Professional Documents
Culture Documents
Ineffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)
Uploaded by
Alba ArjunOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ineffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)
Uploaded by
Alba ArjunCopyright:
Available Formats
Ineffective Cerebral Tissue Perfusion Stroke (CVA) Nursing Care Plan (NCP)
Nursing Interventions Determine factors related to individual situation/cause for coma/decreased cerebral perfusion and potential for increased ICP. Rationale Influences choice of interventions. Deterioration in neurological signs/symptoms or failure to improve after initial insult may reflect decreased intracranial adaptive capacity requiring patient be transferred to critical care area for monitoring of ICP, other therapies. If the stroke is evolving, patient can deteriorate quickly and require repeated assessment and progressive treatment. If the stroke is completed, the neurological deficit is nonprogressive, and treatment is geared toward rehabilitation and preventing recurrence. Monitor/document neurological status frequently and compare with baseline. Assesses trends in level of consciousness (LOC) and potential for increased ICP and is useful in determining location, extent, and progression/resolution of CNS damage. May also reveal presence of TIA, which may warn of impending thrombotic CVA. Monitor vital signs, i.e., note:Hypertension/hypotension, compare BP readings in both arms;Heart rate and rhythm; auscultate for murmurs; Fluctuations in pressure may occur because of cerebral pressure/injury in vasomotor area of the brain. Hypertension or postural hypotension may have been a precipitating factor. Hypotension may occur because of shock (circulatory collapse). Increased ICP may occur because of tissue edema or Respirations, noting patterns and rhythm, e.g., periods of apnea after hyperventilation, CheyneStokes respiration. clot formation. Subclavian artery blockage may be revealed by difference in pressure readings between arms.Changes in rate, especially bradycardia, can occur because of the brain damage. Dysrhythmias and murmurs may reflect cardiac disease, which may have precipitated CVA (e.g., stroke after MI or from valve dysfunction).Irregularities can suggest location of cerebral insult/increasing ICP and need for further intervention, including possible respiratory support. Evaluate pupils, noting size, shape, equality, light reactivity. Pupil reactions are regulated by the oculomotor (III) cranial nerve and are useful in determining whether the brainstem is intact. Pupil size/equality is determined by balance between parasympathetic and
sympathetic enervation. Response to light reflects combined function of the optic (II) and oculomotor (III) cranial nerves. Document changes in vision, e.g., reports of blurred vision, alterations in visual field/depth perception. Specific visual alterations reflect area of brain involved, indicate safety concerns, and influence choice of interventions. Assess higher functions, including speech, if patient is alert. Changes in cognition and speech content are an indicator of location/degree of cerebral involvement and may indicate deterioration/increased ICP. Position with head slightly elevated and in neutral position. Reduces arterial pressure by promoting venous drainage and may improve cerebral circulation/perfusion. Maintain bedrest; provide quiet environment; restrict visitors/activities as indicated. Provide rest periods between care activities, limit duration of procedures. Prevent straining at stool, holding breath. Continual stimulation/activity can increase ICP. Absolute rest and quiet may be needed to prevent rebleeding in the case of hemorrhage. Valsalva maneuver increases ICP and potentiates risk of rebleeding. Assess for nuchal rigidity, twitching, increased restlessness, irritability, onset of seizure activity. Indicative of meningeal irritation, especially in hemorrhage disorders. Seizures may reflect increased ICP/cerebral injury, requiring further evaluation and intervention. Administer supplemental oxygen as indicated. Reduces hypoxemia, which can cause cerebral vasodilation and increase pressure/edema formation. Administer medications as indicated:Alteplase (Activase), t-PA; Thrombolytic agents are useful in dissolving clot when started within 3 hr of initial symptoms. Thirty percent are likely to recover with little or no disability. Treatment is based on trying to limit the size of the infarct, and use requires close monitoring for signs of intracranial hemorrhage. Note: These agents are Anticoagulants, e.g., warfarin sodium (Coumadin), low-molecular-weight heparin (Lovenox); antiplatelet agents, e.g., aspirin (ASA), dipyridamole (Persantine), ticlopidine (Ticlid); Antifibrolytics, e.g., aminocaproic acid (Amicar); contraindicated in cranial hemorrhage as diagnosed by CT scan.May be used to improve cerebral blood flow and prevent further clotting when embolus/thrombosis is the problem. Contraindicated in hypertensive patients because of increased risk of hemorrhage.Used with caution in hemorrhagic disorder to prevent lysis of formed clots and subsequent rebleeding. Antihypertensives; Preexisting/chronic hypertension requires cautious
