Professional Documents
Culture Documents
326 PDF
326 PDF
Uploaded by
simonsahiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
326 PDF
326 PDF
Uploaded by
simonsahiCopyright:
Available Formats
The following article was published in ASHRAE Journal, May 2004.
Copyright 2004 American Society of Heating, Refrigerating and AirConditioning Engineers, Inc. It is presented for educational purposes only. This article may not be copied and/or distributed electronically or
in paper form without permission of ASHRAE.
Legionella
in rresidential
esidential w
ater sy
stems
wa
systems
By Janet E. Stout, Ph.D., and Robert R. Muder, M.D.
ecent studies1,2 indicate that sporadic cases of Legionnaires
disease are acquired from a previously underappreciated
sourceresidential water systems. This article gives an overview
of research findings and what can be done to eradicate Legionella
in home systems.
Legionnaires in Hospitals
Shortly after the discovery of Legionnaires disease in the community setting,
outbreaks of Legionnaires disease were
reported in hospitals . Although cooling
towers were first implicated as the source
of exposure in early investigations, it soon
became clear that potable water distribution systems (warm water systems) represented the primary source of exposure for
hospital-acquired Legionnaires disease.3
Subsequent investigations showed that
12% to 70% of hospital water systems
were colonized with Legionella.4 Prospective clinical studies have demonstrated a direct link between the presence
52
ASHRAE Journal
of the bacterium in the water supply and
the occurrence of disease.5
If hospital water distribution systems
were colonized with Legionella
pneumophila and were the source of infection for hospitalized patients, investigators hypothesized that the same must
be true for residential water systems. In
1987, we published the first report of
community-acquired Legionnaires disease acquired from exposure within the
home.6 Subsequent reports showed that
6% to 32% of homes could be colonized
with Legionella (Table 1).1 Investigation
of cases of community-acquired
legionellosis has led to the emerging recashrae.org
ognition that the disease can be contracted from the water in a patients home.
We are involved in a large-scale study
of community-acquired Legionnaires
disease sponsored by the U.S. Environmental Protection Agency. The studys
objective is to determine, in a systematic fashion, how often residential
water systems are the source of exposure
for community-acquired Legionnaires
disease.
Legionella in Home Systems
The preliminary results of this study
were reported in October 2003.2 Our
study is ongoing. However, the results
are consistent with the message that the
overall risk of acquiring this disease
from exposure within the home is likely
to be low. However, certain individuals
are at greater risk of acquiring Legionnaires disease from exposure to the bacterium in residential water systems.
About the Authors
Janet E. Stout, Ph.D., is director of the Special
Pathogens Laboratory and Robert R. Muder,
M.D., is a hospital epidemiologist, at the Pittsburgh VA Healthcare System, Pittsburgh, Pa.
May 2004
Recent studies 1,2 indicate that sporadic cases
of Legionnaires disease are acquired from a
previously underappreciated sourceresiden-
tial water systems.
We followed 35 cases of Legionnaires disease caused by L.
pneumophila, serogroup 1 (15 from Ohio and 20 from Pennsylvania). For 24 cases the diagnosis was made by culture, for
10 by urinary antigen testing, and one by direct fluorescent
antibody (DFA).
Environmental testing of the residential water system was
performed for 60% (21/35) of eligible cases. A link to home
exposure was made if the identical strain that infected the
patient was also found in the home water system. L.
pneumophila, serogroup 1 was the disease-causing species in
all patients and was isolated from the home water
systems of 24% (5/21) of these patients. Molecular typing of patient and environmental isolates
was performed by pulsed-field gel electrophoresis (PFGE) for 2/5 cases. The diagnosis of Legionnaires disease was made by the urinary antigen test for the
remaining three cases, thus no isolate was available for typing.
This analysis supports the conclusion that the source of exposure was the residential water supply.
Home water systems of patients infected with L. pneumophila,
serogroup 1 were extensively colonized with L. pneumophila,
serogroup 1. In these homes, 92% (22/24) of water outlets were
positive for L. pneumophila, serogroup 1. Similarly in a Quebec
survey, positive cultures were found in the hot water tank in
52.2% (36/69), at a distal site (faucet or showerhead) in 43.5%
(30/69), and in both hot water tank and distal sites 4.3% (3/69).7
Thus, it is important that multiple sites in a patient home
must be cultured for maximal sensitivity.
May 2004
Two of our patients had a previous hospital admission within
the incubation period for the disease. Interestingly, for one
patient both the hospital and home water systems were positive for L. pneumophila, serogroup 1. PFGE typing supported
the conclusion that the disease-causing strain came from the
home water system and not the hospital water system.
