Professional Documents
Culture Documents
2004-SCI-029 Commissioning Cataract Surgery
Uploaded by
abuahmed&jana0 ratings0% found this document useful (0 votes)
18 views5 pagesA number of contracts have been awarded to independent providers to undertake elective cataract surgery. The care of patients already on the waiting list of a local consultant ophthalmologist has been transferred to an alternative provider without the knowledge of the local consultant.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA number of contracts have been awarded to independent providers to undertake elective cataract surgery. The care of patients already on the waiting list of a local consultant ophthalmologist has been transferred to an alternative provider without the knowledge of the local consultant.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views5 pages2004-SCI-029 Commissioning Cataract Surgery
Uploaded by
abuahmed&janaA number of contracts have been awarded to independent providers to undertake elective cataract surgery. The care of patients already on the waiting list of a local consultant ophthalmologist has been transferred to an alternative provider without the knowledge of the local consultant.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
The Royal College of Ophthalmologists
Commissioning Cataract Surgery an Outline of Good Practice
Background
The NHS Plan
1
set out a ten year strategy aimed at building a more responsive and
more patient-centred NHS with more uniform standards of care and access. Central
to the strategy was a staged reduction in the time that patients wait for surgery down
to six months in 2005 and eventually, three months. Similar targets have also been
introduced for waiting times for routine outpatient appointments.
The government initiative: Action on Cataracts (Department of Health 1999) made an
attempt to address the issue of capacity for cataract surgery by investment in
infrastructure (though not manpower) in NHS ophthalmic units across the country,
aimed at increasing throughput. The NHS Plan recognized that a considerable
expansion in the consultant workforce would also be required if the targets for
waiting times for elective surgery in the NHS Plans were to be met. Despite an
increase in the number of UK Medical School places, it will be a number of years
before this translates into a corresponding increase in the number of fully trained
specialists emerging from surgical training programmes.
A further Government paper
2
paved the way for a rapid increase in elective surgical
capacity by commissioning overseas surgical teams to perform elective surgical
procedures either within NHS premises or in independent facilities. A number of
contracts have since been awarded to independent providers (mostly but not
exclusively from outside the UK) to undertake elective cataract surgery. Primary
Care Trusts will be required to offer patients who have been referred for cataract
surgery a choice of provider.
In the days of general practice fund-holding, the outsourcing of cataract surgery to
distant NHS providers or the private sector was not uncommon, but was normally
instigated by the GP in discussion with the patient. Since the end of GP fund-
holding, block contracts between commissioning agencies and providers have
become the norm, and the College has received a number of reports of cases where
the care of patients already on the waiting list of a local consultant ophthalmologist
has been transferred to an alternative provider without the knowledge of the local
consultant, and sometimes without the prior knowledge of the patient. In some
cases, patient care has been compromised either because of inappropriate selection
of cases for transfer, or because of inadequate arrangements for post-operative
follow-up (especially where complications have occurred).
Potential problems of outsourcing cataract surgery
Leaving aside the political controversies surrounding the outsourcing of surgical
procedures (especially from the private sector and abroad), there are a number of
practical problems which may arise from this practice. A number of examples of
these problems have been brought to the attention of this College in recent years;
Problems for the patient:
Travel to a more distant provider may be difficult, and adequate follow
up care may difficult to arrange.
There may be little or no opportunity for the patient to discuss their
operation with the surgeon before the day of surgery, and the patient
may feel an obligation to proceed if they feel that special arrangements
have been made for their treatment.
Problems for the provider
It may be difficult to obtain relevant information about the patients
previous history (eg adverse reactions to previous treatment, ongoing
medical or ophthalmic problems), leading to unexpected difficulties
with surgery.
If complications occur, it may be difficult to provide treatment or
adequate follow up if the patient lives some distance away.
Problems for the local eye unit
If a significant proportion of cataract surgery is cherry picked by other
providers, the workload of the local unit may be distorted, with potential
adverse effects on training, skill-retention, recruitment and retention of
staff
The local unit may have to make urgent arrangements to deal with
postoperative complications from surgery performed by a distant
provider, without adequate background information. This is a
particularly potent source of resentment, and poses a threat to patient
safety.
