Professional Documents
Culture Documents
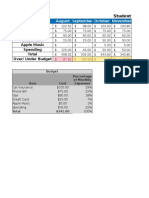
2016 Health Benefits Table
Uploaded by
Ryan YK ChiangCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2016 Health Benefits Table
Uploaded by
Ryan YK ChiangCopyright:
Available Formats
2016 Standard Benefit Designs and Medical Cost Shares
Benefits in blue are NOT subject to a deductible
Coverage Category
Minimum Coverage
Bronze
Silver
Enhanced Silver 73
Enhanced Silver 87
Enhanced Silver 94
Gold
Platinum
Percent of cost coverage
Covers 0% until
out-of-pocket
maximum is met
Covers 60% average
annual cost
Covers 70% average
annual cost
Covers 73% average
annual cost
Covers 87% average
annual cost
Covers 94% average
annual cost
Covers 80% average
annual cost
Covers 90% average
annual cost
Cost-sharing Reduction
Single Income Range
N/A
N/A
N/A
N/A
N/A
Annual Wellness Exam
$0
$0
$0
$0
$0
$0
$0
$0
Primary Care Vist
after first 3 nonpreventive visits,
pay negotiated
carrier rate per
instance until
out-of-pocket
maximum is met
$70*
$45
$40
$15
$5
$35
$20
Specialist Visit
$90*
$70
$55
$25
$8
$55
$40
Urgent Care
$120*
$90
$80
$30
$6
$60
$40
Full cost until
deductible is met
$250
$250
$75
$30
$250
$150
$40
$35
$35
$15
$8
$35
$20
$65
$50
$25
$8
$50
$40
$250
$250
$100
$50
$250 copay
20% coinsurance***
$150 copay
10% coinsurance***
$15
$15
$5
$3
$15
$5
$50**
$45**
$20**
$10
$50 or less
$15 or less
$70**
$70**
$35**
$15
$70 or less
$25 or less
20% up to $250**
per script
20% up to $250**
per script
15% up to $150**
per script
10% up to $150
per script
20% up to $250
per script
10% up to $250
per script
Emergency Room
Laboratory Tests
pay negotiated
carrier rate per
service until
out-of-pocket
maximum is met
X-Rays and Diagnostics
Full cost until
deductible is met
Imaging
Tier 1 (Generic Drugs)
Tier 2 (Preferred Drugs)
Tier 3 (Non-preferred Drugs)
pay negotiated
carrier rate per
script until
out-of-pocket
maximum is met
Full cost
up to $500
after drug
deductible is met
Tier 4 (Specialty Drugs)
$23,451 to $29,425
$17,656 to $23,450
up to $17,655
(>200% to 250% FPL) (>150% to 200% FPL) (100% to 150% FPL)
Medical Deductible
N/A
Individual: $6,000
Family: $12,000
Individual: $2,250
Family: $4,500
Individual: $1,900
Family: $3,800
Individual: $550
Family: $1,100
Individual: $75
Family: $150
N/A
N/A
Pharmacy Deductible
N/A
Individual: $500
Family: $1,000
Individual: $250
Family: $500
Individual: $250
Family: $500
Individual: $50
Family: $100
N/A
N/A
N/A
Annual Out-of-Pocket
Maximum
$6,850
individual only
$6500 individual
$13,000 family
$6,250 individual
$12,500 family
$5,450 individual
$10,900 family
$2,250 individual
$4,500 family
$2,250 individual
$4,500 family
$6,200 individual
$12,400 family
$4,000 individual
$8,000 family
Drug prices are for a 30 day supply.
* Copay is for any combination of the first three visits. After three visits, future visits will be at full cost until the out-of-pocket maximum is met.
** Price is after pharmacy deductible amount is met.
*** See plan Evidence of Coverage for imaging cost share.
You might also like
- Travel Insurance - Out of Province DetailsDocument2 pagesTravel Insurance - Out of Province DetailsMan DanaNo ratings yet
- How Much Should A Consultant CostDocument3 pagesHow Much Should A Consultant CostBogdanBNo ratings yet
- VRC-2301 (V10 Rate Card)Document2 pagesVRC-2301 (V10 Rate Card)lead sulphideNo ratings yet
- Output:: Item No. Unit Cost Annual Usage % Total Quantity Total Value % of Total Value Cum % of Total ValueDocument1 pageOutput:: Item No. Unit Cost Annual Usage % Total Quantity Total Value % of Total Value Cum % of Total ValueLeakhanakNguonNo ratings yet
- ExcelDocument2 pagesExcelapi-300241947No ratings yet
- Gold Extras Cover at a GlanceDocument3 pagesGold Extras Cover at a GlanceLaura Leander WildeNo ratings yet
- The Hopeful Family Team Final Project Fin 101 - Part BDocument22 pagesThe Hopeful Family Team Final Project Fin 101 - Part Bapi-314991266No ratings yet
- CONDICIONES DE FARODocument3 pagesCONDICIONES DE FARONorma VillegaNo ratings yet
- Barbados NemCare Individuals Health InsuranceDocument3 pagesBarbados NemCare Individuals Health InsuranceKammieNo ratings yet
- 44.pratibha Sahoo (Micro Economics)Document4 pages44.pratibha Sahoo (Micro Economics)SHREEMAYEE PANDANo ratings yet
- Binder 3-13141Document93 pagesBinder 3-13141Anubhav JainNo ratings yet
- AISAUCES2Document8 pagesAISAUCES2jlehartNo ratings yet
- Multiple RegressionDocument4 pagesMultiple Regressionsumit kumarNo ratings yet
- 2015 Brackets & Planning Limits (Janney)Document5 pages2015 Brackets & Planning Limits (Janney)John CortapassoNo ratings yet
