Professional Documents
Culture Documents
Chapter Contents: 8. Maternal Resuscitation
Uploaded by
Ibnu YudistiroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter Contents: 8. Maternal Resuscitation
Uploaded by
Ibnu YudistiroCopyright:
Available Formats
8.
MATERNAL RESUSCITATION Chapter contents Cardio-pulmonary resuscitation CPR Algorithm Resuscitation drug dosages Convulsions Anaphylactic shock Pulmonary embolism
Venous thromboembolus: Amniotic fluid embolus: Venous Air Embolus
Pulmonary oedema Malignant hyperpyre ia CARDIO-PULMONARY RESUSCITATION (CPR) Cardiac arrest is rare !ith an incidence of ":#$%$$$ pregnancies& 'he survival of mother and fetus depends on prompt recognition and treatment& Main causes of cardiac arrest
Anaesthetic Problems
(ailed intubation Aspiration of gastric contents 'otal spinal anaesthesia )rug induced reactions *ocal anaesthetic to icity
Obstetric Problems
Massive haemorrhage Amniotic fluid embolism Venous and+or air embolism ,ntracranial haemorrhage Magnesium to icity After -. !eeks of pregnancy aortocaval compression is likely& ,f cardiac arrest occurs the complete absence of any vascular tone leads to a reduction in venous return to the right side of the heart& E ternal cardiac compression may therefore be ineffective% as the heart is empty& 'he patient must be tilted to at least a #$/ angle& 'his is best achieved using a specially !edged board% although it is possible to use a 0human !edge0&
Fig 8.1
Wedged board
Human wedge
,f CPR is not effective 1"2:- ratio3 in generating a po!erful pulse 1"$$+min3 or ade4uate perfusion !ithin # - 5 minutes and there is no other obvious remediable cause% e&g& massive haemorrhage% bilateral tension pneumothora or pulmonary embolus% the fetus must be delivered !hile CPR is continuing6 effective cardiac filling and output should then occur& Early delivery may also save the baby 1the fetus is more resistant to hypo ia than the mother3&
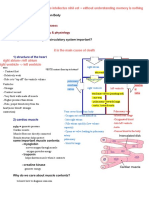
THE CHAIN OF SURVIVAL Early Access Early as!c L!"e S#$$%r&
Early De"!'r!lla&!%( Early A)*a(ce) L!"e S#$$%r&
(or every minute that elapses follo!ing the onset of a shockable arrhythmia% there is 2-"$7 less chance of survival& Early defibrillation is critical6 therefore it should not be delayed if available and appropriate& Administration of -$$% -$$ and #.$ 8oule shocks% given in se4uence if re4uired !ith a monophasic defibrillator% should not take any longer than #$ seconds& As soon as the shocks have been delivered% 9&*&: must be restarted immediately& Available data suggests that defibrillation is safe in all phases of pregnancy and labour as only a small amount of current penetrates the uterus& 9iphasic defibrillators are effective at lo!er energy levels e&g& -$$ ;& 'hey reverse current flo! during defibrillation and are as effective or better than monophasic defibrillators& ADVANCED LIFE SUPPORT AL+ORITHM FOR THE MANA+EMENT OF CARDIAC ARREST IN ADULTS
ote! each successi"e step is based on the assumption that the one before has been unsuccessful
#esuscitation Council $%. &able 8.1 #esuscitation drug doses TRACHEAL DRU+S 1a)e #$ !( a all )%ses 'ase) %( INTRAVENOUS COMMENT *%l#1e %" 2a ,- ./ 0%1a( 1l sal!(e E$!(e$3r!(e 242-5--2- 1l 6 2 1/ A&r%$!(e -.< 1/;1l -.2-2 1/ 2 1/ = 1/ 7 1/ 7 1/ a() 8 rece$&%r s&!1#la(& I("#s!%( 9 1/49-- 1l sal!(e (2- :/;1l) I(creases 3ear& ra&e C%1$le&ely 'l%c.s &3e *a/#s (er*e5 #se) !( asys&%le
=-- 1/ A1!%)ar%(e !( 7sec%() )%se 1l 9> )e?&r%se 29- 1/ 9retylium tosylate 2$$ mg 2$ mg+ml Me iletine "2$ mg bolus -2 mg+ml Calcium gluconate "$7 "$ ml 1$&--2 mmol Ca+ml3 *idocaine -7 Adenosine "$$ mg . mg -$$ mg