Problems for the commissioning agency
The commissioning agency has a duty of care to the patient when
placing a contract for their surgery and may share legal liability with the
provider for failings in the standard of care, particularly if monitoring of
the contract is shown to be inadequate, or if the provider is based
outside British legal jurisdiction
It may be difficult to obtain or validate information on standards of care
and outcomes from providers prior to placing a contract.
Purpose of this document
General guidelines for NHS employers who plan to commission and use overseas
clinical teams have recently been circulated in the form of a consultation document
3
.
The primary purpose of this document is not to deter commissioning agencies from
placing contracts for cataract surgery with providers other than their local NHS eye
unit, but rather to provide guidance on the standards which commissioning agencies
should expect of any provider of ophthalmic care, whether in the NHS, in
Independent Sector Treatment Centres or abroad, with whom they plan to place
contracts for cataract surgery.
Recommendations
1. Communication. The provider should inform the patients general
practitioner at the points when the patient is listed for surgery, when the
surgery occurs and when the patient is discharged. Where a patient is under
the ongoing care of another ophthalmologist, he/she should also be copied
into the correspondence. The provider is responsible for arranging handover
of care to another ophthalmologist where this is necessary (eg for
management of a complication or where ongoing monitoring of another eye
condition is required). Where a commissioning agency arranges transfer of
patients already on the waiting list of a consultant ophthalmologist to an
alternative provider, the agency is responsible for obtaining the consent of the
patient, and should inform the consultant from whose list the patient is being
removed, and the patients general practitioner (L Donaldson, personal
communication, 14 November 2001).
2. Case selection and preoperative preparation. The provider must perform a
detailed preoperative assessment to ensure that case selection is appropriate
to the level of expertise of the operating team and the clinical facilities. In
particular, it is vital to take adequate account of ocular or systemic co-
morbidity which might increase the technical difficulty of the procedure, or
increase the risk of complications. The provider should also ensure that
adequate account is taken of the patients social circumstances (availability of
transport, help at home etc) when planning the episode of care.
3. Patient information and consent. The provider is responsible for providing
adequate verbal and / or written information about cataract and cataract
surgery to allow the patient to give informed consent to the procedure.
Informed consent must be taken by someone who has the knowledge and
competence to explain the benefits and risks of the procedure and to provide
accurate answers to questions. Although NHS patients do not have a right to
choose their surgeon, they have a right to expect that their surgeon has the
experience and skill to perform their operation. It is reasonable that the
patient should have the opportunity to know the identity and qualifications of
the operating surgeon and to meet him / her prior to entering the operating
theatre. It is the final responsibility of the operating surgeon (or the
supervising surgeon where the operating surgeon is a trainee) to ensure that
the patient has been adequately assessed, prepared and consented prior to
the start of the operation.
4. Hotel Facilities The commissioning agency and the provider have a joint
responsibility for ensuring that the adequate facilities are available for the
patient to be accommodated for the duration of the episode of care. This is
particularly important where the provider unit is too distant from the patients
home to allow a return journey in the same day.
5. Clinical facilities. The commissioning agency and the provider have a joint
responsibility to ensure that the premises and equipment in the provider unit is
adequate for performing modern small incision cataract surgery safely, and
that the unit complies with relevant legislation.
6. Anaesthesia and perioperative care. Most cataract surgery is carried out
under local anaesthesia, and has a very low mortality and systemic morbidity,
especially considering that a high proportion of patients are elderly and would
be graded as 2 or worse on the American Society of Anaesthetists (ASA)
scoring system. However, the provider has a responsibility to ensure that
resuscitation facilities are readily available, and that an appropriately qualified
person is readily available to undertake resuscitation should the need arise.
Contingency plans should be in place for emergency transfer of patients who
suffer a life-threatening complication. The National Confidential Enquiry into
Perioperative Deaths (NCEPOD) has criticized the practice of undertaking
ophthalmic surgical procedures on very unfit patients in isolated units.
Provider units which are geographically isolated from accident and emergency
or intensive care facilities should give particular consideration to contingency
planning for life-threatening emergencies and to case selection.
