Professional Documents
Culture Documents
1819 04
Uploaded by
Vaithya Nathan0 ratings0% found this document useful (0 votes)
29 views18 pagesll
Original Title
1819_04 (1)
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentll
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views18 pages1819 04
Uploaded by
Vaithya Nathanll
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 18
Current Cancer Drug Targets, 2007, 7, 541-558 541
1568-0096/07 $50.00+.00 2007 Bentham Science Publishers Ltd.
Myelodysplastic Syndromes: Review of Pathophysiology and Current Novel
Treatment Approaches
E.D. Warlick* and B.D. Smith
Hematologic Malignancies Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins 1650 Orleans Street, room 246
Baltimore, MD 21231, USA
Abstract: Myelodysplastic syndromes (MDS) are a heterogeneous group of clonal disorders of hematopoietic progenitors manifest by
cytopenias, bleeding, infection, and potential for progression to acute myelogenous leukemia. The wide spectrum of clinical
manifestations, including variability in illness severity and potential for progression, suggest that myelodysplastic syndromes encompass
a multitude of disorders, likely involving numerous pathologic pathways. In fact, it is the effort to understand the underlying biology of
these syndromes that has led to recent advances in treatment approaches, including the FDA approval of three new agents (5-azacitidine,
decitabine, and lenalidomide) for the treatment of MDS. This review will present data supporting each of the current pathophysiologic
pathways implicated in the development and progression of MDS; summarize the emerging clinical paradigms for treating patients with
MDS; and offer insights into several novel approaches attempting to improve treatment options for future MDS patients.
Keywords: Myelodysplastic syndrome, pathophysiology, differentiation therapy, epigenetic therapy, bone marrow transplantation,
immunomodulation.
INTRODUCTION
Myelodysplastic syndromes (MDS) are a complex and
heterogeneous group of bone marrow failure disorders characterized
by ineffective hematopoiesis. This dysfunctional blood cell
production is manifest by peripheral cytopenias, marked morphologic
dysplasia, and cellular dysfunction resulting in an increased risk of
infection and need for transfusions in most MDS patients. In the
general population, the incidence of MDS is approximately 2-10
cases per 100,000 people with the incidence rising to approximately
50 cases per 100,000 people over age 70 [1]. The median age at
presentation approaches 70 with a slight male predominance of
unknown clinical significance. Traditionally, MDS is characterized as
either primary (idiopathic) or secondary with exposure to benzene
[2], occupational chemicals [3], or prior treatment with radiation [4]
or chemotherapy agents [5] well documented secondary causes.
Additional data implicates exposure to tobacco [6], excessive alcohol
[7], viral infections [8], or autoimmune disorders [9] as potential
associations with MDS.
Alterations in many individual biologic pathways have been
implicated in MDS pathophysiology. However, the generally
accepted primary hypothesizes involves an initial deleterious genetic
event within a hematopoietic stem cell, subsequent development of
excessive cytokines/inflammatory response leading to a pro-
apoptotic/proliferative state, and resultant peripheral cytopenias
despite a hypercellular bone marrow. The presence of detectable
cytogenetic abnormalities in approximately 40-70% of patients with
primary MDS and over 80% with secondary MDS [10] as well as the
validated prognostic value of cytogenetic data in MDS supports the
theory of an incident genetic event. Specifically, good prognostic
cytogenetic groups (5q minus syndrome or deletion of the long arm
of chromosome 20 (20q)) are typically associated with more indolent
MDS that requires less intensive therapy while poor prognostic
cytogenetic groups (loss of chromosome 5 or 7 or complex
abnormalities) have a more aggressive course and are often poorly
responsive even to aggressive treatments [11]. The variable response
to treatment and course of disease correlating with cytogenetic
findings suggests likely differential behavior of the MDS clone:
differentiation arrest and a pro-apoptotic cytokine state in low risk
cytogenetic cohorts versus a state of proliferative advantage, possibly
due to underlying genomic instability or via altered gene expression
silencing of DNA repair or tumor suppressor genes, in high risk
*Address correspondence to this author at the Hematologic Malignancies Sidney Kimmel
Comprehensive Cancer Center at Johns Hopkins 1650 Orleans Street, room 246
Baltimore, MD 21231, USA; Tel: (410) 614-5068; Fax: (410) 614-7437; E-mail:
edahl2@jhmi.edu
cohorts [12-14]. Additionally, altered immune surveillance
potentially creates an environment where the transformation to acute
leukemia becomes possible [15]. The pathophysiology of low and
high grade MDS is slowly being incorporated into the evolving
classification hierarchies as well as treatment paradigms.
CLASSIFICATION SYSTEMS
Throughout the years, various classification systems have been
developed to describe myelodysplastic syndromes. There is no clear
best schema, yet the numerous revisions and expansions based on
the ongoing understanding of MDS pathophysiology and clinical
outcomes are notable improvements.
FAB Morphologic Classification
The initial FAB (French-American British) system was
developed by an international group of clinicians and pathologists in
the mid 1970s, refined in 1982, and primarily used cellular
morphology to define the MDS subgroups focusing on bone marrow
blast percentage, the presence or absence of monocytosis, and the
presence or absence of ringed sideroblasts. These morphologic
findings, aligned with important prognostic outcomes, were
eventually divided into four groups:1) Lower-risk MDS (RA and
RARS) with a median survival of 4-5 years and low risk of AML
transformation; 2) Intermediate-risk MDS (RAEB) with a median
survival close to 1 year; 3) Higher-risk MDS (RAEBt) with a median
survival measured in months and a very high risk of AML
transformation; and 4) CMML associated with a wildly variable risk
[16,17]. The FAB classification served as the first framework to
systematically identify and describe the different clinical entities of
MDS. However, the FAB system was limited by lack of cytogenetic
and molecular information now commonly available, and did not
adequately accommodate hypoplastic MDS, MDS with
myelofibrosis, and other overlap syndromes [18, 19].
WHO Classification
More recently, in 1999, the World Health Organization (WHO)
proposed a newer classification system attempting to address some of
the limitations of the FAB system [20]. The main goal of this schema
was to formally incorporate biologic data, specifically cytogenetic
and molecular findings, clinical outcomes, and number of dysplastic
lineages involved, in order to better separate subgroups and delineate
syndromes within the previous FAB classification. Notably, the
WHO classification recognized the unique 5q- syndrome and
CMML within their own categories, lowered the blast percentage
defining AML to 20% and eliminated the RAEBt category, assigned
542 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
patients with characteristic AML-associated chromosomal
abnormalities to AML regardless of blast percentage, and used the
percentage of marrow blasts to divide RAEB into two groups noting
that patients with >10% blasts had a shorter survival and increased
transformation to acute leukemia compared to patients with <10%
[20]. The WHO system also distinguished MDS patients with <5%
marrow blasts between those with multilineage dysplasia (worse
outcome) and those with erythroid-only dysplasia (better outcome),
and added an unclassifiable MDS category [19-21]. Although the
WHO classification system built on the FAB foundation by including
important biologic and clinical data, there remained some obvious
shortcomings such as the MDS-unclassifiable category and
controversies such as the elimination of RAEBt [18]. These concerns
epitomize the larger problem that MDS is truly a pleomorphic
grab bag term for multiple disorders that offer significant
challenges to both physicians treating patients as well as scientists
studying these disorders.
IPSS Prognostic Classification
In 1997, Peter Greenberg and colleagues proposed a plan to
combine known prognostic variables with outcomes data from seven
large, risk-based studies in an effort to determine the most important
variables for assigning prognosis to MDS patients. The International
Prognostic Scoring System (IPSS) emerged from the analysis of this
data from nearly 900 MDS patients and represents the best effort to
date for prediction of prognosis and outcome. The variables most
predictive of prognosis included percentage bone marrow blasts,
cytogenetic abnormalities, and number of peripheral cytopenias.
Subsequent IPSS score calculation then assigns patients to one of four
risk groups: Low, Intermediate-1 (INT-1), Intermediate-2 (INT-2),
and High risk with decreasing survival and increasing risk of AML
progression as the score increases [22]. Like each of the classification
schemas, the IPSS also has limitations including failure to offer
prognostic points for treatment-related MDS (t-MDS) or CMML, and
lack of scoring for most of the cytogenetic abnormalities commonly
found in MDS. These limitations aside, the IPSS remains a
paramount tool in predicting prognosis, categorizing patients for
studies, and analyzing treatment outcomes. In combination with the
other classification systems, it represents the most quantitative
assignment of MDS risk available.
THEORIES IN MDS PATHOPHYSIOLOGY
Better understanding of the underlying MDS biology is crucial
for the development of better treatments for individual patients. It is
commonly accepted that MDS develops through a multi-step process
encompassing changes within the hematopoietic stem cell, the bone
marrow microenvironment, and the complex interactions between the
two [1, 15, 18, 23, 24]. Below we survey specific theories and
pathways implicated in the pathogenesis and progression of MDS
divided into five major categories: 1) cellular damage related to toxic
environmental exposures and cellular aging; 2) genetic alterations
including loss or gain of function due to both cytogenetic and
epigenetic abnormalities (Table I); 3) changes in the bone marrow
microenvironment; 4) dysregulation of the immune system; and 5)
altered cell cycle regulation and blocked differentiation. (Theories
Summarized in Table II)
Cellular Damage: Toxic Environmental Exposures and Cellular
Aging
The epidemiology of MDS has offered pivotal links between
various environmental exposures, aging, and the development of
disease, namely the accumulation of DNA damage. Numerous
environmental exposures have been associated with the development
of MDS including tobacco [6] and alcohol use [7], infections [8], or
auto-immune disorders [9]; however, the classic example linking an
environmental toxin exposure to MDS development is highlighted
from the observational case control studies involving benzene, an
aromatic hydrocarbon and organic solvent derived from petroleum-
refining, used in many occupational compounds [25]. The
association, first described in Turkish shoe workers who developed
bone marrow failure/pancytopenia states, [26] lead to further
prospective cohort studies involving 74,828 benzene exposed subjects
in China and revealed a significantly increased relative risk of MDS
development approaching infinity [2]. The potential mechanisms of
MDS development in benzene-exposed individuals have been
described in two contexts: genotoxic and non-genotoxic. Genotoxic
mechanisms are characterized by the generation of oxygen free
radicals from benzene metabolites with subsequent DNA damage and
apoptosis [27, 28]. Support for this mechanism includes the findings
of chromosomal abnormalities (trisomy (+9), deletions (-5 or -7) and
translocations [t (8, 21)]), oncogene mutations, and somatic mutations
in benzene-exposed MDS patients [29-31]. Additionally, as
increasing somatic mutations may occur with aging, exposure to
benzene and other directly genotoxic agents could lead to more
significant damage that progresses to clonal expansion and MDS
[31]. Suggested non-genotoxic mechanisms include alteration of the
bone marrow microenvironment and immune function through
reduced immunoglobulin and complement levels [31].
Radiation and prior chemotherapy are other well documented
exposures that can lead to the development of MDS [24, 23, 31].
Specifically, chemotherapy-associated MDS has been associated with
treatment using Topoisomerase II inhibitors, anthracyclines, and
alkylating agents. MDS from exposure to Topoisomerase II inhibitors
and anthracyclines typically has an early onset within 1-3 years and
causes balanced genetic alterations typically involving 11q23 (Mixed
Lineage leukemia, MLL gene) [5] while exposure to alkylating agents
results in a later onset within 5-10 years and yields unbalanced
chromosomal alterations often involving chromosomes 5 and 7 [10,
32]. With regard to radiation, epidemiologic studies of atomic bomb
survivors have illustrated the connection between previous radiation
exposure and leukemia/MDS development, [33] and have
characterized the importance of exposure dose and duration [34].
Specific effects and chromosomal abnormalities, additionally, seem
to be similar to those seen with exposure to alkylating agents [4].
With a median age of newly diagnosed MDS patients nearing 70,
the importance of aging in MDS is clear, yet the specific role it plays
biologically remains under investigation [1]. It is theorized that aging
itself may produce increased genetic mutations and alterations that
result in MDS. Comparing bone marrow from normal controls and
older patients is one approach to highlighting potential similarities
and differences that could explain the increased incidence of MDS in
the elderly. Ogawa et al. evaluated the bone marrows of 100 normal
controls of a variety of ages [35] and found increased apoptosis and
decreased cellularity in patients of advanced age [36] with apoptosis
levels similar in degree to MDS patients. Other studies describing
MDS marrows detail a skew in specific TNF-alpha receptor
expression leading to increased rates of apoptosis comparable to that
seen in normal elderly marrows. While the increased apoptosis in
both normal elderly marrows and MDS patients may have distinct
biologic causes, the finding may also suggest a reason for the
preponderance of increased MDS in the elderly [37].
Another biologic link between aging, stem cell damage, and
cancers such as MDS includes the study of telomeres and telomerase
activity. Telomeres are simple tandem repeats at the ends of
chromosomes in somatic cells that shorten with age and are also
found to be shortened in many cancers [38-40]. The shortening is
theorized to result from incomplete DNA replication leading to
genomic instability, subsequent chromosomal abnormalities, and
eventual mutations impacting disease progression once a certain
threshold is breeched. Telomerase is the enzyme required for the
replication of telomeres, and although not typically found in most
somatic cells, has been found in over 85% of primary malignancies
[41]. Telomerase may not be required for initiation of malignancy but
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 543
Table I. Cytogenetic Abnormalities in MDS
Chromosomal
Alteration
Incidence
(Approximate)
Associations: Exposures /
Other Disorders
Classic Clinical or
Morphologic
Description
Prognostic Impact Research
Chromosome 5
Abnormalities
- 10-20% de novo MDS
cases
- Tx-related in 40% of cases
[31]
-Chemical Exposure
-Chemotherapy [49]
Clinical:
-5q Minus Syndrome =
macrocytic anemia, nl
platelet count, female
predominance [50]
- 5q alone/5q syndrome =
good/low risk of AML
transformation [47, 50,
51]
- Complex / other abn of
5 / t-MDS = poor
prognosis
- 5q CDS: genes for
cell cycle & cellular
cytokine receptors
- No specific gene loss
yet identified [52-57]
Deletion 20q
- 5% de novo MDS cases
- Tx-related in 7% of cases
[11]
Polycythemia Vera [58]
Morphologic:
Dyserythropoiesis [58]
Clinical:
! freq. in low-risk dz,
longer survival: low
progression to AML [59]
- Isolated 20q = good
outcomes
- 20q del + complex =
poor outcome [22]
- CDS (20q11.2-q12)
contains numerous
tumor suppressor genes
[11, 58, 60, 61]
- No specific gene loss
yet identified
Loss of Y
Associated w/ not diagnostic
of MDS [58]
- Numerous cancers
- Normal Aging population
[11, 58]
Favorable prognosis if
isolated abn [22]
Chromosome 7
abnormalities
-5% de novo MDS cases
- Tx-related in 55% of cases
[11]
Associated w/ AML, MDS,
NF-1, Fanconis anemia,
Downs Syndrome [62]
Poor risk dz w/ high
progression to AML [63,
58]
- Monosomy 7
uniformly bad
regardless of dz
- CDS (7q22 and 7q32-
33) found but often full
7 loss so difficult to
study [64, 62]
17p Syndrome
- 5% of MDS cases [58]
- Tx-related in 33% of cases
[65]
Morphologic:
Dysgranulopoiesis, pseudo-
pelger huet cells,
hypogranularity [48]
- Often tx related = poor
prognosis
- Often seen w/ other abn
(5 and 7) = poorer
prognosis [11, 58, 65]
- Loss of p53 function
- Due to point mutation
in p53 at 17p13 in 70%
pts [58]
Trisomy 8
- 10-15% of MDS cases [58]
- Sole abn. in 10% of cases
[49]
- AML/MDS
- Linked to Benzene
exposure
- Solid Tumors: Breast,
Colon, Sarcoma [66]
Morphologic:
MDS with monocytic
component [58]
- Isolated = Intermediate
Prognosis [22]
- Not specifically linked
with FAB class/ AML
progression [11]
-High incidence in
MDS but not sufficient
for leukemogenesis
alone [49]
3q Abnormalities
-2% of MDS cases [58]
- Typically tx-related [58]
Morphologic:
Abn megakaryocytic
development
Clinical:
Retained platelet count
-EVI-1 gene (3q26)
alterations:
- Interference w/ 3q26
transcription linked w/
abnormal
differentiation: may
interfere w/ GATA-1,
(erythrocyte
differentiation) [58]
Complex Cytogenetics
- 10-20% of de novo MDS
cases
- Tx-related in 90% [67]
Only partial correlation
w/ outcome: poor
prognosis [67]
Oncogene/Tumor
Suppressor
Abnormalities
Oncogene/Tumor
Suppressor Function
Frequency of
Abnormality in MDS
Patients
Specifics of Abnormality Prognostic Implications Research
11q23/MLL Gene
Abnormality
MLL fusion products
involved in numerous cell
functions: precise oncogenic
mechanism still poorly
understood [68]
- 5% of MDS cases [58]
- often tx-related [32]
Clinical:
Typically later stage dz,
high AML transformation,
shorter survival
[69,11]
- Forms numerous fusion
protein pairs
Assoc. w/ other abn:
Complex, 5 and 7 [69]
- MLL Amplification:
role in oncogenic
changes
-Gain of function via
HOX9A expression
found [70]
- absent in de novo
MDS [71]
Ras Family of genes encoding
GTP-binding proteins: role
in signal transduction
-Paquette Study of 220
MDS Pts 9% w/ n-ras
mutations [72]
- Point Mutations [73]
-N-ras mutations assoc.
w/ shorter survival and
increased progression to
AML [72]
-Study showing 70% of
pts w/ mutation
progressed to AML w/i
2 yrs compared to
control [72]
p53 Control of DNA replication
repair: crucial for
maintaining genome [74]
- In 69% of pts w/ 17p
deletion [75]
- ! p53 mutations in 17p +
complex cytogenetics [76]
-In t-MDS often found w/
chromosome 5 abn and
complex cytogenetics [65]
- Not usually assoc. w/
chromosome 7 abn [32]
-Resistance to chemo:
shorter survival: Shorter
time to leukemia
development [76, 77]
Legend: MDS = Myelodysplastic Syndrome; Tx = treatment; Nl = normal; AML = Acute Myelogenous Leukemia; t-MDS = treatment related MDS; CDS = Commonly Deleted Segment; w/ = with; Freq. = frequency;
Del = deletion; Abn = abnormality; NF-1 = neurofibromatosis 1; Dz = Disease; FAB = French American British; Assoc. = Associated; MLL = multi-lineage leukemia; Pts = patients; w/i - within
544 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
\may be important in tumor propagation [42]. Interestingly,
telomerase activity is found in cell populations with high renewal
requirements such as hematopoietic stem cells [43]. In MDS, studies
evaluating telomeres and telomerase activity show loss of the typical
correlation between telomere length and age: specifically, decreasing
telomere length with increasing age [44]. Further studies have found
an association between shortened telomeres and abnormal
cytogenetics, where progressively shortening telomeres correlated
with worsening IPSS risk group [44]. Telomerase activity has also
been assessed in MDS: high levels of activity have not commonly
been found. The culmination of this data may suggest that the
hematopoietic stem cells in MDS patients have insufficient
telomerase to adequately restore cellular telomeres to their normal
lengths subsequently resulting in increased genetic instability [44].
Gain or Loss of Gene Expression: Cytogenetic and Epigenetic
Alterations
One of the common end results of exposure to environmental
toxins is DNA damage and the loss or alteration of gene expression.
Yet, chromosomal abnormalities are often detected in MDS that are
not associated with such exposures. In addition, newer techniques,
including comparative genomic hybridization (CGH) and single
nucleotide polymorphisms (SNP) arrays, now allow the detection of
even microscopic deletions of genes and continue to fuel the
understanding of MDS and its pathophysiology. Finally, it is now
clear that epigenetic gene silencing plays a role in loss or gain of gene
expression even when the DNA sequence is completely intact.