Use) !( re"rac&%ry "!'r!lla&!%(. C%(s!)er as early as "%#r&3 s3%c. <sed in refractory fibrillation Membrane stabilisation% reduces tendency to tachyarrythmias ,notropic action ,nfusion "&2 g:2$$ ml # mg+ml then "- mg # every - min >ot as routine% only refractory cases% p? to be measured as soon as possible @-blocker used for supraventricular arrythmias 1:V'3
:odium bicarbonate 2$ ml =&57 Metoprolol 2 mg 1" mg+ml3
Any effects of these drugs on the fetus can be addressed after delivery% resuscitation of the mother is the prime consideration& Al/%r!&31s "%r &rea&1e(& %" Per!arres& Arr3y&31!as ca( 'e accesse) 3ere 9RA)ACAR),A 9RBA) CBMP*EC 'AC?ACAR),A >ARRBD CBMP*EC 'AC?ACAR),A CONVULSIONS Main causes Eclampsia% epilepsy and local anaesthetic to icity& Consider all obstetric convulsions eclamptic in origin despite a normal blood pressure until proved other!ise& Premonitor' signs Eclampsia - May be NONE: severe frontal headache !ith visual disturbance% photophobia% nausea and vomiting% right upper 4uadrant pain& Epilepsy - Aura% history of epilepsy% anticonvulsant therapy& Local anaesthesia - >umbness of the tongue and circumoral tissues% light-headedness% diEEiness% difficulty focusing% tinnitus% slurred speech% shivering and muscle t!itching& Management
'urn the patient on her side to avoid aortocaval compression& Maintain and protect the air!ay% administer "$$7 o ygen& Ensure fetal monitoring& (ollo! one of the t!o regimes:Diazepam 2 - -$ mg i&v& 1more than #$ mg may cause neonatal hypotonia3 Intravenous thiopentone 2$ mg increments - su amethonium% cricoid pressure and intubation may be re4uired& ,f eclampsia is suspected once convulsions have ceased then the magnesium sulphate protocol is follo!ed& ANAPHYLACTIC SHOC@ Common labour !ard causes:- antibiotics% su amethonium% late % o ytocin% >:A,)s and colloids& An anaphylactic reaction is !here previous sensitisation has occurred and vasoactive substances e&g& histamine% serotonin are released from mast cells in response to an ,gE antibody mediated reaction& An anaphylactoid reaction is !here there is no antibody mediation in mast cell release& Management :top the administration of all suspected drugs and curtail surgery if appropriate& Maintain the air!ay% give "$$7 o ygen% and avoid aortocaval compression& Five e$!(e$3r!(e 242-5--- (2 1/42- 1l sal!(e) !.*. as -.9 - 2 1l '%l#ses % titrate as necessary for hypotension and bronchospasm& :tart rapid intravascular volume e pansion !ith crystalloid or colloid&
(pecific measures Hypotension - Elevate the legs% establish monitoring !ith ECF and possibly CVP and arterial line& Circulatory support !ith catecholamines& Bronchospasm aminophylline salbutamol -2$ - 2$$ mg i&v& slo!ly -2$ Gg i&v& slo!ly -&2 - 2 mg nebulised in # ml saline Antihistamines chlorpheniramine Steroids hydrocortisone "$$ - -$$ mg i&v& "$ - -$ mg i&v&
A(a$3yla?!s al/%r!&31 ca( 'e accesse) 3ere4-
I(*es&!/a&!%( ,mmediate - mast cell tryptase% the principle protein content of mast cell granules is released !ith histamine and other amines in anaphylactic and anaphylactoid reactions& Plasma concentration is raised " - . h after a reaction& >ormal level $&= - "&2 ng+ml H-$ng+ml *ong term - referral to allergist for skin testing and specific ,gE antibody detection by radio-allergosorbent test 1RA:'3 Anaphylactic reactions occur at concentrations