treatment because aggressive management increases the risk of extension of tissue damage. Transient hypertension often occurs during acute stroke and resolves often without therapeutic Peripheral vasodilators, e.g., cyclandelate (Cyclospasmol), papaverine (Pavabid), isoxsuprine (Vasodilan); Steroids, e.g., dexamethasone (Decadron); Neuroprotective agents, e.g., calcium channel blockers, excitatory amino acid inhibitors, gangliosides; These agents are being researched as a means to protect the brain by interrupting the destructive cascade of biochemical events (e.g., influx of calcium into cells, release of excitatory neurotransmitters, Phenytoin (Dilantin), phenobarbital; buildup of lactic acid) to limit ischemic injury. May be used to control seizures and/or for sedative action. Note: Phenobarbital enhances action of Stool softeners. antiepileptics. Prevents straining during bowel movement and corresponding increase of ICP. Prepare for surgery, as appropriate, e.g., endarterectomy, microvascular bypass, cerebral angioplasty. Monitor laboratory studies as indicated, e.g., prothrombin time (PT)/activated partial thromboplastin time (aPTT) time, Dilantin level. Provides information about drug effectiveness/therapeutic level. May be necessary to resolve situation, reduce neurological symptoms/risk of recurrent stroke. Use is controversial in control of cerebral edema. Used to improve collateral circulation or decrease vasospasm. intervention.
The client will maintain adequate cerebral tissue perfusion as evidenced by: 1. absence of dizziness, visual disturbances, and speech impairments 2. usual or improved mental status 3. usual or improved sensory and motor function.
The body's fluid balance is frequently in flux as a result of electrolyte disturbances thus increasing the risk of peripheral edema.
With regards to the swelling, in my experience this is usually caused by a lack of vascular tone in the affected limb, causing leakage of fluid into the soft tissue. The best way to treat this is with
mobilization of the leg, elevating it above the level of the heart when he is sitting or lying, and using compression stockings to push the fluid out. The one thing that you must be sure about, however, and you must check with his doctor about, is whether a clot in the veins of the leg has been excluded. If he was immobile for long enough, a clot could form in that leg and cause swelling. That is a dangerous possibility. An ultrasound can quickly evaluate for that possibility.
Impaired Verbal Communication Stroke (CVA) Nursing Care Plan (NCP)
Nursing Interventions Assess type/degree of dysfunction: e.g., patient does not seem to understand words or has trouble speaking or making self understood. Rationale Helps determine area and degree of brain involvement and difficulty patient has with any or all steps of the communication process. Patient may have trouble understanding spoken words (receptive aphasia/damage to Wernickes speech area), speaking words correctly (expressive Differentiate aphasia from dysarthria; aphasia/damage to Brocas speech areas), or may experience damage to both areas.Choice of interventions depends on type of impairment. Aphasia is a defect in using and interpreting symbols of language and may involve sensory and/or motor components, e.g., inability to comprehend written/spoken words or to write, make signs, speak. A dysarthric person can understand, read, and write language but has difficulty forming/pronouncing words Listen for errors in conversation and provide feedback; because of weakness and paralysis of oral musculature. Patient may lose ability to monitor verbal output and be unaware that communication is not sensible. Feedback helps patient realize why caregivers are not Ask patient to follow simple commands (e.g., Shut your eyes, Point to the door); repeat simple words/ sentences; Tests for receptive aphasia. Point to objects and ask patient to name them; understanding/responding appropriately and provides opportunity to clarify content/meaning.
Have patient produce simple sounds, e.g., Sh, Cat.
Tests for expressive aphasia; e.g., patient may recognize item but not be able to name it. Identifies dysarthria, because motor components of speech (tongue, lip movement, breath control) can
Ask patient to write name and/or a short sentence. If unable to write, have patient read a short sentence.
affect articulation and may/may not be accompanied by expressive aphasia. Tests for writing disability (agraphia) and deficits in reading comprehension (alexia), which are also part of receptive and expressive aphasia.
