal Reading Syaraf-SuleDrosophila Meilani GasterNo ratings yet
- Diagnoses and Management Acute Headache Emergency DepartmentDocument37 pagesDiagnoses and Management Acute Headache Emergency DepartmentBendy Dwi IrawanNo ratings yet
- HeadacheDocument41 pagesHeadacheNatalia Khan100% (1)
- Cefaleas 2018Document87 pagesCefaleas 2018Anonimo DesconocidoNo ratings yet
- Headache - A Quick TutorialDocument7 pagesHeadache - A Quick TutorialLeilia FibrianasariNo ratings yet
- Headache 2Document11 pagesHeadache 2khaled alahmadNo ratings yet
- Advances in Migraine Prevention: Clinical Experience With TopiramateDocument64 pagesAdvances in Migraine Prevention: Clinical Experience With TopiramateontabarkerNo ratings yet
- Drug StudyDocument3 pagesDrug StudyGlaiza M. BañaresNo ratings yet
- Headache: & Associated EmergenciesDocument63 pagesHeadache: & Associated EmergenciesMahad IbrahemNo ratings yet
- 5 Headache Algorithm: Chapter 2 - Diagnostic AlgorithmsDocument3 pages5 Headache Algorithm: Chapter 2 - Diagnostic AlgorithmsNdaa JutexNo ratings yet
- Ukdi Preparation I:: Neurogenic Pain Syndromes Peripheral Nerve DisordersDocument65 pagesUkdi Preparation I:: Neurogenic Pain Syndromes Peripheral Nerve DisordersFelicia SutarliNo ratings yet
- Care of The Client With Altered Intracranial Functioning: Headaches Seizures Meningitis/EncephalitisDocument33 pagesCare of The Client With Altered Intracranial Functioning: Headaches Seizures Meningitis/Encephalitisdcline18No ratings yet
- Activity 56 Headache Zillah QuizolDocument6 pagesActivity 56 Headache Zillah QuizolARAGON GEMMA LYNNo ratings yet
- Anti Psychotic DrugsDocument2 pagesAnti Psychotic DrugsJohn Corpuz100% (1)
- Yuli - Kuliah Blok 11 - Headache 2019Document66 pagesYuli - Kuliah Blok 11 - Headache 2019reshaNo ratings yet
- Psychotropic Drugs: By: Rheajane Aguilar-RosalesDocument77 pagesPsychotropic Drugs: By: Rheajane Aguilar-Rosalesjean samson100% (1)
- Headache Disorder and Pain ManagementDocument11 pagesHeadache Disorder and Pain ManagementDaenica Lorraine Abella SebastianNo ratings yet
- 3B2 Preceptorial Nov 18 SFSeizuresDocument79 pages3B2 Preceptorial Nov 18 SFSeizuresAbigail PaasaNo ratings yet
- Headache Management: Dr. Pawan BhusalDocument34 pagesHeadache Management: Dr. Pawan BhusalNabin pokhrelNo ratings yet
- HaloperidolDocument2 pagesHaloperidolMikz JocomNo ratings yet
- 4 HeadacheDocument33 pages4 HeadacheNathaniel BudayNo ratings yet
- Tension-Type HeadacheDocument10 pagesTension-Type HeadacheImran KhanNo ratings yet
- Trigeminal Autonomic CephalalgiasDocument23 pagesTrigeminal Autonomic CephalalgiasAmelia GunawanNo ratings yet
- Bipolar Lecture11Document5 pagesBipolar Lecture11hhanono924097No ratings yet
- 4 Headache PDFDocument39 pages4 Headache PDFJohn Ryan ParisNo ratings yet
- MigraineDocument16 pagesMigraineBheru LalNo ratings yet
- Nursing-Bullets Compress PDFDocument73 pagesNursing-Bullets Compress PDFheluNo ratings yet
- Headache: by Yahya Ibrahim MBCHB 3. Dr. BacwaDocument54 pagesHeadache: by Yahya Ibrahim MBCHB 3. Dr. BacwaHarun MohamedNo ratings yet
- Module 10Document5 pagesModule 10Yuki Xairah TunayNo ratings yet
- Headache in Primary CareDocument32 pagesHeadache in Primary CareSaif SinghNo ratings yet
- Unit 2 Anti Migraine and Drugs For Trigeminal Neuralgia Pharmacy-IIDocument38 pagesUnit 2 Anti Migraine and Drugs For Trigeminal Neuralgia Pharmacy-IIAsad MirajNo ratings yet
- MigraineDocument16 pagesMigraineAbigail CruzNo ratings yet
- HA, Fever, PainDocument11 pagesHA, Fever, PainLeonardo RanderNo ratings yet
- Pharmacotherapy 1 Pain Fever Musculoskeletal Pain 2024Document64 pagesPharmacotherapy 1 Pain Fever Musculoskeletal Pain 2024elifuygur09No ratings yet
- Basic Mouse and Keyboarding PPDocument65 pagesBasic Mouse and Keyboarding PPfouadNo ratings yet
- Physical Diagnostics - HeadacheDocument7 pagesPhysical Diagnostics - Headachemskleon1No ratings yet
- CCJM Relieving Migraine PainDocument12 pagesCCJM Relieving Migraine PainBrian HarrisNo ratings yet
- Migraine Diagnosis: SupplementsDocument3 pagesMigraine Diagnosis: Supplementsseema yadavNo ratings yet
- Management of Opioid Withdrawal and Relapse PreventionDocument34 pagesManagement of Opioid Withdrawal and Relapse PreventionJared KeburiNo ratings yet
- PsychopharmacologyDocument84 pagesPsychopharmacologyKhyra Ysabelle VillanuevaNo ratings yet
- Headache 2Document21 pagesHeadache 2geeeelzy07No ratings yet
- AntipsychoticsDocument36 pagesAntipsychoticsGlory MimiNo ratings yet
- Beta Blocker TitrationDocument2 pagesBeta Blocker TitrationAwalunisa IstiqomahNo ratings yet