PULMONARY EM OLISM 'his is the commonest cause of maternal death in the <nited Iingdom& Emboli may be thrombus% amniotic fluid or air& 'he physiological changes that occur depend on the degree of obstruction to blood flo! through the pulmonary artery and the increase in dead space ventilation& 'hese may lead to pulmonary hypertension% right ventricular strain and cardiac failure& )uring anaesthesia an early sign is an abrupt fall in end tidal PCB)enous thromboembolus 'he risk of venous thrombosis is increased in pregnancy due to the relatively hypercoagulable state% particularly in the postpartum period& 'he presentation includes retrosternal discomfort% dyspnoea% pleuritic pain% haemoptysis% profound collapse% raised central venous pressure and cardiac arrest& 'he ECF sho!s: :"J#'# pattern !ith prominent : !ave in lead ,% J !ave and inverted ' in lead ,,, :inus tachycardia ' !ave inversion in leads V"-V# Right bundle branch block *o! amplitude deflection
A ventilation perfusion scan !ill sho! normal ventilation !ith a segmental perfusion defect& Pulmonary angiography may demonstrate an intraluminal filling defect and+or the abrupt termination of a branch vessel& Management of minor thromboembolism ?eparinisation - 2%$$$ -"$%$$$ i+u i&v& follo!ed by a continuous infusion of "%$$$--%$$$ i+u per hour& Monitored !ith the APP' - therapeutic range "&2--&2& Antenatally heparin is given sc - "-%$$$ i+u "- hourly& Postnatally oral !arfarin is started at the same time as i&v& heparin - "$ mg+day for -days& :ubse4uent dosage depends on the ,>R - therapeutic range --#&
Management of massi"e thromboembolism
B ygen therapy% cardiac massage and intermittent positive pressure ventilation 1,PPV3 An intravenous bolus of heparin - "2%$$$ i+u should be given& Cardiovascular support !ith a norepinephrine infusion 5 mg in 2$$ ml of saline A pulmonary angiogram should be obtained immediately: if this is not available thrombolytic therapy must be started !ith streptokinase in a loading dose of .$$%$$$ units !ith a maintenance dose of "$$%$$$ u+h for -5 hours& 'he thrombin time should be maintained at a level of "K times the control value&
Amniotic fluid embolus *Anaph'lactoid ('ndrome of Pregnanc'+ 'he incidence is " in #$%$$$ pregnancies !ith a maternal mortality rate approaching =27% ,t can occur during labour 1L$73% after Caesarean delivery 1"M73% or after vaginal delivery 1""73& 'he presenting features are :udden collapse E cessive bleeding in labour or post partum :eiEures )yspnoea (etal bradycardia
'here is a history in 5"7 of mothers of atopy 1asthma% ecEema% hay fever3 or allergy% often to drugs& 'here is a biphasic response to the presence of amniotic fluid 1or meconium3 in the maternal circulation causing release of substances that produce pulmonary vascular spasm% pulmonary hypertension% hypo ic in8ury to the pulmonary capillaries and heart& 'his leads to left ventricular failure and subse4uent adult respiratory distress syndrome& Coagulopathy may be related to the presence of a factor C activator in amniotic fluid& )iagnosis is made on clinical grounds& 'he presence of fetal cells in the maternal blood is >B' pathognomonic and they are commonly detected in normal patients& ,n primates it has been sho!n that infusions of large amounts of amniotic fluid do >B' cause the syndrome& Minor degrees of the syndrome are probably 4uite common& Management Cardiopulmonary resuscitation !ith the patient !edged if the fetus is still in utero )eliver the fetus and placenta as soon as possible ,nsert - large peripheral cannulae% CVP line% urinary catheter% arterial line and if possible a pulmonary artery catheter Aspirate blood from the right side of the heart Monitor ECF% pulse% blood pressure% CVP and pulmonary artery !edge pressure Cardiovascular support !ith dopamine and epinephrine ),C management in consultation !ith the ?aematology )epartment