Post notice at nurses station and patients room about speech impairment. Provide special call bell if necessary.
Allays anxiety related to inability to communicate and fear that needs will not be met promptly. Call bell that is activated by minimal pressure is useful when patient is unable to use regular call system.
Provide alternative methods of communication, e.g., writing or felt board, pictures. Provide visual clues gestures, pictures, needs list, demonstration). Anticipate and provide for patients needs.
Provides for communication of needs/desires based on individual situation/underlying deficit.
Helpful in decreasing frustration when dependent on others and unable to communication desires.
Talk directly to patient, speaking slowly and distinctly. Use yes/no questions to begin with, progressing in complexity as patient responds.
Reduces confusion/anxiety at having to process and respond to large amount of information at one time. As retraining progresses, advancing complexity of communication stimulates memory and further enhances word/idea association.
Speak in normal tones and avoid talking too fast. Give patient ample time to respond. Talk without pressing for a response.
Patient is not necessarily hearing impaired, and raising voice may irritate or anger patient. Forcing responses can result in frustration and may cause patient to resort to automatic speech, e.g., garbled speech, obscenities.
Encourage SO/visitors to persist in efforts to communicate with patient, e.g., reading mail, discussing family happenings even if patient is unable to respond appropriately. Discuss familiar topics, e.g., job, family, hobbies.
It is important for family members to continue talking to patient to reduce patients isolation, promote establishment of effective communication, and maintain sense of connectedness with family. Promotes meaningful conversation and provides opportunity to practice skills.
Respect patients preinjury capabilities; avoid speaking down to patient or making patronizing remarks. Consult with/refer to speech therapist.
Enables patient to feel esteemed, because intellectual abilities often remain intact.
Assesses individual verbal capabilities and sensory, motor, and cognitive functioning to identify deficits/therapy needs.
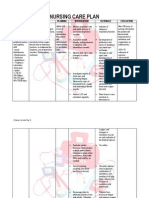
Hi, this is my first post and I'm not sure if anyone would be willing to proof this care plan for me or not, but hopefully someone will give me their opinion. We have to complete 1 nursing diagnosis for a care plan (our first) so if someone would read over this and leave comments, I'd appreciate it. Thanks !! Acute pain r/t vascular inflammation secondary to DVT. AEB: 1) Pain level of 8 on 0-10 scale. 2) Edema in right leg. 3) Facial grimacing. 4) Pt reports "uncomfortable and pressure on lower legs when in bed." Pt Goals: 1) The pt will report relief of pain to a level of 5-6 on pain scale of 0-10 by 1/23/09 0900. 2) The pt's right leg will have a reduction in edema by 1/23/09 0900. 3) The pt will report relief of pressure on lower leg when in bed by 1/23/09 0900. 4) The pt will exhibit less facial grimacing by 1/23/09 0900. Plan: 1) Administer Dilaudid 1 mg q4h PRN 1/23/09 0900. 2) Assist reduction of edema by elevating lower legs on pillows below the knee PRN 1/23/09 0900. 3) Provide comfort by elevating lower legs on pillows below the knee PRN 1/23/09 0900. 4) Assess pain in patient by using self report on pain sacle 0-10 q4h 1/23/09 0900. 5) Provide emotional support by talking with patient PRN 1/23/09 0900. 6) Assess edema in right leg by comparing it with baseline circumference measurements q8h 1/23/09 0900. Rationale: 1) Dilaudid blocks pain receptors inhibiting the transmission of pain, which provides pain relief. 2) Elevating the legs removes pressure, promotes the return of blood through leg veins, which reduces edema. 3)Elevating the legs removes pressure, promotes the return of blood through leg veins, which provides physical comfort to the patient. 4) Assessing the patient's pain level indicates if relief measures are working and provides valid and reliable measures of pain intensity. 5) Providing emotional support assists in relieving the patient's fear, anxiety, and provides distraction, assisting the patient in coping with pain. 6) Assessing edema in the right leg by measuring circumference and comparing to baseline measurements provides a reliable measure of edema reduction. Evaluation: (I think this part is very easy, so don't need it proofed) Thanks a Bunch for any advice !!!