Clonal cytogenetic abnormalities (Table I) are found in 30-70%
of patients with primary myelodysplastic syndrome and in over 80%
of treatment-related MDS and remain the most important individual
prognostic tool [11, 45-47]. The majority of the chromosomal
abnormalities in primary MDS involve unbalanced losses: entire
chromosomal loss or point mutations [11, 45]. Consequently, it is
easy to invoke such abnormalities resulting in the loss or inactivation
of a critical tumor suppressor protein; however, efforts to determine a
culprit gene or cluster of genes have been much more difficult.
Characteristic chromosomal abnormalities in MDS include alterations
of chromosomes 5, 7, 8, 11, 17, 20 and Y or complex karyotypes
involving multiple abnormalities within individual clonal populations
[45, 46]. Several of these abnormalities are shared with AML (e.g.,
deletions of chromosomes 5 or 7, trisomy 8, and complex
cytogenetics), while others appear almost exclusively in AML (e.g., t
(15; 17), t (8; 21), and inversion 16) [22]. Although specific
cytogenetic abnormalities within MDS do not typically correlate with
WHO or FAB classifications, it is now clear that there are
characteristic syndromes within MDS, namely 5q- and 17p-
syndromes [47, 48] that have unique clinical and prognostic
outcomes. Additionally, evidence suggests a correlation with
increasing frequency of cytogenetic abnormalities and severity of
disease.
The traditional cytogenetic alterations noted above are typically
evaluated using conventional cytogenetic (CC) techniques that
require adequate metaphase chromosomes for analysis. The
development of newer techniques has allowed investigators to
uncover more subtle genetic alterations that help to reveal further
components of MDS pathophysiology.
Comparative genomic hybridization (CGH) is a useful tool that
can uncover genomic imbalances without the requirement for quality
mitoses or dividing cells. Specifically, it allows for detection of
changes in chromosome copy number by hybridization techniques
between normal and tumor cells [78]. Studies comparing information
obtained through CC, FISH analysis, and CGH, showed close
correlation between the three techniques with CGH providing
additional information on the abnormalities identified by CC as well
as uncovering unbalanced genetic alterations not described by CC
[79, 80]. CGH continues to add valuable information to many
common cytogenetic findings [81, 82].
Identifying alterations of single nucleotide polymorphism (SNPs)
arrays have also been used to help investigators study and explain the
heterogeneity of MDS. Moreover, this technique has led to insights
on genetic predispositions for these diseases. SNPs are the most
common form of genetic variation between individuals, and recent
reports have investigated the possibility that genetic polymorphisms
in genes required for proliferation and differentiation may play a role
in MDS development. Specifically, a GLU785Lys polymorphism in
the G-CSF receptor was described and demonstrated functional
alterations in growth factor responsiveness in high risk MDS patients
suggesting a potential role in MDS pathophysiology [83]. It is likely
that further investigations will reveal pathways impacted by these
subtle changes in gene expression. SNP techniques have also looked
at the possibility that polymorphisms create a genetic predisposition
to MDS. Based on evidence of defective DNA mismatch repair
enzymes in patients with t-MDS and mitochondrial/genetic instability
in patients with primary MDS [84], obvious implicated pathways
could include those involving metabolic activation or detoxification
enzymes. Utilizing both specific and non-specific probes,
polymorphisms in detoxification enzymes such as glutathione S-
transferase [85] as well as in quinone oxidoreductase have been
found, where the presence of NQO1 quinone oxidoreductase
polymorphisms correlated with an increased risk of benzene-related
and treatment-related MDS [86, 87]. Additional investigation has also
shown microsatellite instability (MSI) in treatment-related MDS, a
hallmark of defective DNA mismatch repair [88].
In addition to these structural alternations in DNA, another
mechanism for altered gene expression leading to gain or loss of
function involves the silencing of genes through epigenetic
modifications. The two most intensely studied alterations include
DNA methylation and histone acetylation. Both of these genetic
alterations can affect chromatin packing and create a DNA / histone
complex that is not able to be transcribed. The result is silencing of
the noted gene despite its non-mutated presence. Although any gene
can be affected by these epigenetic phenomena, many of the genes
implicated in cancer development involve tumor suppression, cell
cycle control, cell death, cell growth, and differentiation. The
silencing of gene expression secondary to DNA methylation is
responsible for a variety of normal, physiologic functions including
X-chromosome inactivation, facilitation of DNA imprinting, and
protection against insertion of viral DNA into the genome [89]. DNA
methyltransferase is the key enzyme that methylates CpG islands in
the promoter region of genes leading to hypermethylation and
silencing of gene transcription [90]. Many cancers appear to have
extensive regional hypermethylation as well as aberrant gene
expression leading researchers to explore the role of
hypermethylation in tumor development and progression: AML and
MDS lead the way in being the best studied diseases. There are
numerous genes that are implicated in MDS/AML pathophysiology
with p15INK4B being one of the most studied. Specifically,
hypermethylation of p15INK4B, a known tumor suppressor and cell
cycle regulatory gene, has been associated with progression of MDS
to AML [91, 92]. Functionally, CDK4 and CDK6 allow cell cycle
progression from G1 to S phase. p15INK4B can act as a tumor
suppressor and inhibit cell cycle progression by inhibiting the
function of CDK4 and 6. Hypermethylation of p15INK4B prevents
this suppressive function and allows uncontrolled progression
through the cell cycle and resultant uncontrolled proliferation [93].
p15INK4B hypermethylation has been seen in up to 50% of patients
with MDS; specifically in higher risk MDS, where the uncontrolled
proliferation has shown increased progression to AML and portends a
worse prognosis [92, 94, 95]. Hypermethylation of the calcitonin
gene has also been described and can be found in 65% of MDS cases.
Its presence spans all morphologic subtypes and is commonly found
in patients with normal cytogenetics [96]. Numerous studies now
suggest that hypermethylation of the calcitonin gene may be an
important marker of transformation from MDS to AML [97-99].
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 545
Other commonly reported hypermethylated genes in implicated in
MDS include E-Cadherin (CDH1), HIC1, and ER [94].
Similarly, conformational alterations of the DNA histone
complex also play an important role in the abnormal gene silencing
seen in many cancers. Acetylation of lysine residues on the N-
terminus of core histones creates an open and readily transcribable
chromatin structure while deacetylation creates a tightly coiled and
non-transcribable chromatin structure [100]. Acetylation status can
also alter transcription factors (GATA-1), nuclear import proteins,
signal transduction proteins, DNA repair enzymes, heat shock
proteins, and numerous other cellular proteins [101-106]. The
epigenetic modulation of these proteins leads to altered expression of
pro-apoptotic and cell cycle proteins (ex. FAS/FAS ligand, Bcl2, p53,
caspases, Bax, and p21WAF1/Cip1) [106] and can result in multiple
cellular effects including growth arrest in G1 or G2/M,
differentiation, and preferential apoptosis of cancer cells [100, 107].
Altered Bone Marrow Microenvironment: Apoptosis,
Cytokines and Angiogenesis
The bone marrow microenvironment has also been implicated in
the development and progression of MDS with numerous studies
showing altered cytokine milieu and apoptosis rates as well as
changes in vascular microdensity. These alterations produce a
common pathway of increased apoptosis of early, CD34+ progenitors
in early-stage MDS and a relative reversal of this ratio in later-stage
disease. As MDS progresses towards AML, these pathways become
less well defined and additional factors, including proliferative
genetic events, may play a more important role [12-14]. Each of these
processes may offer scientists numerous targets upon which to focus
new therapies.
Bone marrow samples from MDS patients traditionally reveal a
hypercellular marrow in the context of increased cytokines, such as
TNF-alpha and IFN-gamma, and persistent peripheral cytopenias.
Interestingly, data support both increased and decreased programmed
cell death within MDS marrows, yet careful analysis suggests that
increased apoptosis is more often associated with early stage MDS
(RA/RARS) while decreased apoptosis is more characteristic of
advanced disease (RAEB2/AML) [13, 14]. Cytokine dynamics offer
one explanation for such cycles of altered apoptosis within the
malignant clones. Elevations of TNF-alpha and IFN-gamma are
consistently described in the MDS bone marrow microenvironment
[37, 108, 109] with additional reports suggesting TGF-beta elevations
as well [110, 111] highlighting the important role cytokines play in
MDS pathogenesis and maintenance. The role of increased TNF-
alpha has been well studied in its involvement in promoting apoptosis
in MDS, particularly early stage disease [14, 37, 108]. TNF-alpha
promotes apoptosis by engaging with the tumor necrosis factor
receptor I and II (TNFRI or TNFRII) and via TNFRI mediates
programmed cell death by direct binding with TNF Receptor 1
associated protein with a death domain (TRADD), subsequent
indirect binding with FAS-associated protein with a death domain
(FADD), and eventual activation of the caspase cascade. TNF-alpha
can also interact with TNFRII, which lacks a death domain, but
interacts directly with TNF receptor-associated factor 2 (TRAF-2),
activating NF-!B and JNK, and ultimately promoting anti-apoptotic
effects [37, 112, 113]. The ratio of these receptors impacts the rates of
apoptosis in MDS with increased TNFRI documented in low-risk
disease and increased TNFRII in high risk disease illustrating, again,
the inverse correlation between rates of apoptosis and potential for
proliferation and disease progression [37].
Raza et al. have suggested that increased levels of TNF-alpha
have a dual impact on MDS development through contrary
stimulatory and inhibitory effects: stimulation of primitive progenitor
cells, yielding the classic hypercellularity of MDS, while exertion of
apoptotic influence on more mature cells, correlating with the
peripheral cytopenias [111]. The etiology of these cytokine alterations
and definition of the cells from which they originate (macrophages,
fibroblasts, or other) remain unanswered questions [114-117].
In addition to TNF-alphas impact on apoptosis in MDS,
abnormalities in FAS and bcl-2 pathways have also been implicated.
FAS is a transmembrane receptor belonging to the same superfamily
as the TNF-alpha receptor and its stimulation follows a similar path to
apoptosis that terminates with caspase cascade stimulation and
degradation of death substrates [14]. Abnormal FAS-signaling has
also been implicated in other bone marrow failure states such as
aplastic anemia as well as in other malignancies with specific studies
in MDS illustrating increased FAS expression and apoptosis in low-
risk disease and decreased FAS expression in high-risk disease.
Interestingly, although increased FAS expression has been seen, no
statistically significant correlation between FAS expression and
degree of apoptosis has been shown [118]. Thus, while increased
apoptosis is an important component in MDS pathophysiology and is
seen more in early stage disease, the mechanism for which this occurs
is not explained by one pathway alone and may involve FAS
signaling either via direct or indirect pathways [14, 118, 119]. While
the TNF-alpha and FAS signaling has supported the increased rates of
apoptosis in early stage disease, decreased apoptosis rates have also
been implicated in the progression from MDS to AML and has been
documented to occur via alterations in anti-apoptotic bcl-2 and bcl-x
expression [14].
Changes in vascular microdensity are another component of the
marrow environment identified as contributing to the development
and sustenance of MDS clones [120]. Originally a focus of research
in solid tumors, increased angiogenesis also appears to play a role in
hematologic malignancies. In solid tumors new blood vessels are
formed to sustain growth of the tumor by supplying blood and
nutrients. The role of angiogenesis in hematologic malignancies is
slowly being unveiled, and early findings suggest not only its
importance but also its varied character among different cancers. New
blood vessel growth can drive cytokine production, but may also be a
byproduct of excessive cytokines. As described above, the milieu in
MDS provides many cytokines capable of influencing new vessel
growth. In addition to increased TNF-alpha and INF-gamma in the
marrow of MDS patients, varying levels of angiogenic factors
including VEGF (vascular endothelial growth factor), bFGF
(fibroblast growth factor), angiogenin, HGF (hepatic growth factor),
EGF (epidermal growth factor), and TGF-beta (transforming growth
factor) have been noted in the plasma of MDS patients. These
findings, coupled with direct evidence of increased microvascular
density (MVD) on marrow biopsies, support the development of early
blood vessels in MDS [120-123]. Both plasma VEGF levels and
increased MVD correlate with advanced MDS FAB class [124-126]
and imply that increased VEGF may drive increased MVD eventually
stimulating MDS progression to AML.
Immune System Dysregulation
Dysregulated immunity has been implicated in the development
of all cancers, including MDS [127], but direct evidence in MDS has
been difficult to uncover. The successful use of immunosuppressive
therapies (i.e., cyclosporine-A, anti-thymocyte globulin), the
potentially curative role of allogeneic stem cell transplant, and the
more recent data showing improved peripheral cytopenias and
elimination of certain common cytogenetic abnormalities with
immunomodulatory agents (i.e., thalidomide and lenalidomide)
highlight the role immune dysregulation plays in the development of
MDS. Changes in both B and T cell dynamics have been implicated
in MDS development. Studies have substantiated an autoimmune-
type T cell attack in MDS pathogenesis. Specific in vitro work by
Smith et al. investigated the possibility of auto-reactive T cells and
noted the presence of inhibitory T cells in patients with MDS [128]
with subsequent clinical studies showing in vivo success using anti T-
cell therapies (anti-thymocyte globulin (ATG) [129] and
cyclosporine-A (CSA)) [130]. Investigation revealed an abnormal T
546 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
cell repertoire and T cell-mediated inhibition of bone marrow CFU-
GM [131] as a potential mechanism to the response to ATG. Further
characterization of the T cell repertoire in MDS patients demonstrated
T cell expansion with recurrent patterns of V-Beta and J region
skewing suggestive of unknown chronic antigenic stimulation [127]
while other studies identified high percentages of cytotoxic T cells
(CD8+, CD28-, CD57+) [132]. In aggregate, these findings indicate
an activated immune environment [133].
Irregularities in B cell function have also been implicated in MDS
based upon epidemiologic data revealing increased frequency of
autoimmune disorders and immune-mediated complications in these
patients [134, 135]. Studies evaluating this correlation revealed the
presence of either clinical or serologic manifestation of auto-
immunity in 10-12% of MDS patients with a higher prevalence in
younger patients, those with treatment-related MDS, or those with
cytogenetic abnormalities [135, 134]. Just as T cell repertoire
skewing has been noted, clonality of B cells within MDS is also
under investigation. The presence or absence of such clonality may
lend insight to the cell of disease origin. Using cytogenetic
abnormalities as a marker to trace lineage, various progenitor and
terminally differentiated populations in MDS samples have been
studied with seemingly discrepant findings. Using Trisomy 8 as the
tracing abnormality in their MDS samples, Saitohs group found the
additional 8th chromosome in granulocytes, monocytes, and
erythroblasts but not in lymphocytes in the BM or in B, T, or NK
cells of the peripheral blood. Additional analysis found Trisomy 8 in
the level of the CFU-GEMM stem cell (CD34+, CD33+) but not in
the pluripotent stem cells (CD34+, Thy1+) indicating absence of B
cell clonality and instead a myeloid progenitor as the neoplastic clone
[136]. Other groups have shown the presence of specific cytogenetic
abnormalities in both myeloid and lymphoid lineages indicting a
more pluripotent stem cell of origin. Specifically, Whites group
showed the presence of deletion 20q in Epstein Barr Virus (EBV)
immortalized lymphoid cell lines derived from an MDS patient [137]
while Nilssons group has shown interesting findings with both 5q
deletion and Trisomy 8 [138, 139]. Specific studies with 5q deletion
documented its presence in the majority of pluripotent (CD34+,
CD38-) stem cells with both myeloid and lymphoid differentiation;
however, transfer of this cell population to SCID mice showed
inability to reconstitute hematopoiesis indicating absence of 5q in the
most primitive progenitors [138]. Interestingly, in cases with both
Trisomy 8 and del 5q, it was evident that Trisomy 8 was a secondary
genetic event potentially explaining the discrepancy by suggesting
that the additional Trisomy 8 event developed in the progeny of the
CD34+CD38- del 5q containing stem cells [139]. The quest to
document the potential clonality of B cells involved in MDS
pathogenesis has led to the deeper discovery that different cytogenetic
abnormalities may originate in different cells of origin in MDS which
could have substantial implications on treatment strategies.
Cell Cycle Dysregulation, Abnormal Differentiation, and
Transcription Factor Alterations
Abnormal differentiation and growth represents the most
dominant morphologic feature of MDS. Although there has been an
exhaustive analysis of cellular signaling pathways in an effort to
define the main problems with differentiation, our best understanding
of this problem is linked to studies of the cell cycle: the cells ability
to initiate normal cellular division, speed of the cell cycle, and
regulation of cell cycle checkpoints. The speed of the cycle plays an
important role in assuring balanced homeostasis between self-renewal
and progenitor expansion with natural aging and cellular death of
each cell type required to maintain an adequate blood supply [140].
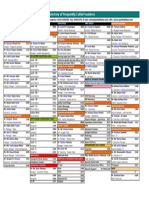
Transplant Candidate?
Yes
NO
INT-2/HIGH LOW/INT-2
INT-2/HIGH
AlloBMT#
Growth Factors**
CSA/ATG~
DMTIs @
Lenalidomide if 5q-
DMTIs
No Response? CLINICAL TRIAL +
# Controversies in BMT for MDS: Approaches to Consider
Timing of transplantation:
Low/INT-1: Delay BMT until progression but prior to
leukemic transformation
INT-2/High: Proceed towards BMT from diagnosis
Treatment Pre-BMT:
Low/INT-1: Consider BMT as 1
o
Therapy
INT-2/High: Consider alternative 1
o
Therapy piror to BMT
** If EPO level <500 consider
Erythropoietin. Consider addition of G-CSF
if no response to erythropoietin alone
! Improved response rates seen in
hypoplastic MDS, PNH clone, HLA-DR15
positivity
@ 5-azacitidine or decitabine
+ Participation in clinical trials encouraged
Fig. (1). Hopkins approach to MDS treatment.
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 547
Detailed molecular work has shown characteristic lineage
specific cell cycle changes required for normal differentiation: 1) up-
regulation of cdc2 and cyclin A in erythroid lines; 2) induction of
cyclin D1 and p15 in myeloid lines; and 3) selective upregulation of
cyclin D3 and induction of p21 in megakaryocyte differentiation
[141]. Alterations in any of these normal differentiation pathways
could thus lead to maturation arrests. Specific blocks in
differentiation in MDS and AML have been linked to abnormalities
such as constitutive activation of CDK inhibitor p16 leading to
G0/G1 arrest and subsequent maturation arrest [141]. Additionally,
cell cycle specific changes, such as alterations to the CDK inhibitor
and tumor suppressor p15INK4B, have been closely linked to
uncontrolled cell cycling and proliferation leading to progression
from MDS to AML [93].
Resultant aberrant cell cycle function in MDS has been the
common final pathway for a number of genetic, epigenetic,
micronenvironmental, and common transcription factor alterations.
The GATA transcription factor family (GATA-1, 2, and 3) is of
interest with alterations implicated in MDS pathogenesis. Normal
GATA-1 is involved in control of erythroid cells, megakaryocytes,
eosinophils, and mast cells while GATA-2 is expressed in more
immature progenitors including hematopoietic stem cells [142].
Abnormalities or increased levels of GATA-1 have previously been
described to affect cell cycle regulation [143], proliferation,
differentiation, and regulation of apoptosis [144] of both erythroid
and megakaryocytic progenitors. Studies show that normal GATA-2
expression is increased in hematopoietic stem cells and its expression
inhibits terminal differentiation thus playing more of a role in
proliferation and self-renewal capacity of the stem cells [145].
Consequently, imbalances of GATA-1 and GATA-2 could skew the
progenitor population contributing to abnormal differentiation [146],
the development of MDS [147], and in the setting of an additional
genetic hit may contribute to the progression to acute leukemia [142].