)enous air embolus 'his can occur during Caesarean section particularly at the time of uterine incision and placental separation& ,t has been sho!n that subclinical venous air embolism occurs in up to 2$7 of patients at this time6 the risk is increased !hen the uterus is e teriorised and the patient is head
do!n& A head up tilt has been advocated during surgery for Caesarean section& A patent foramen ovale is present in -$ - -2 7 of patients and parado ical air embolism is possible although very rare in clinical practice& *arge air embolism !ill result in frothing of blood in the right ventricle causing an air lock and cardiac arrest& 'he diagnosis is made !ith a precordial or oesophageal )oppler probe& A mill !heel murmur is accompanied by hypotension% a fall in SpB-% end tidal PECB- and an increase in central venous pressure& Management "$$7 o ygen must be given :top the nitrous o ide to reduce the air bubble siEe Replace the uterus if e teriorised (lood the !ound !ith fluid to prevent further aspiration of air& Place the patient in a head do!n position on the left side to allo! any air to collect in the ape of the right ventricle Aspirate air from the right atrium via a central venous line& Provide cardio-respiratory support as necessary& ,nternal cardiac massage may be re4uired - access to the great vessels !ill permit direct aspiration of air 1or amniotic fluid3 &
PULMONARY OEDEMA Maternal pulmonary oedema is associated !ith: Pre-eclampsia - capillary permeability is increased and colloid osmotic pressure falls due to proteinuria& 'here may also be an element of left ventricular failure secondary to severe hypertension& Antihypertensive therapy !ith @-blockers may contribute to this& (luid overload - due to over-treatment of severe haemorrhage% or fluid challenges in preeclamptic patients& Myocardial disease - e&g& cardiomyopathy of pregnancy or myocardial ischaemia& 'he use of tocolytic therapy for premature labour !ith @-adrenergic agonists% e&g&% ritodrine% iso uprine% salbutamol& 'achycardia is a prominent feature& :teroid therapy for fetal lung maturation may be a contributory factor
,t presents !ith tachycardia% tachypnoea% hypo ia and cyanosis& An early sign is a fall in o ygen saturation& Bn auscultation of the chest% basal crepitations and rhonchi are heard& Chest -ray sho!s fluffy shado!ing or the more e tensive butterfly !ing appearance& Management B ygen :edation !ith i&v& morphine to relieve agitation + an iety and reduce the pre-load by venodilatation& )iuretic therapy !ith frusemide 5$ - =$ mg i&v&% repeated as necessary& )opamine - - 2 Gg+kg+min may be re4uired i&v&& ,ntubation and ,PPV may be necessary !ith positive end e piratory pressure 1PEEP3 'reatment of the underlying cause
MALI+NANT HYPERPYREAIA (MH)
'he incidence is ":#$%$$$ of all general anaesthetic administered& >ot every patient !ith a genetic predisposition developes a M? crisis during e posure to triggering agents !hich include all volatile anaesthetics and depolarising muscle rela ants& M? presents !ith the follo!ing
signs:
<ne plained tachycardia 'achypnoea A rise in body temperature !hich increases by more than -/ C+h An abnormal reaction to su amethonium - trismus is an early sign of this Cyanosis Muscular rigidity developing later during the anaesthetic ,ncreased ooEing is usually a sign of ),C A fall in SpB-% a rise in PECB-% metabolic acidosis and hyperkalaemia A )!a/(%s!s %" MH s3%#l) 'e ass#1e) !" s#s$!c!%(s are ar%#se).
