Professional Documents
Culture Documents
Functional (Non-Ulcer) Dyspepsia and Gastroesophageal Refl Ux Disease: One Not Two Diseases ?
Uploaded by
Reynalth Andrew Sinaga0 ratings0% found this document useful (0 votes)
12 views3 pagesHeartburn and regurgitation occur frequently in functional dyspepsia, even after objective gastroesophageal reflux disease has been exhaustively excluded. Heartburn and acid regurgitation are considered classical gastroesphagageal refux disease (GERD) symptoms.
Original Description:
Original Title
ajg2013102a
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHeartburn and regurgitation occur frequently in functional dyspepsia, even after objective gastroesophageal reflux disease has been exhaustively excluded. Heartburn and acid regurgitation are considered classical gastroesphagageal refux disease (GERD) symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
12 views3 pagesFunctional (Non-Ulcer) Dyspepsia and Gastroesophageal Refl Ux Disease: One Not Two Diseases ?
Uploaded by
Reynalth Andrew SinagaHeartburn and regurgitation occur frequently in functional dyspepsia, even after objective gastroesophageal reflux disease has been exhaustively excluded. Heartburn and acid regurgitation are considered classical gastroesphagageal refux disease (GERD) symptoms.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
775
2013 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
nature publishing group 775
see related article on page 767
S
T
O
M
A
C
H
EDITORIAL
Abstract: Functional dyspepsia is a very common,
distressful, and costly condition. New data
indicate that heartburn and regurgitation occur
frequently in functional dyspepsia, even after
objective gastroesophageal reux disease has
been exhaustively excluded by appropriate testing.
Arbitrarily excluding heartburn in functional
dyspepsia studies appears misguided.
Am J Gastroenterol 2013; 108:775 777; doi: 10.1038/ajg.2013.102
Dyspepsia and refux symptoms are both remarkably common and
tend to travel together; in a telephone survey of over 21,000 adults
in the United States, the three most prevalent symptoms occur-
ring at least once a month were early satiety (reported by 23 % ),
heartburn (22 % ), and postprandial fullness (21 % ) ( 1 ). Heartburn
(a burning rising retosternal discomfort) and acid regurgitation
are considered classical gastroesophageal refux disease (GERD)
symptoms, which typically arise when abnormally increased tran-
sient lower esophageal sphincter relaxations allow gastric acid to
reach the distal esophagus. In GERD gastroduodenal dysfunction
is not thought to be of major relevance, although a subset also
have gastric emptying delay ( 2 ). Patients ofen do not know what
the word dyspepsia means and one might argue many physicians
do not either; dyspepsia is not uniformly defned in the literature
( 3,4 ). In the United Kingdom, dyspepsia refers to epigastric pain,
heartburn, or any other upper gastrointestinal (GI) symptom ( 4 )
which is not terribly useful. Some physicians still use really vague
terms such as gastritis (or worse gastropathy) to describe symp-
toms thought to arise from the gastroduodenal region ( 3,4 ).
Te current international Rome III consensus, based on expert
opinion, is that dyspepsia should be restricted to only one of the
four cardinal gastroduodenal symptoms (the dyspepsia complex ):
epigastric pain, epigastric burning, early satiety (inability to fn-
ish a normal-sized meal), and / or postprandial fullness; heartburn
is considered to be quite distinct and not part of dyspepsia ( 3 ),
even though most have a cluster of symptoms, not one or two
( 5 ). Early satiety and postprandial fullness can occur when the
proximal stomach fails to relax or the stomach is hypersensitive
to mechanical distension ( 6 ). Epigastric pain or burning might
arise from acid bathing the esophagus, stomach, or duodenum,
based on experimental data, but is also most ofen attributed
to gastroduodenal and not esophageal dysfunction ( 7 ). Practice
guidelines currently recommend diferent pathways if a patient
presents with predominant heartburn vs. those presenting with
one of the four cardinal dyspepsia symptoms; for example, empiric
Helicobacter pylori test and treat is only recommended in the
dyspepsia pathway ( 8 ).