Table II. Theories of Pathophysiology involved in MDS Development
Theories of
Pathophysiology involved
in MDS Development
Potential Targets/Components Involved Overall Result of Abnormality
Current Directed Therapies,
Potential Directed Therapies,
and Investigatory Treatments for MDS
Environmental/Aging
Aging Increased BM apoptosis Decreased hematopoietic stem cell pool
Environmental Exposures
! Smoking
! Radiation
! Benzene
! Viral Infections
! Chemotherapy
! Direct Toxicity to hematopoietic stem
cells
! Genotoxic: O2 free radicals, DNA
damage
! Non-Genotoxic: Immune
modulation
(Immunoglobulin/complement
alterations) and altered BM
microenvironment
Telomere Abnormalities
! Potential decreased telomerase and
subsequent telomere shortening
! Impaired ability to renew stem cell pool
! Genetic Instability
Genetic Alterations
Cytogenetic Abnormalities
Common Abnormalities:
! 5q- ! 20q-
! Y- ! Trisomy 8
! 7q-/Monosomy7 ! 17p Syndrome
! 11q23 ! 3q
! P53 mutations ! Ras mutations
! Complex Cytogenetics
! Abnormalities: typically unbalanced
genetic loss
! Numerous theories of tumor suppressor
loss
! Multi-Hit progression from low risk
MDS to AML
! Genetic Instability
! Lenalidomide:* 5q- syndrome
! Ph III Lenalidomide in del 5q- pts @
NCT00179621
Epigenetic Modulation
! Hypermethylation:
! Calcitonin gene
! p15INK4B
! ER
! E-Cadherin
! Acetylation Alterations:
! Cell cycle components: p21WAF1
! Alteration of differentiation and
apoptotic machinery
! Alterations of angiogenesis
! Methylation and acetylation
abnormalities lead to silencing of
genes important in cell cycle,
differentiation, apoptosis,
angiogenesis
! DNA Methyltransferase Inhibitors: (DMTIs)#
! 5 Azacitidine*
! Ph I Aza maintenance post AlloBMT
@ NCT00350818
! Decitabine*
! Ph I/II Decitabine + Tretinoin @
NCT00382200
! Ph II Decitabine post Aza failure @
NCT00113321
! Histone Deacetylase Inhibitors (HDIs)
! Ph I MS-275 + Aza @ NCT00101179
! Ph II Aza,VPA, ATRA @NCT00339196
! Ph II Aza vs. VPA vs. Ara-C @
NCT00382590
! Ph II Decitabine +/- VPA @ NCT00414310
! Ph II MGCD0103 @ NCT00374296
! Ph I Vorinistat + Ara-C + VP-16 @
NCT00357305
Microscopic Genetic
Alterations
! Comparative Genomic Hybridization:
! Single Nucleotide Polymorphisms
(SNPs):
! NQO1
! Glutathione S-transferase
! G-CSF Receptor
! Microsatellite instability
! Dysfunction of enzymes required for
detoxification, DNA mismatch repair,
or differentiation
548 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
Given the complexity of the cell cycle control in hematopoiesis,
alterations of any key component could lead to abnormal
differentiation and the potential for MDS.
STANDARD TREATMENT FOR MDS
Until the recent past, treatment for MDS was limited to best
supportive care (growth factors and transfusion support) for the
(Table II). Contd..
Theories of
Pathophysiology involved
in MDS Development
Potential Targets/Components Involved Overall Result of Abnormality
Current Directed Therapies,
Potential Directed Therapies,
and Investigatory Treatments for MDS
Altered Bone Marrow
Microenvironment
Altered Bone Marrow
Microenvironment
Cytokines
! Upregulation of:
! TNF-"
! IFN-gamma
! TGF-Beta
! IL-1B
! IL-6
! Il-11
! Alteration of growth, differentiation,
angiogenesis
! Immune modulation
Anti-TNF-" Trials:
! Ph I/II Aza + Etanercept: INT-2 / High Risk @
NCT00118287
! Ph II ATG + Etanercept: low / INT-1 @
NCT00217386
! Ph II Infliximab: Low / INT-1 @ NCT00074074
! SCIO-469 Open Label Study: Inhibitor of
p38MAPK (TNF-"/other cytokine/Fas blocker)
@ NCT00113893
Alterations in Apoptosis via
Signaling
Increased TNF-! levels:
! Increased Apoptosis: Low Risk MDS
! Binding to TNFRI
oligomerization TRADD/FAD
association -- activation of
Caspase cascade -- increased
apoptosis
! Decreased Apoptosis: High Risk MDS
! Binding to TNFRII -- TRAF-2
interaction -- activation of NFkB
apoptosis inhibition
FAS: Increased Apoptosis
! Increased FAS binds to FAS-Ligand --
trimerization -- activation of FADD --
association with Caspase 8 --
triggering protease/caspase cascade
cleaving DNA repair proteins
BCL-2 alterations:
! Oncogene Interactions:
! Inhibits c-myc: required for
progression from G1/S
! Interacts with Raf-1
! Interacts with Ras
! Increased apoptosis and proliferation in
early stage MDS leading to
hypercellular marrow with peripheral
cytopenias
! Decreased apoptosis and increased
proliferation in later stage MDS
leading to progression to AML
Anti-TNF-" Trials: direct blockage see above
! Bortezamib @ NCT00440076 (indirect NFkB
inhibitor: implicated in TNF-" production)
Arsenic Trials: (Target TNF-", increase
susceptibility to apoptosis, suppress VEG-F, induce
differentiation via p21/p27 activation)
! Ph II Arsenic Trioxide @ NCT00225992
! Ph I/II Arsenic+ Ara-C @ NCT00195104
! Ph II Arsenic + Gemtuzimab @NCT00274781
! Ph I/II Aza + Arsenic @ NCT00234000
FAS Target:
! See above SCIO-469 trial ( FAS blocker)
BCL-2 Target: Ph II BCL- 2 inhibitor GX15-
070MS @ NCT00413114
Oncogene Targets:
! Ph I Sorafenib (Sorafenib: raf kinase/VEGF
inhibitor) @ NCT00217646
! Ph III Lonafarnib vs Placebo (farnesyl
transferase inhibitor: inhibits RAS) @
NCT00109538
Increased Angiogenesis
! Increased VEG-F
! Possible Increase:
! gFGF and EGF
! Angiogenin
! Increased Microvessel Density (MVD):
role in pathogenesis not clearly
elucidated but associated with
progression to AML
! Ph II Vatalanib (anti-angiogenesis/ VEGF
inhibitor) @ NCT000072475
! See above Sorafenib trial (VEGF inhibitor)
! See Arsenic Trioxide Trials
Immune Dysregulation
! T cell Expansion
! Skewed V# and J regions
! Increased Cytotoxic T cells CD8+,
CD28-, CD57+
! B cell alterations
! Clonal B cell expansion/connection
with increased frequency of
autoimmune phenomena in MDS
! Increased T cells leading to potential
attack on hematopoietic stem cells
! Etiology: Possible chronic antigenic
stimulation
IMIDs:
! Ph I Bortezomib + Thalidomide* @
NCT00271804
! Ph I Lenolidamide* + Aza @
NCT00326846
Other Immune Modulation:
! Ph III ATG + CSA vs. Best Supportive Care @
NCT00004208
! Ph I/II Campath +CSA @ NCT00217594
! WT-1/PR-1 Peptide Vaccine + GM-CSF @
NCT00313638
! K562/GM-CSF Vaccine @NCT00361296
! Alloreactive NK Infusion + AlloBMT : Ph I/II
@ NCT00402558 and Ph II @ NCT00303667
! Cytoxan + DLI @ NCT00356928
Abnormal Differentiation
! Cell Cycle Maturation arrest: Ex: p16 alt.
! Altered Proliferation: Ex. p15INK4B
! Transcription Factors alt: GATA-1/GATA-2
! Impaired maturation
! Cytopenias
! Progression to leukemia
! Ph II Calcitriol + Dex @ NCT00030069
Growth Factors + Differentiating Agents:
! Ph II Bexarotene+GM-CSF@NCT00425477
Legend: *-FDA-Approved for MDS; @- clinical trials from clinicaltrials.gov; # = Numerous epigenetic trial combinations active: representative sample included.
BM = bone marrow; DMTIs = DNA Methyltransferase inhibitors; HDIs = Histone deacetylase inhibitors, MDS = myelodysplastic syndrome; AML = acute myelogenous leukemia; ER = Estrogen receptor; Aza =5-
Azacitidine; Ph = Phase; VPA = valproic acid; ATRA= all-trans retinoic acid; CSA = cyclosporine A; gFGF = fibroblast growth factor; EGF = epidermal growth factor; ATG = anti-thymocyte globulin; NK = natural
killer; AlloBMT = allogeneic bone marrow transplant; DLI = donor lymphocyte infusion; dex = decadron; GM-CSF = granulocyte macrophage colony stimulating factor; alt = alterations
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 549
majority of patients and allogeneic stem cell transplant for the small
minority of patients eligible for the procedure. Of these treatments,
only transplant offered an approach that changed the natural history
of the disease and offered a cure. More recently, newer agents, such
as azacitidine and decitabine, have been FDA approved to treat MDS
based on their impact on the natural history of disease through
decreasing the rate of transformation from MDS to AML. Formal
evaluation of response to treatment has been described by
International Working Group (IWG) criteria, which has recently been
modified and described in Table III [148]. We review current
standard treatments (Table IV), describe future directions and novel
treatment approaches, and conclude with a treatment algorithm for
MDS patients (Fig. (1)).
Supportive Care
Based on concerns of poor tolerance to traditional cytotoxic
agents in patients with advanced age, poor performance status, or
medical co-morbidities, supportive care has been the longstanding
approach to MDS patients. Unfortunately, these criteria of concern
are common in the MDS population. Traditionally, supportive care
has taken the form of close blood count monitoring, blood product
transfusions, systemically administered lineage-directed growth
factors, and often prophylactic antibiotics with the sole intent of
improving marrow function and minimizing the impact of the bone
marrow failure on the patients lives. While somewhat effective, each
of these approaches is relatively limited. Close monitoring of blood
counts requires a compliant and diligent patient and takes time each
week for testing and follow-up. Use of transfusions is ultimately
limited by the development of alloimmunization and the resultant
antibodies that effectively reduce the impact of both red cell and
platelet transfusions. Myeloid growth factors are generally only
recommended in patients plagued by recurrent neutropenic fevers,
severe systemic infections, or in combination with erythropoietin.
Erythropoietin is generally considered the most effective supportive
approach yet yields an overall response of approximately 16% as a
single agent [149, 150] and up to 36-50% in combination with G-CSF
Table III. Modified IWG Response Criteria
Response Category Response Criteria ( must last minimum of 4 weeks)
Complete Remission BM: < 5% blasts with normal trilineage maturation
Any persistent dysplasia
PB:
Hgb> 11g/dl
Neutrophils > 1 X 10
9
/L
Blasts 0%
Partial Remission If abnormal before treatment, all CR criteria except:
BM blasts decreased by >50% but still greater than 5%
Marrow CR BM: < 5% blasts and greater than 50% decrease over pre-treatment
PB: HI responses will be described in addition to marrow CR
Stable Disease
PR not achieved but no progression for >8 weeks
Failure
Death or disease progression
Relapse post CR/PR 1+ of the following:
Recurrence of pre-treatment BM blast %
> 50% Decrease from greatest response in neutrophils or platelets
Hgb reduced by greater than 1.5 g/dl or transfusion dependence
Cytogenetic Response Complete: Resolution of all cytogenetic abnormalities
Partial: 50%+ reduction of cytogenetic abnormality
Disease Progression For patients with:
1) < 5% BM blasts: > 50% increase in blasts to >5%
2) 5-10% BM blasts: > 50% increase in blasts to >10%
3) 10-20% BM blasts: > 50% increase in blasts to >20%
4) 20-30% BM blasts: > 50% increase in blasts to >30%
Any of:
1) 50%+ decrease in maximum neutrophil or platelet response
2) Hgb reduction by > 2g/dl
3) Transfusion Dependence
Survival Endpoints:
OS: Death by any cause
EFS: Treatment failure or death by any cause
PFS: progressive disease or death from MDS
DFS: time to relapse
Cause-specific death: any death related to MDS
Hematologic Improvement
(HI)
Responses must be sustained for at least 8 weeks:
Erythroid Responses (pre-treatment <11 gm/dl):
! Hgb increase by > 1.5 g/dl
! Reduced PRBC transfusions by at least 4 per 8 week period compared to pre-treatment transfusion requirements (only those
given for Hgb < 9 g/dl counted)
Platelet Responses (pre-treatment < 100 X 10
9
/L)
! Absolute increase of > 30 X 10
9
/L for pts starting with > 20 X 10
9
/L
! Increase from < 20 X 10
9
/L to > 20 X 10
9
/L by > 100%
Neutrophil Response (pre-treatment < 1 X 10
9
/L)
! > 100% increase and final count > 0.5 X 10
9
/L
Progression or relapse after HI:
At least one of the following:
! 50%+ decrease from maximum response in neutrophils or platelets
! Hgb reduction by > 1.5 g/dl
! Transfusion dependence
Legend: BM = Bone marrow; PB = peripheral blood; g/dl = grams per deciliter; CR = Complete Remission; PR = Partial Remission; HI = Hematologic Response; Hgb = Hemoglobin; OS = Overall Survival; EFS =
Event-free survival; PFS = Progression Free Survival; DFS = Disease-Free Survival
Adapted from [148]
550 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
[150-154]. Prolonged administration may yield higher responses with
Terpos et al. showing response rates approximating 50% in patients
with a low blast percentage [155]. Responders are typically limited to
patients with significant anemia, transfusion independence, and low
endogenous EPO levels [155, 149]. Newer studies using darbepoetin
in MDS patients have reported erythroid response rates ranging from
26% in previous erythropoietin failures [156] to rates as high as 71%
[157]. Interestingly, new reports have highlighted adverse outcomes
in patients receiving high doses of erythropoietin or darbepoetin to
achieve a hemoglobin level greater than 12. While tumor progression
and decreased survival were the adverse outcomes in head and neck
and breast cancer patients respectively, general adverse events
included increased venous and arterial thrombosis, strokes,
myocardial infarction, and congestive heart failure. Given the
increased concern, the FDA has altered its safety information to
recommend using the lowest dose of the agent needed to decrease
transfusion requirements, increasing the hemoglobin gradually, and
not exceeding a hemoglobin level of 12mg/dl.
1
While these studies
prompt caution in the extended use of erythropoietin growth factors
in MDS patients, reaching a hemoglobin level greater than 12 is
unusual, and consequently the degree to which these findings will
affect this patient population is yet to be determined.
Allogeneic Stem Cell Transplantation
Allogeneic stem cell transplant, the only known curative
treatment option for MDS patients, lies at the other treatment
extreme. Unfortunately, several factors limit its application for most
patients and include advanced age, poor performance status, limited
access to an HLA matched sibling or matched un-related donor
(MUD), and significant potential for treatment related morbidity and
mortality. Despite these problems, allogeneic transplants are
commonly recommended for younger patients. Transplant outcomes
for more than 452 MDS patients conducted and reported by the
IBMTR from 1989 through 1997 were recently presented. The
median age of the group undergoing the transplant was 38 years with
an overall disease free survival of 53% at 1 year and 40% at 3 years
and cumulative incidences of relapse of 17% at 1 year and 23% at 3
years [158]. The most important predictor of survival was the blast
percentage prior to transplant with increased relapse correlating with
increasing blast percentage and higher IPSS scores. Transplant-
related mortality was 32% at 1 year and 37% at 3 years. Generally,
most data cite improved transplant outcomes in patients treated both
early in their disease course and with low level disease [158].
Alternative reports indicate that some pause should be taken when
making decisions regarding allogeneic BMT in younger or low risk
MDS patients. Kuendgen et al. reported their series following over
200 untreated MDS patients younger than 50 years of age in an
attempt to establish a more accurate natural history of disease and
compared their outcomes to a registry of over 2000 MDS patients
older than 50. In IPSS low risk or INT-1 disease, untreated patients
less than 50 years of age had an overall survival nearing 80% (median
still not reached at 360 months) compared to an overall survival less
than 20% with a median of 45 months in the untreated older cohort
[159]. In IPSS INT-2 or high risk disease, there appeared to be no
difference in survival between the two age groups thus indicating that
age was an important predictor for survival particularly in IPSS early
stage disease, while treatment more a predictor of outcome in
advanced stage disease. The study also evaluated outcomes
comparing treatment versus best supportive care and showed no
improvement in survival in low risk and INT-1 disease but superior
outcomes in treated INT-2 and high risk IPSS disease [159].
Additionally, Cutler et al. contributed to decision analysis for use of
alloBMT in MDS patients and showed improved outcomes when
transplant was delayed from diagnosis but completed prior to
leukemic transformation in low risk MDS [160]. With previous
1
www.FDA-news.com. 3/1/2007 report: FDA Warnings Regarding High Dose
Erythropoietin Products.
reports recommending allogeneic BMT for young patients with low
grade, early stage disease, these data provide an updated perspective
and would suggest that in young, low risk and INT-1 IPSS MDS
patients, transplant should be delayed until IPSS progression or
progression of cytogenetic abnormalities.
Most patients will not be considered medical candidates for
myeloablative preparative regimens, and many of those who are
candidates will not have a matched sibling donor. Strategies have
evolved to make allogeneic treatments more broadly available by
developing approaches that adjust for each of the limiting factors.
Reduced intensity conditioning (RIC) and non-myeloablative
regimens have successfully minimized the preparative regimen
toxicities to make older patients and those with mild to moderate end-
organ dysfunction eligible. Graft manipulation methods have focused
on decreasing the rates and severity of the most lethal complication of
allogeneic transplants, graft versus host disease. In addition,
alternative stem cell sources, including the use of cord blood stem
cells and haploidentical stem cells, have been developed to expand
the donor pool.
Recent retrospective analysis of 993 MDS patients undergoing
allogeneic transplant comparing myeloablative and reduced intensity
conditioning (RIC) regimens showed improvements in favor of RIC
in terms of non-relapse mortality at 3 years (22% vs. 32%) and rates
of acute GVHD (43% vs. 58%); however, these improvements
were offset by a higher rate of relapse at 3 years (45% vs. 27%) [161].
Not surprisingly, relapse rates were higher in individual risk groups
of older age (>50 years), poor risk cytogenetics, and in those
undergoing transplant greater than 6 month from diagnosis.
Interestingly, the overall survival and progression free survival rates
were not statistically different between the two groups with 3 year OS
of 41% and 45% in RIC and myeloablative regimens respectively and
a 3 year PFS of 33% and 39% [161]. Reduced intensity regimens, or
non-myeloablative regiments, have thus been successful with regards
to decreasing transplant-related toxicity in terms of end organ
toxicity; however, this proposed benefit has been offset by the higher
incidence of relapse, mixed chimerism, and similar or higher rates of
GVHD [162-165]. One proposed mechanism for the increased
relapse, or decreased graft versus leukemia effect, is the loss of direct
cytoreduction and increased occurrence of mixed chimerism from
reduced intensity preparative regimens [162]. Despite the fact that
RIC regimens allow for use of alloBMT in the older MDS
population, several reports now suggest the importance of preparative
regimen dose intensity for allogeneic BMT in MDS, particularly due
to its ability to control active disease [162-165]. Unfortunately, better
disease control with intensity comes at the expense of increased
mortality, particularly in elderly patients. Given these issues, an
alternative method of transplant maintaining conditioning intensity
while decreasing treatment related toxicity and adequately dealing
with relapse is needed. The use of T cell depleted allografts following
a myeloablative preparative regimen could reduce the toxicity of
alloBMT while maintaining dose intensity; however, the success of
TCD has also been limited due to increased relapse [166, 158]
suggesting that in such settings additional post-BMT interventions are
needed.
