Professional Documents
Culture Documents
Exposure Factors: DR Hussein Ahmed Hassan
Uploaded by
chowhk0 ratings0% found this document useful (0 votes)
16 views39 pagesexposurefactors2-131218145159-phpapp02.pdf
Original Title
exposurefactors2-131218145159-phpapp02
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentexposurefactors2-131218145159-phpapp02.pdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views39 pagesExposure Factors: DR Hussein Ahmed Hassan
Uploaded by
chowhkexposurefactors2-131218145159-phpapp02.pdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 39
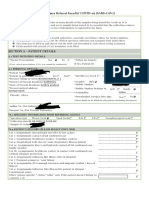
EXPOSURE FACTORS
DR Hussein Ahmed Hassan
Exposure factors are factors that control
density (blackening) and contrast of
radiographic image.
They are some of the tools that
technologists use to create high-quality
radiographs
Exposure Factors Controlled by the
Operator
kVp
mA times Exposure Time = mAs
Determines the quality and quantity of
the exposure
FFD (SID), Focal Spot and Filtration are
secondary factors
1- EXPOSURE FACTORS:
KVP. :
It controls the quality of the beam, i.e.
PENETRATION.
It influences :
a: penetration power, i.e. beam quality;
kVp. penetration power.
b: Radiographic contrast;
kVp. 1/radiographic contrast.
c: Radiation dose to patient.
kVp. 1/radiation dose.
KVP
kVp controls radiographic contrast.
kVp determines the ability for the beam
to penetrate the tissue.
kVp has more effect than any other
factor on image receptor exposure
because it affects beam quality.
KVP
To a lesser extent it also influences the
beam quantity.
As we increase kVp, more of the beam
penetrates the tissue with higher energy
so they interact more by the Compton
effect.
This produces more scatter radiation
which increases image noise and
reduces contrast.
KVP
50 kV 79% is photoelectric, 21%
Compton, < 1% no interaction
80 kVp 46% is photoelectric, 52%
Compton 2% no interaction
110 kVp 23% photoelectric, 70%
Compton, 7% no interaction
As no interaction increases, less
exposure is needed to produce the
image so patient exposure is decreased.
High kVp.
low radiographic contrast
Low kVp.
High radiographic contrast
MA.:
1 Ampere = 1 C/s = 6.3 x 1018 electrons/
second.
The mA selected for the exposure
determines the number of x-rays
produced.
The number of x-rays are directly
proportional to the mA assuming a fixed
exposure time.
100 mA produced half the x-ray that 200
mA would produce.
MA
Patient dose is also directly proportional
to the mA with a fixed exposure time.
A change in mA does not affect kinetic
energy of the electrons therefore only
the quantity is changed.
MA
Many x-ray machines are identified by
the maximum mA or mAs available.
A MP 500 has a maximum mAs of 500
mAs.
A Universal 325 has a maximum mA of
300 and maximum kVp of 125
MA
More expensive three phase machines
will have a higher maximum mA.
A General Electric MST 1050 would have
1000 mA and 150 kVp.
EXPOSURE TIME
The exposure time is generally always
kept as short as possible.
This is not to reduce patient exposure
but to minimize motion blur resulting
from patient movement.
This is a much greater problem with
weight bearing radiography.
EXPOSURE TIME
Older machine express time as a
fraction.
Newer machines express exposure time
as milliseconds (ms)
It is easy to identify the type of high
voltage generation by looking at the
shortest exposure time.
EXPOSURE TIME
Single phase half wave rectified fasted
exposure time is 1/60 second 17 ms.
Single phase full wave rectified fastest
exposure time is 1/120 second or 8 ms
Three phase and high frequency can
provide exposure time down to 1 ms.
(4) MAS. :
It affect the total number of x-ray
produced by the tube during exposure, i.e.
QUANTITY.
It is the product of two quantities;
mA. the tube current;
s. the exposure time;
MAS
mA and exposure time is usually
combined and used as one factor
expressed as mAs.
mAs controls radiation quantity, optical
density and patient dose.
mAs determine the number of x-rays in
the beam and therefore radiation
quantity.
mAs does not influence radiation quality.
MAS
Any combination of mA and time that will
give the same mAs should provide the
same optical density on the film. This is
referred to as the reciprocity law.
As noted earlier for screen film
radiography, 1 ms exposure and
exposure longer than 1 seconds do not
follow this rule.
