Professional Documents
Culture Documents
7284007
7284007
Uploaded by
kitsilcCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
7284007
7284007
Uploaded by
kitsilcCopyright:
Available Formats
Maternal and Child Health Nursing
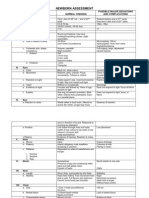
Newborn Assessment
MATERNAL and CHILD HEALTH NURSING
NEWBORN ASSESSMENT
Lecturer: Mark Fredderick R. Abejo RN, MAN
______________________________________________________________________
Newborn Assessment
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
Newborn Assessment and Nursing Care
Temperature - range 36.5 to 37 axillary
Common variations
o Crying may elevate temperature
Stabilizes in 8 to 10 hours after
delivery
o Temperature is not reliable indicator
of infection
A temperature less than 36.5
Temp: rectal- newborn to rule out imperforate
Anus
- take it once only, 1 inch insertion
Imperforate anus
1. atretic no anal opening
2. agenetialism no genital
3. stenos has opening
4. membranous has opening
Earliest sign:
1. no mecomium
2. abd destention
3. foul odor breath
4. vomitous of fecal matter
5. can aspirate resp problem
Mgt: Surgery with temporary colostomy
Heart Rate
range 120 to 160 beats per minute
Common variations
Heart rate range to 100 when sleeping
to 180 when crying
Color pink with acrocyanosis
Heart rate may be irregular with
crying
Although murmurs may be due to
transitional circulation-all murmurs
should be followed-up and referred for
medical evaluation
Deviation from range
Faint sound
Cardiac rate: 120 160 bpm newborn
Apical pulse left lower nipple
Radial pulse normally absent. If present PDA
Femoral pulse normal present. If absent COA
Respiration
- range 30 to 60 breaths per minute
Common variations
Bilateral bronchial breath sounds
Moist breath sounds may be present
shortly after birth
Signs of potential distress or deviations
from expected findings
Asymmetrical chest movements
Apnea >15 seconds
Diminished breath sounds
Seesaw respirations
Grunting
Nasal flaring
Retractions
Deep sighing
Newborn Assessment
Tachypnea - respirations > 60
Persistent irregular breathing
Excessive mucus
Persistant fine crackles
Stridor
Breathing ( ventilating the lungs)
check for breathlessness
if breathless, give 2 breathsambu bag
1 yr old- mouth to mouth, pinch nose
< 1 yr mouth to nose
force different between baby &
child
infant puff
Circulation
Check for pulslessness :carotidadult
Brachial infants
CPR breathless/pulseless
Compression inf 1 finger breath
below nipple line or 2 finger breaths
or thumb
CPR inf 1:5
Adults 2:30
Blood Pressure - not done routinely
Factors to consider
Varies with change in activity level
Appropriate cuff size important for accurate
reading
65/41 mmHg
General Measurements
Head circumference - 33 to 35 cm
Expected findings
Head should be 2 to 3 cms larger than the
chest
Abdominal circumference 31-33 cm
Weight range - 2500 - 4000 gms (5 lbs. 8oz.
- 8 lbs. 13 oz.)
Length range - 46 to 54 cms (19 - 21 inches)
Normal length- 19.5 21 inch or 47.5
53.75cm, average 50 cm
Head circumference 33- 35 cm or 13 14
Hydrocephalus - >14
Chest 31 33 cm or 12 13
Abd 31 33 cm or 12 13
Signs of increased ICP
1. abnormally large head
2. bulging and tense fontanel
3. increase BP and widening pulse pressure
4. Decreased RR, decreased PR
5. projective vomiting- sure sign of cerebral
irritation
6. high deviation diplopia sign of ICP older
child
a. 4-6 months- normal eye deviation
b. >6 months- lazy eyes
7. High pitch shrill cry-late sign of ICP
Abejo
Maternal and Child Health Nursing
Newborn Assessment
Head to Toe Newborn Assessment
CIRCULATORY
STATUS
UMBILICAL VEIN and DUCTUS VENOSUS constrict after cord id clamped
DUCTUS ARTERIOSUS constrict with establishment of respiratory function
FORAMEN OVALE closes functionally as respirations established, but anatomic or
permanent closure may take several months
HEART RATE averages 140 b.p.m.
BP 73/55 mmHg
PERIPHERAL CIRCULATION acrocyanosis within 24 hours
RBC high immediately after birth; falls after 1 st week
ABSENCE/ NORMAL FLORA INTESTINE Vitamin K
RESPIRATORY
STATUS
Adequate levels of surfactants (Lecithin and spingomyelin) ensure mature lung
function; prevent alveolar collapse and respiratory distress syndrome
RR = 30-80 breaths /minutes with short periods of apnea (< 15 seconds) = assess for
1 full minute change noted during sleep or activity
NOTE: Periodic apnea is common in preterm infants. Usually, gentle stimulation is
sufficient to get the infant to breathe
RENAL SYSTEM
Urine present in the bladder at birth but NB may not void doe 1st 12-24 hours
Later pattern is 6-10 voidings/ day indicative of sufficient fluid intake
Urine is pale and straw colored initial voidings may leave brick-red spots on
diaper ( d/t passage of uric acid crystals in urine)
Infant unable to concentrate urine for the 1st 3 months
DIGESTIVE
SYSTEM
IMMATURE CARDIAC SPHINCTER may allow reflux of food, burped,
REGURGITATE- placed NB right side after feeding
Newborn cant move food from lips to pharynx. Insert nipple well to mouth
FEEDING PATTERS vary
- Newborns may nurse vigorously immediately afterbirth or may need as long as
several days to suck effectively
- Provide support and encouragement to new mothers during this time as infant
feeding is very emotional doe most mothers
NOTE: Distinguishing Neonatal Vomiting from Regurgitation
Vomiting is usually sour, looks like curdled milk due to HCL, with a sour odor, while
regurgitation has no sour odor or curdling of milk, or occurs during or immediately
after feeding.