Efforts are also underway to expand the potential source of
donors for MDS patients requiring bone marrow transplantation by
using alternative stem cell sources such as cord blood and
haploidentical transplants. A recent analysis of 22 MDS patients
undergoing unrelated cord blood transplants showed a four year
disease free survival of 76% with relatively low severe acute GVHD
and a moderate degree of extensive stage chronic GVHD [167]
showing feasibility of this alternative source of bone marrow for
patients without a suitable matched unrelated donor. Additionally,
recent studies with haploidentical donors have shown similar
outcomes to fully-matched transplants in terms of GVHD and
morbidity and mortality in myeloid malignancies with only advanced
acute leukemia associated with higher rates of relapse and mortality
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 551
[168]. Efforts continue to expand the potential alternative donor
source and improve upon outcomes.
Targeting Epigenetic Changes
Within the past 3 years, options for the medical management of
MDS has evolved from the limited supportive care approach of
careful count monitoring, transfusions, and growth factors to now
having 3 FDA-approved agents indicated for the treatment of patients
with MDS. This progress has led to enthusiasm among physicians
and their patients and families. However, the availability of these
drugs has raised many important questions including how to best use
each of the drugs including when to initiate therapy, which agent to
use, and how to best administer each of the drugs. There is also
intensive ongoing investigation to better understand the mechanism
of action of each of the drugs.
The data supporting the close relationship between epigenetic
modifications and the biology of MDS grows almost daily.
Importantly, 5-azacitidine and decitabine, two newly FDA approved
DNA methyltransferase inhibitors, are clinically effective in high risk
MDS and appear to work at least in part, by reversing these
epigenetic changes. The agents cause demethylation of commonly
involved promoter regions by incorporation into DNA as nucleoside
analogues resulting in inhibition of the methyltransferase activity
responsible for maintaining these hyper-methylated regions [169]. A
phase III CALGB trial comparing 5-azacitidine versus best
supportive care showed an overall response rate of 60% (7% CR, 16
% PR, and 37% improved) compared to only 5% in the supportive
care only arm [170]. The responses also appeared to confer a survival
advantage and a decrease in the risk of AML transformation (21
months versus 13 months) in the 5-azacitidine treated group [170].
Retrospective analysis of several 5-azacitidine trials done in the
CALGB (trials 8421, 8921, and 9221) incorporated the new IWG
[171] response criteria (Table III) and confirmed its effectiveness but
showed lower complete response rates (10-17%) and increased
hematologic responses (23-26%) with most responses being seen by
the sixth cycle [171].
Similar response data also exists for a second, FDA-approve
DNA methyltransferase inhibitor, decitabine. Early studies with
varying treatment schedules showed hematopoietic responses nearing
50% [172, 173] and lead to further Phase III trials randomizing
patients to decitabine versus best supportive care. In this Phase III
study, the decitabine treatment resulted in a complete response rate of
9%, a hematologic improvement rate of 13%, and median response
duration of 10 months [174]. Although no survival benefit was seen,
most patients became transfusion independent and there was a trend
towards a delay to AML transformation or death [174]. Retrospective
subset review suggested that responses were associated with
cytogenetic complete remissions in 35% of patients [174]. More
recent studies have focused on improving dosing schedules of
decitabine (namely lower dosing over increased days) for higher risk
MDS patients and show higher CR rates (21-30%) and overall
responses of up to 73% noting a median of 3 cycles needed to obtain
CR [175].
Chromatin remodeling via histone acetylation status is a second
epigenetic target [176] with histone deacetylase inhibitors (HDIs)
another group of agents used to modify epigenetic changes.
Acetylation of lysine residues on the N-terminus of core histones
creates an open and readily transcribable chromatin structure. HDIs
function to reverse the gene silencing caused by deacetylation and
maintain the histones in an acetylated and transcribable state [100]
and exist as several different classes of drugs including hydroximates
(trichostatin A and SAHA), cyclic peptides (cyclic tetrapeptides),
aliphatic acids (phenylbutyrate and valproic acid), and benzamides
(MS-275) [177]. A variety of clinical trials have shown both single
agent clinical and biologic activity. For example, the use of valproic
acid either alone or in combination with all-trans-retinoic acid
(ATRA) in MDS patients has shown an overall hematologic response
rate of 24%. Interestingly, response rate correlated inversely with
bone marrow blast percentage and those with a normal blast count
had a greater than 50% response rate while those with > 10% blasts
(RAEB I or II) had only a 6% response rate [178, 179]. Additional
studies with various HDIs such as MS-275, valproic acid, and SAHA
are ongoing.
Use of IMIDS as Immune Therapy
Cyclosporine and ATG were among the first immunomodulatory
agents used in the treatment of MDS and showed partial success in
producing transfusion independence [129, 130]. The mechanism of
action of these agents remained unclear, but investigators identified a
small subset of patients, typically RA patients with less than 5%
blasts, with the following associations that responded with transfusion
independence: HLA-DR15 or HLA-DR2 association, younger age,
and shorter duration of red cell transfusion dependence [180]. Efforts
to study agents that had immunomodulatory impact in MDS were
undertaken and thalidomide emerged as having mild clinical activity
with very interesting potential mechanisms of action, including: 1)
immunomodulatory effects related to a shift of T cell response from
Th1 to a Th2 [181], partial T cell activation via alteration of
secondary T cell signals, and increased NK cell number and cellular
lytic activity [182]; 2) anti-angiogenic properties through possible
mechanisms such as nitric oxide inhibition and blockage of
endothelial cell migration [183], inhibition of VEG-F and bFGF
[120], inhibition of TNF-alpha-induced upregulation of cell adhesion
markers, [184] and additional TNF-alpha independent mechanisms
[185]; 3) alterations of the bone marrow microenvironment through
the impact of cytokines and augmentation of stromal cell growth
[120]; 4) alterations of apoptosis [182, 186]; and 5) alterations of
adhesion molecule expression [187, 182].
Early studies of thalidomides effectiveness in patients with MDS
reported 31% hematologic responses after twelve weeks of therapy
[188]. Subsequent studies revealed response rates from minimal to
nearly 50% with partial success inducing transfusion independence
seen in a subset of patients [189-192]. Unfortunately, the side effect
profile of hypotension, neuropathy, constipation, and drowsiness
makes the drug poorly tolerated, especially in elderly patients [190].
Consequently, based on the clinical activity of thalidomide, newer
analogues have been developed to try to minimize side effects.
Lenalidomide is the only currently clinically available thalidomide
analogue for treatment of patients with MDS. It is reported to share
many of the same mechanisms of action with thalidomide; however,
lenalidomide has not shown the same effect on endothelial cell
proliferation [193-195]. Given the better toxicity profile and similar
mechanism of action, clinical investigation by List et al. began with
early phase I/II trials showing extraordinary clinical response
specifically in a subset of MDS patients who either hadnt responded
to EPO therapy or had high endogenous levels, had low risk IPSS, or
had cytogenetic abnormalities involving chromosome 5 [196]. The
study boasted a 56% overall hematologic response rate across all
cytogenetic abnormalities; in predominantly low risk IPSS, with 63%
of previously transfusion-dependant patients achieving transfusion
independence. Median time to hematologic response ranged from 9 to
11.5 weeks depending on the dose of lenalidomide. Hematologic
effects, primarily erythroid, were the most notable in patients with
deletion 5q31. Additionally, complete cytogenetic responses were
seen in 50% with a median time to response of 8 weeks. Toxicities
included significant neutropenia and thrombocytopenia in greater
than half the patients [196]. Further larger scale trials are ongoing to
study the effects of lenalidomide in specific subsets of MDS and have
substantiated the early success [197]. Additionally, trials investigating
the combination of lenalidomide with other agents are ongoing.
NEW THERAPEUTIC APPROACHES UNDER DEVELOP-
MENT FOR MDS
The incredibly complex pathophysiology intrinsic to MDS
provides many targets and fertile ground for investigators to develop
552 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
new treatment approaches. A very well done recent review captured
many of these approaches [199]. We focus our new therapeutic
discussion on three areas under development at our own institution:
epigenetics, immune modulation, and differentiation-based
approaches.
Table IV. Standard Treatments for MDS
Treatment Categories Drugs Dose Expected Response Studies
Erythropoietin Standard Starting Dose:
! 150 IU/kg SQ 3 times weekly
(Micromedix)
vs.
! 40,000-60,000 IU 2-3 times a
week for 2-3 months (NCCN
Guidelines)
! Prolonged EPO administration
(minimum 26 weeks) using 150
IU/kg 3 times weekly dose
Overall HR: 16% [149]
RR by certain characteristics:
! Trans. Indep. vs. Dep. (44% vs. 10%)
! Mode using FAB group (RARS vs. other)
+ Epo level + trans. status predicts
response to EPO
! MDS (not RARS) + Trans. Indep. RR
>50%
! RARS + EPO>200U/l RR=0%
Overall RR: 45%
Better RR if:
! low blast %
! Good Cytogenetics
! EPO<150U/l
Hellstrom-Linberg
et al. Meta-
analysis [149]
Terpos et al. [155]
Darbepoetin ** under
investigation for
MDS
! 300mcg SQ weekly then 300mcg
SQ q2weeks maintenance
! Transition from EPO to Dar:
Darbepoetin dose 200mcg
q2weeks
Tx for 12 wks: ER: 71%
! 8/13 patients previous EPO non-
responders
Tx. Naive Patients:
! Epo: MR 35%
! Dar: MR 46%
Prev EPO:
! Epo: MR 17%
! Dar: MR 26%
Mannone et al.
[157]
Patton et al. [156]
Growth Factors
Erythropoietin + G-
CSF
Varied Schedules
! EPO 5000-10,000 IU/day SQ + G-
CSF 30-75-150mcg/day SQ
! EPO 300U/kg 3 times weekly for
8 weeks + G-CSF 1mcg/kg/day
SQ
! G-CSF 1mcg/kg daily X 2 weeks
then EPO 300U /Kg per day for
minimum 8 weeks combined then
G-CSF stopped
! Review of studies
Results:
Overall ER: 38%
ER: 50%
Combined treatment:
! Neutrophil response 96% and ER 48%
After G-CSF Cessation:
! All neutrophil responses lost and 8/55
continued ER
Hellstrom-Lindberg
et al. [198]
Remacha et al. [152]
Negrin et al.[153]
Kasper et al. [154]
5-Azacitidine 75mg/m2 SQ qd X 7 days q4 weeks Response Typically Seen after 4 cycles:
Phase III CALGB:
OR: 60%
CR: 7% + PR: 16% + Improved: 37%
CALGB Reanalysis:
CR: 10-17%
HR: 23-26%
Majority of Responses seen by 6
th
cycle
Silverman et al.
[170]
Silverman et al.
[171]
Epigenetic Modulators
DNA Methyltransferase
Inhibitors
(DMTIs)
Decitabine 15mg/m2 IV q8hours times 3 days q6
wks
Alternative Treatment Schedules: Total
Dose: 100mg/m2
20mg/m2 IV qd X 5d
20mg/m2 SQ qd X 5d
10mg/m2 IV qd X 10d
Phase III Trial:
OR: 30%
CR: 9% + PR: 8% + HR: 13%
! All responders gained trans. indep.
! Majority of Responders: cytogenetic
response
Overall Response: 73%
CR: 34% + PR: 1% + Marrow CR: 11% +
Marrow CR + HI: 14% + HI: 13%
CR % per dosing schedule:
20mg/m2 IV: 39%
20mg/m2 SQ: 21%
10mg/ms IV: 24%
Kantarjian et al.
[174]
Kantarjian et al.
[175]
Standard
Myeloablative
Conditioning
Per specific regimens 3 yr DFS: 40%
3 yr Relapse Rate: 23%
3 yr TRM: 37%
IBMTR Data/
Sierra et al. [158]
Reduced Intensity
Conditioning
Per specific Regimens 3 yr PFS: 33%
3 yr Relapse Rates: 45%
3 year NRM: 22%
Martino et al.
[161]
Bone Marrow Transplant
T Cell Depletion
(TCD)
Per specific regimen Entire Group:
2 yr DFS: 39%
2 yr Relapse: 34%
RA Pts:
DFS: 73%
Relapse: 11%
Advanced MDS: (in CRI)
DFS: 42%
Relapse: 34%
IBMTR Data: TCD
Relative Risk of TRM: 0.6
Relative Risk of Relapse: 1.8
Mattijssen et al.
[166]
Sierra et al. [158]
Thalidomide 100mg titrated to 400mg/day for 12 wks
Survey of studies
ER: 31%
Varied Response:
! 0 50%
Raza et al. [188]
Numerous Studies
[189-192]
Immunotherapy
Lenalidomide 10mg po qday
10mg/day for 21 days
ER: 54%
ER: 65%
Improved Response:
Low IPSS/FAB class and highest in del5q-83%
List et al. [196]
Legend: Trans. = Transfusion; Indep. = Independence; Dep.= Dependence; kg = kilogram; mcg = microgram; OR = Overall response; MR = Major Response; Epo = Erythropoietin; CR = Complete response; ER =
Erythroid Response; Dar = Darbepoetin; PR = Partial response; RARS = Refractory Anemia w/ Ringed Sideroblasts; HR = HematologicResponse; RR = Response Rate; mg/m2 = milligrams per meters squared; CALGB
= The Cancer and Leukemia Group B; NRM = Non-relapse mortality; TRM = Treatment-related mortality; DFS = Disease Free Survival; PFS = Progression Free Survival; Pts = patients, TCD = T Cell Depletion.
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 553
Epigenetic Treatments Expanding Targets
Epigenetic modulation through a combination of DMTIs and
HDIs seemed to be a logical approach noting the responses seen with
these individual classes of agents. A pilot study combining
phenylbutyrate (HDI) with 5-azacitidine showed that both complete
and partial remissions could be achieved in nearly half of the MDS
and AML patients and showed a strong association between the
clinical responses and changes in hypermethylation and expression of
p15 [200]. The clinical responses were supported with findings from
a second pilot study of the same combination [201]. Gore et al.
combined MS-275 (HDI) with 5-azacitidine (DMTI) in a follow-up
pilot study recently presented in abstract form at ASH 2006
2
. Thirty
one patients (13 MDS, 4CMMol, and 14 AML 4 of which had multi-
lineage dysplasia) were treated with the combination. Azacitidine was
given in 3 different doses subcutaneously for 10 days and MS-275
was given orally in 4 different doses on day 3 and 10 of a 28 day
cycle. The treatment regimen was based on in vitro studies illustrating
the optimal timing for reversal of epigenetic silencing. Of patients
with MDS or AML w/ MLD, 50% responded with a median time to
best hematologic response of 4 cycles. Of the entire cohort, 6 clinical
responses were seen in the 20 patients with cytogenetic abnormalities
and included 4 with complete cytogenetic responses. Best cytogenetic
responses were seen in a median of 4 cycles. Correlative studies
showed increased H3 or H4 acetylation after 5 azacitidine alone in
30% of patients with increase in H3 and H4 acetylation after
combination therapy in 25/29 and 28/29 patients respectively. Gores
study provided additional excitement for the successful combination
of DMTIs and HDIs in treating MDS and AML w/ MDL and
prompted the current ECOG randomized trial comparing MS-275 +
5-azacitidine to 5-azacitidine alone.
Immune Strategies Immune System Modulation through
Vaccines
Vaccine strategies have been employed in many solid tumor
malignancies and more recently, hematologic malignancies. Despite
the enthusiasm from many clinical immunologists, there is little
published clinical efficacy data for these approaches to date. Some
strategies are based on targeting tumor antigens preferentially
expressed by the cancer cells. Specifically in MDS and AML, much
of the vaccines work has been based on overexpressed antigens (WT-
1, survivin, and proteinase 3). A peptide vaccine against WT-1 was
developed and studied in a phase I trial in Japan [202]. The study
treated 12 patients with AML and considered 7 responders based on a
decrease in WT-1 serum levels following the vaccines. Of interest, 2
MDS patients receiving the vaccine became markedly cytopenic.
Based on concerns that the vaccine may in fact be targeting both
normal and MDS stem cells, no further patients with MDS were
enrolled [202]. However, this may be the stronger piece of correlative
data supporting the activity of such approaches. Currently at the
Sidney Kimmel Cancer Center at Johns Hopkins, we have created a
pilot study evaluating the use of an institutionally-developed,
K562/GM-CSF secreting vaccine in patients with MDS. Given that
K562 expresses a number of defined myeloid antigens, such as WT-
1, proteinase 3, and survivin, found overexpressed in MDS as well as
other myeloid malignancies, it has the potential to generate specific
anti-tumor responses to these antigens. Open to 15 MDS patients, our
trial will evaluate treatment success based on clinical parameters
including resolution of cytogenetic abnormalities or improvement of
transfusion requirements with additional investigation of immune
correlates.
2
Gore, S. D.; Jiemjit, A.; Silverman, L. B.; Aucott, T.; Baylin, S.; Carraway, H.;
Dauses, T.; Fandy, T.; Herman, J.; Karp, J.; Licht, J. D.; Murgo, A. J.; Odchimar-
Reissig, R.; Smith, B. D.; Zwiebel, J. A.; Sugar, E. Combined
Methyltransferase/Histone Deacetylase Inhibition with 5-Azacitidine and MS-275 in
Patients with MDS, CMMoL and AML: Clinical Response, Histone Acetylation and
DNA Damage. Blood (ASH Annual Meeting Abstracts) 2006, 108, 517.
Differentiation Therapy Combinations that Improve
Responses
The outstanding success of ATRA in the treatment of acute
promyelocytic leukemia (APL) is proof of the principle that
differentiation therapy has potential to be an important therapy [203].
MDS has also been the target of attempts at utilizing differentiation
therapy with the use of agents such as interferon, polar planar
compounds, homoharringtonine, 5-azacitidine, ara-c, butyrates,
amifostine, retinoids, vitamin D derivatives, growth factors, and/or
combinations of the above drugs [204]. Each of these agents has
shown glimpses of differentiating activity, including single agent
interferon [205-209], demethylating agents [170, 171, 173, 174],
vitamin D derivatives [210-212], and retinoids in combination with
other compounds [179, 213, 214].
Interestingly, each of these agents appears to have differing
mechanisms of action raising the question of how pharmacologic
differentiating agents actually work. In vitro studies have shown that
lineage-specific growth factors can enhance the activity of many
pharmacologic differentiation agents noted above in both AML and
MDS cell lines and primary bone marrow cells [215-217]. Further
investigation noted that this synergy only occurred with cytostatic
doses of the pharmacologic differentiating agents. This supported the
hypothesis that pharmacologic differentiating agents functioned
primarily through inhibition of cell cycle and could preferentially
augment the differentiating capacity of growth factors indicating that
the agents were not sufficient in and of themselves for terminal
differentiation of malignant cells [217]. Matsuis group went on to
show that growth factors were actually required for substantial in
vitro differentiation [215-217]. While growth factors alone are
sufficient to induce differentiation, their use as single agents is limited
due to their pleiotropic effects of stimulating proliferation and
enhancing survival via inhibition of apoptosis [218, 219]. Thus, in
theory, preferential enhancement of self-renewal and survival could
cause tumor progression while selective induction of differentiation
could exhaust the neoplastic clone. This hypothesis was recently
tested in a phase I study with the differentiating agent bryostatin in
combination with GM-CSF at the Sidney Kimmel Cancer Center at
Johns Hopkins. Bryostatin, a protein kinase C agonist, was
administered via continuous infusion in a dose escalation fashion.
Smith and colleagues
3
found that Bryostatin, in conjunction with
GM-CSF, had remarkable clinical activity with 1 poor risk AML
patient achieving a CR following a single course of the combination
therapy and a second MDS patient having a morphologic CR and
partial cytogenetics response following 2 cycles. Unfortunately,
further development was limited due to an intolerable side effect
profile at clinically active doses. Future directions that build upon
these principles include agents with in vitro activity in combination
with growth factors including the HDI, MS-275, and novel retinoids,
like bexarotene.
SUMMARY
The myelodysplastic syndromes are an incredibly complex
spectrum of hematopoietic stem cell disorders. Their range of severity
along with variations in response to multiple treatment approaches
suggests that the pathophysiology underpinning these disorders is just
as complex. We are only beginning to unravel the biology of MDS.