You might also like
- Clinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessFrom EverandClinical Autonomic and Mitochondrial Disorders: Diagnosis, Prevention, and Treatment for Mind-Body WellnessNo ratings yet
- Ineffective Cerebral Tissue PerfusionDocument3 pagesIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- NCP of CavDocument3 pagesNCP of CavHenry Roque TagalagNo ratings yet
- A Neurological-WPS OfficeDocument33 pagesA Neurological-WPS OfficeEvidence ChaibvaNo ratings yet
- CVA SsDocument39 pagesCVA SsAnushri ManeNo ratings yet
- Child's Head Growth ConcernDocument8 pagesChild's Head Growth ConcernAlden MendozaNo ratings yet
- Care of Unconscious PatientDocument6 pagesCare of Unconscious PatientSuparna SinghaNo ratings yet
- NEUROLOGY BasicsDocument179 pagesNEUROLOGY BasicsmuntahaNo ratings yet
- Cerebrovascular Accident Nursing Care PlanDocument4 pagesCerebrovascular Accident Nursing Care PlanCyrus De Asis67% (12)
- AssigmentDocument3 pagesAssigmentShakir Ullah AfridiNo ratings yet
- Cerebral Vascular Accident (Stroke)Document5 pagesCerebral Vascular Accident (Stroke)SN. CaRNo ratings yet
- Rapid Focused Neurological Assessment in The Emergency Department and ICUDocument16 pagesRapid Focused Neurological Assessment in The Emergency Department and ICUAnnie RicoNo ratings yet
- Chapter 1Document182 pagesChapter 1muntahaNo ratings yet
- Ayuarista 805Document3 pagesAyuarista 805mirawati galuhNo ratings yet
- CVA-notesDocument21 pagesCVA-notesVaibhav BhatiaNo ratings yet
- Head TraumaDocument4 pagesHead TraumaDinarkram Rabreca EculNo ratings yet
- NCSBN All System Points To RememberDocument21 pagesNCSBN All System Points To Rememberhops2393% (45)
- Approach to Coma: Assessment, Management and PrognosisDocument36 pagesApproach to Coma: Assessment, Management and PrognosisashuNo ratings yet
- NCP Ineffective Cerebral Tissue PerfusionDocument2 pagesNCP Ineffective Cerebral Tissue PerfusionAngelo ︻╦̵̵͇̿̿̿̿╤── Bulacan50% (6)
- Enls V 4 0 Protocol Coma FinalDocument16 pagesEnls V 4 0 Protocol Coma Finalsucipto suciptoNo ratings yet
- Anesthesia NotesDocument25 pagesAnesthesia NotesReddyNo ratings yet
- Cerebrovascular Disorders Guide: Strokes & Risk FactorsDocument20 pagesCerebrovascular Disorders Guide: Strokes & Risk FactorsPrimas Shahibba RidhwanaNo ratings yet
- THYROIDECTOMYDocument7 pagesTHYROIDECTOMYmardsz100% (8)
- Anesthesia NotesDocument25 pagesAnesthesia NotesSaad AbdullahNo ratings yet
- Acute Cardiac Pain Management GuideDocument31 pagesAcute Cardiac Pain Management Guidejan100% (1)
- Glasgow Coma Scale and Causes of ComaDocument6 pagesGlasgow Coma Scale and Causes of ComaEm Hernandez AranaNo ratings yet
- NCPDocument9 pagesNCPTracy Camille EscobarNo ratings yet
- Neurology Nursing Study GuideDocument19 pagesNeurology Nursing Study GuideHayleyLangley100% (5)
- Hemorrhagic StrokeDocument4 pagesHemorrhagic StrokeIamanamay TrinidadNo ratings yet
- Jade R. Dinolan BSN-4: Diagnosi SDocument5 pagesJade R. Dinolan BSN-4: Diagnosi SJhade Relleta100% (1)
- Stroke 1. Disease/DisorderDocument11 pagesStroke 1. Disease/DisorderBiandaNo ratings yet
- II-E Altered PerceptionDocument16 pagesII-E Altered PerceptionDharylle CariñoNo ratings yet
- Stroke Management and Nursing CareDocument46 pagesStroke Management and Nursing Caresybilla17No ratings yet