IMPORTANT CONSIDERATIONS:
Breastfeeding can usually begin immediately after birth; bottle-fed newborns
may be offered few milliliters of sterile water or 5% dextrose 1 to 4 hours after
birth prior to a feeding with formula
An infant with gastrostomy tube should receive a pacifier during feeding
unless contraindicated to provide normal sucking activity and satisfy oral
needs.
At age4-6 months, an infant should begin to receive solid food foods one at a
time and 1 week apart.
FIRST STOOL is MECONIUM
- Black, tarry residue from lower intestine
- Usually passed within 12-24 hours after birth
If the amniotic fluid shows evidence of meconium staining, the physician most likely do
immediately after delivery is to suction the oropharynx immediately after the head is
delivered and before the chest is delivered.
TRANSITIONAL STOOLS thin, brownish green in color
After 3 days MILK STOOLS are usually passed
a. MILK STOOLS for BF infant loose and golden yellow
b. MILK STOOLS for FORMULATED FED- formed and pale yellow
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
HEPATIC
TEMPERATURE
Liver responsible for changing Hgb into conjugated bilirubin, which is further
changed into conjugated (water soluble) bilirubin that can be excreted
Excess unconjugated bilirubin can permeate the sclera and the skin, giving a jaundiced
or yellow appearance to these tissues
HEAT PRODUCTION in newborn accomplished by:
a. Metabolism of BROWN FAT
- A special structure in NB is a source of heat
- Increased metabolic rate and activity
Axillary temperature: 96.8 to 99F
Newborn cant shiver as an adult does to release heat
Newborns are unable to maintain a stable body temperature because they have an
immature vasomotor center, and unable to shiver to increase body heat.
NBs body temperature drops quickly after birth after stress occurs easily
Body stabilizes temperature in 8-10 hours if unstressed
Cold stress increases o2 consumption may lead to metabolic acidosis and
respiratory distress
IMMUNOLOGIC
NB develops own antibodies during 1st 3 months but at risk for infection during the
first 6 weeks
Ability to develop antibodies develops sequentially
Neonatal Physical Assessment
Birth weight=2500-400 grams (5 lbs. 8oz. 8 lbs. 13 oz.)
Length= 45.7 55.9 cm. (18-22 inches)
HEAD
Head circumference = 33-35 cm (2-3 cm. Greater than chest circumference)
Anterior fontanel (diamond shape) = closes 12-18 months
Posterior fontanel (triangle shape)= closes 2-3 months
NOTE: The posterior fontanel is located at the intersection of the sagittal and
lambdoid suture is the space between the pariental bones; the lambdoid suture
separates the two parietal bones and the occipital bone
Molding- asymmetry of head as a result of pressure in birth cana
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
EYES
Blue/ gray d/t scleral thinness; permanent color established w/in 3-12 mos.
Lacrimal glands immature at birth; tearless cry up to 2 months
Absence of tears is common because the neonates tear glands are not yet fully
developed
Transient strabismus
Dolls eye reflex persist for about ten days
Red Reflex: A red circle on the pupils seen when an ophthalmoscopes light is shining
onto the retina is a normal finding. This indicates that the light is shining onto the
retina.
CONVERGENT STRABISMUS (CROSS EYED)
It is common during infancy until age 6 months because of poor oculomotor
coordination
NOTE : Congenital Glaucoma
It is due to increased intraocular pressure caused by an abnormal outflow or
manufacturing of normal eye fluid.
Unequal size should be reported immediately.
