Professional Documents
Culture Documents
Ebola Virus Patient Advisory 181014
Uploaded by
eblackhole10 ratings0% found this document useful (0 votes)
42 views7 pagesAn advisory from Raffles Medical Group on the Ebola virus.
Please read the advisory on the latest development and understand the precautionary steps to take to protect yourselves and your family members.
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAn advisory from Raffles Medical Group on the Ebola virus.
Please read the advisory on the latest development and understand the precautionary steps to take to protect yourselves and your family members.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
42 views7 pagesEbola Virus Patient Advisory 181014
Uploaded by
eblackhole1An advisory from Raffles Medical Group on the Ebola virus.
Please read the advisory on the latest development and understand the precautionary steps to take to protect yourselves and your family members.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
18 October 2014
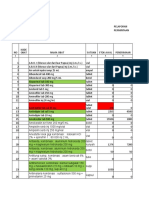
Ebola patients treated outside West Africa* (updated 15 Oct 2014)
*In all but 3 cases, the patient was infected with Ebola while in West Africa. Infection outside Africa has been restricted to health workers in Madrid and in
Dallas. DR Congo has also reported a separate outbreak of an unrelated strain of Ebola.
Ebola virus was first identified in Sudan and Zaire in 1976. It belongs to the family of Filoviridae.
It causes Ebola Virus Disease (EVD), formerly known as Ebola Hemorrhagic Fever. EVD is a rare
disease which causes severe, often fatal illness in humans. There are 5 different species of Ebola
virus identified and isolated from different regions in Africa. The different species has different
infectivity and mortality in humans. The Zaire species is the most virulent and can result in up to 90%
mortality in humans who are infected with it.
Outbreaks occur primarily in remote villages in Central and West Africa. The current outbreak of EVD
in West Africa started in March 2014.
The 2014 Ebola epidemic is the largest in history, affecting
multiple countries. As of 15 Oct 2014, WHO released new
figures stating that more than 8,997 confirmed, probable and
suspected cases have been reported in seven affected
countries: Liberia, Nigeria Guinea, Sierra Leone, Senegal,
Spain, and the United States of America. 4493 people have
died. (Case fatality rate of about 50%). The situation in
Guinea, Liberia, and Sierra Leone is deteriorating, with
widespread and persistent transmission of EV. These severely
affected countries have very weak health systems, lacking
human and infrastructural resources. WHO estimates that
Liberia's number of Ebola cases is likely even greater than the
number that has been reported as there is difficulty
gathering data in Liberia.
In Nigeria, there have been 20 cases and 8 deaths. In Senegal, there has been one travel-associated
case. Nigeria and Senegal have not reported any new cases since September 5, 2014, and August 29,
2014, respectively. In Spain there has been one case. These cases are thus considered to be
contained, with no further spread in these countries (localized transmission).
In the United States (Dallas, Texas), 2 cases and 1 death have
been reported. The first index case in US involved an
imported case in a man who had traveled to Dallas, Texas
from West Africa on 30 September 2014. The patient did not
have symptoms when leaving West Africa, but developed
symptoms approximately four days after arriving in the
United States. The person sought medical care at Texas
Presbyterian Hospital of Dallas after developing symptoms
consistent with Ebola. He died of Ebola on October 8 and was
cremated. On October 10, a healthcare worker at Texas
Presbyterian Hospital who provided care for the index patient fell ill and was tested positive for
Ebola, and is currently being treated at Texas Health Presbyterian Hospital Dallas.
On October 14, a second healthcare worker at Texas Presbyterian Hospital who also provided care
for the index patient reported to the hospital with a low-grade fever and was isolated. The
healthcare worker tested positive for Ebola; she however, travelled by a Frontier airlines flight on 13
October evening, the day before she reported symptoms. In view of the proximity in time between
the evening flight and first report of illness the following morning, CDC is now reaching out to 132
passengers who flew on Frontier Airlines flight 1143 Cleveland to Dallas/Fort Worth Oct. 13.
CDC is also working with other U.S. government agencies, the World Health Organization (WHO),
and other domestic and international partners and has activated its Emergency Operations Center to
help coordinate technical assistance and control activities with partners. CDC has also deployed
teams of public health experts to West Africa and will continue to send experts to the affected
countries.
(Adapted from http://www.cdc.gov/vhf/ebola/resources/virus-ecology.html)
In an Ebola virus outbreak, the virus is transmitted through direct contact of broken skin or mucous
membranes with blood, stool, vomitus, urine, saliva and tissues of symptomatic persons or animals,
or indirect contact with environments contaminated with such fluids. Humans may also be infected
through exposure to secretions or excretions of bats. Infection can also be acquired through
ingesting the meat of infected primates (apes, gorilla, and chimpanzees) and animals.