- Unconsciousness: Law and MedicineDocument10 pagesUnconsciousness: Law and MedicineDhivya GaneshNo ratings yet
- Nursing Diagnosis For SeizureDocument6 pagesNursing Diagnosis For SeizureKenneth Cole100% (1)
- Document 2Document4 pagesDocument 2Ezra Miguel DarundayNo ratings yet
- 8 StrokeDocument8 pages8 StrokeAhmed aljumailiNo ratings yet
- Sleep Consult TemplateDocument5 pagesSleep Consult Templatesbonvallet3912100% (1)
- Ms Presentation 1Document159 pagesMs Presentation 1Francia ToledanoNo ratings yet
- Nursing DiagnosisDocument58 pagesNursing DiagnosisPrecious Santayana100% (3)
- Askep Stroke NewDocument46 pagesAskep Stroke NewArkan RadityaNo ratings yet
- General physical exam of neuro systemDocument112 pagesGeneral physical exam of neuro systemSuganya BalachandranNo ratings yet
- What Is A StrokeDocument5 pagesWhat Is A StrokeLintsuNo ratings yet
- Intracranial Aneurysm GuideDocument5 pagesIntracranial Aneurysm GuideSarah Eddiah0% (1)
- Pediatric Neuroanesthesia: Sulpicio G. Soriano, MD, Elizabeth A. Eldredge, MD, Mark A. Rockoff, MDDocument16 pagesPediatric Neuroanesthesia: Sulpicio G. Soriano, MD, Elizabeth A. Eldredge, MD, Mark A. Rockoff, MDbuddy9568No ratings yet
- Nursing Care Plan For Acute Head InjuryDocument4 pagesNursing Care Plan For Acute Head InjuryAngie Mandeoya67% (3)
- Guillain - Barre Syndrome (Polyradiculoneuritis)Document7 pagesGuillain - Barre Syndrome (Polyradiculoneuritis)Nadjmiah N. GuilingNo ratings yet
- Nur 111 Session 9 Sas 1Document6 pagesNur 111 Session 9 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Emergency Neurological Life Support - Subarachnoid HemorrhageDocument9 pagesEmergency Neurological Life Support - Subarachnoid HemorrhageIsabel VillalobosNo ratings yet
- A Head Nurse Oversees Nursing Activities in A Range of Health Care SettingsDocument8 pagesA Head Nurse Oversees Nursing Activities in A Range of Health Care SettingsMitch MaLagambaNo ratings yet
- Head InjuryDocument3 pagesHead InjuryItzel MahiyaNo ratings yet
- Understanding Stroke: Causes, Symptoms, and TreatmentDocument3 pagesUnderstanding Stroke: Causes, Symptoms, and TreatmentZnad Pein AlivioNo ratings yet
- Assessing the Neurologic Status of Patients with Traumatic Brain InjuryDocument9 pagesAssessing the Neurologic Status of Patients with Traumatic Brain InjuryNicole BertulfoNo ratings yet
- Stroke 101Document49 pagesStroke 101api-232466940No ratings yet
- Wikipedia - Vasovagal Response (CHECKED)Document7 pagesWikipedia - Vasovagal Response (CHECKED)vitruvianxyzNo ratings yet
- Dent Clin N Am 50 (2006) 625-633Document9 pagesDent Clin N Am 50 (2006) 625-633lalajanNo ratings yet
- Traumatic Brain Injury NCPDocument4 pagesTraumatic Brain Injury NCPwyneNo ratings yet
- I. Tonsilo-Pharyngeal Infections/inflammations A. AbscessesDocument5 pagesI. Tonsilo-Pharyngeal Infections/inflammations A. AbscessesAlba ArjunNo ratings yet
- FghdfghdeujDocument5 pagesFghdfghdeujAlba ArjunNo ratings yet
- Defining Communication TheoriesDocument9 pagesDefining Communication TheoriesMia SamNo ratings yet
- FsdfasdfadadaDocument3 pagesFsdfasdfadadaAlba ArjunNo ratings yet
- Caring for a child with autism requires immense patienceDocument18 pagesCaring for a child with autism requires immense patienceAlba ArjunNo ratings yet