MAS
On many modern machines, only mAs
can be selected. The machine
automatically gives the operator the
highest mA and shortest exposure time.
The operator may be able to select mA
by what is referred to as Power level.
MAS
mAs is one way to measure electrostatic
charge. It determines the total number
of electrons.
Only the quantity of the photons are
affected by changes in the mAs.
Patient dose is therefore a function of
mAs.
20 mA. X 1.0 s = 20 mAs
40 mA. X 0.5 s = 20 mAs
80 mA. X 0.25 s = 20 mAs
200 mA. X 0.1 s = 20 mAs
400 mA. X 0.05s = 20 mAs
Ampere is 1 coulomb (C) of electrostatic
charge flowing each second.
1A = 1C/s = 6.3 X 10
18
electron/s
20 mAs = 0.2 Amperes.
This charge releases this No. of electrons:
6.3 X 10
18
X 0.2 = 1.26 X 10
18
electron/s
(5) Focal spot:
Most x-ray tubes offer two focal spot
sizes:
a. Fine focus:
b. Broad focus:
a/ Fine focus: (0.3 0.6 mm
2
)
It records fine details.
It can not withstand too much heat.
Its usage may require long exposure
time.
Used whenever geometric factors are
more (long subject-film distance, short
FFD ... etc).
a/ Broad focus: (0.6 1.2 mm
2
)
It can withstand too much heat.
Always used in combination with short
(s) and fast film/screen system.
Used whenever voluntary or
involuntary motion is highly expected.
Used when radiosensitive organ is
within exposed area or 10 cm from
collimation border.
Two focal spot
FOCAL SPOT SIZE
The focal spot size limits the tubes
capacity to produce x-rays. The
electrons and resulting heat are
placed on a smaller portion of the
x-ray tube.
The mA is therefore limited for the
small focal spot. This results in
longer exposure times with greater
chance of patient movement.
FOCAL SPOT SIZE
If the mA is properly calibrated, the
focal spot will have no impact on the
quantity or quality of the beam.
(6) F.F.D. :
The intensity of x-ray beam reduces with
increased FFD.
It follows the Inverse Square Law ( I.S.L.) .
I 1/d
2
.
DISTANCE
Distance affects the intensity of the x-
ray beam at the film but has no effect on
radiation quality.
Distance affects the exposure of the
image receptor according to the inverse
square law.
INVERSE SQUARE LAW
mAs (second exposure) SID2 2nd exposure
---------------------------- = ------------------------
mAs (first exposure) SID2 1st exposure
DISTANCE
The most common source to image
distances are 40 (100 cm) and 72(182
cm)
Since SID does not impact the quality of
the beam, adjustments to the technical
factors are made with the mAs.
To go from 40 to 72 increase the mAs
3.5 time.
DISTANCE
Increasing the distance will impact the
geometric properties of the beam.
Increased SID reduces magnification
distortion and focal spot blur.
With the need to increase the mAs 3.5
times for the 72 SID, tube loading
becomes a concern.
DISTANCE
72 SID is used for Chest radiography
and the lateral cervical spine to reduce
magnification.
72 SID used for the full spine to get a
36 beam.
(7) FILTERATION:
Thin sheet of Al (aluminum) 1mm or 2mm
thick added to the pathway of radiation to
filter the low energy radiation.
Increasing filtration will increase the
quality and reduce the quantity of the
beam.
It removes low energy radiation:
Reduce skin dose;
Harden the beam;
FILTRATION
All x-ray beams are affected by the
filtration of the tube. The tube housing
provides about 0.5 mm of filtration.
Additional filtration is added in the
collimator to meet the 2.5 mm of
aluminum minimum filtration required by
law.
2.5 mm is required for 70 kVp.
FILTRATION
3.0 mm is required for at 100 kVp.
3.2 mm is required for operations at 120
kVp.
Most machines now are capable of over
100 kVp operation.
We have no control on these filters.
FILTRATION
3.0 mm is required for at 100 kVp.
3.2 mm is required for operations at
120 kVp.
Most machines now are capable of
over 100 kVp operation.
We have no control on these filters.
FILTRATION
CHIROPRACTIC RADIOGRAPHY IS A LEADER IN
THE USE OF COMPENSATING FILTERS. WE
HAVE TOTAL CONTROL OVER COMPENSATING
FILTRATION.