If you read the Montreal classifcation of GERD ( 9 ) and the
Rome III classifcation of functional dyspepsia ( 3 ), you would
be forgiven for concluding that endoscopy-negative GERD and
functional dyspepsia are distinct disorders easy to pry apart in
research and practice. Among those presenting with upper GI
symptoms in primary and secondary care, it has been generally
assumed that the presence of frequent heartburn or acid regur-
gitation, especially if one of these is the predominant symptom,
indicates the patient almost certainly has GERD even if dyspepsia
coexists. Vakil and colleagues ( 10 ) in this issue of the American
Journal of Gastroenterology present data that cast doubt on the
assumption GERD and dyspepsia are distinguishable based on
heartburn. If we cannot use symptoms, how do we guide optimal
therapy in practice? In this Editorial, lets review what we do know,
what have we learned from the Vakil paper, and where to go from
here for both research and practice.
Emerging data support the view that heartburn and dyspepsia
are really part of one disease complex. For example, in epide-
miological studies, heartburn is recognized to occur commonly
in those reporting dyspepsia, in fact more so than expected by
chance despite heartburn and dyspepsia being such frequent
complaints ( 5,11 ). Limited pathophysiological data also support
a link, although why there is the co-occurrence of dyspepsia and
GERD symptoms is not well conceptualized. Gastric emptying is
delayed in a subset of patients with GERD (perhaps one-third),
but gastric emptying correlates very poorly with symptoms unless
Functional (Non-Ulcer) Dyspepsia and Gastroesophageal
Reux Disease: One Not Two Diseases ?
Nicholas J. Talley , MD, PhD
1
1
University of Newcastle , Callaghan , New South Wales , Australia . Correspondence: Nicholas J. Talley, MD, PhD , University of Newcastle , Callaghan ,
New South Wales 2308 , Australia . E-mail: nicholas.talley@newcastle.edu.au
Received 6 March 2013; accepted 7 March 2013
The American Journal of GASTROENTEROLOGY VOLUME 108
|
MAY 2013 www.amjgastro.com
S
T
O
M
A
C
H
776 Talley
Most of the randomized trials in functional dyspepsia have tried
to exclude GERD and have relied on asking about heartburn to rule
out refux ( 3,4 ). However, this approach may actually have ensured
that an atypical functional dyspepsia population was recruited; the
Vakil data support the concept that heartburn is an integral part
of the dyspepsia complex. An example of this paradox (excluding
heartburn may reduce the observed therapeutic response in func-
tional dyspepsia) has potentially been demonstrated. Itopride is a
prokinetic agent via dopamine D2 antagonism and antiacetylcho-
linesterase activity. In a carefully conducted Phase II trial, itopride
was superior to placebo in patients with functional dyspepsia, but
heartburn was not an exclusion ( 15 ) . In a subsequent Phase III
program comprising two similar randomized placebo control-
led trials, following advice from the Food and Drug Administra-
tion, refux symptoms were more rigorously excluded, itopride
was overall no better than placebo ( 16 ). In a subgroup analysis,
heartburn was the best predictor of response to itopride in the
Phase III program. Now we can speculate because heartburn is a
common, even characteristic symptom of functional dyspepsia,
excluding these cases will dampen response rates a revelation for
future trial design. A recent meta-analysis has suggested itopride
is superior to placebo in functional dyspepsia when all the data
are pooled ( 17 ).
In functional dyspepsia treatment trials, identifying and poten-
tially stratifying by the subgroups EPS and PDS is now widely
accepted, but Vakil and colleagues ( 10 ) suggest in primary care
that such subgrouping is likely of limited value because the condi-
tions overlap; in their study 66 % had both PDS and EPS. While
in epidemiological studies it has been easier to separate EPS and
PDS and overlap has been less striking ( 5,18 ), other studies in ter-
tiary care have similarly identifed the overlap of PDS and EPS as
dominating the clinical setting ( 19 ). Does this mean all comers
very severely impaired ( 12 ). While gastric accommodation is well
accepted to be impaired in a subset with functional dyspepsia
(perhaps as high as 40 % ) ( 3,4,6 ), Tack and colleagues ( 13 ) have
also shown that among those with a diagnosis of functional dys-
pepsia assessed by 24-h esophageal pH testing, impaired gastric
accommodation was actually numerically more common in those
dyspeptics with an abnormal esophageal pH study (although the
diference was not signifcant). In GERD, impaired accommoda-
tion may in part account for associated dyspeptic complaints such
as early satiety. Other data indicate that acid suppression may
beneft not only refux symptoms but also dyspepsia in patients
with GERD, supporting a direct relationship between heartburn
and dyspepsia ( 14 ).