NOSE
MOUTH
Nose breathers for first few months of life
Scant saliva with pink lips
Epsteins Pearls - small shiny white specks on the neonates gums and hard palate
which are normal
EARS
Incurving of pinna and cartilage deposition
NECK
Short and weak with deep fold of skin
CHEST
Characterized by cylindrical thorax and flexible ribs
NOTE:
appears circular since anteroposterior and lateral diameters are about equal
Respirations appear diaphragmatic
Nipples prominent and often edematous
Milky secretion (witch's milk) common ( effect of estrogen)
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
ABDOMEN
Cylindrical with some protrusion; scaphoid appearance indicates diaphragmatic hernia
Umbilical cord is white and gelatinous with two arteries and one vein and begins to dry
within 1-2 hours after delivery
NOTE: Umbilical cord
Three vessels, two arteries and one vein, in cord; if fewer than three vessels
are noted notify the physician
Small, thin cord may be associated with poor fetal growth
Assess for intact cord, and ensure that damp is cured
Cord should be clamped for at least the first 4 hours after birth; clamp can
be removed hen the cord is dried and occluded
Umbilical clamp can be removed after 24 hours
GENITALIA
MALE: includes rugae on the scrotum and testes descended into the scrotum
Urinary meatus:
Hypospadias (ventral surface)
Epispadias (dorsal surface)
NOTE:
Meatus at tip of penis
Testes descended but may retract with cold
Assess for hernia or hydrocele
First voiding should occur within 24 hours
FEMALE: labia majora cover labia minora and clitoris
Pseudomenstruation possible (blood-tinged mucus) effect of estrogen
First voiding should occur within 24 hours
EXTREMITIES
All neonates have bowlegged and flat feet
NOTE NORMAL FEATURES:
Major gluteal folds even
Creases on soles of feet
Assess for fractures (especially clavicle) or dislocations (hip)
Assess for hip dysplasia; when thighs are rotated outward, no clicks should be
heard
Some neonates may have abnormal extremities:
Polydactyl (more than 5 digits on extremity)
Syndactyl (two or more digits fused together)
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
Polydactyl
Syndactyl
SPINE
Should be straight and flat
Anus should be patent without any fissure
Dimpling at the base is associated with spina bifida
A degree of hypotonicity or hypertonicity is indicative of central nervous system (CNS
damage)
SKIN
Assessment for Jaundice
The #1 technique is to blanch the skin over the bony prominence such as the
forehead, chest or tip of the nose.
NOTE: Jaundice starts at the head first, spreads to the chest, then the abdomen, then the
arms and legs, followed by the hands and feet, which are the last to be jaundiced.
Jaundice in the first 24 hours after the birth is a cause for concern that requires
further assessment. Possible causes of early jaundice are blood incompatibility,
oxytocin induction, and severe hemolytic process.
Mongolian Spots
Gary, blue or black marks that are frequently found on the sacral area, buttocks, arms
shoulders or other areas.
Harlequins Sign
Occurs on one side of the body turns deep red color. It occurs when blood vessels on
one side constrict, while those on the other side of the body dilate.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
Erythema toxicum
Is an eruption of lesions in the area surrounding a hair follicle that are firm, vary
in size from 1-3 mm, and consist of a white or pale yellow papule or pustule w/ an
erythematous base.
It is often called newborn rash or flea-bite dermatitis
The rash may appear suddenly, usually over the trunk and diaper area and is
frequently widespread.
The lesions do not appear on the palms of the hands or soles of the feet.
The peak incidence is 24-48 hours of life.
Cause is unknown and no treatment necessary
Acrocyanosis versus Central Cyanosis
Acrocyanosis involves the extremities of the neonate, for example bluish hands
and feet due to neonates being cold or poor perfusion of the blood to the
periphery of the body.
Central cyanosis, which involves the lips, tongue and trunk indicating
HYPOXIA which needs further assessment by the nurse.
.
Milia are blocked sebaceous glands located on the chin and the nose of the infant.
VERNIX CASEOASA
Should not be removed by oil or hand lotion, because it is a protective layer of the
neonate after birth, and it disappears after birth. Never remove it with alcohol or
cotton balls, unless meconium skinned.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
BIRTH MARKS
Telangiectatic nevi (stork bites)
Appear as pale pink or red spots and are frequently found on the eyelids, nose,
lower occipital bone and nape of the neck
These lesions are common in NB w/ light complexions and are more noticeable
during periods of crying. These areas have no clinical significance and usually
fade by the 2nd birthday
Hemangioma is benign vascular tumor that may be present on the newborn
3 types Hemangiomas
1. Nevus Flammeus port wine stain macular purple or dark red lesions seen
on face or thigh. NEVER disappear. Can be removed surgically
2. Strawberry hemangiomas nevus vasculosus dilated capillaries in the
entire dermal or subdermal area. Enlarges, disappears at 10 yo.
3. Cavernous hemangiomas communication network of venules in SQ tissue
that never disappear with age.
Nevus Flammeus (port-wine stain)
A capillary angioma directly below the epidermis, is a non-elevated, sharply
demarcated, red-to-purple area of dense capillaries.
Macular purple
The size & shape vary, but it commonly appears on the face. It does not grow in
size, does not fade in time and does not blanch. The birthmark maybe concealed by
using an opaque cosmetic cream.
If convulsions and other neurologic problem accompany the nevus flammeus,---5th cranial nerve involvement.
Nevus vasculosus (strawberry mark)
A capillary hemangioma, consists of newly formed and enlarged capillaries in the
dermal and subdermal layers.
It is a raised,clearly delineated, dark-red, rough-surfaced birthmark commonly
found in the head region.
Such marks usually grow starting the second or third week of life and may not
reach their fullest size for 1 to 3 months; disappears at the age of 1 yr. but as the
baby grows it enlarges.