Those at highest risk of infection are:
health workers;
family members or others in close contact with infected people;
mourners who have direct contact with the bodies of the deceased as part of burial ceremonies.
Other risk factors include:
hunters in the rain forest who come into contact with dead animals found lying in the forest.
The incubation period of EVD varies from 2 to 21 days, usually 5 to 10 days. Patients are not
contagious during the incubation period. Infected individuals become contagious only when they
manifest symptoms.
Symptoms usually begin as a flu-like
syndrome (sudden onset of fever, chills,
general malaise, muscle pain, joint pain,
headache, non-productive cough and sore
throat).
Other symptoms that may follow include
nausea, vomiting, diarrhea, abdominal pain,
non-itchy rash.
As the illness progresses, kidney and liver
function become impaired and in some cases,
patients start developing internal or external
bleeding.
Ebola virus infections can only be confirmed
through laboratory testing, which detect:
antibodies,
viral antigen (ELISA assays),
Ebola RNA by reverse-transcription polymerase chain reaction (PCR),
Viral cultures and isolation may also be performed with infected material / specimens
There is currently no specific treatment for Ebola virus infection. Management is supportive, which
may include oxygen, blood transfusion and fluids.
(1) Can I still travel to Africa or any of the affected countries?
You are encouraged to refer to the MOH web page on Ebola for the latest Health Advisory, before
travelling to West or Central Africa. You should consider postponing travel to countries with
reported Ebola Virus Disease activity, if it is non-essential.
(2) How do I prevent myself from being infected?
There is currently no vaccine against Ebola virus infection available. The risk of infection can be
significantly reduced by barrier techniques; through the use of wearing appropriate protective
equipment, such as masks, gloves, and gowns, eye shields, and regular hand washing.
(3) Whats the situation in Singapore?
There has not been any reported case of Ebola in Singapore. MOH has been closely watching the
Ebola situation, including developments in Spain and the United States. These show that an
imported case and the potential for community exposure from imported cases cannot be ruled out.
(4) What is Singapore doing to control the spread of Ebola?
Singapore had stepped up additional screening measures at arrival halls in Singapore Changi Airport
with effect from 15 Oct, 12 noon. Nationals and travellers from countries with reported Ebola Virus
Disease activity (currently Guinea, Liberia, Sierra Leone, Nigeria, Senegal and Democratic Republic of
Congo) will be directed to a screening station, where they will be screened for temperature and
exposure to Ebola through a Health Declaration Card, which will include their contact details in
Singapore.
How not to spread and/or catch Ebola
Strict isolation of the infected patients,
Avoid direct contact with sick patients as the virus is spread through contaminated body
fluids
Proper personal protective equipment for the people in contact with the patients,
Proper handling and disposal of remains. Clothing and clinical waste should be incinerated
and any medical equipment that needs to be kept should be decontaminated
Maintain good personal hygiene
People who recover from Ebola should abstain from sex or use condoms for three months
Travelers who are cleared will then be directed to the duty desk at the arrival hall, where they will
clear immigration control. Those who are found to have a fever will be transported in an appropriate
ambulance transport to Tan Tock Seng Hospital for further medical assessment. Travellers who are
well but who are identified as having possible exposure to Ebola virus infection will be quarantined
or put under surveillance depending on the risk assessment. Measures are in place to carry out
contact tracing and quarantine of all close contacts, in the event of an imported case.
Aside from Singapore Changi Airport, a Health Declaration Card will also be implemented at land and
sea checkpoints, as well as at Seletar Airport.
(4) What should I look out for if I need to travel to Africa or any of the affected countries?
If your travel to these countries is necessary, it is advisable that you closely monitor the advice
provided by local health authorities and the WHO.
You must maintain strict hygiene standards such as hand hygiene and avoid any direct contact with
patients with Ebola or unknown illnesses and any objects that may be contaminated with bodily
fluids. Hospital visits are strongly discouraged.
You must also avoid contact with wild animals such as chimpanzee or gorillas (especially if the
animal has been sick) and avoid eating or handling raw or undercooked animal products, such as
blood and meat. Exploration of caves that may be inhabited by bats should be avoided.
If you should fall ill with symptoms described above and you have possible exposure history, consult
the doctor immediately.