IN AREAS OF THE BODY WITH HIGH SUBJECT
CONTRAST OR WIDE DIFFERENCES IN DENSITY,
COMPENSATING FILMS IMPROVE IMAGE
QUALITY AND REDUCE PATIENT EXPOSURE.
THE END
You might also like
- Measurement While Drilling: Signal Analysis, Optimization and DesignFrom EverandMeasurement While Drilling: Signal Analysis, Optimization and DesignNo ratings yet
- 7 - Individual Limits For Member of The Public-8Document15 pages7 - Individual Limits For Member of The Public-8Bashar BassamNo ratings yet
- Radiographic TechniqueDocument40 pagesRadiographic TechniqueShan Angelie SarmientoNo ratings yet
- Radiographic ExposureDocument70 pagesRadiographic ExposurechowhkNo ratings yet
- Chapter 013Document2 pagesChapter 013Zaid juttNo ratings yet
- Chapter 13 Radiographic TechniqueDocument9 pagesChapter 13 Radiographic TechniqueCziara JustineNo ratings yet
- Technical Proficiency CriteriaDocument61 pagesTechnical Proficiency CriteriaMOHD AZUAN ABDUL RASHIDNo ratings yet
- Beam Therapy Equipment I Cobalt KV Xray Feb 2015Document65 pagesBeam Therapy Equipment I Cobalt KV Xray Feb 2015Lê Thị Thu TâmNo ratings yet
- 2021 3528 Moesm1 EsmDocument30 pages2021 3528 Moesm1 Esm1356055749No ratings yet
- Applied Lasers: Although Basically Research Certain Specific Communication or For Communication Across TheDocument5 pagesApplied Lasers: Although Basically Research Certain Specific Communication or For Communication Across TheTaha Al-abedNo ratings yet
- Successful Intraoral RadiographyDocument19 pagesSuccessful Intraoral RadiographyMonica Agustine HartonoNo ratings yet
- Factors Influencing The X-Ray BeamDocument17 pagesFactors Influencing The X-Ray BeambontleNo ratings yet
- Topic 2 RT202Document27 pagesTopic 2 RT202allexa jimlaniNo ratings yet
- Acelerador Lineal Alta Energía IXDocument16 pagesAcelerador Lineal Alta Energía IXChristina OsbornNo ratings yet
- MIT X-Ray Laser ProjectDocument47 pagesMIT X-Ray Laser ProjectWiji AstutiNo ratings yet
- TT - Ultrashort Laser PulsesDocument19 pagesTT - Ultrashort Laser Pulsesbiomed41No ratings yet
- David E. Moncton - An X-Ray Laser at The Transform Limit: Technical Challenges and Scientific PayoffDocument35 pagesDavid E. Moncton - An X-Ray Laser at The Transform Limit: Technical Challenges and Scientific PayoffDublin000No ratings yet
- Vet Cardiology and Radiology Equipment OverviewDocument4 pagesVet Cardiology and Radiology Equipment OverviewTiti DarabanNo ratings yet
- X Ray Tube Warm-Up ProcedureDocument4 pagesX Ray Tube Warm-Up Procedureleul TizazuNo ratings yet
- Quiz ReviewerDocument3 pagesQuiz ReviewerJerick JusayNo ratings yet
- SUN MON TUE WED THU FRI SAT: - Rays Are Produce by Electron DecelerationDocument6 pagesSUN MON TUE WED THU FRI SAT: - Rays Are Produce by Electron DecelerationapollyonmdNo ratings yet
- Microwave 1Document37 pagesMicrowave 1Kennedy MutaiNo ratings yet
- LinacDocument16 pagesLinacLomombNo ratings yet
- Chapter 8 X-Ray EmissionDocument8 pagesChapter 8 X-Ray EmissionMegNo ratings yet
- Topic 6Document2 pagesTopic 6Rabia BagewadiNo ratings yet
- Notebook 1Document3 pagesNotebook 1api-340731900No ratings yet
- 7 Designing For Radiation ProtectionDocument45 pages7 Designing For Radiation ProtectionAngelo RamosNo ratings yet
- Apd Intro JraDocument8 pagesApd Intro JraIftekher1175No ratings yet
- Technique Charts RadtechDocument17 pagesTechnique Charts RadtechJenica Mandagan100% (1)