Providing appropriate information about the cause and course of birthmarks often
relieves the fears and anxieties of the family. Note any bruises, abrasions,or
birthmarks seen on admission to the nursery.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
GESTATIONAL ASSESSMENT
PARAMETER
BREAST TISSUE
FEMALE GENITALIA
NURSING
ACTION
Fold the pinna
(auricle) forward
Measure it
Observe
MALE GENITALIA
Observe
HEEL CREASES
Observe
EAR
TERM born between
37-42 weeks gestation
Pinna recoils (springs
back)
3 mm
Labia majora cover
labia minora
Scrotal sac very
wrinkled
Extend 2/3 of the way
from the toes to the heel
PRETERM born before 37 weeks
gestation
Pinna opens slowly or stays folded
in very premature infants
Less than 3 mm
Labia minora are more prominent;
vaginal opening can be seen
Fewer shallow rugae on the scrotum
Soles are smoother, creases extend
less than 2/3 of the way from the
toes to the heel
NEWBORN REFLEXES
Immature central nervous system (CNS) of newborn is characterized by variety of reflexes
o Some reflexes are protective, some aid in feeding, others stimulate interaction
o Assess for CNS integration
Protective reflexes are blinking, yawning, coughing, sneezing, drawing back from pain
Rooting and sucking reflexes assist with feeding
What reflexes should be present in a newborn? Reflexes are involuntary movements or actions. Some movements
are spontaneous, occurring as part of the baby's usual activity. Others are responses to certain actions. Reflexes
help identify normal brain and nerve activity. Some reflexes occur only in specific periods of development. The
following are some of the normal reflexes seen in newborn babies
PALMAR GRASP
REFLEX
ROOTING
REFLEX
SUCKING
REFLEX
Newborn Assessment
Newborns fingers curl around the examiners fingers and the newborns toes
curl downward.
The palmar grasp reflex is elicited by placing an object in the palm of a
neonate; the neonate's fingers close around it. This reflex disappears between
ages 6 and 9 months.
Palmar response lessens within 3-4 months
Palmar response lessens within 8 months
The rooting reflex is elicited by stroking the neonate's cheek or stroking near
the corner of the neonate's mouth.
The neonate turns the head in the direction of the stroking, looking for food.
This reflex disappears by 6 weeks.
The sucking reflex is seen when the neonate's lips are touched
Lasts for about 6 months
Abejo
Maternal and Child Health Nursing
Newborn Assessment
MORO REFLEX
Symmetric & bilateral abduction & extension of arms and hands
Thumb & forefinger form a C
EMBRACE reflex
Present at birth, complete response may occur up to 8 weeks
A persistent response lasting more than 6 months may indicate the occurrence
of brain damage during pregnancy
A normal reflex in a young infant caused by a sudden loud noise. It results in drawing
up the legs, an embracing position of the arms, and usually a short cry.
BABINSKI SIGN
Beginning at the heel of the foot, gently stroke upward along the lateral aspect of
the sole; then the examiner moves the fingers along the ball of the foot
The newborns toes hyperextend while the big toe dorsiflexes
Absence of this reflex indicates the need for a neurological examination
The Babinski reflex is elicited by stroking the neonate's foot, on the side of the
sole, from the heel toward the toes.
A neonate will fan his toes, producing a positive Babinski sign, until about age 3
months
STEPPING OR
WALKING
REFLEX
The newborn simulates walking, alternately flexing and extending the feet
The reflex is usually present 3-4 months
TONIC NECK
REFLEX
While the newborn is falling asleep or sleeping, gently and quickly turn the head
to one side
As the newborn faces the left side, the left arm & leg extend outward while the
right arm & leg flex
When the head is turned to the right side, the right arm & leg extend outward while
the left arm & leg flex
Usually disappears within 3-4 months
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
CRAWLING
Place the newborn on the abdomen
The newborn begins making crawling movements with the arms and legs
The reflex usually disappears after about 6 weeks
BASIC TEACHING NEEDS OF NEW PARENTS
CORD CARE
Cleanse the cord with alcohol and sometimes triple dye once a day
Keep the area clean and dry
Keep the newborns diaper below the cord to prevent irritation
Signs of infection: redness, drainage, swelling, odor
Notify physician for signs of infection
NOTE:
Note any bleeding or drainage from the cord
Triple dye may be applied for initial cord care because it minimizes
microorganisms and promotes drying; use a cotton-tipped applicator to paint
the dye, one time, on the cord on 1 inch of surrounding skin
Application of 70% isopropyl alcohol to the cord with each diaper change and
at least two r three times a day to minimize microorganisms and promote
drying.
NOTE: The skin is surrounded with alcohol which promotes drying and cleans the area.
The umbilical cord dries and falls off about 14 days. Peroxide and lanolin promote
moisture, which can inhibit drying and allow growth of bacteria. Water doesnt
promote drying.
It is best to care for the neonates umbilical cord area by cleaning it with cotton
pledgets moistened with alcohol. The alcohol promotes drying and helps decrease the
risk of infection. An antibiotic ointment maybe used instead of alcohol, because there
are a lot of bacteria which is resistant against some bacteria. Other agents such as
wipes, sterile water and soap & water are not as effective as alcohol.
CIRCUMCISION
CARE
BONDING
Observe for bleeding, first urination
Apply diaper loosely to prevent irritation
Notify physician for signs of infection
Encourage parent to talk to, hold, and sing to infant
Promotes skin-to-skin contact between parent and infant
Feedings are opportunities for parent-infant bonding
Notify physician for signs of infection
NOTE: Sense of Touch
The most highly developed sense at birth that is why, neonates responds well to
touch.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
PRE TERM INFANT ( PREMATURE INFANT)
Definition
PRE TERM INFANT
A neonate born before 38 weeks age of gestation
Synonym
Low birth weight
Contributing factors
Cardinal signs
Low socioeconomic level
Poor nutritional status
Lack of pre natal care
Multiple pregnancy
Prior previous early birth
Race (non whites have a higher incidence of prematurity than
whites)
Cigarette smoking
The age of the mother ( the highest incidence is in mothers
younger than age 20.)