Who Is at Risk?
Legionellosis typically occurs in individuals with underlying illnesses that increase their risk of disease. These conditions
include chronic lung disease, immunosuppression, organ transplant recipients, HIV infection,
diabetes, advance age, and cancer. Treatment
with high doses of corticosteroids also significantly increases the risk of infection.
In our current study, those individuals that acquired Legionnaires disease from exposure to the organism in the home water system were >70 years of age, or had an underlying disease
such as cancer, leukemia or HIV.
Demographic data also is available for 13 Legionnaires disease cases from other studies where the home water system was
the source of infection.1 In these studies, the median age was 56
years (range 20 to 76 years), 23% (3/13) were cigarette smokers,
one patient had chronic lung disease, and 54% (7/13) were considered immunosuppressed. The mortality was 23% (3/13).
In health care today, most hospitalized patients have a short
hospital stay and are sent home with serious medical conditions. An unfortunate consequence of this practice is an everASHRAE Journal
53
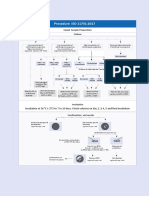
Risk Factors for Colonization
Temp. Hot
Electric Heater
Other
Water Tank
Location
Number of
Homes
Percent
Colonization
Legionella
Serogroups
Pittsburgh
55
10.9%
(6/55)
Lp1
Low
Yes
Quebec, Canada
211
32.7%
(69/21)
Lp4 (24.8%)
Lp2 (21%)
Low
Yes
Pittsburgh
218
6.4%
(14/218)
Lp1 (85%)
Low
No *
Germany,
Netherlands and
Austria
65
8%
(5/65)
Lp
N/A
N/A
City Area
Low Temp., Faucet,
Old Heater, Old
District
City Area, Iron Level,
Low Temp. Faucet
Copper Plumbing,
Low Water Use
* Only 5% of homes had electric heaters; Lp = L. pneumophilia; N/A = not available. Reprinted with permission from European Journal of Clinical Microbiology and Infectious Diseases.
Table 1: Risk factors for Legionella environmental colonization in homes.
expanding pool of individuals that may be susceptible to
Legionella infection from exposure within the home.
Mode of Transmission
Aspiration (from contaminated water or transient oropharyngeal colonization) or intense aerosolization via a humidifier or
whirlpool spa may be the mode of transmission in sporadic
cases of community-acquired Legionnaires disease rather than
by aerosolization. Although aerosolization via showering is intuitively attractive, showering has not been shown to be a major
disseminator of Legionella.8 We have shown that multiple outlets within the home may be colonized with the bacterium. Exposure to Legionella could occur from any one of these outlets.
Therefore, it is virtually impossible to pinpoint the precise mode
of transmission within the home environment.
What Can be Done?
When we found a home water system heavily colonized
with L. pneumophila, a thermal eradication (heat and flush) procedure was performed. Thermal eradication has been used in
hospitals for Legionella disinfection for many years. This procedure is labor intensive in the hospital setting, but it is relatively easy to perform in the residential setting. The procedure
involves raising the hot water temperature to the maximum setting on the hot water tank (140F [60C]) and flushing each
outlet for 20 to 30 minutes with the super-heated water. After the
procedure the temperature was returned to the previous setting.
A thermal eradication procedure was performed in four
homes. The reduction in Legionella percent positivity of outlets for each home was 75% to 25%, 100% to 0%, 100% to 0%,
and 100% to 0%, respectively. This procedure appeared to be
as effective in home water systems as it has been in hospital
water systems. Likewise, we would expect that the reduction
in Legionella colonization may be short-term (months) and
may have to be repeated if recolonization occurs.
Conclusions and Recommendations
A recent publication provides an extensive review of the
subject of Legionnaires disease acquired from residential wa54
ASHRAE Journal
ter systems. 1 This publication can be viewed at
www.legionella.org. Our results, and the results from other studies, provide growing evidence that sporadic cases of Legionnaires disease are acquired from a previously unappreciated
sourceexposure to potable water sources within the home.
Based on these results we conclude the following:
1. Community-acquired Legionnaires disease is acquired
from exposure to residential water systems more often than
previously appreciated.
2. Residential water systems should be investigated as possible sources for sporadic cases of Legionnaires disease before implicating cooling towers and aerosol-producing devices.
3. Patients with underlying conditions that increase their
risk of contracting Legionnaires disease (cancer, immunosuppressive therapy, advanced age) may benefit from preventive
measures to reduce exposure to Legionella within the home.
This may include periodic thermal disinfection, point-of-use
filtration, or use of boiled water for drinking.