Management )iscontinue inhalational agents% terminate surgery CALL FOR HELP. ?yperventilate !ith "$$7 o ygen - - # times the predicted minute volume Five dantrolene - mg+kg i&v&& Repeat as necessary up to a total of "$ mg+kg Cool !ith " - - litres iced saline i&v&% apply surface cooling over the ma8or vessels% and lavage to the pleural or peritoneal cavities& Consider cardiopulmonary bypass via femorofemoral circulation Correct metabolic acidosis !ith sodium bicarbonate% monitor blood gases and p? and correct hyperkalaemia& 'reat arrhythmias if severe& Establish the follo!ing monitoring: SpB-% ECF% arterial cannulation% a muscle temperature probe% central venous cannulation% urinary catheter% blood pressure and a fluid balance chart& ,nvestigations should include the follo!ing: blood gases% haemoglobin% urea% electrolytes% clotting screens and CPI level Admit to the intensive care unit *ate management must include screening of the patient and her family for M? susceptibility
,n the management of kno!n M? or M? susceptible patients% the techni4ue of choice is regional anaesthesia& 'he administration of general anaesthesia re4uires the follo!ing conditions: A clean anaesthetic machine !ith disposable tubing and no vaporisers 'he circuit !hich has been flushed !ith "$ litres of o ygen for at least -$ minutes before use A cooling blanket on the operating table% )antrolene and ice must be available& Bnly NsafeN drugs must be used SAFE )iaEepam% thiopentone% propofol% methohe itone& UNSAFE :uccinylcholine
>itrous o ide Atracurium% pancuronium% vecuronium% mivacurium%% rocuronium *ocal anaesthetic drugs B ytocin% PF(-a% ergometrine >itroglycerine% magnesium sulphate Ephedrine% epinephrine% norepinephrine FURTHER READIN+
?alothane% enflurane% isoflurane% desflurane% sevoflurane
'he American ?eart Association in Collaboration !ith the ,nternational *iaison Committee on Resuscitation 1,*CBR3 Fuidelines -$$$ for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - An ,nternational Consensus on :cience& Resuscitation -$$$6 5.: "-55= 'he "MM= European Resuscitation Council Fuidelines for Adult Advanced *ife :upport& ,n: 9ossaert * 1ed&3& European Resuscitation Council uidelines !or Resuscitation & Amsterdam: Elsevier% "MM=6 #.-#L& 'he "MM= European Resuscitation Council Fuidelines for the management of the air!ay and ventilation during resuscitation& ,n: 9ossaert * 1ed&3& European Resuscitation Council uidelines !or Resuscitation& Amsterdam: Elsevier% "MM=6 "-M-"2=& Iudenchuk P;% Cobb *A% Copass MI et al& Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation& "e# En$land %ournal o! &edicine "MMM6 #5": =L"=L=&Clic' here !or &edline lin' 'he Association of Anaesthetists of Freat 9ritain and ,reland and 'he 9ritish Association of Allergy and ,mmunology( Suspected anaphylactic reactions associated #ith anaesthesia & Published by: 'he Association of Anaesthetists of Freat 9ritain and ,reland "MM2& MedicAlert (oundation 1Registered Charity3 (letcher :;% Parr M;A& Amniotic fluid embolism: a case report and revie!& Resuscitation -$$$: 5#6"5"-"5. Clic' here !or &edline lin' ?alsall P% Ellis (R& Malignant hyperthermia& Current Anaesthesia and Critical Care "MM.6 ,6 #: "2=-"..&
You might also like
- Anesthesia For High Risk PatientDocument5 pagesAnesthesia For High Risk PatientAfrida SahestinaNo ratings yet
- Guidelines For The Management of Severe Pre-Eclampsia (Anaes and Analgesia) 31.07.06Document5 pagesGuidelines For The Management of Severe Pre-Eclampsia (Anaes and Analgesia) 31.07.06grigmihNo ratings yet