In the Vakil study ( 10 ), primary care patients with one or more
upper GI symptoms at least twice a week for a month or longer
were recruited from Canada and Europe. Patients completed a
physician assessment, validated questionnaire, esophagogastrodu-
odenoscopy, and 48-h esophageal pH testing. GERD was defned
objectively by either esophagitis, pathological acid refux, or a
positive symptom associated profle, while functional dyspepsia
cases were broadly defned as upper GI symptoms with no objec-
tive evidence of GERD or peptic ulcer; excluding peptic ulcer, 189
(58 % ) had GERD whereas 138 (42 % ) had functional dyspepsia.
It was striking that typical symptoms of functional dyspepsia
occurred in over 80 % with GERD, but on the other hand heart-
burn and acid regurgitation were common in dyspepsia regard-
less of underlying Rome III symptom grouping into postprandial
distress syndrome (early satiety or postprandial fullness PDS) or
epigastric pain syndrome (epigastric pain or epigastric burning
EPS; Figure 1 ). In other words, symptoms classically attributed to
refux disease do not seem to help determine who does and does
not have functional dyspepsia.
53.8%
69.2%
66.7%
66.7%
59.3%
52.3%
81.5%
72.8%
0%
50%
100%
Heartburn Regurgitation Heartburn Regurgitation
64.5%
45.2%
73.8%
73.8%
PDS EPS PDS+EDS
Functional dyspepsia
P=0.7 P=0.3
P=0.7
P=0.2
Positive GERD testing
Figure 1 . Prevalence of dyspepsia subgroups (by Rome III) in those with documented functional dyspepsia (normal esophageal pH) vs. gastroesophageal
reux disease (abnormal esophageal pH study etc). Data from Vakil et al. ( 10 ). EPS, epigastric pain syndrome; GERD, gastroesophageal reux disease;
PDS, postprandial distress syndrome.
2013 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
S
T
O
M
A
C
H
777 Editorial
must be included in future functional dyspepsia trials? I think not.
Accumulating evidence suggests functional dyspepsia is a hetero-
geneous disorder, and while we need to better dissect this het-
erogeneity, subgrouping by symptoms is likely of assistance. For
example, a potential biomarker in functional dyspepsia (duodenal
esoinophilia) was only identifed in PDS, not EPS ( 20 ); if causal,
those with duodenal eosinophilia are likely to respond difer-
ently to those who develop functional dyspepsia via an alternative
mechanism. Montelukast in children has been shown to reduce
dyspepsia symptoms and possibly stabilize eosinophil degranu-
lation, but more robust trials are urgently needed ( 21 ). Targeted
drug therapy by symptom subgroup also appears promising.
Acotiamide is a selective anticholinesterase inhibitor that has
prokinetic properties. In a recent controlled trial that randomized
only patients with functional dyspepsia and PDS, 52 % on active
drug responded (vs. 35 % on placebo), for a number needed to
treat of six ( 22 ). While impressive overall, it is interesting to spec-
ulate why a subset of PDS respond and other with similar symp-
toms did not are there at least two diferent types of PDS?
Functional dyspepsia is a very common, distressful, and costly
condition. Te new data indicate that heartburn and regurgitation
occur much more ofen than has been expected in functional dys-
pepsia, even afer objective GERD has been exhaustively excluded
by appropriate testing; arbitrarily excluding heartburn in func-
tional dyspepsia studies appears misguided, and guidelines may
need to be rewritten. One could speculate functional dyspepsia
may ofen now be misdiagnosed as GERD in clinical practice,
although this needs to be confrmed. Many patients with func-
tional dyspepsia have both PDS and EPS, but despite the overlap
there is evidence a symptom-based approach may help identify
biomarkers and partially guide therapy. Targeting subgroups of
functional dyspepsia based on a combination of pathophysiologi-
cal markers and specifc symptoms (e.g., duodenal eosinophilia
and early satiety?) may lead to new therapeutic breakthroughs .
C ONFLICT OF INTEREST
Te author declares no confict of interest.
REFERENCES
1 . Camilleri M , Dubois D , Coulie B et al. Prevalence and socioeconomic
impact of upper gastrointestinal disorders in the United States: results
of the US Upper Gastrointestinal Study . Clin Gastroenterol Hepatol
2005 ; 3 : 543 52 .
2 . Stacher G , Lenglinger J , Bergmann H et al. Gastric emptying: a contribu-
tory factor in gastro-oesophageal refux activity? Gut 2000 ; 47 : 661 6 .