- Benedict's ReagentDocument2 pagesBenedict's ReagentAlba ArjunNo ratings yet
- Ineffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Document6 pagesIneffective Cerebral Tissue Perfusion - Stroke (CVA) Nursing Care Plan (NCP)Alba ArjunNo ratings yet
- National Institutes of Health Stroke Scale: From Wikipedia, The Free EncyclopediaDocument11 pagesNational Institutes of Health Stroke Scale: From Wikipedia, The Free EncyclopediaAlba ArjunNo ratings yet
- Hgfjfghjset 4Document83 pagesHgfjfghjset 4Alba ArjunNo ratings yet
- Benedict's ReagentDocument2 pagesBenedict's ReagentAlba ArjunNo ratings yet
- 9 Qualitative Research DesignsDocument14 pages9 Qualitative Research DesignspizdixNo ratings yet
- Benedict's ReagentDocument2 pagesBenedict's ReagentAlba ArjunNo ratings yet
- AdadadadDocument18 pagesAdadadadAlba ArjunNo ratings yet
- Alba, Arnaldo Jr. A. BSN Iv-3 Group G-1 Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument2 pagesAlba, Arnaldo Jr. A. BSN Iv-3 Group G-1 Assessment Diagnosis Inference Planning Intervention Rationale EvaluationAlba ArjunNo ratings yet
- NCP NSDDocument3 pagesNCP NSDshigemasamayumi60% (5)
- CutDocument1 pageCutAlba ArjunNo ratings yet
- AaaaaaaaaaaaaaaaaaDocument11 pagesAaaaaaaaaaaaaaaaaaAlba ArjunNo ratings yet
- Chapt 1Document7 pagesChapt 1Nurse DianneNo ratings yet
- How computers generate randomness vs true random numbers from RANDOM.ORGDocument1 pageHow computers generate randomness vs true random numbers from RANDOM.ORGAlba ArjunNo ratings yet
- Conceptest 9.1: Rolling in The RainDocument16 pagesConceptest 9.1: Rolling in The RainAlba ArjunNo ratings yet
- The Department of Health (DOH) PhilippinesDocument21 pagesThe Department of Health (DOH) PhilippinesAlba ArjunNo ratings yet
- Eula Microsoft Visual StudioDocument3 pagesEula Microsoft Visual StudioqwwerttyyNo ratings yet
- Momentum, Impulse, and CollisionsDocument45 pagesMomentum, Impulse, and CollisionsTesfaye KebedeNo ratings yet
- 111 Samp 08Document7 pages111 Samp 08Alba ArjunNo ratings yet
- Motivation in LearningDocument3 pagesMotivation in LearningAlba ArjunNo ratings yet
- 12 Rotational EquilibriumDocument6 pages12 Rotational EquilibriumAlba ArjunNo ratings yet
- 111 Samp 08Document7 pages111 Samp 08Alba ArjunNo ratings yet
- AbstractDocument8 pagesAbstractAlba ArjunNo ratings yet
- Coping MechanismsDocument9 pagesCoping MechanismsAlba ArjunNo ratings yet
- WWW - Augusta.edu: Page 3 of About 6,73,00,000 Results (0.43 Seconds)Document2 pagesWWW - Augusta.edu: Page 3 of About 6,73,00,000 Results (0.43 Seconds)Csvv VardhanNo ratings yet
- Jadwal PublikasiDocument5 pagesJadwal Publikasidr_nadheemNo ratings yet
- Drugs in PregnancyDocument33 pagesDrugs in PregnancyserbalexNo ratings yet
- Haematology CBC (Complete Blood Count) : Name: MR - Shivam Shukla Lab No.: 011910270053Document3 pagesHaematology CBC (Complete Blood Count) : Name: MR - Shivam Shukla Lab No.: 011910270053Anant ShuklaNo ratings yet
- SLU Pathology CBL Cases for Gastrointestinal and Liver PathologyDocument6 pagesSLU Pathology CBL Cases for Gastrointestinal and Liver PathologyAaron O. CafeNo ratings yet
- Srac 0260Document4 pagesSrac 0260Wahyu SatriojatiNo ratings yet