- E-Therapeutics+ - Minor Ailments - Therapeutics - Central Nervous System Conditions - Vertigo and DizzinessDocument5 pagesE-Therapeutics+ - Minor Ailments - Therapeutics - Central Nervous System Conditions - Vertigo and DizzinessSamMansuriNo ratings yet
- Drug Levothyroxine SodiumDocument2 pagesDrug Levothyroxine SodiumSrkocher0% (1)
- Medical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcFrom EverandMedical Encyclopedia XXL: Prof. J.P. Schadé, M.D., Ph.D. D.Sc.hcNo ratings yet
- Migraines: Migraine Treatment and Prevention Options: The most important information you need to improve your healthFrom EverandMigraines: Migraine Treatment and Prevention Options: The most important information you need to improve your healthNo ratings yet
- The Ultimate Headache Free Migraine: A comprehensive 30 Day Migraine Cure PlanFrom EverandThe Ultimate Headache Free Migraine: A comprehensive 30 Day Migraine Cure PlanNo ratings yet
- Keto Migraine: A Beginner's Quick Start Guide for Women on Managing Migraines Through the Ketogenic Diet, With Sample Curated RecipesFrom EverandKeto Migraine: A Beginner's Quick Start Guide for Women on Managing Migraines Through the Ketogenic Diet, With Sample Curated RecipesNo ratings yet
- How To Deal With Depression: A Practical Step by Step Non-Clinical Approach To Managing And Overcoming DepressionFrom EverandHow To Deal With Depression: A Practical Step by Step Non-Clinical Approach To Managing And Overcoming DepressionNo ratings yet
- Business Ethics N CSR PDFDocument8 pagesBusiness Ethics N CSR PDFsibusaavi0% (1)
- Mitch CVDocument3 pagesMitch CVmitchellisimoNo ratings yet
- Group 5 Cultural Adaptation and Cultural CompetenceDocument15 pagesGroup 5 Cultural Adaptation and Cultural CompetenceJoshua ArollanNo ratings yet
- Implementation of Cocoa Expert System NewDocument8 pagesImplementation of Cocoa Expert System NewNofri Ferdiansyah SoritonNo ratings yet
- Research Paper: Coaching and Counseling - What Can We Learn From Each Other?Document11 pagesResearch Paper: Coaching and Counseling - What Can We Learn From Each Other?International Coach AcademyNo ratings yet
- Operational ControlDocument14 pagesOperational ControlKirat Brar100% (1)
- Buchanan, J.M. 1959. Positive Economics, Welfare Economics, and Political Economy.Document16 pagesBuchanan, J.M. 1959. Positive Economics, Welfare Economics, and Political Economy.Ken100% (1)
- Literature Review 5Document4 pagesLiterature Review 5api-463653994No ratings yet
- 18 Analysis of Virginia Woolfs Essay Modern FictionDocument4 pages18 Analysis of Virginia Woolfs Essay Modern FictionAbhishek M N83% (6)
- Life Stars On EarthDocument6 pagesLife Stars On EarthFrancez Anne GuanzonNo ratings yet
- Per - Devt. Reader SHS v.1Document143 pagesPer - Devt. Reader SHS v.1Rette CayudacNo ratings yet
- Lesson PlanDocument12 pagesLesson PlanVikneswaran Gunahlan NeshNo ratings yet
- Learning Curve Test BankDocument8 pagesLearning Curve Test BankBehbehlynn100% (1)
- Devils DenDocument3 pagesDevils DenMisti Walker100% (1)
- DLL Aug. 22 26 2022 1st Week of ClassesDocument5 pagesDLL Aug. 22 26 2022 1st Week of ClassesHarline AbanNo ratings yet
- CREC's Advanced Alternate Route To Certification: Special Education Cross EndorsementDocument5 pagesCREC's Advanced Alternate Route To Certification: Special Education Cross EndorsementTom SullivanNo ratings yet
- 3 - Grade 6 - New Ontario Math Curriculum 2020 - DataDocument9 pages3 - Grade 6 - New Ontario Math Curriculum 2020 - DataJayjoNo ratings yet
- Black Swan Theory - WikipediaDocument5 pagesBlack Swan Theory - Wikipediamonika ramosNo ratings yet
- Skiming - EnglishDocument3 pagesSkiming - EnglishMohaiminur ArponNo ratings yet
- Default Mode Network Dark-Energy@0Document6 pagesDefault Mode Network Dark-Energy@0zhigpNo ratings yet
- Cot-Rpms Observation Notes FormsDocument4 pagesCot-Rpms Observation Notes FormsSteve MaiwatNo ratings yet
- Health Education CourseDocument2 pagesHealth Education CourseAmiel Francisco Reyes100% (2)
- PACMADDocument6 pagesPACMADMahmudul_Islam_du100% (1)
- 3 Domains of LearningDocument6 pages3 Domains of LearningCarlz BrianNo ratings yet
- Nadia Lesson Plan Day 2Document2 pagesNadia Lesson Plan Day 2api-305524125No ratings yet
- The Entry Level Nursing Competencies and The Gaps Between Nursing Education and PracticeDocument6 pagesThe Entry Level Nursing Competencies and The Gaps Between Nursing Education and PracticeIJARP PublicationsNo ratings yet
- Employee MotificationDocument66 pagesEmployee MotificationGokul KrishnanNo ratings yet