- Anaesthetic Management of Pre-EclampsiaDocument28 pagesAnaesthetic Management of Pre-EclampsiaGeorge Junior AdomakoNo ratings yet
- DEFIBrilatorDocument43 pagesDEFIBrilatoranon_632568468No ratings yet
- Apnea 2019Document10 pagesApnea 2019aiswarya sreekumarNo ratings yet
- 287 Paediatric Anaesthetic Emergencies Part 1Document6 pages287 Paediatric Anaesthetic Emergencies Part 1Maaida MuzaffarNo ratings yet
- Maternal Collapse During PregnancyDocument57 pagesMaternal Collapse During PregnancytapayanaNo ratings yet
- Shock in ObstetricsDocument38 pagesShock in ObstetricsBeulah AlexNo ratings yet
- Short Answer Questions AnaesthesiaDocument91 pagesShort Answer Questions AnaesthesiaMeena Ct100% (11)
- MX of EclampsiaDocument5 pagesMX of EclampsiaYwagar YwagarNo ratings yet
- 21 Obstetric Anaesthesia PDFDocument0 pages21 Obstetric Anaesthesia PDFjuniorebindaNo ratings yet
- Chapter33Walker2015 PDFDocument12 pagesChapter33Walker2015 PDFMai AngelNo ratings yet
- Unit 5 Cardiac Emergencies: StructureDocument27 pagesUnit 5 Cardiac Emergencies: StructurebtaleraNo ratings yet
- Neonatal Shock: Intensive Care Nursery House Staff ManualDocument2 pagesNeonatal Shock: Intensive Care Nursery House Staff ManualSedaka DonaldsonNo ratings yet
- Clinical Evaluation Test Result Trends: DiagnosisDocument3 pagesClinical Evaluation Test Result Trends: DiagnosisStephen CrossNo ratings yet
- Post Partum HaemorrhageDocument6 pagesPost Partum Haemorrhagenancy jeyakumarNo ratings yet
- 185 Anaesthesia in Pregnancy For Non Obstetric SurgeryDocument9 pages185 Anaesthesia in Pregnancy For Non Obstetric SurgeryaangrohmananiaNo ratings yet
- Anaesthetic Crisis ManualDocument63 pagesAnaesthetic Crisis ManualkushishaNo ratings yet
- Changes in Maternal Physiology During PregnancyDocument4 pagesChanges in Maternal Physiology During PregnancyTina Ong SinagaNo ratings yet
- Final Assignment of ShockDocument21 pagesFinal Assignment of Shocknyandap tanyuNo ratings yet
- Nursing Diagnosis: Aurelio, Lyca Mae M. BSN II-DDocument2 pagesNursing Diagnosis: Aurelio, Lyca Mae M. BSN II-DLyca Mae AurelioNo ratings yet
- Amniotic Fluid EmbolismDocument30 pagesAmniotic Fluid EmbolismDonmer Ibañez Juan100% (1)
- Nclex Disease: 4. Oral ContraceptivesDocument7 pagesNclex Disease: 4. Oral ContraceptivesMeijia SongNo ratings yet
- Obstetrical ShockDocument56 pagesObstetrical ShockDrPreeti Thakur ChouhanNo ratings yet
- Heart Disease in Pregnancy VoiceoverDocument30 pagesHeart Disease in Pregnancy VoiceoverMohammed AbdNo ratings yet
- Amniotic Fluid EmbolismDocument19 pagesAmniotic Fluid EmbolismStar Alvarez100% (1)
- Management of PPHDocument24 pagesManagement of PPHMutabazi SharifNo ratings yet
- EclampsiaDocument34 pagesEclampsiaاحمد وائل عبد الشافى ابو المعاطى UnknownNo ratings yet
- Anaesthesia and Atrial FibrillationDocument15 pagesAnaesthesia and Atrial FibrillationNaresh Dhawan100% (1)
- Pre EclampsiaDocument3 pagesPre Eclampsiaapi-142637023No ratings yet
- Nclex Review Uworld (6515)Document137 pagesNclex Review Uworld (6515)whereswaldo007yahooc88% (8)
- Emmergency MedicineDocument48 pagesEmmergency MedicineSherein HagrasNo ratings yet
- Obstetrical Shock FinalDocument25 pagesObstetrical Shock Finalsanthiyasandy92% (13)
- Obstetrical Shock FinalDocument25 pagesObstetrical Shock Finalsanthiyasandy100% (1)
- 2-PLAB Answer Big Mock April 2021-PrintDocument12 pages2-PLAB Answer Big Mock April 2021-Printali etikar100% (1)
- Neonatal Resuscitation DrugsDocument4 pagesNeonatal Resuscitation Drugsblast2111No ratings yet