3 . Tack J , Talley NJ , Camilleri M et al. Functional gastroduodenal disorders .
Gastroenterology 2006 ; 130 : 1466 79 .
4 . Lacy BE , Talley NJ , Locke 3rd GR et al. Review article: current treatment
options and management of functional dyspepsia . Aliment Pharmacol Ter
2012 ; 36 : 3 15 .
5 . Jones MP, Talley NJ , Eslick GD et al. Community subgroups in dyspepsia
and their association with weight loss . Am J Gastroenterol 2008 ; 103 :
2051 60 .
6 . Haag S , Senf W, Tagay S et al. Is there any association between disturbed
gastrointestinal visceromotor and sensory function and impaired
quality of life in functional dyspepsia? Neurogastroenterol Motil
2010 ; 22 : 262 70 , e79 .
7 . van Boxel OS , ter Linde JJ , Siersema PD et al. Role of chemical stimulation
of the duodenum in dyspeptic symptom generation . Am J Gastroenterol
2010 ; 105 : 803 11 ; quiz 2, 12 .
8 . Talley NJ , Vakil NB , Moayyedi P. American gastroenterological association tech-
nical review on the evaluation of dyspepsia . Gastroenterology 2005 ; 129 : 1756 80 .
9 . Vakil N , van Zanten SV, Kahrilas P et al. Te Montreal defnition and
classifcation of gastroesophageal refux disease: a global evidence-based
consensus . Am J Gastroenterol 2006 ; 101 : 1900 20 ; quiz 43 .
10 . Vakil NH , K , Ohlsson L et al . Symptom overlap between postprandial
distress and epigastric pain syndromes of the Rome III dyspepsia
classifcation . Am J Gastroenterol 2013 ; 108 : 767 74 (this issue) .
11 . Talley N , Zinmeister A , Schleck C et al. Dyspepsia and dyspepsia subgroups:
a population-based study . Gastroenterology 1992 ; 102 (4 Part 1) : 1259 68 .
12 . Talley NJ , Locke 3rd GR , Lahr BD et al. Functional dyspepsia, delayed
gastric emptying, and impaired quality of life . Gut 2006 ; 55 : 933 9 .
13 . Tack J , Caenepeel P, Arts J et al. Prevalence of acid refux in functional
dyspepsia and its association with symptom profle . Gut 2005 ; 54 : 1370 6 .
14 . Monnikes H , Schwan T , van Rensburg C et al. Randomised clinical trial:
sustained response to PPI treatment of symptoms resembling functional
dyspepsia and irritable bowel syndrome in patients sufering from an
overlap with erosive gastro-oesophageal refux disease . Aliment Pharmacol
Ter 2012 ; 35 : 1279 89 .
15 . Holtmann G , Talley NJ , Liebregts T et al. A placebo-controlled trial of
itopride in functional dyspepsia . N Engl J Med 2006 ; 354 : 832 40 .
16 . Talley NJ , Tack J , Ptak T et al. Itopride in functional dyspepsia: results of
two phase III multicentre, randomised, double-blind, placebo-controlled
trials . Gut 2008 ; 57 : 740 6 .
17 . Huang X , Lv B , Zhang S et al. Itopride therapy for functional dyspepsia: a
meta-analysis . World J Gastroenterol 2012 ; 18 : 7371 7 .
18 . Choung RS , Locke GR , Schleck CD et al. Do distinct dyspepsia subgroups
exist in the community? A population-based study . Am J Gastroenterol
2007 ; 102 : 1983 9 .
19 . Tack J , Talley NJ . Functional dyspepsia-symptoms, defnitions and validity
of the Rome III criteria . Nat Rev Gastroenterol Hepatol 2013 ; 10 : 134 41 .
20 . Walker MM , Salehian SS , Murray CE et al. Implications of eosinophilia in
the normal duodenal biopsy an association with allergy and functional
dyspepsia . Aliment Pharmacol Ter 2010 ; 31 : 1229 36 .
21 . Friesen CA , Neilan NA , Schurman JV et al. Montelukast in the treatment of
duodenal eosinophilia in children with dyspepsia: efect on eosinophil density
and activation in relation to pharmacokinetics . BMC Gastroenterol 2009 ; 9 : 32 .