This review hopes to not only provide a broad introduction to the
complex pathways involved in the development and progression of
these disorders but also to intrigue and challenge both basic and
clinical scientists to continue to work towards unlocking the
mysteries of MDS.
3
Smith, B. D.; Matsui, W.; Gladstone, D. E.; Karp, J.; Gore, S.; Huff, C. A.; Vala, M.;
Baker, S.; Zhao, M.; Piantadosi, S.; Jones, R. J. Differentiation Therapy for Poor Risk
Myeloid Malignancies: Results of a Dose Finding Study of Bryostatin-1 (BRYO) +
GM-CSF. Blood (ASH Annual Meeting Abstracts) 2005, 106, 2792.
554 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
ACKNOWLEDGEMENTS
Special thanks to Dr. Michael Mcdevitt for review of the
manuscript and expert advice. Special thanks to Dr. Steven Gore for
his instrumental help in development of the Hopkins Treatment
Algorithm. Special thanks also to Kimberly Pate for her help in table
and manuscript formatting.
REFERENCES
[1] Aul, C.; Giagounidis, U.; Germing, U. Epidemiological features of
myelodysplastic syndrome: real or factitious? Int. J. Hematol. 2001, 73(4),
405-410.
[2] Yin, S. N.; Hayes, R. B.; Linet, M. S.; Li, G. L.; Dosemeci, M.; Travis, L. B.;
Li, C. Y.; Zhang, Z. N.; Li, D. G.; Chow, W. H.; Wacholder, S.; Wang, Y.
Z.; Jiang, Z. L.; Dai, T. R.; Zhang, W. Y.; Chao, X. J.; Ye, P. Z.; Kou, Q. R.;
Zhang, X. C.; Lin, X. F.; Meng, J. F.; Ding, C. Y.; Zho, J. S.; Blot, W. J. A
cohort study of cancer among benzene-exposed workers in China: overall
results. Am. J. Ind. Med. 1996, 29(3), 227-235.
[3] West, R. R.; Stafford, D. A.; Farrow, A.; Jacobs, A. Occupational and
environmental exposures and myelodysplasia: a case-control study. Leuk.
Res. 1995, 19(2), 127-139.
[4] Moloney, W. C. Radiogenic leukemia revisited. Blood 1987, 70(4), 905-908.
[5] Pedersen-Bjergaard, J.; Philip, P.; Larsen, S. O.; Andersson, M.; Daugaard,
G.; Ersboll, J.; Hansen, S. W.; Hou-Jensen, K.; Nielsen, D.; Sigsgaard, T. C.
Therapy-related myelodysplasia and acute myeloid leukemia. Cytogenetic
characteristics of 115 consecutive cases and risk in seven cohorts of patients
treated intensively for malignant diseases in the Copenhagen series.
Leukemia 1993, 7(12), 1975-1986.
[6] Pasqualetti, P.; Festuccia, V.; Acitelli, P.; Collacciani, A.; Giusti, A.; Casale,
R. Tobacco smoking and risk of haematological malignancies in adults: a
case-control study. Br. J. Haematol. 1997, 97(3), 659-662.
[7] Ido, M.; Nagata, C.; Kawakami, N.; Shimizu, H.; Yoshida, Y.; Nomura, T.;
Mizoguchi, H. A case-control study of myelodysplastic syndromes among
Japanese men and women. Leuk. Res. 1996, 20(9), 727-731.
[8] Mundle, S.; Allampallam, K.; Aftab, R. K.; Dangerfield, B.; Cartlidge, J.;
Zeitler, D.; Afenya, E.; Alvi, S.; Shetty, V.; Venugopal, P.; Raza, A.
Presence of activation-related m-RNA for EBV and CMV in the bone
marrow of patients with myelodysplastic syndromes. Cancer Lett. 2001,
164(2), 197-205.
[9] Dalamaga, M.; Petridou, E.; Cook, F. E.; Trichopoulos, D. Risk factors for
myelodysplastic syndromes: a case-control study in Greece. Cancer Causes
Control. 2002, 13(7), 603-608.
[10] Rund, D.; Ben Yehuda, D. Therapy-related leukemia and myelodysplasia:
evolving concepts of pathogenesis and treatment. Hematology 2004, 9(3),
179-187.
[11] Olney, H. J.; Le Beau, M. M. The cytogenetics of myelodysplastic
syndromes. Best. Pract. Res. Clin. Haematol. 2001, 14(3), 479-495.
[12] Parker, J. E.; Mufti, G. J.; Rasool, F.; Mijovic, A.; Devereux, S.; Pagliuca, A.
The role of apoptosis, proliferation, and the Bcl-2-related proteins in the
myelodysplastic syndromes and acute myeloid leukemia secondary to MDS.
Blood 2000, 96(12), 3932-3938.
[13] Rajapaksa, R.; Ginzton, N.; Rott, L. S.; Greenberg, P. L. Altered oncoprotein
expression and apoptosis in myelodysplastic syndrome marrow cells. Blood
1996, 88(11), 4275-4287.
[14] Parker, J. E.; Mufti, G. J. Ineffective haemopoiesis and apoptosis in
myelodysplastic syndromes. Br. J. Haematol. 1998, 101(2), 220-230.
[15] Rosenfeld, C.; List, A. A hypothesis for the pathogenesis of myelodysplastic
syndromes: implications for new therapies. Leukemia 2000, 14(1), 2-8.
[16] Bennett, J. M.; Catovsky, D.; Daniel, M. T.; Flandrin, G.; Galton, D. A.;
Gralnick, H. R.; Sultan, C. Proposals for the classification of the acute
leukaemias. French-American-British (FAB) co-operative group. Br. J.
Haematol. 1976, 33(4), 451-458.
[17] Bennett, J. M.; Catovsky, D.; Daniel, M. T.; Flandrin, G.; Galton, D. A.;
Gralnick, H. R.; Sultan, C. Proposals for the classification of the
myelodysplastic syndromes. Br. J. Haematol. 1982, 51(2), 189-199.
[18] Steensma, D. P.; Tefferi, A. The myelodysplastic syndrome(s): a perspective
and review highlighting current controversies. Leuk. Res. 2003, 27(2), 95-
120.
[19] Steensma, D. P.; Bennett, J. M. The myelodysplastic syndromes: diagnosis
and treatment. Mayo Clin. Proc. 2006, 81(1), 104-130.
[20] Harris, N. L.; Jaffe, E. S.; Diebold, J.; Flandrin, G.; Muller-Hermelink, H.
K.; Vardiman, J.; Lister, T. A.; Bloomfield, C. D. World Health Organization
classification of neoplastic diseases of the hematopoietic and lymphoid
tissues: report of the Clinical Advisory Committee meeting-Airlie House,
Virginia, November 1997. J. Clin. Oncol. 1999, 17(12), 3835-3849.
[21] Vardiman, J. W.; Harris, N. L.; Brunning, R. D. The World Health
Organization (WHO) classification of the myeloid neoplasms. Blood 2002,
100(7), 2292-2302.
[22] Greenberg, P.; Cox, C.; LeBeau, M. M.; Fenaux, P.; Morel, P.; Sanz, G.;
Sanz, M.; Vallespi, T.; Hamblin, T.; Oscier, D.; Ohyashiki, K.; Toyama, K.;
Aul, C.; Mufti, G.; Bennett, J. International scoring system for evaluating
prognosis in myelodysplastic syndromes. Blood 1997, 89(6), 2079-2088.
[23] Catenacci, D. V.; Schiller, G. J. Myelodysplasic syndromes: A
comprehensive review. Blood Rev. 2005, 19(6), 301-319.
[24] Mufti, G. J. Pathobiology, classification, and diagnosis of myelodysplastic
syndrome. Best. Pract. Res. Clin. Haematol. 2004, 17(4), 543-557.
[25] Kuang, S.; Liang, W. Clinical analysis of 43 cases of chronic benzene
poisoning. Chem. Biol. Interact. 2005, 153-154, 129-135.
[26] Aksoy, M.; Dincol, K.; Erdem, S.; Dincol, G. Acute leukemia due to chronic
exposure to benzene. Am. J. Med. 1972, 52(2), 160-166.
[27] Yardley-Jones, A.; Anderson, D.; Parke, D. V. The toxicity of benzene and
its metabolism and molecular pathology in human risk assessment. Br. J. Ind.
Med. 1991, 48(7), 437-444.
[28] Hiraku, Y.; Kawanishi, S. Oxidative DNA damage and apoptosis induced by
benzene metabolites. Cancer Res. 1996, 56(22), 5172-5178.
[29] Smith, M. T. The mechanism of benzene-induced leukemia: a hypothesis and
speculations on the causes of leukemia. Environ. Health Perspect. 1996,
104(Suppl. 6), 1219-1225.
[30] Rothman, N.; Haas, R.; Hayes, R. B.; Li, G. L.; Wiemels, J.; Campleman, S.;
Quintana, P. J.; Xi, L. J.; Dosemeci, M.; Titenko-Holland, N. Benzene
induces gene-duplicating but not gene-inactivating mutations at the
glycophorin A locus in exposed humans. Proc. Natl. Acad. Sci. USA 1995,
92(9), 4069-4073.
[31] Aul, C.; Bowen, D. T.; Yoshida, Y. Pathogenesis, etiology and epidemiology
of myelodysplastic syndromes. Haematologica 1998, 83(1), 71-86.
[32] Pedersen-Bjergaard, J.; Andersen, M. K.; Christiansen, D. H.; Nerlov, C.
Genetic pathways in therapy-related myelodysplasia and acute myeloid
leukemia. Blood 2002, 99(6), 1909-1912.
[33] Matsuo, T.; Tomonaga, M.; Bennett, J. M.; Kuriyama, K.; Imanaka, F.;
Kuramoto, A.; Kamada, N.; Ichimaru, M.; Finch, S. C.; Pisciotta, A. V.
Reclassification of leukemia among A-bomb survivors in Nagasaki using
French-American-British (FAB) classification for acute leukemia. Jpn. J.
Clin. Oncol. 1988, 18(2), 91-96.
[34] Kadhim, M. A.; Lorimore, S. A.; Hepburn, M. D.; Goodhead, D. T.; Buckle,
V. J.; Wright, E. G. Alpha-particle-induced chromosomal instability in
human bone marrow cells. Lancet 1994, 344(8928), 987-988.
[35] Kitagawa, M.; Yamaguchi, S.; Takahashi, M.; Tanizawa, T.; Hirokawa, K.;
Kamiyama, R. Localization of Fas and Fas ligand in bone marrow cells
demonstrating myelodysplasia. Leukemia 1998, 12(4), 486-492.
[36] Ogawa, T.; Kitagawa, M.; Hirokawa, K. Age-related changes of human bone
marrow: a histometric estimation of proliferative cells, apoptotic cells, T
cells, B cells and macrophages. Mech. Ageing Dev. 2000, 117(1-3), 57-68.
[37] Sawanobori, M.; Yamaguchi, S.; Hasegawa, M.; Inoue, M.; Suzuki, K.;
Kamiyama, R.; Hirokawa, K.; Kitagawa, M. Expression of TNF receptors
and related signaling molecules in the bone marrow from patients with
myelodysplastic syndromes. Leuk. Res. 2003, 27(7), 583-591.
[38] Moyzis, R. K.; Buckingham, J. M.; Cram, L. S.; Dani, M.; Deaven, L. L.;
Jones, M. D.; Meyne, J.; Ratliff, R. L.; Wu, J. R. A highly conserved
repetitive DNA sequence, (TTAGGG)n, present at the telomeres of human
chromosomes. Proc. Natl. Acad. Sci. USA 1988, 85(18), 6622-6626.
[39] Iwama, H.; Ohyashiki, K.; Ohyashiki, J. H.; Hayashi, S.; Yahata, N.; Ando,
K.; Toyama, K.; Hoshika, A.; Takasaki, M.; Mori, M.; Shay, J. W. Telomeric
length and telomerase activity vary with age in peripheral blood cells
obtained from normal individuals. Hum. Genet. 1998, 102(4), 397-402.
[40] Allsopp, R. C.; Vaziri, H.; Patterson, C.; Goldstein, S.; Younglai, E. V.;
Futcher, A. B.; Greider, C. W.; Harley, C. B. Telomere length predicts
replicative capacity of human fibroblasts. Proc. Natl. Acad. Sci. USA 1992,
89(21), 10114-10118.
[41] Kim, N. W.; Piatyszek, M. A.; Prowse, K. R.; Harley, C. B.; West, M. D.;
Ho, P. L.; Coviello, G. M.; Wright, W. E.; Weinrich, S. L.; Shay, J. W.
Specific association of human telomerase activity with immortal cells and
cancer. Science 1994, 266(5193), 2011-2015.
[42] Shay, J. W.; Bacchetti, S. A survey of telomerase activity in human cancer.
Eur. J. Cancer 1997, 33(5), 787-791.
[43] Engelhardt, M.; Kumar, R.; Albanell, J.; Pettengell, R.; Han, W.; Moore, M.
A. Telomerase regulation, cell cycle, and telomere stability in primitive
hematopoietic cells. Blood 1997, 90(1), 182-193.
[44] Ohyashiki, J. H.; Iwama, H.; Yahata, N.; Ando, K.; Hayashi, S.; Shay, J. W.;
Ohyashiki, K. Telomere stability is frequently impaired in high-risk groups
of patients with myelodysplastic syndromes. Clin. Cancer Res. 1999, 5(5),
1155-1160.
[45] Hirai, H. Molecular mechanisms of myelodysplastic syndrome. Jpn. J. Clin.
Oncol. 2003, 33(4), 153-160.
[46] Look, A. T. Molecular Pathogenesis of MDS. Hematology (Am. Soc.
Hematol. Educ. Program) 2005, 156-160.
[47] Nimer, S. D. Clinical management of myelodysplastic syndromes with
interstitial deletion of chromosome 5q. J. Clin. Oncol. 2006, 24(16), 2576-
2582.
[48] Jary, L.; Mossafa, H.; Fourcade, C.; Genet, P.; Pulik, M.; Flandrin, G. The
17p-syndrome: a distinct myelodysplastic syndrome entity? Leuk. Lymphoma
1997, 25(1-2), 163-168.
[49] Paulsson, K.; Johansson, B. Trisomy 8 as the sole chromosomal aberration in
acute myeloid leukemia and myelodysplastic syndromes. Pathol. Biol.
(Paris) 2007, 55(1), 37-48.
[50] Boultwood, J.; Lewis, S.; Wainscoat, J. S. The 5q-syndrome. Blood 1994,
84(10), 3253-3260.
[51] Nimer, S. D.; Golde, D. W. The 5q- abnormality. Blood 1987, 70(6), 1705-
1712.
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 555
[52] Fairman, J.; Chumakov, I.; Chinault, A. C.; Nowell, P. C.; Nagarajan, L.
Physical mapping of the minimal region of loss in 5q- chromosome. Proc.
Natl. Acad. Sci. USA 1995, 92(16), 7406-7410.
[53] Zhao, N.; Stoffel, A.; Wang, P. W.; Eisenbart, J. D.; Espinosa, R., III;
Larson, R. A.; Le Beau, M. M. Molecular delineation of the smallest
commonly deleted region of chromosome 5 in malignant myeloid diseases to
1-1.5 Mb and preparation of a PAC-based physical map. Proc. Natl. Acad.
Sci. USA 1997, 94(13), 6948-6953.
[54] Jaju, R. J.; Boultwood, J.; Oliver, F. J.; Kostrzewa, M.; Fidler, C.; Parker, N.;
McPherson, J. D.; Morris, S. W.; Muller, U.; Wainscoat, J. S.; Kearney, L.
Molecular cytogenetic delineation of the critical deleted region in the 5q-
syndrome. Genes Chromosomes Cancer 1998, 22(3), 251-256.
[55] Horrigan, S. K.; Arbieva, Z. H.; Xie, H. Y.; Kravarusic, J.; Fulton, N. C.;
Naik, H.; Le, T. T.; Westbrook, C. A. Delineation of a minimal interval and
identification of 9 candidates for a tumor suppressor gene in malignant
myeloid disorders on 5q31. Blood 2000, 95(7), 2372-2377.
[56] Le Beau, M. M.; Espinosa, R., III; Neuman, W. L.; Stock, W.; Roulston, D.;
Larson, R. A.; Keinanen, M.; Westbrook, C. A. Cytogenetic and molecular
delineation of the smallest commonly deleted region of chromosome 5 in
malignant myeloid diseases. Proc. Natl. Acad. Sci. USA 1993, 90(12), 5484-
5488.
[57] Boultwood, J.; Fidler, C.; Strickson, A. J.; Watkins, F.; Kostrzewa, M.; Jaju,
R. J.; Muller, U.; Wainscoat, J. S. Transcription mapping of the 5q-
syndrome critical region: cloning of two novel genes and sequencing,
expression, and mapping of a further six novel cDNAs. Genomics 2000,
66(1), 26-34.
[58] Vallespi, T.; Imbert, M.; Mecucci, C.; Preudhomme, C.; Fenaux, P.
Diagnosis, classification, and cytogenetics of myelodysplastic syndromes.
Haematologica 1998, 83(3), 258-275.
[59] Wattel, E.; Lai, J. L.; Hebbar, M.; Preudhomme, C.; Grahek, D.; Morel, P.;
Bauters, F.; Fenaux, P. De novo myelodysplastic syndrome (MDS) with
deletion of the long arm of chromosome 20: a subtype of MDS with distinct
hematological and prognostic features? Leuk. Res. 1993, 17(11), 921-926.
[60] Davis, M. P.; Dewald, G. W.; Pierre, R. V.; Hoagland, H. C. Hematologic
manifestations associated with deletions of the long arm of chromosome 20.
Cancer Genet. Cytogenet. 1984, 12(1), 63-71.
[61] Asimakopoulos, F. A.; Green, A. R. Deletions of chromosome 20q and the
pathogenesis of myeloproliferative disorders. Br. J. Haematol. 1996, 95(2),
219-226.
[62] Liang, H.; Fairman, J.; Claxton, D. F.; Nowell, P. C.; Green, E. D.;
Nagarajan, L. Molecular anatomy of chromosome 7q deletions in myeloid
neoplasms: evidence for multiple critical loci. Proc. Natl. Acad. Sci. USA
1998, 95(7), 3781-3785.
[63] Pasquali, F.; Bernasconi, P.; Casalone, R.; Fraccaro, M.; Bernasconi, C.;
Lazzarino, M.; Morra, E.; Alessandrino, E. P.; Marchi, M. A.; Sanger, R.
Pathogenetic significance of "pure" monosomy 7 in myeloproliferative
disorders. Analysis of 14 cases. Hum. Genet. 1982, 62(1), 40-51.
[64] Le Beau, M. M.; Espinosa, R., III; Davis, E. M.; Eisenbart, J. D.; Larson, R.
A.; Green, E. D. Cytogenetic and molecular delineation of a region of
chromosome 7 commonly deleted in malignant myeloid diseases. Blood
1996, 88(6), 1930-1935.
[65] Merlat, A.; Lai, J. L.; Sterkers, Y.; Demory, J. L.; Bauters, F.; Preudhomme,
C.; Fenaux, P. Therapy-related myelodysplastic syndrome and acute myeloid
leukemia with 17p deletion. A report on 25 cases. Leukemia 1999, 13(2),
250-257.
[66] Albin, M.; Bjork, J.; Welinder, H.; Tinnerberg, H.; Mauritzson, N.;
Johansson, B.; Billstrom, R.; Stromberg, U.; Mikoczy, Z.; Ahlgren, T.;
Nilsson, P. G.; Mitelman, F.; Hagmar, L. Acute myeloid leukemia and clonal
chromosome aberrations in relation to past exposure to organic solvents.
Scand. J. Work Environ. Health 2000, 26(6), 482-491.
[67] Thirman, M. J.; Larson, R. A. Therapy-related myeloid leukemia. Hematol.
Oncol. Clin. North Am. 1996, 10(2), 293-320.