- Prime Factors of Radiographic ExposureDocument3 pagesPrime Factors of Radiographic ExposureThilak raj SNo ratings yet
- Radiography Testing GuideDocument63 pagesRadiography Testing GuideBhavani Prasad100% (2)
- SemifinalsDocument51 pagesSemifinalsmaricar paracadNo ratings yet
- Exposure Chart Mobile X Ray PDFDocument8 pagesExposure Chart Mobile X Ray PDFlutfiaNo ratings yet
- Characterization of A High-Power Erbium-Doped Fiber LaserDocument4 pagesCharacterization of A High-Power Erbium-Doped Fiber Laserwarse1No ratings yet
- Echelle Monochromators ExplainedDocument105 pagesEchelle Monochromators Explainedyogeshsingh15No ratings yet
- Radiology ReviewDocument52 pagesRadiology ReviewFourthMolar.com50% (2)
- Spectrophotometric Stud Ies of Ultra Low Loss Optical Glasses II: Double Beam MethodDocument5 pagesSpectrophotometric Stud Ies of Ultra Low Loss Optical Glasses II: Double Beam MethodMSKNo ratings yet
- Radiographic InterpretationDocument34 pagesRadiographic InterpretationAzim SukimanNo ratings yet
- Control of Sactter Radiation Week 9Document62 pagesControl of Sactter Radiation Week 9Rupali SinghNo ratings yet
- Process sequence of the lithography processDocument176 pagesProcess sequence of the lithography processlinjefNo ratings yet
- If There Are Images IDocument4 pagesIf There Are Images ISaurav BansalNo ratings yet
- CMOS ScalingDocument19 pagesCMOS ScalingnsrkntNo ratings yet
- 2session 27 Overview: Biomedical CircuitsDocument26 pages2session 27 Overview: Biomedical CircuitsGiang HoaiNo ratings yet
- Radar Performance FactorsDocument10 pagesRadar Performance FactorsCodruţ ErașcuNo ratings yet
- X Ray EmissionDocument66 pagesX Ray EmissiondanasardyNo ratings yet
- Physics Mentoring 2Document28 pagesPhysics Mentoring 2Cziara JustineNo ratings yet
- UEMB3244 Tutorial 3QDocument2 pagesUEMB3244 Tutorial 3QYee Kai TeeNo ratings yet
- Notebook 13Document1 pageNotebook 13api-338661748No ratings yet
- CBM355 Medical Imaging Systems 2-MarksDocument23 pagesCBM355 Medical Imaging Systems 2-Markssanthosh sekar100% (2)
- 8.4.4 - Radiographic Training ProgramDocument31 pages8.4.4 - Radiographic Training ProgramMaduabuchi Serge Enemuo100% (1)
- Art Versus Science4Document11 pagesArt Versus Science4wilcodpNo ratings yet
- X-Ray Data Booklet Section 4.5 X-RAY DETECTORS: Albert C. ThompsonDocument5 pagesX-Ray Data Booklet Section 4.5 X-RAY DETECTORS: Albert C. ThompsonRajul PandeyNo ratings yet
- MUCLecture_2023_10755503Document5 pagesMUCLecture_2023_10755503sanyengereNo ratings yet
- Titanium Sapphire Lasers and Femtosecond LasersDocument25 pagesTitanium Sapphire Lasers and Femtosecond LasersaliflailasurumiNo ratings yet
- Notes On Radn and RadioactivityDocument7 pagesNotes On Radn and RadioactivityYael Opeña AlipNo ratings yet
- Peter R. Herman Et Al - Laser Micromachining of 'Transparent' Fused Silica With 1-ps Pulses and Pulse TrainsDocument8 pagesPeter R. Herman Et Al - Laser Micromachining of 'Transparent' Fused Silica With 1-ps Pulses and Pulse TrainsPocxaNo ratings yet
- RT 203 Principles of Imaging 32 62Document31 pagesRT 203 Principles of Imaging 32 62Bea SeloterioNo ratings yet
- Introduction To X-RaysDocument4 pagesIntroduction To X-RaysRoberto HermenegildoNo ratings yet
- Absorption of Gamma RaysDocument9 pagesAbsorption of Gamma RaysRachit KanchanNo ratings yet
- MACC Chief: Graft is Malaysia's Public Enemy No. 1Document2 pagesMACC Chief: Graft is Malaysia's Public Enemy No. 1chowhkNo ratings yet