References
1. Pedro-Botet, M.L., J.E. Stout, V.L. Yu. 2002. Legionnaires disease contracted from patient homes: the coming of the third plague?
Eur J Clin Microbiol Infect Dis, 21:699705.
2. Stout, J.E., R.R. Muder, A.P. Dufour, et al. 2003. Communityacquired Legionnaires disease: residential water systems are an underappreciated source of exposure. 43rd Interscience Conference for
Antimicrobial Agents and Chemotherapy, p. 341.
3. Muder, R.R., V.L.Yu, A. Woo. 1986. Mode of transmission of
Legionella pneumophila: a critical review. Arch Intern Med, 146:1607
1612.
4. Lin, Y.E., R.D. Vidic, J.E. Stout, et al. 1998. Legionella in water
distribution systems. J Amer Water Works Assoc, 90:112121.
5. Yu, V.L. 1998. Resolving the controversy on environmental cultures for Legionella. Infect Cont Hosp Epid, 19: 893897.
6. Stout, J.E., V.L. Yu, and P. Muraca. 1987. Legionnaires disease
acquired within the homes of two patients. Link to the home water
supply. JAMA, 257(9):12151217.
7. Alary, M., J.R. Joly. 1991. Risk factors for contamination of
domestic hot water systems by Legionella. Appl Environ Microbiol,
57:23602367.
8. Sabria, M., V.L. Yu. 2002. Hospital-acquired legionellosis: solutions for a preventable disease. Lancet Infect Dis, 2:368373.
ashrae.org
May 2004
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Maintaining Water Quality For Hemodialysis - UpToDateDocument22 pagesMaintaining Water Quality For Hemodialysis - UpToDateRudy Alvarez100% (2)
- NEA Code of Practice For Control of Legionella Bacteria in Cooling TowersDocument33 pagesNEA Code of Practice For Control of Legionella Bacteria in Cooling TowersVishwajeet SinghNo ratings yet
- Puthoff Et Al - Engineering The Zero-Point Field and Polarizable Vacuum For Interstellar Flight (2002)Document8 pagesPuthoff Et Al - Engineering The Zero-Point Field and Polarizable Vacuum For Interstellar Flight (2002)ramy86No ratings yet
- Legionella ToolkitDocument32 pagesLegionella Toolkitilieoniciuc100% (1)
- HANNA General Catalog v28 Chapter10 PhotometersDocument88 pagesHANNA General Catalog v28 Chapter10 PhotometersOrtomet_SANo ratings yet
- Environmental Infection Control in Health-CareDocument249 pagesEnvironmental Infection Control in Health-Caresutheeranand100% (1)
- Australian/New Zealand StandardDocument29 pagesAustralian/New Zealand StandardKayleigh Maynard100% (1)
- EUROHEAT & POWER Guidelines For District Heating SubstationsDocument72 pagesEUROHEAT & POWER Guidelines For District Heating SubstationsVadim Lisnic100% (1)
- Model Cooling Tower Maintenance Program PDFDocument41 pagesModel Cooling Tower Maintenance Program PDFMyo SeinNo ratings yet
- ISO 11731-2017 Legionella - NewDocument1 pageISO 11731-2017 Legionella - Newsylvana0% (2)
- BS1881-131 1998Document17 pagesBS1881-131 1998venkateswara rao PothinaNo ratings yet
- Legionella Pocket GuideDocument32 pagesLegionella Pocket GuideIoR100% (1)
- Design OTDocument7 pagesDesign OTyafetNo ratings yet
- Title: Intrinsic Safety Made Easy: Profile of Kuan Teik HuaDocument14 pagesTitle: Intrinsic Safety Made Easy: Profile of Kuan Teik Huaramy86No ratings yet
- Recent Developments in Eddy Viscosity Modelling of TurbulenceDocument11 pagesRecent Developments in Eddy Viscosity Modelling of Turbulenceramy86No ratings yet
- Type 262K FilterDocument4 pagesType 262K Filterramy86No ratings yet
- Conservation Laws of Fluid Motion and Boundary Conditions: Ibrahim SezaiDocument20 pagesConservation Laws of Fluid Motion and Boundary Conditions: Ibrahim Sezairamy86No ratings yet
- The Benchtop: A Useful But Little-Known Tool For Science and EngineeringDocument3 pagesThe Benchtop: A Useful But Little-Known Tool For Science and Engineeringramy86No ratings yet
- 951 Eng PerfmodDocument126 pages951 Eng Perfmodramy86No ratings yet