22 . Matsueda K , Hongo M , Tack J et al. A placebo-controlled trial of acotiamide
for meal-related symptoms of functional dyspepsia . Gut 2012 ; 61 : 821 8 .
You might also like
- Laryngopharyngeal and Gastroesophageal Reflux: A Comprehensive Guide to Diagnosis, Treatment, and Diet-Based ApproachesFrom EverandLaryngopharyngeal and Gastroesophageal Reflux: A Comprehensive Guide to Diagnosis, Treatment, and Diet-Based ApproachesCraig H. ZalvanNo ratings yet
- Gastroparesis: Pathophysiology, Clinical Presentation, Diagnosis and TreatmentFrom EverandGastroparesis: Pathophysiology, Clinical Presentation, Diagnosis and TreatmentRichard MccallumNo ratings yet
- GI - Pathophysiology, Evaluation, and Treatment of BloatingDocument11 pagesGI - Pathophysiology, Evaluation, and Treatment of BloatingTriLightNo ratings yet
- Functional Dyspepsia: Advances in Diagnosis and Therapy: ReviewDocument9 pagesFunctional Dyspepsia: Advances in Diagnosis and Therapy: Reviewjenny puentesNo ratings yet
- Diagnosis and Management of Functional HeartburnDocument9 pagesDiagnosis and Management of Functional Heartburnal ghiffari muhammad rayhanNo ratings yet
- Organic Versus Functional: DyspepsiaDocument16 pagesOrganic Versus Functional: DyspepsiahelenaNo ratings yet
- Ebp PaperDocument5 pagesEbp Paperapi-251752244No ratings yet
- Functional Dyspepsia: Review ArticleDocument11 pagesFunctional Dyspepsia: Review Articlejenny puentesNo ratings yet
- GerdDocument10 pagesGerdMulia NtiNo ratings yet
- Dyspepsia ReviewDocument13 pagesDyspepsia ReviewalbertrianthoNo ratings yet
- Functional Dyspepsia: Recent Advances in Pathophysiology: Update ArticleDocument5 pagesFunctional Dyspepsia: Recent Advances in Pathophysiology: Update ArticleDen BollongNo ratings yet
- Update On The Evaluation and Management of Functional DyspepsiaDocument7 pagesUpdate On The Evaluation and Management of Functional DyspepsiaDenuna EnjanaNo ratings yet
- CTC Gerd FinalDocument36 pagesCTC Gerd FinaljaipreyraNo ratings yet
- Therapeutic Strategies For Functional Dyspepsia and The Introduction of The Rome III Classification (2006)Document12 pagesTherapeutic Strategies For Functional Dyspepsia and The Introduction of The Rome III Classification (2006)Yuriko AndreNo ratings yet
- DispepsiaDocument11 pagesDispepsiaPendikNo ratings yet
- Nejm 2015 Functional DyspepsiaDocument12 pagesNejm 2015 Functional DyspepsiarisewfNo ratings yet
- Gastroesophageal Reflux Disease Control of Symptoms, Prevention of ComplicationsDocument9 pagesGastroesophageal Reflux Disease Control of Symptoms, Prevention of ComplicationsTiurma SibaraniNo ratings yet
- Gerd Info and LinksDocument14 pagesGerd Info and Linksapi-357798429No ratings yet
- Irritable Bowel Syndrome and Other Functional Gastrointestinal DisordersDocument3 pagesIrritable Bowel Syndrome and Other Functional Gastrointestinal DisordersdavpierNo ratings yet
- Richter 2017Document10 pagesRichter 2017Rachel RiosNo ratings yet
- JGastr10 GERDDocument8 pagesJGastr10 GERDEnderNo ratings yet
- Clinical Review: DyspepsiaDocument5 pagesClinical Review: Dyspepsiajenny puentesNo ratings yet
- Vignette UlfiDocument12 pagesVignette UlfiHiya Ulfi MuniraNo ratings yet
- Functional DyspepsiaDocument4 pagesFunctional DyspepsiaEasy Orient DewantariNo ratings yet
- Dyspepsia PDFDocument14 pagesDyspepsia PDFCdma Nastiti FatimahNo ratings yet
- Refractory Gastroesophageal Reflux Disease Diagnosis and ManagementDocument12 pagesRefractory Gastroesophageal Reflux Disease Diagnosis and Managementg-46005995No ratings yet