[68] Wiederschain, D.; Kawai, H.; Shilatifard, A.; Yuan, Z. M. Multiple mixed
lineage leukemia (MLL) fusion proteins suppress p53-mediated response to
DNA damage. J. Biol. Chem. 2005, 280(26), 24315-24321.
[69] Papenhausen, P. R.; Griffin, S.; Tepperberg, J. Oncogene amplification in
transforming myelodysplasia. Exp. Mol. Pathol. 2005, 79(2), 168-175.
[70] Poppe, B.; Vandesompele, J.; Schoch, C.; Lindvall, C.; Mrozek, K.;
Bloomfield, C. D.; Beverloo, H. B.; Michaux, L.; Dastugue, N.; Herens, C.;
Yigit, N.; De Paepe, A.; Hagemeijer, A.; Speleman, F. Expression analyses
identify MLL as a prominent target of 11q23 amplification and support an
etiologic role for MLL gain of function in myeloid malignancies. Blood
2004, 103(1), 229-235.
[71] Pappa, V.; Young, B. D.; Economopoulos, T.; Papageorgiou, E.; Panani, A.;
Lilington, D.; Bollas, G.; Stamouli, M.; Kontsioti, F.; Tsiotra, P.; Vessalas,
G.; Dervenoulas, J.; Raptis, S. Absence of MLL gene rearrangement in de
novo myelodysplastic syndromes (MDS). Ann. Hematol. 2004, 83(3), 170-
175.
[72] Paquette, R. L.; Landaw, E. M.; Pierre, R. V.; Kahan, J.; Lubbert, M.;
Lazcano, O.; Isaac, G.; McCormick, F.; Koeffler, H. P. N-ras mutations are
associated with poor prognosis and increased risk of leukemia in
myelodysplastic syndrome. Blood 1993, 82(2), 590-599.
[73] Bos, J. L. ras oncogenes in human cancer: a review. Cancer Res. 1989,
49(17), 4682-4689.
[74] Harris, C. C.; Hollstein, M. Clinical implications of the p53 tumor-
suppressor gene. N. Engl. J. Med. 1993, 329(18), 1318-1327.
[75] Lai, J. L.; Preudhomme, C.; Zandecki, M.; Flactif, M.; Vanrumbeke, M.;
Lepelley, P.; Wattel, E.; Fenaux, P. Myelodysplastic syndromes and acute
myeloid leukemia with 17p deletion. An entity characterized by specific
dysgranulopoiesis and a high incidence of P53 mutations. Leukemia 1995,
9(3), 370-381.
[76] Horiike, S.; Kita-Sasai, Y.; Nakao, M.; Taniwaki, M. Configuration of the
TP53 gene as an independent prognostic parameter of myelodysplastic
syndrome. Leuk. Lymphoma 2003, 44(6), 915-922.
[77] Wattel, E.; Preudhomme, C.; Hecquet, B.; Vanrumbeke, M.; Quesnel, B.;
Dervite, I.; Morel, P.; Fenaux, P. p53 mutations are associated with
resistance to chemotherapy and short survival in hematologic malignancies.
Blood 1994, 84(9), 3148-3157.
[78] Paulsson, K.; Heidenblad, M.; Strombeck, B.; Staaf, J.; Jonsson, G.; Borg,
A.; Fioretos, T.; Johansson, B. High-resolution genome-wide array-based
comparative genome hybridization reveals cryptic chromosome changes in
AML and MDS cases with trisomy 8 as the sole cytogenetic aberration.
Leukemia 2006, 20(5), 840-846.
[79] Verdorfer, I.; Brecevic, L.; Saul, W.; Schenker, B.; Kirsch, M.; Trautmann,
U.; Helm, G.; Gramatzki, M.; Gebhart, E. Comparative genomic
hybridization-aided unraveling of complex karyotypes in human
hematopoietic neoplasias. Cancer Genet. Cytogenet. 2001, 124(1), 1-6.
[80] Wilkens, L.; Tchinda, J.; Burkhardt, D.; Nolte, M.; Werner, M.; Georgii, A.
Analysis of hematologic diseases using conventional karyotyping,
fluorescence in situ hybridization (FISH), and comparative genomic
hybridization (CGH). Hum. Pathol. 1998, 29(8), 833-839.
[81] Babicz, M.; Kowalczyk, J. R.; Winnicka, D.; Gaworczyk, A.; Lejman, M.;
Dmowski, R.; Kaczanowska, K. The effectiveness of high-resolution-
comparative genomic hybridization in detecting the most common
chromosomal abnormalities in pediatric myelodysplastic syndromes. Cancer
Genet. Cytogenet. 2005, 158(1), 49-54.
[82] Wilkens, L.; Burkhardt, D.; Tchinda, J.; Busche, G.; Werner, M.; Nolte, M.;
Ganser, A.; Georgii, A. Cytogenetic aberrations in myelodysplastic
syndrome detected by comparative genomic hybridization and fluorescence
in situ hybridization. Diagn. Mol. Pathol. 1999, 8(1), 47-53.
[83] Wolfler, A.; Erkeland, S. J.; Bodner, C.; Valkhof, M.; Renner, W.; Leitner,
C.; Olipitz, W.; Pfeilstocker, M.; Tinchon, C.; Emberger, W.; Linkesch, W.;
Touw, I. P.; Sill, H. A functional single-nucleotide polymorphism of the G-
CSF receptor gene predisposes individuals to high-risk myelodysplastic
syndrome. Blood 2005, 105(9), 3731-3736.
[84] Willman, C. L. Molecular genetic features of myelodysplastic syndromes
(MDS). Leukemia 1998, 12(Suppl. 1), S2-S6.
[85] Chen, H.; Sandler, D. P.; Taylor, J. A.; Shore, D. L.; Liu, E.; Bloomfield, C.
D.; Bell, D. A. Increased risk for myelodysplastic syndromes in individuals
with glutathione transferase theta 1 (GSTT1) gene defect. Lancet 1996,
347(8997), 295-297.
[86] Rothman, N.; Smith, M. T.; Hayes, R. B.; Traver, R. D.; Hoener, B.;
Campleman, S.; Li, G. L.; Dosemeci, M.; Linet, M.; Zhang, L.; Xi, L.;
Wacholder, S.; Lu, W.; Meyer, K. B.; Titenko-Holland, N.; Stewart, J. T.;
Yin, S.; Ross, D. Benzene poisoning, a risk factor for hematological
malignancy, is associated with the NQO1 609C-->T mutation and rapid
fractional excretion of chlorzoxazone. Cancer Res. 1997, 57(14), 2839-2842.
[87] Naoe, T.; Takeyama, K.; Yokozawa, T.; Kiyoi, H.; Seto, M.; Uike, N.; Ino,
T.; Utsunomiya, A.; Maruta, A.; Jin-nai, I.; Kamada, N.; Kubota, Y.;
Nakamura, H.; Shimazaki, C.; Horiike, S.; Kodera, Y.; Saito, H.; Ueda, R.;
Wiemels, J.; Ohno, R. Analysis of genetic polymorphism in NQO1, GST-
M1, GST-T1, and CYP3A4 in 469 Japanese patients with therapy-related
leukemia/ myelodysplastic syndrome and de novo acute myeloid leukemia.
Clin. Cancer Res. 2000, 6(10), 4091-4095.
[88] Olipitz, W.; Hopfinger, G.; Aguiar, R. C.; Gunsilius, E.; Girschikofsky, M.;
Bodner, C.; Hiden, K.; Linkesch, W.; Hoefler, G.; Sill, H. Defective DNA-
mismatch repair: a potential mediator of leukemogenic susceptibility in
therapy-related myelodysplasia and leukemia. Genes Chromosomes Cancer
2002, 34(2), 243-248.
[89] Robertson, K. D.; Jones, P. A. DNA methylation: past, present and future
directions. Carcinogenesis 2000, 21(3), 461-467.
[90] Singal, R.; Ginder, G. D. DNA methylation. Blood 1999, 93(12), 4059-4070.
[91] Herman, J. G.; Civin, C. I.; Issa, J. P.; Collector, M. I.; Sharkis, S. J.; Baylin,
S. B. Distinct patterns of inactivation of p15INK4B and p16INK4A
characterize the major types of hematological malignancies. Cancer Res.
1997, 57(5), 837-841.
[92] Quesnel, B.; Guillerm, G.; Vereecque, R.; Wattel, E.; Preudhomme, C.;
Bauters, F.; Vanrumbeke, M.; Fenaux, P. Methylation of the p15(INK4b)
gene in myelodysplastic syndromes is frequent and acquired during disease
progression. Blood 1998, 91(8), 2985-2990.
[93] Leone, G.; Teofili, L.; Voso, M. T.; Lubbert, M. DNA methylation and
demethylating drugs in myelodysplastic syndromes and secondary
leukemias. Haematologica 2002, 87(12), 1324-1341.
[94] Aggerholm, A.; Holm, M. S.; Guldberg, P.; Olesen, L. H.; Hokland, P.
Promoter hypermethylation of p15INK4B, HIC1, CDH1, and ER is frequent
in myelodysplastic syndrome and predicts poor prognosis in early-stage
patients. Eur. J. Haematol. 2006, 76(1), 23-32.
[95] Christiansen, D. H.; Andersen, M. K.; Pedersen-Bjergaard, J. Methylation of
p15INK4B is common, is associated with deletion of genes on chromosome
arm 7q and predicts a poor prognosis in therapy-related myelodysplasia and
acute myeloid leukemia. Leukemia 2003, 17(9), 1813-1819.
556 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
[96] Dhodapkar, M.; Grill, J.; Lust, J. A. Abnormal regional hypermethylation of
the calcitonin gene in myelodysplastic syndromes. Leuk. Res. 1995, 19(10),
719-726.
[97] Wu, S.; Xie, G.; Bai, R.; Wang, Y.; Zhu, P. Semi-quantitative study of
calcitonin gene methylation in myelodysplastic syndrome. Chin. Med. J.
(Engl.) 1998, 111(8), 690-693.
[98] Bai, R.; Wu, S.; Zhu, P.; Xue, H.; Xu, Y.; Qin, X. Quantitative study of
calcitonin gene methylation in myelodysplastic syndromes. Zhonghua Xue.
Ye. Xue. Za Zhi. 1997, 18(1), 17-20.
[99] Li, G.; Zou, D.; Bai, R. Clinical significance of human calcitonin and gene-
related peptide in the serum of myelodysplastic syndromes patients.
Zhonghua Xue. Ye. Xue. Za Zhi. 1999, 20(2), 79-81.
[100] Marks, P.; Rifkind, R. A.; Richon, V. M.; Breslow, R.; Miller, T.; Kelly, W.
K. Histone deacetylases and cancer: causes and therapies. Nat. Rev. Cancer
2001, 1(3), 194-202.
[101] Haggarty, S. J.; Koeller, K. M.; Wong, J. C.; Grozinger, C. M.; Schreiber, S.
L. Domain-selective small-molecule inhibitor of histone deacetylase 6
(HDAC6)-mediated tubulin deacetylation. Proc. Natl. Acad. Sci. USA 2003,
100(8), 4389-4394.
[102] Wolf, D.; Rodova, M.; Miska, E. A.; Calvet, J. P.; Kouzarides, T.
Acetylation of beta-catenin by CREB-binding protein (CBP). J. Biol. Chem.
2002, 277(28), 25562-25567.
[103] Bannister, A. J.; Miska, E. A.; Gorlich, D.; Kouzarides, T. Acetylation of
importin-alpha nuclear import factors by CBP/p300. Curr. Biol. 2000, 10(8),
467-470.
[104] Cohen, H. Y.; Lavu, S.; Bitterman, K. J.; Hekking, B.; Imahiyerobo, T. A.;
Miller, C.; Frye, R.; Ploegh, H.; Kessler, B. M.; Sinclair, D. A. Acetylation
of the C terminus of Ku70 by CBP and PCAF controls Bax-mediated
apoptosis. Mol. Cell 2004, 13(5), 627-638.
[105] Fuino, L.; Bali, P.; Wittmann, S.; Donapaty, S.; Guo, F.; Yamaguchi, H.;
Wang, H. G.; Atadja, P.; Bhalla, K. Histone deacetylase inhibitor LAQ824
down-regulates Her-2 and sensitizes human breast cancer cells to
trastuzumab, taxotere, gemcitabine, and epothilone B. Mol. Cancer Ther.
2003, 2(10), 971-984.
[106] Morgan, M. A.; Reuter, C. W. Molecularly targeted therapies in
myelodysplastic syndromes and acute myeloid leukemias. Ann. Hematol.
2006, 85(3), 139-163.
[107] Johnstone, R. W.; Licht, J. D. Histone deacetylase inhibitors in cancer
therapy: is transcription the primary target? Cancer Cell 2003, 4(1), 13-18.
[108] Kitagawa, M.; Saito, I.; Kuwata, T.; Yoshida, S.; Yamaguchi, S.; Takahashi,
M.; Tanizawa, T.; Kamiyama, R.; Hirokawa, K. Overexpression of tumor
necrosis factor (TNF)-alpha and interferon (IFN)-gamma by bone marrow
cells from patients with myelodysplastic syndromes. Leukemia 1997, 11(12),
2049-2054.
[109] Stifter, G.; Heiss, S.; Gastl, G.; Tzankov, A.; Stauder, R. Over-expression of
tumor necrosis factor-alpha in bone marrow biopsies from patients with
myelodysplastic syndromes: relationship to anemia and prognosis. Eur. J.
Haematol. 2005, 75(6), 485-491.
[110] Shetty, V.; Mundle, S.; Alvi, S.; Showel, M.; Broady-Robinson, L.; Dar, S.;
Borok, R.; Showel, J.; Gregory, S.; Rifkin, S.; Gezer, S.; Parcharidou, A.;
Venugopal, P.; Shah, R.; Hernandez, B.; Klein, M.; Alston, D.; Robin, E.;
Dominquez, C.; Raza, A. Measurement of apoptosis, proliferation and three
cytokines in 46 patients with myelodysplastic syndromes. Leuk. Res. 1996,
20(11-12), 891-900.
[111] Raza, A.; Mundle, S.; Shetty, V.; Alvi, S.; Chopra, H.; Span, L.; Parcharidou,
A.; Dar, S.; Venugopal, P.; Borok, R.; Gezer, S.; Showel, J.; Loew, J.; Robin,
E.; Rifkin, S.; Alston, D.; Hernandez, B.; Shah, R.; Kaizer, H.; Gregory, S.
Novel insights into the biology of myelodysplastic syndromes: excessive
apoptosis and the role of cytokines. Int. J. Hematol. 1996, 63(4), 265-278.
[112] Hsu, H.; Xiong, J.; Goeddel, D. V. The TNF receptor 1-associated protein
TRADD signals cell death and NF-kappa B activation. Cell 1995, 81(4), 495-
504.
[113] Hsu, H.; Huang, J.; Shu, H. B.; Baichwal, V.; Goeddel, D. V. TNF-
dependent recruitment of the protein kinase RIP to the TNF receptor-1
signaling complex. Immunity 1996, 4(4), 387-396.
[114] Flores-Figueroa, E.; Gutierrez-Espindola, G.; Montesinos, J. J.; Arana-Trejo,
R. M.; Mayani, H. In vitro characterization of hematopoietic
microenvironment cells from patients with myelodysplastic syndrome. Leuk.
Res. 2002, 26(7), 677-686.
[115] Wetzler, M.; Kurzrock, R.; Estrov, Z.; Estey, E.; Talpaz, M. Cytokine
expression in adherent layers from patients with myelodysplastic syndrome
and acute myelogenous leukemia. Leuk. Res. 1995, 19(1), 23-34.
[116] Deeg, H. J.; Beckham, C.; Loken, M. R.; Bryant, E.; Lesnikova, M.;
Shulman, H. M.; Gooley, T. Negative regulators of hemopoiesis and stroma
function in patients with myelodysplastic syndrome. Leuk. Lymphoma 2000,
37(3-4), 405-414.
[117] Koike, M.; Ishiyama, T.; Tomoyasu, S.; Tsuruoka, N. Spontaneous cytokine
overproduction by peripheral blood mononuclear cells from patients with
myelodysplastic syndromes and aplastic anemia. Leuk. Res. 1995, 19(9),
639-644.
[118] Bouscary, D.; De Vos, J.; Guesnu, M.; Jondeau, K.; Viguier, F.; Melle, J.;
Picard, F.; Dreyfus, F.; Fontenay-Roupie, M. Fas/Apo-1 (CD95) expression
and apoptosis in patients with myelodysplastic syndromes. Leukemia 1997,
11(6), 839-845.
[119] Gersuk, G. M.; Lee, J. W.; Beckham, C. A.; Anderson, J.; Deeg, H. J. Fas
(CD95) receptor and Fas-ligand expression in bone marrow cells from
patients with myelodysplastic syndrome. Blood 1996, 88(3), 1122-1123.
[120] Estey, E. H. Modulation of angiogenesis in patients with myelodysplastic
syndrome. Best. Pract. Res. Clin. Haematol. 2004, 17(4), 623-639.
[121] Aguayo, A.; Kantarjian, H.; Manshouri, T.; Gidel, C.; Estey, E.; Thomas, D.;
Koller, C.; Estrov, Z.; O'Brien, S.; Keating, M.; Freireich, E.; Albitar, M.
Angiogenesis in acute and chronic leukemias and myelodysplastic
syndromes. Blood 2000, 96(6), 2240-2245.
[122] Zorat, F.; Shetty, V.; Dutt, D.; Lisak, L.; Nascimben, F.; Allampallam, K.;
Dar, S.; York, A.; Gezer, S.; Venugopal, P.; Raza, A. The clinical and
biological effects of thalidomide in patients with myelodysplastic syndromes.
Br. J. Haematol. 2001, 115(4), 881-894.
[123] Brunner, B.; Gunsilius, E.; Schumacher, P.; Zwierzina, H.; Gastl, G.;
Stauder, R. Blood levels of angiogenin and vascular endothelial growth
factor are elevated in myelodysplastic syndromes and in acute myeloid
leukemia. J. Hematother. Stem Cell Res. 2002, 11(1), 119-125.
[124] Wimazal, F.; Krauth, M. T.; Vales, A.; Bohm, A.; Agis, H.; Sonneck, K.;
Aichberger, K. J.; Mayerhofer, M.; Simonitsch-Klupp, I.; Mullauer, L.;
Sperr, W. R.; Valent, P. Immunohistochemical detection of vascular
endothelial growth factor (VEGF) in the bone marrow in patients with
myelodysplastic syndromes: correlation between VEGF expression and the
FAB category. Leuk. Lymphoma 2006, 47(3), 451-460.
[125] Pruneri, G.; Bertolini, F.; Soligo, D.; Carboni, N.; Cortelezzi, A.; Ferrucci, P.
F.; Buffa, R.; Lambertenghi-Deliliers, G.; Pezzella, F. Angiogenesis in
myelodysplastic syndromes. Br. J. Cancer 1999, 81(8), 1398-1401.
[126] Korkolopoulou, P.; Apostolidou, E.; Pavlopoulos, P. M.; Kavantzas, N.;
Vyniou, N.; Thymara, I.; Terpos, E.; Patsouris, E.; Yataganas, X.; Davaris, P.
Prognostic evaluation of the microvascular network in myelodysplastic
syndromes. Leukemia 2001, 15(9), 1369-1376.
[127] Epperson, D. E.; Nakamura, R.; Saunthararajah, Y.; Melenhorst, J.; Barrett,
A. J. Oligoclonal T cell expansion in myelodysplastic syndrome: evidence
for an autoimmune process. Leuk. Res. 2001, 25(12), 1075-1083.
[128] Smith, M. A.; Smith, J. G. The occurrence subtype and significance of
haemopoietic inhibitory T cells (HIT cells) in myelodysplasia: an in vitro
study. Leuk. Res. 1991, 15(7), 597-601.