- Postpartum HemorrhageDocument53 pagesPostpartum HemorrhageDr_Soranus100% (2)
- Halls OB Anesthesia NotesDocument1 pageHalls OB Anesthesia NotesEric YaoNo ratings yet
- Seminar On Obstetrical EmergencieDocument21 pagesSeminar On Obstetrical EmergencieJyothi RameshNo ratings yet
- تخدير نظري 12 .Document13 pagesتخدير نظري 12 .adalk8y79No ratings yet
- Update ON Amniotic Fluid Embolism (AFE) : Dr. Ashraf KhalafDocument30 pagesUpdate ON Amniotic Fluid Embolism (AFE) : Dr. Ashraf KhalafMostafa EissaNo ratings yet
- Pre EclampsiaDocument39 pagesPre EclampsiaStanly Elliemo100% (1)
- Obstetric HaemorrhageDocument4 pagesObstetric Haemorrhageapi-142637023No ratings yet
- Hypovolemic Shock Neurogenic ShockDocument40 pagesHypovolemic Shock Neurogenic ShockWemslaiNo ratings yet
- Anaphylaxis: How To Recognize, Treat, and Prevent Potentially Fatal AttacksDocument8 pagesAnaphylaxis: How To Recognize, Treat, and Prevent Potentially Fatal AttacksИван Марковић ИскеNo ratings yet
- Nursing Bullets Med Surg 1 1 1Document94 pagesNursing Bullets Med Surg 1 1 1Phoebe PitallanoNo ratings yet
- Anaesthesia EclampsiaDocument39 pagesAnaesthesia EclampsiaAlfitoHarfahGiffaryNo ratings yet
- Chapter3Shock CirculationDocument13 pagesChapter3Shock CirculationSri AgustinaNo ratings yet
- Epilepsi Status EpileptikusDocument35 pagesEpilepsi Status EpileptikusLussy HendrikNo ratings yet
- Emergencia 0bstétricas PDFDocument15 pagesEmergencia 0bstétricas PDFgladymarNo ratings yet
- Neurologiccomplications Inpregnancy: Mauricio Ruiz Cuero,, Panayiotis N. VarelasDocument17 pagesNeurologiccomplications Inpregnancy: Mauricio Ruiz Cuero,, Panayiotis N. VarelasgustavoNo ratings yet
- Drug StudyDocument7 pagesDrug StudydivineNo ratings yet
- Sudden Maternal Collapse: Max Brinsmead MB Bs PHD May 2015Document23 pagesSudden Maternal Collapse: Max Brinsmead MB Bs PHD May 2015DrChauhanNo ratings yet
- 2 EclampsiaDocument17 pages2 EclampsiaDrMohammad KhadrawyNo ratings yet
- Chest Pain, Bradycardia, & Cardiac Dysrhythmias.: Oxygen As An Emergency DrugDocument11 pagesChest Pain, Bradycardia, & Cardiac Dysrhythmias.: Oxygen As An Emergency DrugMin Hong LuoNo ratings yet
- Management of Eclampsia: Baha M. SibaiDocument9 pagesManagement of Eclampsia: Baha M. SibaiPiyawan Fern YodpetchNo ratings yet
- 288 Paediatric Anaesthetic Emergencies Part 2Document6 pages288 Paediatric Anaesthetic Emergencies Part 2Maaida MuzaffarNo ratings yet
- 288 Paediatric Anaesthetic Emergencies Part 2 (1) - 0Document6 pages288 Paediatric Anaesthetic Emergencies Part 2 (1) - 0Parvathy R NairNo ratings yet
- Quote For RSDODocument1 pageQuote For RSDOChristine Notoningtiyas SantosoNo ratings yet
- Wo 9122 25 - 31 Agustus 2014Document6 pagesWo 9122 25 - 31 Agustus 2014Christine Notoningtiyas SantosoNo ratings yet
- Nama:Hanes Andriani T.P/F3212037/M.P.B/Upt B Andika KurniawanDocument5 pagesNama:Hanes Andriani T.P/F3212037/M.P.B/Upt B Andika KurniawanChristine Notoningtiyas SantosoNo ratings yet
- Brestfeeding Defense ObesityDocument4 pagesBrestfeeding Defense ObesityChristine Notoningtiyas SantosoNo ratings yet
- Burn Injury Decreases Myocardial Na-K-Atpase Activity: Role of PKC InhibitionDocument9 pagesBurn Injury Decreases Myocardial Na-K-Atpase Activity: Role of PKC InhibitionChristine Notoningtiyas SantosoNo ratings yet
- 6 Thrombosis MorphologyDocument20 pages6 Thrombosis MorphologySawera RaheemNo ratings yet
- A Pulmonary EmbolismDocument11 pagesA Pulmonary EmbolismMonica Damayani SusiloNo ratings yet
- General Pathology NotesDocument29 pagesGeneral Pathology NotesMohd Syaiful Mohd ArisNo ratings yet