- Kitov China DealDocument1 pageKitov China DealAnonymous ipErpL6No ratings yet
- StickkDocument4 pagesStickkNikesh PatelNo ratings yet
- Brochure PDF MANHATTHAN LIFEDocument2 pagesBrochure PDF MANHATTHAN LIFEEmanuel ChirinosNo ratings yet
- Daily Profit CalculatorDocument9 pagesDaily Profit CalculatorHarrati IliasNo ratings yet
- Maru Betting Center Excel SheetDocument16 pagesMaru Betting Center Excel SheetRohan ShahNo ratings yet
- Budget Variance ReportDocument2 pagesBudget Variance ReportaryanneNo ratings yet
- Analisis Suturas 2020Document6 pagesAnalisis Suturas 2020David SantoandreNo ratings yet
- Premium Table Plus Rider EISDocument2 pagesPremium Table Plus Rider EISHarry SmithNo ratings yet
- Libro 1Document2 pagesLibro 1yonathanNo ratings yet
- Libro 1Document2 pagesLibro 1yonathanNo ratings yet
- BudgetDocument2 pagesBudgetMitch FelsmanNo ratings yet
- OAN AND Avings Ates: Loan Rates - Effective As of July 24, 2013Document1 pageOAN AND Avings Ates: Loan Rates - Effective As of July 24, 2013indianbuddyNo ratings yet
- Your Customized Benefits Plan at HCL America IncDocument2 pagesYour Customized Benefits Plan at HCL America IncShiv RanjanNo ratings yet
- Premium Table Deluxe Rider EISDocument2 pagesPremium Table Deluxe Rider EISHarry SmithNo ratings yet
- Cuadro de MarchaDocument1 pageCuadro de MarchaJoaco LledxNo ratings yet
- Mec 31 Act05Document1 pageMec 31 Act05chinNo ratings yet
- Fin 3060 IncomestatementDocument2 pagesFin 3060 Incomestatementapi-295008203No ratings yet
- Analysis of investment alternatives using IRRDocument7 pagesAnalysis of investment alternatives using IRRmeta pratiwiNo ratings yet
- Tithe - Percentage Giving ChartDocument1 pageTithe - Percentage Giving ChartRay Anthony Rodriguez0% (1)
- Excell FinalDocument1 pageExcell Finalapi-248089671No ratings yet
- Indic AdoresDocument139 pagesIndic AdoresAndreyPonteNo ratings yet
- Workbook 2Document3 pagesWorkbook 2api-332346855No ratings yet
- Resturant Break Even Analysis v4Document4 pagesResturant Break Even Analysis v4chris51bNo ratings yet
- Premier 3-28-14Document1 pagePremier 3-28-14api-239720148No ratings yet
- New Hire Benefits Summary: Medical, PTO, Life Ins & MoreDocument3 pagesNew Hire Benefits Summary: Medical, PTO, Life Ins & MoreRavi Prakash MayreddyNo ratings yet
- Stud-E PresentationDocument13 pagesStud-E Presentationapi-242374745No ratings yet
- Estimate weekly bike rental demand using linear regressionDocument6 pagesEstimate weekly bike rental demand using linear regressionMrunmaiNo ratings yet
- Numero Referencia Valor Total % Costo Unitario Unidades Demanda Anual Porcentaje AcumuladoDocument3 pagesNumero Referencia Valor Total % Costo Unitario Unidades Demanda Anual Porcentaje Acumuladoyenni viloriaNo ratings yet
- Revenue ForecastDocument3 pagesRevenue ForecastMarc BeaupréNo ratings yet
- Vista NB Special Offer February 2020Document2 pagesVista NB Special Offer February 2020aneeshNo ratings yet
- Excel Chapter 2 - Lab Test ADocument2 pagesExcel Chapter 2 - Lab Test AFurqan Ali KhanNo ratings yet
- Traffic intersection improvement cost analysisDocument1 pageTraffic intersection improvement cost analysisUn Tal Alberto MelendezNo ratings yet
- Forex Trading Income CalculatorDocument14 pagesForex Trading Income CalculatorPrashantPatilNo ratings yet
- Sample Development CostsDocument1 pageSample Development Costsrahul240486No ratings yet
- Key Financial Indicators For Spa SuccessDocument34 pagesKey Financial Indicators For Spa SuccessdclmanNo ratings yet
- Why Rent When You Can Buy?: Buying Costs Less Per Month. Down Payment Can Be A GiftDocument1 pageWhy Rent When You Can Buy?: Buying Costs Less Per Month. Down Payment Can Be A Giftapi-328599640No ratings yet
- All Dollar Values in Millions: Operating InformationDocument15 pagesAll Dollar Values in Millions: Operating InformationJose Hines-AlvaradoNo ratings yet
- TABL2751 Tax Rates 2021 - UpdatedDocument4 pagesTABL2751 Tax Rates 2021 - UpdatedPeper12345No ratings yet
- EQ Employee Benefits Plan Brochure (January 2023)Document8 pagesEQ Employee Benefits Plan Brochure (January 2023)Darren ChenNo ratings yet
- NSTP 1Document4 pagesNSTP 1MelbaNo ratings yet
- Total RevenueDocument1 pageTotal RevenueethanselphNo ratings yet
- Marks of Gyne-2 For 6Th Year Medical Students 2016/2017Document4 pagesMarks of Gyne-2 For 6Th Year Medical Students 2016/2017Bariqah SalahNo ratings yet
- Dental Practice BSC ReportDocument46 pagesDental Practice BSC ReportlnhpNo ratings yet
- Stock Trading P&L AnalysisDocument5 pagesStock Trading P&L AnalysisSilat KaliNo ratings yet