(5) What should I do if I fall ill after returning from Africa or any of the affected countries?
Returning travellers from countries with reported Ebola Virus Disease activity or travellers who
suspect that they have been exposed to Ebola virus should seek immediate medical attention, if they
develop any disease symptoms within 3 weeks of their return. They should inform their doctor of
their recent travel or contact history.
EVD should be considered as a possible diagnosis in individuals who presented with the following
symptoms and travel history:
A person with a fever (>38 C) or history of sudden onset of high fever AND has travelled in
particular regions in West Africa (currently Guinea, Liberia, and Sierra Leone) within 21 days, OR
A person with fever (>38 C) or history of sudden onset of high fever AND has cared for or come
into contact with body fluids (blood, urine, faeces, tissues, laboratory cultures) from an
individual known or strongly suspected to have EVD.
Clinic
585 North Bridge Road, Level 1
Raffles Hospital, Singapore 188770
Contact Tel: 6311 2233
Fax: 6311 2123
Operating Hours Daily 8.00am - 10.00pm
Clinic
Raffles Medical @ T3
Singapore Changi Airport
65 Airport Boulevard, B2-01
Singapore 819663
Contact Tel: 6241 8818
Fax: 6241 3498
Operating Hours Daily 24 Hours
You might also like
- Screenshot 2022-11-06 at 5.51.25 PMDocument1 pageScreenshot 2022-11-06 at 5.51.25 PMHadiya KhaleelNo ratings yet
- Histrionic Personality DisorderDocument2 pagesHistrionic Personality DisorderRodeneNo ratings yet
- RBC DisordersDocument70 pagesRBC DisordersNdor Baribolo100% (1)
- EbolaDocument3 pagesEbolaankeritenursing 647No ratings yet
- Transmicion: FiloviridaeDocument15 pagesTransmicion: FiloviridaeDaniela Ortiz100% (1)
- HematuriaDocument32 pagesHematuriaSurya Nirmala DewiNo ratings yet
- Pemeriksaan Thorax: Coass Interna RSI Sultan Agung SemarangDocument59 pagesPemeriksaan Thorax: Coass Interna RSI Sultan Agung SemarangImada KhoironiNo ratings yet
- PRO Post Natal AssessmentDocument9 pagesPRO Post Natal AssessmentMali KanuNo ratings yet
- Health Assessment LectureDocument115 pagesHealth Assessment Lectureteuuuu100% (1)
- Combinazioni SSC Unico PDFDocument73 pagesCombinazioni SSC Unico PDFGiovanni PasqualiniNo ratings yet
- Annotated BibliographyDocument3 pagesAnnotated BibliographypeterhjeonNo ratings yet
- Ebola Virus DiseaseDocument4 pagesEbola Virus Diseasev_vijayakanth7656No ratings yet
- General Ebola InformationDocument8 pagesGeneral Ebola InformationChellaMarieNo ratings yet
- Submitted To - Shalini Mam Submitted by - Yash Nagar Class - XII B Roll No.Document10 pagesSubmitted To - Shalini Mam Submitted by - Yash Nagar Class - XII B Roll No.Yash Nagar100% (1)
- Ebola - The Killer VirusDocument3 pagesEbola - The Killer VirusLalit SinghNo ratings yet
- Ebola Virus Disease: Key FactsDocument5 pagesEbola Virus Disease: Key Facts黄銮添No ratings yet
- Ebola Virus Disease Grassroots Talking PointsDocument4 pagesEbola Virus Disease Grassroots Talking PointsMargaretWilsonNo ratings yet
- Ebola Virus DiseaseDocument3 pagesEbola Virus DiseasePoonam RanaNo ratings yet
- Key FactsDocument4 pagesKey FactsAnonymous JOOQkGbwoRNo ratings yet
- Bahasa Inggris 1Document41 pagesBahasa Inggris 1RizqyAuliaNestaNo ratings yet
- Ebola Virus Disease (EVD) : What Are The Symptoms?Document2 pagesEbola Virus Disease (EVD) : What Are The Symptoms?Travel Health FremantleNo ratings yet
- EbolaDocument20 pagesEbolaFabian PitkinNo ratings yet
- Ebola Virus Disease: Key FactsDocument5 pagesEbola Virus Disease: Key FactsMichaelKimDugeniaNo ratings yet