- Short-Term Assistance For Those Left VulnerableDocument1 pageShort-Term Assistance For Those Left VulnerablechowhkNo ratings yet
- Barisan Nasional Would Do All in Its Power To Help IndiansDocument1 pageBarisan Nasional Would Do All in Its Power To Help IndianschowhkNo ratings yet
- TNB Announces Record Dividend Payout of RM3Document2 pagesTNB Announces Record Dividend Payout of RM3chowhkNo ratings yet
- Siti Kasim Blasts Syed Saddiq Over Oktoberfest PetitionDocument1 pageSiti Kasim Blasts Syed Saddiq Over Oktoberfest PetitionchowhkNo ratings yet
- LoudDocument2 pagesLoudchowhkNo ratings yet
- MACC Teams Visit Six Offices To Gather Evidence On Kuching Luxury Hotel PurchaseDocument3 pagesMACC Teams Visit Six Offices To Gather Evidence On Kuching Luxury Hotel PurchasechowhkNo ratings yet
- PM: Economy Still GrowingDocument2 pagesPM: Economy Still GrowingchowhkNo ratings yet
- Allardyce Sues FA for Damages Over SackingDocument1 pageAllardyce Sues FA for Damages Over SackingchowhkNo ratings yet
- 15 Missing After Boat Loses Contact Off SarawakDocument1 page15 Missing After Boat Loses Contact Off SarawakchowhkNo ratings yet
- Cells at LockDocument1 pageCells at LockchowhkNo ratings yet
- Malaysians Travelling More Despite UncertaintiesDocument1 pageMalaysians Travelling More Despite UncertaintieschowhkNo ratings yet
- Surface Preparation Standards Comparison ChartDocument2 pagesSurface Preparation Standards Comparison ChartajuhaseenNo ratings yet
- Thrill Jet Boat Rides Now Available in Tanjung AruDocument1 pageThrill Jet Boat Rides Now Available in Tanjung AruchowhkNo ratings yet
- Fluid CodeDocument1 pageFluid CodechowhkNo ratings yet
- Business Process DocumentDocument7 pagesBusiness Process DocumentAnneMangsat50% (2)
- 9 Practical Cswip 3.0 Practical Visual Inspection PDFDocument13 pages9 Practical Cswip 3.0 Practical Visual Inspection PDFAzim Samiin77% (13)
- Is Crayon Shin-Chan The Bad Boy of MangaDocument3 pagesIs Crayon Shin-Chan The Bad Boy of MangachowhkNo ratings yet
- 17915Document11 pages17915chowhkNo ratings yet
- 17915Document11 pages17915chowhkNo ratings yet
- 古穿今之天后来袭Document282 pages古穿今之天后来袭chowhkNo ratings yet
- 111523Document12 pages111523chowhkNo ratings yet
- PCN Level III BrochureDocument5 pagesPCN Level III Brochuremayav1100% (1)
- Building A SystemDocument24 pagesBuilding A SystemchowhkNo ratings yet
- Gmaw Fcaw Mcaw WeldingDocument4 pagesGmaw Fcaw Mcaw Weldingsajeed76743031No ratings yet
- Generating A Photogrammetric Model UsingDocument5 pagesGenerating A Photogrammetric Model UsingchowhkNo ratings yet
- (15 12 07) (11 55 47) PDFDocument2 pages(15 12 07) (11 55 47) PDFchowhkNo ratings yet
- Qas 4 05 Welding Heat Treatment 082914Document7 pagesQas 4 05 Welding Heat Treatment 082914chowhkNo ratings yet
- Key Criteria For Matching Filler Metals To Your Base MaterialDocument3 pagesKey Criteria For Matching Filler Metals To Your Base MaterialchowhkNo ratings yet
- Austenitic Stainless Steel CompositionDocument10 pagesAustenitic Stainless Steel Compositionrajmv7No ratings yet
- A. Lesson Preview / Review: This Document Is The Property of PHINMA EDUCATIONDocument11 pagesA. Lesson Preview / Review: This Document Is The Property of PHINMA EDUCATIONTherese Anne ArmamentoNo ratings yet
- PREXC Operational Definition and Targets CY 2019 - 2020Document12 pagesPREXC Operational Definition and Targets CY 2019 - 2020iamaj8No ratings yet