Order of birth ( early termination is highest in first pregnancies
and in those beyond the forth )
Closely spaced pregnancies
Abnormalities of the reproductive system such as intrauterine
septum
Infections ( specially urinary tract infections)
Obstetric complications such as premature rupture of membranes
or premature separation of the placenta
Early induction of labor
Elective cesarian birth
Appears small and underdeveloped
The head is disproportionately large ( 3 cm or more greater than
chest size)
Skin is thin with visible blood vessel and minimal subcutaneous
fat pads
Vernix caseosa is absent
Both anterior and posterior fontanelles are small
Abnormal laboratory values
Decreased RBCs
Decreased serum glucose
Increased concentration of indirect bilirubin
Decreased serum albumin
NOTE:
The normal range of urine output for a preterm
baby is 1 to 2ml/kg/day. The normal specific gravity for a
preterm baby is 1.020. The normal range for blood glucose
level in a preterm baby is 40 to 60 mg/dl.
Best procedure
Resuscitation
NOTE: resuscitation becomes important for infant who fails to
take first breath or difficulty maintaining adequate
respiratory movements on his own.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
Best position
Suctioning
NOTE: allows removing mucus and prevents aspiration of any
mucus and amniotic fluid present in the mouth and
nose of the newborn to establish clear airway.
Intubations
NOTE: head of the infant in neutral position with towel under
shoulder.
Positioning the infant on the back with the head of the mattress
elevated approximately 15 degrees to allow abdominal contents to
fall away from the diaphragm affording optimal breathing space.
Best position for suctioning:
Infant on the back and slide a folded towel or pad under shoulders
to rise, head is in neutral position.
Anemia of prematurity
Hyperbilirubinemia/ kernicterus
Persistent patent ductus arteriosus
Periventricular / intraventricular hemorrhage
Respiratory distress syndrome
Retinopathy of prematurity
Retrolental fibroplasias are a complication that occurs if the
infant is overexposed to high oxygen levels.
Necrotizing enterocolitis
Bedside equipment
Preterm size laryngoscope
ET tube
Suction catheter with synthetic surfactant
Isolettes (incubator)
Drug study
1.
Naloxone (Narcan)
Nature of the drug:
Narcotic antagonist
Side effects:
Hypertension, irritability, tachycardia
2.
Surfactan ( Survanta)
Nature of the drug:
Lung surfactant to improve lung compliance
Side effect:
Transient bradycardia, rales
3.
Vitamin K (Aquamephyton)
Use for prophylaxis to treat hemorrhagic disease of the
newborn.
Side effects:
Hyperbilirubinuria
4.
Eye prophylaxis
(Erythromycin 0.5% Ilotycin, Tetracycline 1%
Silver Nitrate 1% ( not already used causes chemical
conjunctivitis)
Prophylactic measure to protect against Neisseria
gonorrhoeae and Chlamydia trachomatis
Side effects:
Silver nitrate can cause chemical conjuctivitis
Complications
Nursing diagnosis
1.
2.
Newborn Assessment
Impaired gas exchange related to immature pulmonary
functioning
Risk for fluid volume deficit related to insensible water loss at
birth and small stomach capacity
Abejo
Maternal and Child Health Nursing
Newborn Assessment
3.
4.
5.
6.
Nursing intervention
Newborn Assessment
Risk for aspiration related to weak or absent gag reflex a nd/or
administration of tube feedings
Hypothermia related to lack of subcutaneous and brown fat
deposits, inadequate shiver response, immature
thermoregulation center, large body surface area in relation to
body weight, and/or lack of flexion of extremities toward the
body.
Risk for infection related to immature immune response, stasis of
respiratory secretions, and/ or aspiration
Imbalanced nutrition: less than body requirements related to
lack of energy to suck and/or weak or absent sucking reflex
The nurses first priority in preparing a safe environment for a
preterm newborn with low Apgar scores is to prepare
respiratory resuscitation equipment. Airway maintenance is the
first priority.
Give the mother oxygen by mask during the birth to provide the
preterm infant with optimal oxygen saturation at birth ( 85-90%).
Keeping maternal analgesia and anesthesia to a minimum also
offers the infant the best chance of initiating effective respiration.
Bedside larngyoscope, endotracheal tube, suction catethers and
synthetic surfactant to be administered by the endotracheal tube.
Infant must be kept warm during resuscitation procedures so he
or she is not expending extra energy to increase the metabolic
rate to maintain body temperature.
Observe for changes in respirations, color and vital signs
Check efficacy of Isolette: maintain heat, humidity and oxygen
concentration, administer oxygen only if necessary
Maintain aseptic technique to prevent infection
Adhere to the techniques of gavage feeding for safety of infant
Observe weight-gain patterns
Determine blood gases frequently to prevent acidosis. Institute
phototherapy when hyperbilirubinemia occurs
Support parents by letting them verbalize and ask questions to
relieve anxiety.
Provide liberal visiting hours for parents, allow them to
participate in care.
Arrange follow-up before and after discharge by a visiting nurse.