- Optimal Management of Severe Symptomatic Gastroesophageal Reflux DiseaseDocument17 pagesOptimal Management of Severe Symptomatic Gastroesophageal Reflux DiseaseGianella VegasNo ratings yet
- SSAT Maintenance of Certification: Literature Review On Gastroesophageal Reflux Disease and Hiatal HerniaDocument5 pagesSSAT Maintenance of Certification: Literature Review On Gastroesophageal Reflux Disease and Hiatal HerniaGosadorNo ratings yet
- Gastrointestinal Fabry DiseaseDocument14 pagesGastrointestinal Fabry DiseasedanradulescuNo ratings yet
- Dyspepsia: Scottish Intercollegiate Guidelines NetworkDocument30 pagesDyspepsia: Scottish Intercollegiate Guidelines NetworkAna Cristina IssaNo ratings yet
- Exploring The Spectrum of GERD: Myths and Realities: Special ArticleDocument9 pagesExploring The Spectrum of GERD: Myths and Realities: Special ArticleedopriyantomoNo ratings yet
- Gastritis and Carditis: University of British Columbia, Vancouver, British Columbia, CanadaDocument17 pagesGastritis and Carditis: University of British Columbia, Vancouver, British Columbia, CanadaJose SirittNo ratings yet
- Referensi 1 PDFDocument4 pagesReferensi 1 PDFYusmiatiNo ratings yet
- Pi Is 1542356517309278Document11 pagesPi Is 1542356517309278Putri SaharaNo ratings yet
- Functional Dyspepsia in ChildrenDocument13 pagesFunctional Dyspepsia in ChildrenTimothy Eduard A. SupitNo ratings yet
- Diagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosDocument6 pagesDiagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosWingga Chrisna AjiNo ratings yet
- ACG Guideline GERD March 2013 Plus CorrigendumDocument22 pagesACG Guideline GERD March 2013 Plus Corrigendumdwifit3No ratings yet
- Gastroparesis Updates On Pathogenesis and Management: ReviewDocument11 pagesGastroparesis Updates On Pathogenesis and Management: Reviewputri permata SariNo ratings yet
- Functional Diarrhea in Toddlers (Chronic Nonspeci Fi C Diarrhea)Document4 pagesFunctional Diarrhea in Toddlers (Chronic Nonspeci Fi C Diarrhea)Dini NanamiNo ratings yet
- William, Update On Approaches To Patients With Dyspepsia and Functional DyspepsiaDocument6 pagesWilliam, Update On Approaches To Patients With Dyspepsia and Functional DyspepsiaRevalitha PutriNo ratings yet
- Dispepsia Functionala UtdDocument15 pagesDispepsia Functionala UtdIulia NiculaeNo ratings yet
- Dispepsia 1Document16 pagesDispepsia 1nainggolan Debora15No ratings yet
- Desordenes Esofagicos Roma IVDocument12 pagesDesordenes Esofagicos Roma IVJose Lopez FuentesNo ratings yet
- Algoritma GerdDocument14 pagesAlgoritma GerdRivaldi ArdiansyahNo ratings yet
- Gastrointestinal Disorders in DiabetesDocument20 pagesGastrointestinal Disorders in Diabetesdoctor327810No ratings yet
- Impaired Gastric Accommodation (IGA) : Patient OverviewDocument10 pagesImpaired Gastric Accommodation (IGA) : Patient OverviewDaniel RosehlilNo ratings yet
- Review: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisDocument8 pagesReview: Epidemiology, Mechanisms, and Management of Diabetic GastroparesisIrma KurniawatiNo ratings yet
- Dyspepsia: Scottish Intercollegiate Guidelines NetworkDocument30 pagesDyspepsia: Scottish Intercollegiate Guidelines NetworkTruly Dian AnggrainiNo ratings yet
- Gastroesophageal Reflux Disease: From Pathophysiology To TreatmentDocument5 pagesGastroesophageal Reflux Disease: From Pathophysiology To TreatmentQoniek Nuzulul FalakhiNo ratings yet
- s13023 015 0302 1 PDFDocument14 pagess13023 015 0302 1 PDFNur Alfia KusumaningsihNo ratings yet
- ACG Guideline GERD March 2013Document21 pagesACG Guideline GERD March 2013Arri KurniawanNo ratings yet
- DyspepsiaDocument7 pagesDyspepsiaFa'iz HeryotoNo ratings yet