- Ebola Virus 2Document17 pagesEbola Virus 2Rashid madniNo ratings yet
- Choo Choy Tian 00000027562 CH219 Practical ReportDocument6 pagesChoo Choy Tian 00000027562 CH219 Practical ReportWei Hao ChanNo ratings yet
- History: Ebolavirus. After This Discovery, Scientists Concluded That The Virus Came From Two DifferentDocument4 pagesHistory: Ebolavirus. After This Discovery, Scientists Concluded That The Virus Came From Two DifferentAsniah Hadjiadatu AbdullahNo ratings yet
- Ebola Virus Disease: Key FactsDocument2 pagesEbola Virus Disease: Key FactsNi-el 'ndra' SantosoNo ratings yet
- Ebola Virus Disease: Key FactsDocument3 pagesEbola Virus Disease: Key FactsAnthony Miguel RafananNo ratings yet
- Ideas and Opinions: Ebola Hemorrhagic Fever in 2014: The Tale of An Evolving EpidemicDocument4 pagesIdeas and Opinions: Ebola Hemorrhagic Fever in 2014: The Tale of An Evolving EpidemicYulias YoweiNo ratings yet
- Ebola Update - TravelDocument4 pagesEbola Update - TravelrodicaciocheaNo ratings yet
- Dissertation Sur LebolaDocument5 pagesDissertation Sur LebolaCustomWrittenPaperCanada100% (1)
- WHO - Ebola Virus DiseaseDocument6 pagesWHO - Ebola Virus Diseasedhoo_babyNo ratings yet
- Ebola EbvDocument5 pagesEbola EbvAmal Bahrum PenasNo ratings yet
- Allen County HDDocument5 pagesAllen County HDtriddle1969No ratings yet
- Ebola VirusDocument22 pagesEbola VirussomyaNo ratings yet
- About Ebola Hemorrhagic FeverDocument5 pagesAbout Ebola Hemorrhagic FeverMiryam ChNo ratings yet
- Ebola FactsheetDocument3 pagesEbola FactsheetJohn Rey AbadNo ratings yet
- Ebola Hemorrhagic Fever: TransmissionDocument3 pagesEbola Hemorrhagic Fever: Transmissionromeoenny4154No ratings yet
- Ebola Virus Disease: Key FactsDocument3 pagesEbola Virus Disease: Key FactsruguNo ratings yet
- Ebola Research PaperDocument57 pagesEbola Research PaperTony Omorotionmwan Airhiavbere100% (1)
- Ebola Overview TemplateDocument35 pagesEbola Overview TemplateNoneyaNo ratings yet
- Prevention and Control of Ebola Virus DiseaseDocument3 pagesPrevention and Control of Ebola Virus DiseasenzeprimeNo ratings yet
- EBOLADocument4 pagesEBOLAwawa3385No ratings yet
- Ebola PDFDocument2 pagesEbola PDFsunchit1986No ratings yet
- Bio Project Class 12Document15 pagesBio Project Class 12joyitaNo ratings yet
- Ebola Epidemic: Unit 3Document2 pagesEbola Epidemic: Unit 3Nia NormayunitaNo ratings yet
- Ebola Virus Disease (Ebola) : AdviceDocument1 pageEbola Virus Disease (Ebola) : AdvicePrabowoNo ratings yet
- Biology Ebola Virus Project ReportDocument19 pagesBiology Ebola Virus Project ReportChaitaneyMorNo ratings yet
- Ebola Virus Disease (EVD)Document10 pagesEbola Virus Disease (EVD)Alan AzadNo ratings yet
- Ebola: What Clinicians Need To KnowDocument3 pagesEbola: What Clinicians Need To KnowIman100% (1)
- Ebola Virus Disease (WHO) : Key FactsDocument5 pagesEbola Virus Disease (WHO) : Key FactsridhosetyawanNo ratings yet
- Ebola For ArticleDocument7 pagesEbola For ArticlehappyNo ratings yet
- CDC Research Paper FinalDocument7 pagesCDC Research Paper Finalapi-273328906No ratings yet
- WHO - Ebola Haemorrhagic Fever.Document3 pagesWHO - Ebola Haemorrhagic Fever.CSilva16No ratings yet
- Ebola Virus DiseaseDocument13 pagesEbola Virus DiseaseMade Sudarsana0% (1)
- Ebola (Ebola Virus Disease) : TransmissionDocument2 pagesEbola (Ebola Virus Disease) : TransmissionCaleb VoosNo ratings yet
- Ebola Virus DiseaseDocument17 pagesEbola Virus DiseaseViorelNo ratings yet