Abejo
Maternal and Child Health Nursing
Newborn Assessment
POST TERM INFANT
POST TERM INFANT
A neonate born after 42 weeks age of gestation
Definition
Contributing factors
Classic signs
Intrauterine weight loss, dehydrations and chronic hypoxia old
man faces
Long & thin with cracked skin which is loose, wrinkled and
strained greenish yellow, with no vernix nor lanugo
Long nails with firm skull
Wide eyed alertness of one month old baby
Increased total no. of RBCs
Increased hematocrit level
Decreased serum glucose
Sonogram
Resuscitation
NOTE: resuscitation becomes important for infant who fails to take
first breath or difficulty maintaining adequate respiratory
movements on his own.
Suctioning
NOTE: allows removing mucus and prevents aspiration of any
mucus and amniotic fluid present in the mouth and nose of the
newborn.
To establish clear airway.
Intubations
NOTE: head of the infant in neutral position with towel under
shoulder.
Positioning the infant on the back with the head of the mattress
elevated approximately 15 degrees to allow abdominal contents
Meconium aspiration syndrome
Respiratory distress syndrome
Abnormal
values
laboratory
Screening test
Best procedure
Best position
Complications
Low socioeconomic level
Poor nutritional status
Lack of pre natal care
Multiparous mothers
Cigarette smoking
The age of the mother (the highest incidence is in mothers younger
than age 20.)
Mothers with diabetes mellitus
Congenital abnormalities such as omphalocele.
Body is covered with lanugo
Old man facies
NOTE: Post mature neonates have difficulty maintaining glucose
reserves. Other common problems include Meconium aspiration
syndrome, polycythemia, congenital anomalies, seizure activity and cold
stress.
NOTE: The infant who are exposed to high blood-glucose levels in
utero may experience rapid and profound hypoglycemia after birth
because of the cessation of a high in-utero glucose load. The small-forgestational-age infant has use up glycogen stores as a result of
intrauterine malnutrition and has blunted hepatic enzymatic response
with which to carry out gluconeogenesis.
Newborn Assessment
Abejo
Maternal and Child Health Nursing
Newborn Assessment
NOTE: The patient with post-term pregnancy is at high risk for
decreased placental functioning, therefore increasing the risk of
inadequate oxygen circulation to the fetus
Bedside equipment
ET tube
Suction catheter
Drug study
1. Vitamin K (Aquamephyton)
Use for prophylaxis to treat hemorrhagic disease of the newborn
Side effects:
Hyperbilirubinuria
2. Eye prophylaxis
(Erythromycin 0.5% Ilotycin, Tetracycline 1% Silver Nitrate 1%
Prophylactic measure to protect against Neisseria gonorrhoeae and
Chlamydia trachomatis
Side effects:
Silver nitrate can cause chemical conjuctivitis
Nursing diagnoses
Nursing interventions
1. Ineffective airway breathing
2. Risk for fluid volume deficit related to insensible water loss at birth
3. Ineffective infant feeding pattern
Assess newborns respiratory rate, depth and rhythm. Auscultate
lung sound.
Note: Meconium stained syndrome of POST MATURE neonates
Aspiration of meconium is best prevented by suctioning the neonates
nasopharynx immediatelt after the head is delivered and before the
shoulders and chest are delivered. As long as the chest is
compressed in the vagina, the infant will not inhale and aspirate
meconium in the upper respiratory tract. Meconium aspiration
blocks the air flow to the alveoli, leading to potentially life
threatening respiratory complications.
Suction every 2 hours or more often as necessary
Position newborn on side or back with the neck slightly extended
Administer O2, anticipate the need for CPAP or PEEP
Continue to assess the newborns respiratory status closely.
Encourage as much parental participation in the newborns care as
condition allows
Administer IV fluids after birth to provide Glucose to prevent
hypoglycemia, monitor closely the infusion rate.
Kept the infant under a radiant heat warmer to preserve energy
Monitor babys weight, serum electrolytes and ensure adequate
fluid intake
Measure urine output by weighing diapers
Check for blood stools to evaluate for possible bleeding from
intestinal tract.
Keep a restful environment.
Anticipate the infants need to be breastfeed
Demonstrate technique for feeding to mother, note proper
positioning of the infant, latching on technique, rate of delivery
of feeding and frequency of burping
Provide a relaxed environment during feeding
Adjust frequency and amount of feeding according to infants
response
Alternate feeding procedure (nipple and gavage feeding) according
to infants ability.