7. Postoperative care and contingency planning for complications. The
provider is responsible for arranging routine postoperative care following
cataract surgery, in order to monitor for postoperative complications and for
the collection of information on outcomes. The patient must be provided with
any necessary postoperative medication and instructions, and a discharge
summary. The provider unit must have adequate arrangements for handling
urgent enquiries from patients who have had surgery. It is not acceptable for
patients merely to be told to go to their local accident and emergency
department or to contact their GP if they have a problem. If operative or
postoperative complications occur, the provider unit should either manage
them, or arrange direct referral to another specialist, keeping the general
practitioner informed. The commissioning agency should ensure that there is
a funded agreement in place with a suitably equipped NHS facility with
adequate capacity for dealing with any early or late post-operative
complications which cannot be managed by the provider.
8. Clinical Governance. The commissioning agency should ensure that the
provider unit follows the requirements of Clinical Governance, whether the
provider is within the NHS or the private sector. In particular, medical staff
should undergo annual peer appraisal, there should be evidence of ongoing
audit of outcomes and complications in relation to national comparators, there
should be a robust mechanism for recording and acting on complaints and
clinical incidents, and there should be facilities for monitoring the progress of
staff in training.
9. Accreditation of private healthcare providers. From 31
st
March 2002, it is
a requirement that doctors and establishments engaged entirely in private
practice must register with the National Care Standards Commission. The
commissioning agency has a responsibility to ensure that a private healthcare
provider with whom they contract is registered, or can demonstrate
exemption.
References:
1: The NHS Plan, a plan for investment, a plan for reform. Department of Health,
J uly 2000.
2. Growing Capacity: a new role for external healthcare providers in England.
Department of Health, J une 2002.
3. Code of Practice and Guidance for NHS employers commissioning and using
overseas teams. Department of Health, February 2004
Further sources of information:
Cataract Surgery Guidelines. Royal College of Ophthalmologists.
Department of Health website: www.dh.gov.uk
Seeking patients consent: the ethical considerations. General Medical Council
November 1998
Good Medical Practice. General Medical Council. May 2001.
Revised 2004
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Usg B SCANDocument11 pagesUsg B SCANabuahmed&janaNo ratings yet
- Ophthalmology - Passmedicine 2012 - 62013146Document18 pagesOphthalmology - Passmedicine 2012 - 62013146abuahmed&janaNo ratings yet
- MnemonicS in OphthaDocument22 pagesMnemonicS in Ophthaabuahmed&janaNo ratings yet
- Infinity Tower, Dubai, UAEDocument10 pagesInfinity Tower, Dubai, UAEryan rakhmat setiadiNo ratings yet
- Natural Gas DistributionDocument46 pagesNatural Gas DistributionscribdmisraNo ratings yet
- AutoPIPE Tutorial PDFDocument156 pagesAutoPIPE Tutorial PDFdhaktodesatyajitNo ratings yet
- Enzyme Kinetics Principles and MethodsDocument268 pagesEnzyme Kinetics Principles and MethodsCarlos Carinelli100% (4)
- Geometrical Optics.Document58 pagesGeometrical Optics.abuahmed&janaNo ratings yet
- Bus Bar Arrangement of SubstationDocument17 pagesBus Bar Arrangement of SubstationBbimafidon_248613673No ratings yet
- HLX 150Document44 pagesHLX 150menendez2050100% (1)
- People Vs SB - Paredes - Ex Post FactoDocument2 pagesPeople Vs SB - Paredes - Ex Post FactoMara Aleah CaoileNo ratings yet
- Overseas Calendar 2011 V3Document4 pagesOverseas Calendar 2011 V3abuahmed&janaNo ratings yet