- Pembahasan Kuis 7 Ppu - Bahasa Inggris: B.Inggris Persiapan Utbk 2021Document8 pagesPembahasan Kuis 7 Ppu - Bahasa Inggris: B.Inggris Persiapan Utbk 202154 Hilmi Nur PersadaNo ratings yet
- Orthopaedic: Congenital, Infection, Neoplasia, Trauma, AppandegesDocument1 pageOrthopaedic: Congenital, Infection, Neoplasia, Trauma, AppandegesdinsNo ratings yet
- Liposomal Doxorubicin ExtravasationDocument2 pagesLiposomal Doxorubicin ExtravasationjathieNo ratings yet
- Focal InfectionDocument2 pagesFocal InfectionRoza NafilahNo ratings yet
- Parkinson's Disease-Diagnosis & TreatmentDocument9 pagesParkinson's Disease-Diagnosis & Treatmentvivek_win95100% (1)
- Fitz Neurology Paces NotesDocument40 pagesFitz Neurology Paces NotesDrShamshad Khan100% (1)
- Congenital Ptosis: Evalution and Management DR - Tarakeswara Rao - MsDocument27 pagesCongenital Ptosis: Evalution and Management DR - Tarakeswara Rao - MsVikram Simha NagendlaNo ratings yet
- Rethinking Asperger S Understanding The Dsm5 Diagnosis Byintroducing Sheldon Cooper 2375 4427 1000146Document4 pagesRethinking Asperger S Understanding The Dsm5 Diagnosis Byintroducing Sheldon Cooper 2375 4427 1000146Arnav NegiNo ratings yet
- Guide to Salivary Gland NeoplasmsDocument28 pagesGuide to Salivary Gland Neoplasmsrameshparajuli14100% (1)
- Mock Patient Record: Patient Management Record For Year 5 Clinical Posting Clerkship Patient ParticularsDocument9 pagesMock Patient Record: Patient Management Record For Year 5 Clinical Posting Clerkship Patient ParticularsNabighah ZukriNo ratings yet
- Paediatrica Indonesiana: Sri Yanti Harahap, Selvi Nafianti, Sri Sofyani, Supriatmo, Atan Baas SinuhajiDocument5 pagesPaediatrica Indonesiana: Sri Yanti Harahap, Selvi Nafianti, Sri Sofyani, Supriatmo, Atan Baas SinuhajiNadira Juanti PratiwiNo ratings yet
- BTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Document2 pagesBTUH Antibiotics Pocket Guidelines For Prescribing in Adults 2017 2018Corry ApriliaNo ratings yet
- Blood ConversationDocument300 pagesBlood ConversationMohsin NabeelNo ratings yet
- HEALTH 7 EXAM (2nd Quarter) QuestionsDocument4 pagesHEALTH 7 EXAM (2nd Quarter) QuestionsKert Cyrel RomeroNo ratings yet
- Mandatory Infants and Children Health Immunization Act of 2011 Compulsory ImmunizationDocument3 pagesMandatory Infants and Children Health Immunization Act of 2011 Compulsory Immunizationbunso padilla100% (2)
- Trichuris VulpisDocument4 pagesTrichuris VulpisGerry MartinNo ratings yet
- BPC-157 A Collection of StudiesDocument28 pagesBPC-157 A Collection of StudiesscribdNo ratings yet
- Pharmacology - A Summary of Common ConditionsDocument50 pagesPharmacology - A Summary of Common ConditionsJeremy YangNo ratings yet
- CATARACT History Taking and ExaminationDocument28 pagesCATARACT History Taking and ExaminationJosephNo ratings yet
- OptoPrep Part1 StudyCalendar 3-MonthDocument4 pagesOptoPrep Part1 StudyCalendar 3-MonthmelanieNo ratings yet
- Cwu 1 OrthoDocument14 pagesCwu 1 OrthoHakimah K. Suhaimi100% (1)
- Eye - Blur Vision Part IIDocument56 pagesEye - Blur Vision Part IIStaporn Kasemsripitak100% (2)
- Top 5 Acupressure Points To Treat Cold, Flu and FeverDocument16 pagesTop 5 Acupressure Points To Treat Cold, Flu and Feverdlpurpos0% (1)
- Causes and Treatment of SplenomegalyDocument4 pagesCauses and Treatment of SplenomegalydoctorimrankabirNo ratings yet