- StreptokinaseDocument4 pagesStreptokinaseAfiqah So Jasmi100% (1)
- Advances in The Management of Cardioembolic Stroke Associated With Patent Foramen OvaleDocument18 pagesAdvances in The Management of Cardioembolic Stroke Associated With Patent Foramen OvaleRaul De Sousa RamosNo ratings yet
- SYROKE - Bare EssentialsDocument11 pagesSYROKE - Bare EssentialsPaula Vergara MenesesNo ratings yet
- MCQ On Disorder of RBCS: Group (4) PresentsDocument6 pagesMCQ On Disorder of RBCS: Group (4) PresentsIrekton GGNo ratings yet
- Contraindications of MassageDocument44 pagesContraindications of MassageBhargav100% (1)
- Pathology Slides 1Document28 pagesPathology Slides 1SydNo ratings yet
- Icd 10Document170 pagesIcd 10Silverius Seantoni SabellaNo ratings yet
- Nursing Care Plan - FractureDocument2 pagesNursing Care Plan - Fracturederic95% (19)
- 1275 Transient Ischemic Attack Secondary To Air Embolism From Right Radial Catheter, Crit Care MedDocument1 page1275 Transient Ischemic Attack Secondary To Air Embolism From Right Radial Catheter, Crit Care MedGojko GošovićNo ratings yet
- A Systematic Literature Review of The Middle Temporal Vein Anatomy Venous Danger Zone' in Temporal Fossa For Filler Injections - Kapoor, 2020Document8 pagesA Systematic Literature Review of The Middle Temporal Vein Anatomy Venous Danger Zone' in Temporal Fossa For Filler Injections - Kapoor, 2020Rafael Autran Cavalcante AraújoNo ratings yet
- Cardioembolic Stroke DefinitionDocument3 pagesCardioembolic Stroke DefinitionJanel TamNo ratings yet
- Nur 111 Session 2 Sas 1Document10 pagesNur 111 Session 2 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Case Study - Respiratory SystemDocument1 pageCase Study - Respiratory SystemMongMouaNo ratings yet
- Disturbances of Blood CirculationDocument59 pagesDisturbances of Blood Circulationсветлый поповNo ratings yet
- Pathology: Fluid & Hemodynamic Derangement - MCQDocument5 pagesPathology: Fluid & Hemodynamic Derangement - MCQahmed jaradNo ratings yet
- Pathophysiology Exam QuestionsDocument11 pagesPathophysiology Exam Questionsjimmy100% (2)
- EmbolismDocument11 pagesEmbolismSubhrajyoti RoyNo ratings yet
- 1996 Bookmatter InternalMedicineDocument117 pages1996 Bookmatter InternalMedicineMenna GalalNo ratings yet
- Autopsy in The Event of Maternal Death - A UK Perspective: ReviewDocument8 pagesAutopsy in The Event of Maternal Death - A UK Perspective: ReviewMayada OsmanNo ratings yet
- Practice Essentials of Pulmonary ThromboembolismDocument39 pagesPractice Essentials of Pulmonary ThromboembolismEzzat Abdelhafeez SalemNo ratings yet
- CDC/NHSN Surveillance Definitions For Specific Types of InfectionsDocument30 pagesCDC/NHSN Surveillance Definitions For Specific Types of InfectionssofiaNo ratings yet
- Pulmonary Embolism: Here Is Where Your Presentation BeginsDocument39 pagesPulmonary Embolism: Here Is Where Your Presentation BeginsAsmaa ahmedNo ratings yet
- Diagnosa & Tindakan 2013Document614 pagesDiagnosa & Tindakan 2013susiariniNo ratings yet
- EmbolismDocument2 pagesEmbolismShannen Joyce FloresNo ratings yet
- Англ тести фармDocument138 pagesАнгл тести фармRodriguez Vivanco Kevin DanielNo ratings yet
- Kami Export - Cardiovascular System Lecture Outline 1st PeriodDocument16 pagesKami Export - Cardiovascular System Lecture Outline 1st PeriodJada NovakNo ratings yet
- Fungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportDocument5 pagesFungal Origin of in Situ Pulmonary Artery Thrombosis: A Case ReportIJAR JOURNALNo ratings yet