- Classification of OA: A. BroadlyDocument1 pageClassification of OA: A. Broadlyabuahmed&janaNo ratings yet
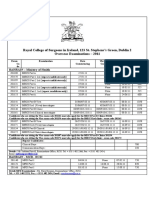
- Examinations Calendar Dublin 2Document3 pagesExaminations Calendar Dublin 2abuahmed&janaNo ratings yet
- Systemic Diseases With RPDocument1 pageSystemic Diseases With RPabuahmed&janaNo ratings yet
- TheHaigisFormula PDFDocument2 pagesTheHaigisFormula PDFabuahmed&janaNo ratings yet
- Anterior Segment Complications of Cataract Surgery: Chapter - 8Document19 pagesAnterior Segment Complications of Cataract Surgery: Chapter - 8abuahmed&janaNo ratings yet
- Kanski Picture Test AnswersDocument2 pagesKanski Picture Test Answersabuahmed&jana100% (2)
- Done By: DR Al - Zahraa El-Sayed El Sherbiny Supervised By: DR Eman Abd El RaoffDocument23 pagesDone By: DR Al - Zahraa El-Sayed El Sherbiny Supervised By: DR Eman Abd El Raoffabuahmed&janaNo ratings yet
- Internship Proposal FormDocument3 pagesInternship Proposal FormMuhammad FidaNo ratings yet
- Markets and Commodity Figures: Total Market Turnover StatisticsDocument6 pagesMarkets and Commodity Figures: Total Market Turnover StatisticsTiso Blackstar GroupNo ratings yet
- Admission Sos 2013-14090513 PDFDocument21 pagesAdmission Sos 2013-14090513 PDFmanoj31285manojNo ratings yet
- Business Mathematics 11 Q2 Week3 MELC20 MELC21 MOD Baloaloa, JeffersonDocument25 pagesBusiness Mathematics 11 Q2 Week3 MELC20 MELC21 MOD Baloaloa, JeffersonJefferson BaloaloaNo ratings yet
- RLB Procuring For Value 18 July PDFDocument56 pagesRLB Procuring For Value 18 July PDFDaniel LixandruNo ratings yet
- Downtown SLO Business Owners Ask City Council To Consider Parking ChangesDocument4 pagesDowntown SLO Business Owners Ask City Council To Consider Parking ChangesKaytlyn LeslieNo ratings yet
- A Gandhari Version of The Rhinoceros Sutra - Salomon.thieuDocument29 pagesA Gandhari Version of The Rhinoceros Sutra - Salomon.thieuTRAN NGOCNo ratings yet
- TaxationDocument26 pagesTaxationReynamae Garcia AbalesNo ratings yet
- CREW Whitaker Recusal Letter DOJ 11-8-2018Document9 pagesCREW Whitaker Recusal Letter DOJ 11-8-2018Beverly TranNo ratings yet
- SwahiliDocument7 pagesSwahiliMohammedNo ratings yet
- Content Kartilya NG Katipunan: Kataastaasan, Kagalanggalangang Katipunan NG Mga Anak NG Bayan)Document6 pagesContent Kartilya NG Katipunan: Kataastaasan, Kagalanggalangang Katipunan NG Mga Anak NG Bayan)AngelaNo ratings yet
- 1.4 Creating Graphic OrganizerDocument1 page1.4 Creating Graphic OrganizerTrixie Roselle Y. MesiasNo ratings yet
- Material Safety Data Sheet: Manufacturer Pt. Bital AsiaDocument3 pagesMaterial Safety Data Sheet: Manufacturer Pt. Bital AsiaediNo ratings yet
- Clause: Extra Element + Independent Clause Dependent ClauseDocument1 pageClause: Extra Element + Independent Clause Dependent ClauseTieng HuangNo ratings yet
- Lubi Dewatering PumpDocument28 pagesLubi Dewatering PumpSohanlal ChouhanNo ratings yet
- Sen Çal KapımıDocument9 pagesSen Çal KapımıMa Gabriela Ojeda CasellaNo ratings yet
- ABC LTD ProposalDocument4 pagesABC LTD ProposalAbhishek JurianiNo ratings yet
- Expanding The Product Range of Leena by Bata (Report)Document104 pagesExpanding The Product Range of Leena by Bata (Report)Rabya TauheedNo ratings yet
- Agmt - Spa Schedule HDocument20 pagesAgmt - Spa Schedule Hapi-340431954No ratings yet
- CALDER New Research On Low-Frequency Membrane AbsorbersDocument11 pagesCALDER New Research On Low-Frequency Membrane AbsorbersAndre VareNo ratings yet
- SSP 861603 - EN - Tire Pressure Monitoring SystemsDocument42 pagesSSP 861603 - EN - Tire Pressure Monitoring Systemsa.diedrichsNo ratings yet
- Resume Relevant CourseworkDocument5 pagesResume Relevant Courseworkdkcvybifg100% (2)
- Activity 9 Let's Check and Let's AnalyzeDocument3 pagesActivity 9 Let's Check and Let's AnalyzeJean Tronco100% (5)