- A European Approach To Irritable Bowel Syndrome Management: Gut Dysfunction in IbsDocument5 pagesA European Approach To Irritable Bowel Syndrome Management: Gut Dysfunction in Ibsa3llamNo ratings yet
- Associations of Circulating Gut Hormone and Adipocytokine Levels With The Spectrum of Gastroesophageal Reflux DiseaseDocument12 pagesAssociations of Circulating Gut Hormone and Adipocytokine Levels With The Spectrum of Gastroesophageal Reflux DiseasekasabeNo ratings yet
- (2021) GerdDocument23 pages(2021) Gerdadri20121989No ratings yet
- New Articles in This Journal Are Licensed Under A Creative Commons Attribution 4.0 United States LicenseDocument16 pagesNew Articles in This Journal Are Licensed Under A Creative Commons Attribution 4.0 United States Licenseandi hajrahNo ratings yet
- Dagli2017 (Elevated Head)Document5 pagesDagli2017 (Elevated Head)askhaeraniNo ratings yet
- Achalasia CardiaDocument3 pagesAchalasia CardiaAnonymous KaJImISFNo ratings yet
- Journal of Gastroenterology and HepatologyDocument9 pagesJournal of Gastroenterology and HepatologyKyla OcampoNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Form Pencatatan Manual Versi 1 Pelaksanaan Skrining Di Meja 2Document16 pagesForm Pencatatan Manual Versi 1 Pelaksanaan Skrining Di Meja 2Reynalth Andrew SinagaNo ratings yet
- Cheat AOEDocument1 pageCheat AOEReynalth Andrew SinagaNo ratings yet
- Form Pencatatan Manual Versi 1 Pelaksanaan Vaksinasi Di Meja 4Document11 pagesForm Pencatatan Manual Versi 1 Pelaksanaan Vaksinasi Di Meja 4Reynalth Andrew SinagaNo ratings yet
- Squamous Cell Carcinoma: Delivering The Best in CareDocument8 pagesSquamous Cell Carcinoma: Delivering The Best in CareReynalth Andrew SinagaNo ratings yet
- Files 110711 Squ AmousDocument4 pagesFiles 110711 Squ AmousReynalth Andrew SinagaNo ratings yet
- CDC - Toxoplasmosis - BiologyDocument2 pagesCDC - Toxoplasmosis - BiologyReynalth Andrew SinagaNo ratings yet
- Difficulties Observed in A Reference Center in The Diagnosis and Management of Pregnant Women With ToxoplasmosisDocument5 pagesDifficulties Observed in A Reference Center in The Diagnosis and Management of Pregnant Women With ToxoplasmosisReynalth Andrew SinagaNo ratings yet
- Understanding Mechanisms and The Role of Differentiation in Pathogenesis of Toxoplasma Gondii - A ReviewDocument7 pagesUnderstanding Mechanisms and The Role of Differentiation in Pathogenesis of Toxoplasma Gondii - A ReviewReynalth Andrew SinagaNo ratings yet
- Previews: Macrophages As A Battleground For Toxoplasma PathogenesisDocument3 pagesPreviews: Macrophages As A Battleground For Toxoplasma PathogenesisReynalth Andrew SinagaNo ratings yet
- Review: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseDocument11 pagesReview: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseReynalth Andrew Sinaga100% (1)
- G G - Star Star StarDocument4 pagesG G - Star Star StarReynalth Andrew SinagaNo ratings yet
- Hypertensi Crisis: Dr. Leonardo Dairy, SPPD - KgehDocument11 pagesHypertensi Crisis: Dr. Leonardo Dairy, SPPD - KgehReynalth Andrew SinagaNo ratings yet
- Myasthenia Gravis, Autoantibodies, Antigens: and Hl-ADocument3 pagesMyasthenia Gravis, Autoantibodies, Antigens: and Hl-AReynalth Andrew SinagaNo ratings yet
- BD9897FS Ic DetailsDocument5 pagesBD9897FS Ic DetailsSundaram LakshmananNo ratings yet
- English 7 Compare Contrast The People Could Fly Harriet TubmanDocument3 pagesEnglish 7 Compare Contrast The People Could Fly Harriet Tubmanapi-508729334No ratings yet
- Zone Raiders (Sci Fi 28mm)Document49 pagesZone Raiders (Sci Fi 28mm)Burrps Burrpington100% (3)