- CTRCTRC TVTRCVT YtvtcvtDocument8 pagesCTRCTRC TVTRCVT Ytvtcvtramy86No ratings yet
- 34536653Document32 pages34536653ramy86No ratings yet
- 944 Turbo Engine Performance ModificationsDocument13 pages944 Turbo Engine Performance Modificationsramy86No ratings yet
- Cvalt PDFDocument2 pagesCvalt PDFramy86No ratings yet
- Laplace Transform InputsDocument4 pagesLaplace Transform Inputsramy86No ratings yet
- Training Attendance Sheet: Committee MentorDocument2 pagesTraining Attendance Sheet: Committee Mentorramy86No ratings yet
- Sanitization-Remove Hidden Data From PDF Files With Adobe Acrobat XIDocument1 pageSanitization-Remove Hidden Data From PDF Files With Adobe Acrobat XIramy86No ratings yet
- A New Hybrid Thermal Comfort Guideline For The Netherlands (ISSO 74: 2014)Document12 pagesA New Hybrid Thermal Comfort Guideline For The Netherlands (ISSO 74: 2014)ramy86No ratings yet
- Incompressible Navier-Stokes RequirementsDocument13 pagesIncompressible Navier-Stokes Requirementsramy86No ratings yet
- Sensormount: SKF Spherical Rolling Bearings and Carb Pioneers in Digital Drive-Up MonitoringDocument2 pagesSensormount: SKF Spherical Rolling Bearings and Carb Pioneers in Digital Drive-Up Monitoringramy86No ratings yet
- Dresser-Rand Engineer Writes Comprehensive Guide To Dry Gas SealsDocument1 pageDresser-Rand Engineer Writes Comprehensive Guide To Dry Gas Sealsramy86No ratings yet
- Compressor Start Up ChecklistDocument2 pagesCompressor Start Up Checklistramy86No ratings yet
- Cloud& Pour Points in Fuel BlendsDocument5 pagesCloud& Pour Points in Fuel Blendsramy86No ratings yet
- Temperature Scales: Visit The Peak Sensors Online Design Guide atDocument1 pageTemperature Scales: Visit The Peak Sensors Online Design Guide atramy86No ratings yet
- GSCP Environmental Reference RequirementsDocument25 pagesGSCP Environmental Reference RequirementsSri KumarNo ratings yet
- Lovibond CatalogDocument96 pagesLovibond CatalogsijinjoyNo ratings yet
- Chlorine Dioxide Generation Bluesense Oxiblu: A Breakthrough in Without PrecursorsDocument29 pagesChlorine Dioxide Generation Bluesense Oxiblu: A Breakthrough in Without PrecursorsMax JunghannsNo ratings yet
- Presentation HuwaSan WT Legionella - CovidDocument22 pagesPresentation HuwaSan WT Legionella - CovidHersh F. HawramyNo ratings yet
- Care Free Water Conditioners EnglishDocument12 pagesCare Free Water Conditioners Englishteguh santosoNo ratings yet
- Biocide BrochureDocument24 pagesBiocide BrochureshalabyahmedNo ratings yet
- Ib 5Document49 pagesIb 5kanishkaNo ratings yet
- Mahon CompileDocument13 pagesMahon CompileSheinor Fae GalzoteNo ratings yet
- WHO Guidelines For Drinking-Water QualityDocument595 pagesWHO Guidelines For Drinking-Water QualityAbdul SalamNo ratings yet
- Drinking Water Parameter Cooperation ProjectDocument240 pagesDrinking Water Parameter Cooperation ProjectramNo ratings yet
- CH 18 Haemophilus and Other Fastidious GNBDocument37 pagesCH 18 Haemophilus and Other Fastidious GNBshericeNo ratings yet
- CoP - 12.0 - Prevention and Control of Legionnaires DiseaseDocument11 pagesCoP - 12.0 - Prevention and Control of Legionnaires DiseaseNiel Brian VillarazoNo ratings yet
- Biofilm Formation On Copper and Galvanized Steel Surfaces in ADocument7 pagesBiofilm Formation On Copper and Galvanized Steel Surfaces in AMarcus ViníciusNo ratings yet
- Equipos Monitoreo de CondicionesDocument11 pagesEquipos Monitoreo de CondicionesJonathan Vasquez LlagunoNo ratings yet
- HuwaSan Brochure PDFDocument8 pagesHuwaSan Brochure PDFKaneki KenNo ratings yet
- Wedeco Sogutma Suyunda Ozon SistemleriDocument8 pagesWedeco Sogutma Suyunda Ozon SistemleriAndrey GyrychNo ratings yet
- Quincy Legionella Report 4-6-18Document35 pagesQuincy Legionella Report 4-6-18Mark MaxwellNo ratings yet
- Spa LegionDocument4 pagesSpa LegionGeorge GeorgievNo ratings yet