- IEEE802.11b/g High Power Wireless AP/Bridge Quick Start GuideDocument59 pagesIEEE802.11b/g High Power Wireless AP/Bridge Quick Start GuideonehotminuteNo ratings yet
- 2746 PakMaster 75XL Plus (O)Document48 pages2746 PakMaster 75XL Plus (O)Samuel ManducaNo ratings yet
- Astm D 4417Document4 pagesAstm D 4417Javier Celada0% (1)
- Cowell - The Wizards of Once PDFDocument315 pagesCowell - The Wizards of Once PDFtatoes n lases100% (1)
- CotomDocument8 pagesCotommuangawaNo ratings yet
- Robotics: Let's Talk About Robots!Document5 pagesRobotics: Let's Talk About Robots!Elizaveta KononovaNo ratings yet
- FINANCIAL REPORTSDocument34 pagesFINANCIAL REPORTSToni111123No ratings yet
- Q3 SolutionDocument5 pagesQ3 SolutionShaina0% (1)
- EPON ONU with 4FE+WiFi EONU-04WDocument4 pagesEPON ONU with 4FE+WiFi EONU-04WAndres Alberto ParraNo ratings yet
- Barcode BasicsDocument3 pagesBarcode Basicsnikhilbajpai_88No ratings yet
- Cambridge IGCSE: Combined Science 0653/41Document24 pagesCambridge IGCSE: Combined Science 0653/41jesslynaureliaNo ratings yet
- Year 7 Bugs Lesson 2Document1 pageYear 7 Bugs Lesson 2api-293503824No ratings yet
- Transferring Maps To Your Mobile Device (Avenza PDF Maps) : For Apple Products (Ipad, Iphone, Ios)Document2 pagesTransferring Maps To Your Mobile Device (Avenza PDF Maps) : For Apple Products (Ipad, Iphone, Ios)m.naufal nurrahmanNo ratings yet
- Sample Id: Sample Id: 6284347 Icmr Specimen Referral Form Icmr Specimen Referral Form For For Covid-19 (Sars-Cov2) Covid-19 (Sars-Cov2)Document2 pagesSample Id: Sample Id: 6284347 Icmr Specimen Referral Form Icmr Specimen Referral Form For For Covid-19 (Sars-Cov2) Covid-19 (Sars-Cov2)Praveen KumarNo ratings yet
- NWQSR - BodyDocument56 pagesNWQSR - BodyRonnie EncarnacionNo ratings yet
- Sample Prayer For Final Thesis DefenseDocument6 pagesSample Prayer For Final Thesis Defensefjfyj90y100% (2)
- "Network Security": Alagappa UniversityDocument1 page"Network Security": Alagappa UniversityPRADEEPRAJANo ratings yet
- RCD-GillesaniaDocument468 pagesRCD-GillesaniaJomarie Alcano100% (2)
- Connect 4 UML Class DiagramDocument1 pageConnect 4 UML Class DiagramDuy Nguyễn Văn NhậtNo ratings yet
- LQRDocument34 pagesLQRkemoNo ratings yet
- Drainage Manual: State of Florida Department of TransportationDocument78 pagesDrainage Manual: State of Florida Department of TransportationghoyarbideNo ratings yet
- To Quantitative Analysis: To Accompany by Render, Stair, Hanna and Hale Power Point Slides Created by Jeff HeylDocument94 pagesTo Quantitative Analysis: To Accompany by Render, Stair, Hanna and Hale Power Point Slides Created by Jeff HeylNino NatradzeNo ratings yet
- 12 Orpic Safety Rules Managers May 17 RevDocument36 pages12 Orpic Safety Rules Managers May 17 RevGordon Longforgan100% (3)
- Region VIII - Eastern Visayas Quickstat On: Philippine Statistics AuthorityDocument3 pagesRegion VIII - Eastern Visayas Quickstat On: Philippine Statistics AuthorityBegie LucenecioNo ratings yet
- D-2 UTEP Currey Final ReportDocument23 pagesD-2 UTEP Currey Final ReporthmcNo ratings yet
- GI6.020 Personal Flotation Devices (PFDS) 10-31-2009Document5 pagesGI6.020 Personal Flotation Devices (PFDS) 10-31-2009GooglegulNo ratings yet
- H2 Physic 2010 A Level SolutionsDocument32 pagesH2 Physic 2010 A Level Solutionsonnoez50% (4)
- SAC SINGLAS Accreditation Schedule 15 Apr 10Document5 pagesSAC SINGLAS Accreditation Schedule 15 Apr 10clintjtuckerNo ratings yet