Monitor mothers effort, provide feedback and assistance as needed
Suggest mother to monitor infants weight periodically
Newborn Assessment
Abejo
You might also like
- Inpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)From EverandInpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)No ratings yet
- Maternity Study GuideDocument43 pagesMaternity Study Guidepgmanski100% (23)
- How Many Phases Are in The Cell Cycle As Shown in The Diagram in Model 1?Document3 pagesHow Many Phases Are in The Cell Cycle As Shown in The Diagram in Model 1?Nick Andrew bohol100% (1)
- STI Chart (Maternity-Nursing)Document4 pagesSTI Chart (Maternity-Nursing)brittney bradyNo ratings yet
- Labor and Delivery Nursing Knowledge & Skills ChecklistDocument4 pagesLabor and Delivery Nursing Knowledge & Skills Checklistnorthweststaffing100% (4)
- Maternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideFrom EverandMaternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideNo ratings yet
- Pedia Nicu NotesDocument32 pagesPedia Nicu NotesChristian Noel Fernandez100% (2)
- Newborn AssessmentDocument7 pagesNewborn Assessmentapi-232728488No ratings yet
- Newborn AssessmentDocument7 pagesNewborn AssessmentMJ Amarillo100% (6)
- Newborn AssessmentDocument3 pagesNewborn AssessmentValerie Ybañez Peñalber100% (2)
- Nicu Must KnowsDocument7 pagesNicu Must KnowsCyfern100% (2)
- Nursing OB Exam Q & ADocument173 pagesNursing OB Exam Q & Ajoerobinson8889323100% (8)
- Pediatric NursingDocument97 pagesPediatric NursingFreeNursingNotes100% (1)
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)From EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)No ratings yet
- Newborn AssessmentDocument15 pagesNewborn Assessmentmarie97% (35)
- Physical Assessment of NewbornDocument39 pagesPhysical Assessment of Newbornwewix100% (3)
- Partogram or PartographDocument5 pagesPartogram or PartographCharo Flores100% (1)
- Peds Mastery Review 2Document55 pagesPeds Mastery Review 2Gabriela Lomeli100% (3)
- Pediatric NursingDocument55 pagesPediatric Nursingbajaoc100% (14)
- LOW RISK NEONATAL NURSING: Passbooks Study GuideFrom EverandLOW RISK NEONATAL NURSING: Passbooks Study GuideNo ratings yet
- Harrisons Neurology in Clinical Medicine, 3E PDFDocument896 pagesHarrisons Neurology in Clinical Medicine, 3E PDFFelly Liu100% (8)
- Biodatas 601-700Document17 pagesBiodatas 601-700Nishant ChandraNo ratings yet
- Immediate Newborn CareDocument9 pagesImmediate Newborn CareLj FerolinoNo ratings yet
- Assessment of The Normal NewbornDocument6 pagesAssessment of The Normal Newborndhalal100% (2)
- Basic Newborn ResuscitationDocument27 pagesBasic Newborn ResuscitationAnusha Verghese100% (1)
- Maternal and Child Health Nursing Care of The NewbornDocument5 pagesMaternal and Child Health Nursing Care of The NewbornJeanilynTanNo ratings yet
- Newborn AssessmentDocument24 pagesNewborn Assessmentvincentsharon100% (2)
- Newborn Assessment ToolDocument5 pagesNewborn Assessment ToolReana AbillarNo ratings yet
- Normal NewbornDocument30 pagesNormal NewbornLekshmi Manu100% (3)
- Newborn AssessmentDocument8 pagesNewborn Assessmentapi-283260051No ratings yet
- Common Neonatal DisordersDocument70 pagesCommon Neonatal DisordersKiran Khasa100% (4)
- Pediatrics Study GuideDocument22 pagesPediatrics Study GuideElizabeth McKee100% (1)
- High Risk NewbornDocument19 pagesHigh Risk Newbornsantosh s u100% (1)
- Care of The Newborn PDFDocument5 pagesCare of The Newborn PDFzhai bambalan100% (2)
- Labor and DeliveryDocument7 pagesLabor and Deliveryplethoraldork100% (20)
- Assessment of NewbornDocument33 pagesAssessment of Newbornmehta shivaniNo ratings yet
- Introduction To Modern Concept of Childcare & History, Principles & Scope of Child Health NursingDocument17 pagesIntroduction To Modern Concept of Childcare & History, Principles & Scope of Child Health Nursingsuper cool100% (2)
- High Risk NeonateDocument85 pagesHigh Risk NeonateWed Lod100% (1)
- New Born CareDocument17 pagesNew Born CareHarrison Tallod100% (1)
- Neonatal NursingDocument53 pagesNeonatal Nursingkrishnasree100% (1)
- High Risk NewbornDocument20 pagesHigh Risk Newborndmrdy50% (2)
- Perinatal Manual of Southwestern OntarioDocument6 pagesPerinatal Manual of Southwestern OntarioƦя de GuzмѧN100% (1)
- Pediatric DR PDFDocument135 pagesPediatric DR PDFVinu Poojapranavam100% (1)
- OB-High Risk PregnancyDocument18 pagesOB-High Risk PregnancyBree EtienneNo ratings yet
- Routine New Born Care GNMDocument55 pagesRoutine New Born Care GNMLeena Pravil100% (3)
- Pediatric NursingDocument37 pagesPediatric Nursingjairize100% (5)
- Initial Newborn AssessmentDocument14 pagesInitial Newborn Assessmentaclark831No ratings yet
- Newborn CareDocument120 pagesNewborn Carejuly3ciaNo ratings yet