[129] Molldrem, J. J.; Caples, M.; Mavroudis, D.; Plante, M.; Young, N. S.;
Barrett, A. J. Antithymocyte globulin for patients with myelodysplastic
syndrome. Br. J. Haematol. 1997, 99(3), 699-705.
[130] Jonasova, A.; Neuwirtova, R.; Cermak, J.; Vozobulova, V.; Mocikova, K.;
Siskova, M.; Hochova, I. Cyclosporin A therapy in hypoplastic MDS patients
and certain refractory anaemias without hypoplastic bone marrow. Br. J.
Haematol. 1998, 100(2), 304-309.
[131] Molldrem, J. J.; Jiang, Y. Z.; Stetler-Stevenson, M.; Mavroudis, D.; Hensel,
N.; Barrett, A. J. Haematological response of patients with myelodysplastic
syndrome to antithymocyte globulin is associated with a loss of lymphocyte-
mediated inhibition of CFU-GM and alterations in T-cell receptor Vbeta
profiles. Br. J. Haematol. 1998, 102(5), 1314-1322.
[132] Melenhorst, J. J.; Eniafe, R.; Follmann, D.; Nakamura, R.; Kirby, M.;
Barrett, A. J. Molecular and flow cytometric characterization of the CD4 and
CD8 T-cell repertoire in patients with myelodysplastic syndrome. Br. J.
Haematol. 2002, 119(1), 97-105.
[133] Voulgarelis, M.; Giannouli, S.; Ritis, K.; Tzioufas, A. G. Myelodysplasia-
associated autoimmunity: clinical and pathophysiologic concepts. Eur. J.
Clin. Invest. 2004, 34(10), 690-700.
[134] Marisavljevic, D.; Kraguljac, N.; Rolovic, Z. Immunologic abnormalities in
myelodysplastic syndromes: clinical features and characteristics of the
lymphoid population. Med. Oncol. 2006, 23(3), 385-392.
[135] Billstrom, R.; Johansson, H.; Johansson, B.; Mitelman, F. Immune-mediated
complications in patients with myelodysplastic syndromes--clinical and
cytogenetic features. Eur. J. Haematol. 1995, 55(1), 42-48.
[136] Saitoh, K.; Miura, I.; Takahashi, N.; Miura, A. B. Fluorescence in situ
hybridization of progenitor cells obtained by fluorescence-activated cell
sorting for the detection of cells affected by chromosome abnormality
trisomy 8 in patients with myelodysplastic syndromes. Blood 1998, 92(8),
2886-2892.
[137] White, N. J.; Nacheva, E.; Asimakopoulos, F. A.; Bloxham, D.; Paul, B.;
Green, A. R. Deletion of chromosome 20q in myelodysplasia can occur in a
multipotent precursor of both myeloid cells and B cells. Blood 1994, 83(10),
2809-2816.
[138] Nilsson, L.; Astrand-Grundstrom, I.; Arvidsson, I.; Jacobsson, B.; Hellstrom-
Lindberg, E.; Hast, R.; Jacobsen, S. E. Isolation and characterization of
hematopoietic progenitor/stem cells in 5q-deleted myelodysplastic
syndromes: evidence for involvement at the hematopoietic stem cell level.
Blood 2000, 96(6), 2012-2021.
[139] Nilsson, L.; Astrand-Grundstrom, I.; Anderson, K.; Arvidsson, I.; Hokland,
P.; Bryder, D.; Kjeldsen, L.; Johansson, B.; Hellstrom-Lindberg, E.; Hast, R.;
Jacobsen, S. E. Involvement and functional impairment of the
CD34(+)CD38(-)Thy-1(+) hematopoietic stem cell pool in myelodysplastic
syndromes with trisomy 8. Blood 2002, 100(1), 259-267.
[140] Furukawa, Y. Cell cycle control during hematopoietic cell differentiation.
Hum. Cell 1997, 10(3), 159-164.
[141] Furukawa, Y.; Kikuchi, J.; Nakamura, M.; Iwase, S.; Yamada, H.; Matsuda,
M. Lineage-specific regulation of cell cycle control gene expression during
haematopoietic cell differentiation. Br. J. Haematol. 2000, 110(3), 663-673.
Myelodysplastic Syndromes Current Cancer Drug Targets, 2007, Vol. 7, No. 6 557
[142] Shimizu, R.; Kuroha, T.; Ohneda, O.; Pan, X.; Ohneda, K.; Takahashi, S.;
Philipsen, S.; Yamamoto, M. Leukemogenesis caused by incapacitated
GATA-1 function. Mol. Cell Biol. 2004, 24(24), 10814-10825.
[143] Dubart, A.; Romeo, P. H.; Vainchenker, W.; Dumenil, D. Constitutive
expression of GATA-1 interferes with the cell-cycle regulation. Blood 1996,
87(9), 3711-3721.
[144] Weiss, M. J.; Orkin, S. H. Transcription factor GATA-1 permits survival and
maturation of erythroid precursors by preventing apoptosis. Proc. Natl. Acad.
Sci. USA 1995, 92(21), 9623-9627.
[145] Briegel, K.; Lim, K. C.; Plank, C.; Beug, H.; Engel, J. D.; Zenke, M. Ectopic
expression of a conditional GATA-2/estrogen receptor chimera arrests
erythroid differentiation in a hormone-dependent manner. Genes Dev. 1993,
7(6), 1097-1109.
[146] McDevitt, M. A.; Shivdasani, R. A.; Fujiwara, Y.; Yang, H.; Orkin, S. H. A
"knockdown" mutation created by cis-element gene targeting reveals the
dependence of erythroid cell maturation on the level of transcription factor
GATA-1. Proc. Natl. Acad. Sci. USA 1997, 94(13), 6781-6785.
[147] Fadilah, S. A.; Cheong, S. K.; Roslan, H.; Rozie-Hanisa, M.; Yen, G. K.
GATA-1 and GATA-2 gene expression is related to the severity of dysplasia
in myelodysplastic syndrome. Leukemia 2002, 16(8), 1563-1565.
[148] Cheson, B. D.; Greenberg, P. L.; Bennett, J. M.; Lowenberg, B.; Wijermans,
P. W.; Nimer, S. D.; Pinto, A.; Beran, M.; de Witte, T. M.; Stone, R. M.;
Mittelman, M.; Sanz, G. F.; Gore, S. D.; Schiffer, C. A.; Kantarjian, H.
Clinical application and proposal for modification of the International
Working Group (IWG) response criteria in myelodysplasia. Blood 2006,
108(2), 419-425.
[149] Hellstrom-Lindberg, E. Efficacy of erythropoietin in the myelodysplastic
syndromes: a meta-analysis of 205 patients from 17 studies. Br. J. Haematol.
1995, 89(1), 67-71.
[150] Stein, R. S. The role of erythropoietin in the anemia of myelodysplastic
syndrome. Clin. Lymphoma 2003, 4(Suppl. 1), S36-S40.
[151] Hellstrom-Lindberg, E.; Negrin, R.; Stein, R.; Krantz, S.; Lindberg, G.;
Vardiman, J.; Ost, A.; Greenberg, P. Erythroid response to treatment with G-
CSF plus erythropoietin for the anaemia of patients with myelodysplastic
syndromes: proposal for a predictive model. Br. J. Haematol. 1997, 99(2),
344-351.
[152] Remacha, A. F.; Arrizabalaga, B.; Villegas, A.; Manteiga, R.; Calvo, T.;
Julia, A.; Fernandez, F., I; Gonzalez, F. A.; Font, L.; Junca, J.; del Arco, A.;
Malcorra, J. J.; Equiza, E. P.; de Mendiguren, B. P.; Romero, M.
Erythropoietin plus granulocyte colony-stimulating factor in the treatment of
myelodysplastic syndromes. Identification of a subgroup of responders. The
Spanish Erythropathology Group. Haematologica 1999, 84(12), 1058-1064.
[153] Negrin, R. S.; Stein, R.; Doherty, K.; Cornwell, J.; Vardiman, J.; Krantz, S.;
Greenberg, P. L. Maintenance treatment of the anemia of myelodysplastic
syndromes with recombinant human granulocyte colony-stimulating factor
and erythropoietin: evidence for in vivo synergy. Blood 1996, 87(10), 4076-
4081.
[154] Kasper, C.; Zahner, J.; Sayer, H. G. Recombinant human erythropoietin in
combined treatment with granulocyte- or granulocyte-macrophage colony-
stimulating factor in patients with myelodysplastic syndromes. J. Cancer
Res. Clin. Oncol. 2002, 128(9), 497-502.
[155] Terpos, E.; Mougiou, A.; Kouraklis, A.; Chatzivassili, A.; Michalis, E.;
Giannakoulas, N.; Manioudaki, E.; Lazaridou, A.; Bakaloudi, V.;
Protopappa, M.; Liapi, D.; Grouzi, E.; Parharidou, A.; Symeonidis, A.;
Kokkini, G.; Laoutaris, N. P.; Vaipoulos, G.; Anagnostopoulos, N. I.;
Christakis, J. I.; Meletis, J.; Bourantas, K. L.; Zoumbos, N. C.; Yataganas,
X.; Viniou, N. A. Prolonged administration of erythropoietin increases
erythroid response rate in myelodysplastic syndromes: a phase II trial in 281
patients. Br. J. Haematol. 2002, 118(1), 174-180.
[156] Patton, J. F.; Sullivan, T.; Mun, Y.; Reeves, T.; Rossi, G.; Wallace, J. F. A
retrospective cohort study to assess the impact of therapeutic substitution of
darbepoetin alfa for epoetin alfa in anemic patients with myelodysplastic
syndrome. J. Support. Oncol. 2005, 3(6), 419-426.
[157] Mannone, L.; Gardin, C.; Quarre, M. C.; Bernard, J. F.; Vassilieff, D.; Ades,
L.; Park, S.; Vaultier, S.; Hamza, F.; Beyne-rauzy, M. O.; Cheze, S.;
Giraudier, S.; Agape, P.; Legros, L.; Voillat, L.; Dreyfus, F.; Fenaux, P.
High-dose darbepoetin alpha in the treatment of anaemia of lower risk
myelodysplastic syndrome results of a phase II study. Br. J. Haematol. 2006,
133(5), 513-519.
[158] Sierra, J.; Perez, W. S.; Rozman, C.; Carreras, E.; Klein, J. P.; Rizzo, J. D.;
Davies, S. M.; Lazarus, H. M.; Bredeson, C. N.; Marks, D. I.; Canals, C.;
Boogaerts, M. A.; Goldman, J.; Champlin, R. E.; Keating, A.; Weisdorf, D.
J.; de Witte, T. M.; Horowitz, M. M. Bone marrow transplantation from
HLA-identical siblings as treatment for myelodysplasia. Blood 2002, 100(6),
1997-2004.
[159] Kuendgen, A.; Strupp, C.; Aivado, M.; Hildebrandt, B.; Haas, R.;
Gattermann, N.; Germing, U. Myelodysplastic syndromes in patients
younger than age 50. J. Clin. Oncol. 2006, 24(34), 5358-5365.
[160] Cutler, C. S.; Lee, S. J.; Greenberg, P.; Deeg, H. J.; Perez, W. S.; Anasetti,
C.; Bolwell, B. J.; Cairo, M. S.; Gale, R. P.; Klein, J. P.; Lazarus, H. M.;
Liesveld, J. L.; McCarthy, P. L.; Milone, G. A.; Rizzo, J. D.; Schultz, K. R.;
Trigg, M. E.; Keating, A.; Weisdorf, D. J.; Antin, J. H.; Horowitz, M. M. A
decision analysis of allogeneic bone marrow transplantation for the
myelodysplastic syndromes: delayed transplantation for low-risk
myelodysplasia is associated with improved outcome. Blood 2004, 104(2),
579-585.
[161] Martino, R.; Iacobelli, S.; Brand, R.; Jansen, T.; van Biezen, A.; Finke, J.;
Bacigalupo, A.; Beelen, D.; Reiffers, J.; Devergie, A.; Alessandrino, E.;
Mufti, G. J.; Barge, R.; Sierra, J.; Ruutu, T.; Boogaerts, M.; Falda, M.; Jouet,
J. P.; Niederwieser, D.; De Witte, T. Retrospective comparison of reduced
intensity conditioning and conventional high dose conditioning for allogeneic
hematopoietic stem cell transplantation using HLA identical sibling donors
in myelodysplastic syndromes. Blood 2006, 108(3), 836-846.
[162] de Lima, M.; Anagnostopoulos, A.; Munsell, M.; Shahjahan, M.; Ueno, N.;
Ippoliti, C.; Andersson, B. S.; Gajewski, J.; Couriel, D.; Cortes, J.; Donato,
M.; Neumann, J.; Champlin, R.; Giralt, S. Nonablative versus reduced-
intensity conditioning regimens in the treatment of acute myeloid leukemia
and high-risk myelodysplastic syndrome: dose is relevant for long-term
disease control after allogeneic hematopoietic stem cell transplantation.
Blood 2004, 104(3), 865-872.
[163] Scott, B. L.; Sandmaier, B. M.; Storer, B.; Maris, M. B.; Sorror, M. L.;
Maloney, D. G.; Chauncey, T. R.; Storb, R.; Deeg, H. J. Myeloablative vs
nonmyeloablative allogeneic transplantation for patients with
myelodysplastic syndrome or acute myelogenous leukemia with multilineage
dysplasia: a retrospective analysis. Leukemia 2006, 20(1), 128-135.
[164] Shimoni, A.; Hardan, I.; Shem-Tov, N.; Yeshurun, M.; Yerushalmi, R.;
Avigdor, A.; Ben Bassat, I.; Nagler, A. Allogeneic hematopoietic stem-cell
transplantation in AML and MDS using myeloablative versus reduced-
intensity conditioning: the role of dose intensity. Leukemia 2006, 20(2), 322-
328.
[165] Alyea, E. P.; Kim, H. T.; Ho, V.; Cutler, C.; Deangelo, D. J.; Stone, R.; Ritz,
J.; Antin, J. H.; Soiffer, R. J. Impact of Conditioning Regimen Intensity on
Outcome of Allogeneic Hematopoietic Cell Transplantation for Advanced
Acute Myelogenous Leukemia and Myelodysplastic Syndrome. Biol. Blood
Marrow Transplant. 2006, 12(10), 1047-1055.
[166] Mattijssen, V.; Schattenberg, A.; Schaap, N.; Preijers, F.; De Witte, T.
Outcome of allogeneic bone marrow transplantation with lymphocyte-
depleted marrow grafts in adult patients with myelodysplastic syndromes.
Bone Marrow Transplant. 1997, 19(8), 791-794.
[167] Ooi, J. The efficacy of unrelated cord blood transplantation for adult
myelodysplastic syndrome. Leuk. Lymphoma 2006, 47(4), 599-602.
[168] Lu, D. P.; Dong, L.; Wu, T.; Huang, X. J.; Zhang, M. J.; Han, W.; Chen, H.;
Liu, D. H.; Gao, Z. Y.; Chen, Y. H.; Xu, L. P.; Zhang, Y. C.; Ren, H. Y.; Li,
D.; Liu, K. Y. Conditioning including antithymocyte globulin followed by
unmanipulated HLA-mismatched/haploidentical blood and marrow
transplantation can achieve comparable outcomes with HLA-identical sibling
transplantation. Blood 2006, 107(8), 3065-3073.
[169] Kizaki, M.; Koeffler, H. P. Differentiation-inducing agents in the treatment
of myelodysplastic syndromes. Semin. Oncol. 1992, 19(1), 95-105.
[170] Silverman, L. R.; Demakos, E. P.; Peterson, B. L.; Kornblith, A. B.; Holland,
J. C.; Odchimar-Reissig, R.; Stone, R. M.; Nelson, D.; Powell, B. L.;
DeCastro, C. M.; Ellerton, J.; Larson, R. A.; Schiffer, C. A.; Holland, J. F.
Randomized controlled trial of azacitidine in patients with the
myelodysplastic syndrome: a study of the cancer and leukemia group B. J.
Clin. Oncol. 2002, 20(10), 2429-2440.
[171] Silverman, L. R.; McKenzie, D. R.; Peterson, B. L.; Holland, J. F.;
Backstrom, J. T.; Beach, C. L.; Larson, R. A. Further analysis of trials with
azacitidine in patients with myelodysplastic syndrome: studies 8421, 8921,
and 9221 by the Cancer and Leukemia Group B. J. Clin. Oncol. 2006,
24(24), 3895-3903.
[172] Zagonel, V.; Lo, R. G.; Marotta, G.; Babare, R.; Sardeo, G.; Gattei, V.; De,
A. V.; Monfardini, S.; Pinto, A. 5-Aza-2'-deoxycytidine (Decitabine) induces
trilineage response in unfavourable myelodysplastic syndromes. Leukemia
1993, 7(Suppl. 1), 30-35.
[173] Wijermans, P. W.; Krulder, J. W.; Huijgens, P. C.; Neve, P. Continuous
infusion of low-dose 5-Aza-2'-deoxycytidine in elderly patients with high-
risk myelodysplastic syndrome. Leukemia 1997, 11(Suppl. 1), S19-S23.
[174] Kantarjian, H.; Issa, J. P.; Rosenfeld, C. S.; Bennett, J. M.; Albitar, M.;
DiPersio, J.; Klimek, V.; Slack, J.; de Castro, C.; Ravandi, F.; Helmer, R.,
III; Shen, L.; Nimer, S. D.; Leavitt, R.; Raza, A.; Saba, H. Decitabine
improves patient outcomes in myelodysplastic syndromes: results of a phase
III randomized study. Cancer 2006, 106(8), 1794-1803.
[175] Kantarjian, H.; Oki, Y.; Garcia-Manero, G.; Huang, X.; O'Brien, S.; Cortes,
J.; Faderl, S.; Bueso-Ramos, C.; Ravandi, F.; Estrov, Z.; Ferrajoli, A.;
Wierda, W.; Shan, J.; Davis, J.; Giles, F.; Saba, H. I.; Issa, J. P. Results of a
randomized study of 3 schedules of low-dose decitabine in higher-risk
myelodysplastic syndrome and chronic myelomonocytic leukemia. Blood
2007, 109(1), 52-57.
[176] Schreiber, S. L.; Bernstein, B. E. Signaling network model of chromatin. Cell
2002, 111(6), 771-778.
[177] Dokmanovic, M.; Marks, P. A. Prospects: histone deacetylase inhibitors. J.
Cell Biochem. 2005, 96(2), 293-304.
[178] Kuendgen, A.; Strupp, C.; Aivado, M.; Bernhardt, A.; Hildebrandt, B.; Haas,
R.; Germing, U.; Gattermann, N. Treatment of myelodysplastic syndromes
with valproic acid alone or in combination with all-trans retinoic acid. Blood
2004, 104(5), 1266-1269.
[179] Kuendgen, A.; Knipp, S.; Fox, F.; Strupp, C.; Hildebrandt, B.; Steidl, C.;
Germing, U.; Haas, R.; Gattermann, N. Results of a phase 2 study of valproic
acid alone or in combination with all-trans retinoic acid in 75 patients with
myelodysplastic syndrome and relapsed or refractory acute myeloid
leukemia. Ann. Hematol. 2005, 84(Suppl. 13), 61-66.
558 Current Cancer Drug Targets, 2007, Vol. 7, No. 6 Warlick and Smith
[180] Saunthararajah, Y.; Nakamura, R.; Nam, J. M.; Robyn, J.; Loberiza, F.;
Maciejewski, J. P.; Simonis, T.; Molldrem, J.; Young, N. S.; Barrett, A. J.
HLA-DR15 (DR2) is overrepresented in myelodysplastic syndrome and
aplastic anemia and predicts a response to immunosuppression in
myelodysplastic syndrome. Blood 2002, 100(5), 1570-1574.
[181] Candoni, A.; Silvestri, F.; Buonamici, S.; Li, D.; Reddy, P.; Galili, N.;
Nucifora, G.; Raza, A. Targeted therapies in myelodysplastic syndromes:
ASH 2003 review. Semin. Hematol. 2004, 41(2 Suppl. 4), 13-20.