- Functions of Ecgc and Exim BankDocument12 pagesFunctions of Ecgc and Exim BankbhumishahNo ratings yet
- Taxation and LibertyDocument28 pagesTaxation and LibertyRitu Raj RamanNo ratings yet
- ICT LegalEthical Issue PowerPoint PresentationDocument4 pagesICT LegalEthical Issue PowerPoint PresentationReydan MaraveNo ratings yet
- SKI Report2008 - 50 2Document46 pagesSKI Report2008 - 50 2nada safitriNo ratings yet
- Science Fiction FilmsDocument5 pagesScience Fiction Filmsapi-483055750No ratings yet
- Presente Progresive TenseDocument21 pagesPresente Progresive TenseAriana ChanganaquiNo ratings yet
- Lesson Plan (Speaking Skills)Document7 pagesLesson Plan (Speaking Skills)Nurul Fathiah Zulkarnain100% (1)
- Modbus Manual TD80 PDFDocument34 pagesModbus Manual TD80 PDFAmar ChavanNo ratings yet
- (CTRL) The Finders' Keeper: An Interview With Marion PettieDocument10 pages(CTRL) The Finders' Keeper: An Interview With Marion PettieSolomanTrismosin100% (2)
- Disciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineDocument12 pagesDisciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineErez CohenNo ratings yet
- Lesson Plan 2 Revised - Morgan LegrandDocument19 pagesLesson Plan 2 Revised - Morgan Legrandapi-540805523No ratings yet
- Gianna Pomata (Editor), Nancy G. Siraisi (Editor) - Historia - Empiricism and Erudition in Early Modern Europe (Transformations - Studies in The History of Science and Technology) (2006)Document493 pagesGianna Pomata (Editor), Nancy G. Siraisi (Editor) - Historia - Empiricism and Erudition in Early Modern Europe (Transformations - Studies in The History of Science and Technology) (2006)Marcelo Rizzo100% (1)
- ( (LEAD - FIRSTNAME) ) 'S Spouse Visa PackageDocument14 pages( (LEAD - FIRSTNAME) ) 'S Spouse Visa PackageDamon Culbert0% (1)
- Gallery IsKCON Desire Tree PDF MudrasDocument2 pagesGallery IsKCON Desire Tree PDF MudrassanatanNo ratings yet
- Course Hand Out Comm. Skill BSC AgDocument2 pagesCourse Hand Out Comm. Skill BSC Agfarid khanNo ratings yet
- EP105Use of English ArantxaReynosoDocument6 pagesEP105Use of English ArantxaReynosoArantxaSteffiNo ratings yet
- Occ ST 1Document3 pagesOcc ST 1Rona Marie BulaongNo ratings yet
- LDS Conference Report 1930 Semi AnnualDocument148 pagesLDS Conference Report 1930 Semi AnnualrjjburrowsNo ratings yet
- Mohit Maru 4th Semester Internship ReportDocument11 pagesMohit Maru 4th Semester Internship ReportAdhish ChakrabortyNo ratings yet
- The Palatability, and Potential Toxicity of Australian Weeds To GoatsDocument163 pagesThe Palatability, and Potential Toxicity of Australian Weeds To Goatsalshokairsaad513No ratings yet
- Microsoft Official Course: Installing and Configuring Windows Server 2012Document18 pagesMicrosoft Official Course: Installing and Configuring Windows Server 2012jttodorovNo ratings yet
- Map Index: RD - To CE MP AR KDocument1 pageMap Index: RD - To CE MP AR KswaggerboxNo ratings yet
- Fruitful Outreaches Intercessory Prayer GuidelinesDocument5 pagesFruitful Outreaches Intercessory Prayer GuidelinesPaul Moiloa100% (1)
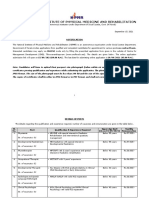
- NIPMR Notification v3Document3 pagesNIPMR Notification v3maneeshaNo ratings yet
- SEO Roadmap - Bayut & DubizzleDocument17 pagesSEO Roadmap - Bayut & Dubizzlebasel kotbNo ratings yet
- Medical Surgical Nursing Nclex Questions 5Document18 pagesMedical Surgical Nursing Nclex Questions 5dee_day_8No ratings yet
- The Newton-Leibniz Book Research - Gate - 06!12!2023Document17 pagesThe Newton-Leibniz Book Research - Gate - 06!12!2023Constantine KirichesNo ratings yet