- NicuDocument46 pagesNicugoal diggers100% (1)
- Pediatric DiseasesDocument10 pagesPediatric DiseasesKira100% (4)
- Assessment and Management of High Risk NeonateDocument14 pagesAssessment and Management of High Risk NeonateSapna thakur50% (2)
- NICUDocument190 pagesNICUSoat Alfajer100% (2)
- Concept, Assessment, Goals, Objectives of High Risk NewbornDocument76 pagesConcept, Assessment, Goals, Objectives of High Risk NewbornEsha KuttiNo ratings yet
- Newborn Assessment NORMALDocument2 pagesNewborn Assessment NORMALVanessaMUellerNo ratings yet
- Newborn AssessmentDocument17 pagesNewborn Assessmentryancohen1100% (1)
- Kangaroo Mother CareDocument6 pagesKangaroo Mother CareUday KumarNo ratings yet
- Assessment and Nursing Management Normal NewbornDocument17 pagesAssessment and Nursing Management Normal NewbornVinay Kp100% (1)
- Maternity Nursing ReviewDocument54 pagesMaternity Nursing ReviewJr Robis100% (6)
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideFrom EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideNo ratings yet
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideFrom EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- Neonatal Nurse Practitioner A Complete Guide - 2020 EditionFrom EverandNeonatal Nurse Practitioner A Complete Guide - 2020 EditionNo ratings yet
- History of Herbal TritmentDocument10 pagesHistory of Herbal TritmentTorentSpyNo ratings yet
- BBC 16W Leg Rock DrillDocument132 pagesBBC 16W Leg Rock DrillMiguel Eleazar Marin ArosNo ratings yet
- Easy Health Proposal FormDocument5 pagesEasy Health Proposal Formomshanker44No ratings yet
- Temple Dental Histology Exam 2 (Dr. Fornatora)Document77 pagesTemple Dental Histology Exam 2 (Dr. Fornatora)Arianna VonaNo ratings yet
- The Cold, Hard Facts of Cryotherapy in Orthopedics and Sports MedicineDocument13 pagesThe Cold, Hard Facts of Cryotherapy in Orthopedics and Sports MedicinepnalamatiNo ratings yet
- Lab ValuesDocument4 pagesLab ValuespninthemakinNo ratings yet
- Fat MalabsorptionDocument22 pagesFat MalabsorptionanimathzNo ratings yet
- Marine PharmacognosyDocument5 pagesMarine PharmacognosyNishamolKSNo ratings yet
- Turmeric (Cucurma Longa) Leaves Extract As Anti-Fungal SoapDocument16 pagesTurmeric (Cucurma Longa) Leaves Extract As Anti-Fungal SoapAlfie JacildoNo ratings yet
- Lichen SclerosusDocument2 pagesLichen SclerosusVidini Kusuma AjiNo ratings yet
- Copy Jindal Prize For Ajay Gandhi Ji - Annexure 4 - From020-RESEARCH BY GURUJIDocument15 pagesCopy Jindal Prize For Ajay Gandhi Ji - Annexure 4 - From020-RESEARCH BY GURUJIAshley AbnesNo ratings yet
- FitnessAssessment 2015 16 PDFDocument16 pagesFitnessAssessment 2015 16 PDFlaxave8817No ratings yet
- Msds CPD Intraplast N UsDocument10 pagesMsds CPD Intraplast N UsJose David CastroNo ratings yet
- Resisting National Breast Cancer Awareness Month - The Rhetoric of Counterpublics and Their Cultural PerformancesDocument22 pagesResisting National Breast Cancer Awareness Month - The Rhetoric of Counterpublics and Their Cultural PerformancesDaniel DouglasNo ratings yet
- Dasar-Dasar Radiologi Musculoskeletal PDFDocument101 pagesDasar-Dasar Radiologi Musculoskeletal PDFIndra MahaputraNo ratings yet
- ECC - List of Compensable Diseases PDFDocument2 pagesECC - List of Compensable Diseases PDFtrina tsai100% (1)
- Alive & Well Test: Part A Grammar and VocabularyDocument6 pagesAlive & Well Test: Part A Grammar and VocabularyDarwin Talledo AyalaNo ratings yet
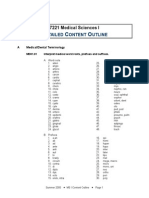
- 7221 Detailed Content OutlineDocument53 pages7221 Detailed Content Outlineapi-258892726No ratings yet
- Anoverviewofacupunctureforpsoriasisvulgaris20092014 PDFDocument10 pagesAnoverviewofacupunctureforpsoriasisvulgaris20092014 PDFRute MacedoNo ratings yet
- Biochemical and Therapeutic Properties of Withania Somnifera in Traditional Medicinal SystemDocument6 pagesBiochemical and Therapeutic Properties of Withania Somnifera in Traditional Medicinal SystemEditor IJTSRDNo ratings yet
- Cleanse and DetoxDocument14 pagesCleanse and DetoxSADDYNo ratings yet
- 02 Egfr-Her2 Vegfr InhibitorDocument19 pages02 Egfr-Her2 Vegfr Inhibitor王貞云No ratings yet
- Drug StudyDocument32 pagesDrug StudyPrincess Gutierrez RositaNo ratings yet
- Metabolic and Endocrine 2010 2 With AnswersDocument13 pagesMetabolic and Endocrine 2010 2 With AnswersWenzy Razzie cruzNo ratings yet
- Lypm Immunity SystemDocument22 pagesLypm Immunity SystemPhoenix JudgeNo ratings yet
- Endocrine Exam ReviewDocument2 pagesEndocrine Exam Reviewrockforj3susNo ratings yet
- Penis Sonography. A Pictorial Review: Poster No.: Congress: Type: AuthorsDocument35 pagesPenis Sonography. A Pictorial Review: Poster No.: Congress: Type: AuthorsOky Sutarto PutraNo ratings yet