[182] Galili, N.; Raza, A. Immunomodulatory drugs in myelodysplastic
syndromes. Expert Opin. Investig. Drugs 2006, 15(7), 805-813.
[183] Tamilarasan, K. P.; Kolluru, G. K.; Rajaram, M.; Indhumathy, M.; Saranya,
R.; Chatterjee, S. Thalidomide attenuates nitric oxide mediated angiogenesis
by blocking migration of endothelial cells. BMC Cell Biol. 2006, 7, 17-29.
[184] Geitz, H.; Handt, S.; Zwingenberger, K. Thalidomide selectively modulates
the density of cell surface molecules involved in the adhesion cascade.
Immunopharmacology 1996, 31(2-3), 213-221.
[185] D'Amato, R. J.; Loughnan, M. S.; Flynn, E.; Folkman, J. Thalidomide is an
inhibitor of angiogenesis. Proc. Natl. Acad. Sci. USA 1994, 91(9), 4082-
4085.
[186] Mitsiades, N.; Mitsiades, C. S.; Poulaki, V.; Chauhan, D.; Richardson, P. G.;
Hideshima, T.; Munshi, N. C.; Treon, S. P.; Anderson, K. C. Apoptotic
signaling induced by immunomodulatory thalidomide analogs in human
multiple myeloma cells: therapeutic implications. Blood 2002, 99(12), 4525-
4530.
[187] Mitsuyasu, R. T.; Champlin, R. E.; Gale, R. P.; Ho, W. G.; Lenarsky, C.;
Winston, D.; Selch, M.; Elashoff, R.; Giorgi, J. V.; Wells, J. Treatment of
donor bone marrow with monoclonal anti-T-cell antibody and complement
for the prevention of graft-versus-host disease. A prospective, randomized,
double-blind trial. Ann. Intern. Med. 1986, 105(1), 20-26.
[188] Raza, A.; Meyer, P.; Dutt, D.; Zorat, F.; Lisak, L.; Nascimben, F.; du, R. M.;
Kaspar, C.; Goldberg, C.; Loew, J.; Dar, S.; Gezer, S.; Venugopal, P.; Zeldis,
J. Thalidomide produces transfusion independence in long-standing
refractory anemias of patients with myelodysplastic syndromes. Blood 2001,
98(4), 958-965.
[189] Strupp, C.; Germing, U.; Aivado, M.; Misgeld, E.; Haas, R.; Gattermann, N.
Thalidomide for the treatment of patients with myelodysplastic syndromes.
Leukemia 2002, 16(1), 1-6.
[190] Musto, P.; Falcone, A.; Sanpaolo, G.; Bisceglia, M.; Matera, R.; Carella, A.
M. Thalidomide abolishes transfusion-dependence in selected patients with
myelodysplastic syndromes. Haematologica 2002, 87(8), 884-886.
[191] Bowen, D.; MacIlwaine, L.; Cavanagh, J.; Killick, S.; Culligan, D.;
Thomson, E.; Mufti, G. Thalidomide therapy for low-risk Myelodysplasia.
Leuk. Res. 2005, 29(2), 235-236.
[192] Bouscary, D.; Legros, L.; Tulliez, M.; Dubois, S.; Mahe, B.; Beyne-Rauzy,
O.; Quarre, M. C.; Vassilief, D.; Varet, B.; Aouba, A.; Gardembas, M.;
Giraudier, S.; Guerci, A.; Rousselot, P.; Gaillard, F.; Moreau, A.; Rousselet,
M. C.; Ifrah, N.; Fenaux, P.; Dreyfus, F. A non-randomised dose-escalating
phase II study of thalidomide for the treatment of patients with low-risk
myelodysplastic syndromes: the Thal-SMD-2000 trial of the Groupe Francais
des Myelodysplasies. Br. J. Haematol. 2005, 131(5), 609-618.
[193] Corral, L. G.; Haslett, P. A.; Muller, G. W.; Chen, R.; Wong, L. M.;
Ocampo, C. J.; Patterson, R. T.; Stirling, D. I.; Kaplan, G. Differential
cytokine modulation and T cell activation by two distinct classes of
thalidomide analogues that are potent inhibitors of TNF-alpha. J. Immunol.
1999, 163(1), 380-386.
[194] Davies, F. E.; Raje, N.; Hideshima, T.; Lentzsch, S.; Young, G.; Tai, Y. T.;
Lin, B.; Podar, K.; Gupta, D.; Chauhan, D.; Treon, S. P.; Richardson, P. G.;
Schlossman, R. L.; Morgan, G. J.; Muller, G. W.; Stirling, D. I.; Anderson,
K. C. Thalidomide and immunomodulatory derivatives augment natural
killer cell cytotoxicity in multiple myeloma. Blood 2001, 98(1), 210-216.
[195] Maier, S. K.; Hammond, J. M. Role of lenalidomide in the treatment of
multiple myeloma and myelodysplastic syndrome. Ann. Pharmacother.
2006, 40(2), 286-289.
[196] List, A.; Kurtin, S.; Roe, D. J.; Buresh, A.; Mahadevan, D.; Fuchs, D.;
Rimsza, L.; Heaton, R.; Knight, R.; Zeldis, J. B. Efficacy of lenalidomide in
myelodysplastic syndromes. N. Engl. J. Med. 2005, 352(6), 549-557.
[197] Sekeres, M. A.; List, A. Immunomodulation in myelodysplastic syndromes.
Best. Pract. Res. Clin. Haematol. 2006, 19(4), 757-767.
[198] Hellstrom-Lindberg, E.; Ahlgren, T.; Beguin, Y.; Carlsson, M.; Carneskog,
J.; Dahl, I. M.; Dybedal, I.; Grimfors, G.; Kanter-Lewensohn, L.; Linder, O.;
Luthman, M.; Lofvenberg, E.; Nilsson-Ehle, H.; Samuelsson, J.; Tangen, J.
M.; Winqvist, I.; Oberg, G.; Osterborg, A.; Ost, A. Treatment of anemia in
myelodysplastic syndromes with granulocyte colony-stimulating factor plus
erythropoietin: results from a randomized phase II study and long-term
follow-up of 71 patients. Blood 1998, 92(1), 68-75.
[199] Meletis, J.; Viniou, N.; Terpos, E. Novel agents for the management of
myelodysplastic syndromes. Med. Sci. Monit. 2006, 12(9), RA194-RA206.
[200] Gore, S. D.; Baylin, S.; Sugar, E.; Carraway, H.; Miller, C. B.; Carducci, M.;
Grever, M.; Galm, O.; Dauses, T.; Karp, J. E.; Rudek, M. A.; Zhao, M.;
Smith, B. D.; Manning, J.; Jiemjit, A.; Dover, G.; Mays, A.; Zwiebel, J.;
Murgo, A.; Weng, L. J.; Herman, J. G. Combined DNA methyltransferase
and histone deacetylase inhibition in the treatment of myeloid neoplasms.
Cancer Res. 2006, 66(12), 6361-6369.
[201] Maslak, P.; Chanel, S.; Camacho, L. H.; Soignet, S.; Pandolfi, P. P.;
Guernah, I.; Warrell, R.; Nimer, S. Pilot study of combination transcriptional
modulation therapy with sodium phenylbutyrate and 5-azacitidine in patients
with acute myeloid leukemia or myelodysplastic syndrome. Leukemia 2006,
20(2), 212-217.
[202] Oka, Y.; Tsuboi, A.; Taguchi, T.; Osaki, T.; Kyo, T.; Nakajima, H.;
Elisseeva, O. A.; Oji, Y.; Kawakami, M.; Ikegame, K.; Hosen, N.;
Yoshihara, S.; Wu, F.; Fujiki, F.; Murakami, M.; Masuda, T.; Nishida, S.;
Shirakata, T.; Nakatsuka, S.; Sasaki, A.; Udaka, K.; Dohy, H.; Aozasa, K.;
Noguchi, S.; Kawase, I.; Sugiyama, H. Induction of WT1 (Wilms' tumor
gene)-specific cytotoxic T lymphocytes by WT1 peptide vaccine and the
resultant cancer regression. Proc. Natl. Acad. Sci. USA 2004, 101(38),
13885-13890.
[203] Tallman, M. S.; Andersen, J. W.; Schiffer, C. A.; Appelbaum, F. R.; Feusner,
J. H.; Ogden, A.; Shepherd, L.; Willman, C.; Bloomfield, C. D.; Rowe, J. M.;
Wiernik, P. H. All-trans-retinoic acid in acute promyelocytic leukemia. N.
Engl. J. Med. 1997, 337(15), 1021-1028.
[204] Santini, V.; Ferrini, P. R. Differentiation therapy of myelodysplastic
syndromes: fact or fiction? Br. J. Haematol. 1998, 102(5), 1124-1138.
[205] Nand, S.; Ellis, T.; Messmore, H.; Fisher, S. G.; Gaynor, E.; Fisher, R. I.
Phase II trial of recombinant human interferon alpha in myelodysplastic
syndromes. Leukemia 1992, 6(3), 220-223.
[206] Maerevoet, M.; Van Den, N. E.; Delannoy, A.; Ferrant, A.; Martiat, P.;
Bosly, A.; Fauchet, M.; Michaux, J. L. Limited activity of mini-dose
interferon alpha-2a in the treatment of myelodysplastic syndrome. Leuk.
Lymphoma 1996, 21(5-6), 519-520.
[207] Holcombe, R. F. Mini-dose interferon alpha-2a in the treatment of
myelodysplasia. Leukemia 1993, 7(2), 192-195.
[208] Elias, L.; Hoffman, R.; Boswell, S.; Tensen, L.; Bonnem, E. M. A trial of
recombinant alpha 2 interferon in the myelodysplastic syndromes: I. Clinical
results. Leukemia 1987, 1(2), 105-110.
[209] Gisslinger, H.; Chott, A.; Linkesch, W.; Fritz, E.; Ludwig, H. Long-term
alpha-interferon therapy in myelodysplastic syndromes. Leukemia 1990,
4(2), 91-94.
[210] Motomura, S.; Kanamori, H.; Maruta, A.; Kodama, F.; Ohkubo, T. The
effect of 1-hydroxyvitamin D3 for prolongation of leukemic transformation-
free survival in myelodysplastic syndromes. Am. J. Hematol. 1991, 38(1),
67-68.
[211] Koeffler, H. P.; Aslanian, N.; O'Kelly, J. Vitamin D(2) analog (Paricalcitol;
Zemplar) for treatment of myelodysplastic syndrome. Leuk. Res. 2005,
29(11), 1259-1262.
[212] Mellibovsky, L.; Diez, A.; Perez-Vila, E.; Serrano, S.; Nacher, M.; Aubia, J.;
Supervia, A.; Recker, R. R. Vitamin D treatment in myelodysplastic
syndromes. Br. J. Haematol. 1998, 100(3), 516-520.
[213] Ganser, A.; Seipelt, G.; Verbeek, W.; Ottmann, O. G.; Maurer, A.; Kolbe,
K.; Hess, U.; Elsner, S.; Reutzel, R.; Wormann, B. Effect of combination
therapy with all-trans-retinoic acid and recombinant human granulocyte
colony-stimulating factor in patients with myelodysplastic syndromes.
Leukemia 1994, 8(3), 369-375.
[214] Hofmann, W. K.; Ganser, A.; Seipelt, G.; Ottmann, O. G.; Zander, C.;
Geissler, G.; Hoffmann, K.; Hoffken, K.; Fischer, J. T.; Isele, G.; Hoelzer, D.
Treatment of patients with low-risk myelodysplastic syndromes using a
combination of all-trans retinoic acid, interferon alpha, and granulocyte
colony-stimulating factor. Ann. Hematol. 1999, 78(3), 125-130.
[215] Matsui, W. H.; Gladstone, D. E.; Vala, M. S.; Barber, J. P.; Brodsky, R. A.;
Smith, B. D.; Jones, R. J. The role of growth factors in the activity of
pharmacological differentiation agents. Cell Growth Differ. 2002, 13(6), 275-
283.
[216] Matsui, W.; Huff, C. A.; Vala, M.; Barber, J.; Smith, B. D.; Jones, R. J. Anti-
tumour activity of interferon-alpha in multiple myeloma: role of interleukin 6
and tumor cell differentiation. Br. J. Haematol. 2003, 121(2), 251-258.
[217] Matsui, W.; Smith, B. D.; Vala, M.; Beal, N.; Huff, C. A.; Diehl, L. F.;
Jones, R. J. Requirement for myeloid growth factors in the differentiation of
acute promyelocytic leukaemia. Br. J. Haematol. 2005, 128(6), 853-862.
[218] Williams, C. D.; Linch, D. C.; Watts, M. J.; Thomas, N. S. Characterization
of cell cycle status and E2F complexes in mobilized CD34+ cells before and
after cytokine stimulation. Blood 1997, 90(1), 194-203.
[219] Williams, G. T.; Smith, C. A.; Spooncer, E.; Dexter, T. M.; Taylor, D. R.
Haemopoietic colony stimulating factors promote cell survival by
suppressing apoptosis. Nature 1990, 343(6253), 76-79.
Received: November 08, 2006 Revised: April 03, 2007 Accepted: April 09, 2007
You might also like
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Cancer Epigenetics - New Therapies and New ChallengesDocument9 pagesCancer Epigenetics - New Therapies and New ChallengesVaithya NathanNo ratings yet
- Private Label Rights for Dealing With LonelinessDocument1 pagePrivate Label Rights for Dealing With LonelinessVaithya NathanNo ratings yet
- F 1639 CMT Azacitidine A Review of Its Use in The Management of Myelodysplastic .PDF 2244Document9 pagesF 1639 CMT Azacitidine A Review of Its Use in The Management of Myelodysplastic .PDF 2244Vaithya NathanNo ratings yet
- Aml - BJH - 2006 Guidelines in AmlDocument25 pagesAml - BJH - 2006 Guidelines in AmlVaithya NathanNo ratings yet
- Epi 8 561Document10 pagesEpi 8 561Vaithya NathanNo ratings yet
- Wide-Spectrum Characterization of TrabectedinDocument14 pagesWide-Spectrum Characterization of TrabectedinVaithya NathanNo ratings yet
- 7MDS Novel TherapyDocument70 pages7MDS Novel TherapyVaithya NathanNo ratings yet
- 13-Leukemia & Lymphoma-Methylation of Promoters of MicroRNAs and Their Host Genes in Myelodysplastic SyndromesDocument20 pages13-Leukemia & Lymphoma-Methylation of Promoters of MicroRNAs and Their Host Genes in Myelodysplastic SyndromesVaithya NathanNo ratings yet
- 280 2011 Article 1697Document10 pages280 2011 Article 1697Vaithya NathanNo ratings yet
- Clearing Your Root Chakra To Banish Fear and Anxiety From Your LifeDocument4 pagesClearing Your Root Chakra To Banish Fear and Anxiety From Your LifeVaithya Nathan0% (1)
- Et 743 1606Document9 pagesEt 743 1606Vaithya NathanNo ratings yet
- 673Document9 pages673Vaithya NathanNo ratings yet
- HBV Therapy During PregnancyDocument9 pagesHBV Therapy During PregnancyVaithya NathanNo ratings yet
- Kalidas ADocument121 pagesKalidas AVaithya NathanNo ratings yet
- Vethathiri - Mind ManagementDocument10 pagesVethathiri - Mind ManagementProf. Madhavan100% (1)
- ThirumandiramDocument150 pagesThirumandiramVaithya NathanNo ratings yet
- Obesity and Female Reproductive FunctionDocument18 pagesObesity and Female Reproductive FunctionVaithya NathanNo ratings yet
- Varahi Krama: Panchaanga NyasamDocument9 pagesVarahi Krama: Panchaanga Nyasamopenid_cRw9IB6K100% (1)
- Consciousness BibliographyDocument500 pagesConsciousness BibliographyVaithya NathanNo ratings yet
- Writing Effectively and PowerfullyDocument38 pagesWriting Effectively and PowerfullynunaazulNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Full SyllabusDocument409 pagesFull SyllabusSanthana BharathiNo ratings yet
- Interface GSKTMTRLBRCHR A4 Int 4webDocument7 pagesInterface GSKTMTRLBRCHR A4 Int 4webROGERIO GUILHERME DE OLIVEIRA MARQUESNo ratings yet
- UMR Introduction 2023Document110 pagesUMR Introduction 2023tu reves mon filsNo ratings yet
- Dip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Document1 pageDip Obst (SA) Past Papers - 2020 1st Semester 1-6-2023Neo Latoya MadunaNo ratings yet
- Book 1Document94 pagesBook 1JOHNNo ratings yet
- Chapter 5Document16 pagesChapter 5Ankit GuptaNo ratings yet
- Grab Go Porter S 5 ForcesDocument2 pagesGrab Go Porter S 5 ForcesUtkarsh SharmaNo ratings yet
- Supply Chain Management of VodafoneDocument8 pagesSupply Chain Management of VodafoneAnamika MisraNo ratings yet
- Job Satisfaction RRLDocument39 pagesJob Satisfaction RRLMarie Tiffany100% (1)
- Esaote MyLabX7Document12 pagesEsaote MyLabX7Neo BiosNo ratings yet
- Quality ImprovementDocument3 pagesQuality ImprovementViky SinghNo ratings yet
- Solids Level Measurement Application Guide en 78224 PDFDocument144 pagesSolids Level Measurement Application Guide en 78224 PDFwalcalNo ratings yet
- 9 To 5 Props PresetsDocument4 pages9 To 5 Props Presetsapi-300450266100% (1)
- Past The Shallows EssayDocument2 pagesPast The Shallows EssaycaitlinNo ratings yet
- EP Series User Manual PDFDocument40 pagesEP Series User Manual PDFa.elwahabNo ratings yet
- Tugas B InggrisDocument9 pagesTugas B InggrisDellyna AlmaNo ratings yet
- Puskesmas Dua Puluh Tiga Ilir Publishes Vaccination Ticket ListDocument98 pagesPuskesmas Dua Puluh Tiga Ilir Publishes Vaccination Ticket ListLaboratorium PKM 23 IlirNo ratings yet
- ME JBP 70A Pen Dissolved Oxygen Meter PDFDocument1 pageME JBP 70A Pen Dissolved Oxygen Meter PDFpiknikmonsterNo ratings yet
- Hinduism Today April May June 2015Document43 pagesHinduism Today April May June 2015jpmahadevNo ratings yet
- Analysis of Heavy Metals Concentration in Landfill Soil IJERTV8IS120019Document2 pagesAnalysis of Heavy Metals Concentration in Landfill Soil IJERTV8IS120019Eustache NIJEJENo ratings yet
- OC - PlumberDocument6 pagesOC - Plumbertakuva03No ratings yet
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- Vaginal Examinations in Labour GuidelineDocument2 pagesVaginal Examinations in Labour GuidelinePooneethawathi Santran100% (1)
- Female Reproductive System Histology IDocument5 pagesFemale Reproductive System Histology ISolomon Seth SallforsNo ratings yet
- Aplikasi Berbagai Jenis Media Dan ZPT Terhadap Aklimatisasi Anggrek VandaDocument15 pagesAplikasi Berbagai Jenis Media Dan ZPT Terhadap Aklimatisasi Anggrek VandaSihonoNo ratings yet
- Affidavit of Consent For Shared Parental AuthorityDocument2 pagesAffidavit of Consent For Shared Parental AuthorityTet LegaspiNo ratings yet
- Block 1 Board Review - Lecture NotesDocument127 pagesBlock 1 Board Review - Lecture NotesCece RereNo ratings yet
- Case Report on Right Knee FuruncleDocument47 pagesCase Report on Right Knee Furuncle馮宥忻No ratings yet
- Reading and Listening 2Document4 pagesReading and Listening 2Hải Anh TạNo ratings yet
- To The OneDocument8 pagesTo The OnePizzaCowNo ratings yet