- PHE Information On Ebola in Pregnancy V2 0Document4 pagesPHE Information On Ebola in Pregnancy V2 0Philip ScofieldNo ratings yet
- CDC Ebola Fact SheetDocument13 pagesCDC Ebola Fact Sheetيوسف سيمنزNo ratings yet
- Infectious DiseasesDocument6 pagesInfectious DiseaseschrisyenNo ratings yet
- Ebola RPRTDocument19 pagesEbola RPRTDel FinNo ratings yet
- Ebola UpdateDocument49 pagesEbola Updatetummalapalli venkateswara raoNo ratings yet
- Ebola Free World-Stopping The Killer Virus: How Nigeria Did It And How Other Countries Can TooFrom EverandEbola Free World-Stopping The Killer Virus: How Nigeria Did It And How Other Countries Can TooNo ratings yet
- Dissertation Virus EbolaDocument8 pagesDissertation Virus EbolaCustomWritingPapersKnoxville100% (1)
- WHO - Ebola Virus Disease (Evd) Key FactsDocument6 pagesWHO - Ebola Virus Disease (Evd) Key FactsBeatrice IoanaNo ratings yet
- Frequently Asked Questions On Ebola Virus DiseaseDocument8 pagesFrequently Asked Questions On Ebola Virus DiseaseNoneyaNo ratings yet
- Introduction and Statement of The ProblemDocument4 pagesIntroduction and Statement of The ProblemShitty headNo ratings yet
- Jama Shadman 2023 RV 230004 1679344287.92157Document15 pagesJama Shadman 2023 RV 230004 1679344287.92157Alejandro PedrazaNo ratings yet
- Communicable Disease Table (GROUP2 BSN IIIB)Document10 pagesCommunicable Disease Table (GROUP2 BSN IIIB)Hershey Cordero BrionesNo ratings yet
- Constipation NCPDocument2 pagesConstipation NCPjudaperlNo ratings yet
- Blood TransfusionDocument2 pagesBlood TransfusionKomal TomarNo ratings yet
- Condom Demo Class February 2015Document54 pagesCondom Demo Class February 2015Kago NgomaNo ratings yet
- PIIS0015028212007017Document9 pagesPIIS0015028212007017marinaNo ratings yet
- Nej M 200202073460618Document8 pagesNej M 200202073460618Adina OlteanuNo ratings yet
- ACL Postop Instructions - HagenDocument7 pagesACL Postop Instructions - HagenkapsicumadNo ratings yet
- Immunity (Lecture Notes)Document5 pagesImmunity (Lecture Notes)Anisha NishanthNo ratings yet
- Tanyut Huidrom - Assignment 4 - HUman PhysiologyDocument1 pageTanyut Huidrom - Assignment 4 - HUman PhysiologyTanyut HuidromNo ratings yet
- Empty Sella SyndromeDocument2 pagesEmpty Sella Syndromewawan_291289No ratings yet
- Evaluation of Factors That Affects The Usage of Insecticide Treated Mosquito Nets in Pregnant Women at IshakaDocument15 pagesEvaluation of Factors That Affects The Usage of Insecticide Treated Mosquito Nets in Pregnant Women at IshakaKIU PUBLICATION AND EXTENSIONNo ratings yet
- Lplpo Agustus 2017Document66 pagesLplpo Agustus 2017Selly Wijaya BermawiNo ratings yet
- 2 CSEP-CPT Aerobictheory v2Document20 pages2 CSEP-CPT Aerobictheory v2Nnaemeka NwobodoNo ratings yet
- Infopia Clover A1cDocument31 pagesInfopia Clover A1cAde NasutionNo ratings yet
- Epulis KongenitalDocument3 pagesEpulis KongenitalFriadi NataNo ratings yet
- 2018-Academic Emergency MedicineDocument278 pages2018-Academic Emergency MedicinederrickNo ratings yet
- PediatricsDocument33 pagesPediatricsnageshwarioshNo ratings yet
- Sirka Health OfficeDocument30 pagesSirka Health OfficeWogen GenaNo ratings yet
- Anxiety Disorder Teaching PlanDocument21 pagesAnxiety Disorder Teaching PlanEcaroh Hew Smailliw0% (1)
- Isotonic, Hypotonic, and Hypertonic IV Fluid Solution: Isotonic Solutions: Contains Approximately The SameDocument1 pageIsotonic, Hypotonic, and Hypertonic IV Fluid Solution: Isotonic Solutions: Contains Approximately The SamemimNo ratings yet
- Personal Data:: Curiculum VitaeDocument7 pagesPersonal Data:: Curiculum Vitaebudi darmantaNo ratings yet