Professional Documents
Culture Documents
Document
Uploaded by
Hadi FirmansyahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Document
Uploaded by
Hadi FirmansyahCopyright:
Available Formats
JDV_478.
fm Page 436 Tuesday, September 10, 2002 5:13 PM
JEADV (2002) 16, 436 437
EDITOR IAL
Collodion baby: whats new
Blackwell Science, Ltd
A Taeb,* C Labrze
Unit de Dermatologie Pdiatrique, Hpital Pellegrin Enfants, 33076 Bordeaux cedex, France. *Corresponding author, tel. +33 556 79 56 22;
fax +33 556 79 59 87; E-mail: alain.taieb@chou-bordeaux.fr
Van Gysel D, Lijnen RLP, Moekti S, de Laat PCJ,
Oranje AP. Collodion baby: a follow-up study of
17 cases. JEADV 2002; 16: 472475
The paper by Van Gysel et al. is the largest study reported at
a single institution (Queen Sophia Childrens Hospital,
Rotterdam, the Netherlands) for the condition named after
Hallopeau Bb collodion or collodion baby; this refers to a
collodion-like membrane that covers the baby at birth, which
is associated with major risks during the neonatal period,
including hypothermia, dehydration, infection and mechanical
compression leading to distal limb ischaemia. As confirmed in
the Rotterdam study, the overall prognosis has dramatically
improved over time with the development of neonatal intensive
care.1 This neonatal membrane is the most severe expression of a
congenital disorder of cornification of variable aetiology, including in the majority the most severe classic ichthyoses, which
are inherited as recessive traits, thus excluding the bullous
forms, at variance with the Rotterdam series (Table 1). The
diagnostic approach is summarized in Table 2. The transglutaminase assay allows us to refine the classification among the
non-associated congenital ichthyoses.2 The outcome is difficult
to predict, but the initial severity of phenotype and time to
membrane shedding may be indicators of the future severity of
the underlying ichthyosis.1 However, the resulting condition may
Table 1 Etiology of collodion baby syndrome
1. Common severe phenotypes (not associated with noncutaneous features)
AR congenital erythrodermic ichthyosis (50% of cases)
AR lamellar ichthyosis (10%)
2. Common milder phenotypes
Ichthyosis vulgaris type (mild form) (10%)
Recovery without sequaelae (10%)
3. Associated congenital ichthyoses
Trichothiodystrophy
Sjgren Larsson syndrome*
Netherton syndrome*
Gaucher disease type 2*
4. Miscellaneous conditions (collodion baby phenotype mentioned at
least once in the literature)*
Congenital hypothyroidism, Conradi syndrome, Dorfman Chanarin
syndrome, Ketoadipiaciduria, koraxitrachitic syndrome, ichthyosis
variegata, palmoplantar keratoderma with anogenital leukokeratosis
*True collodion membrane poorly documented.
436
Table 2 Major diagnostic procedures in collodion baby syndrome
1. Genetic anamnesis and family tree (consanguinity++)
2. Hair, eyebrows examination with polarized light (trichothiodystrophy,
Nethertons syndrome)
3. Search for lipid inclusions in leukocytes (Dorfman Chanarin syndrome,
Neonatal Gaucher disease)
4. Skin biopsy for transglutaminase assay, conventional and electron
microscopy. Keep frozen sample if possible for further studies
5. Blood sample for specialized biochemical and molecular studies
6. Others: neurosensory evaluation, bone X rays when needed
be quite mild (ichthyosis vulgaris type) or even difficult to detect
[this has been seen especially documented at the Unit de
Dermatologie Pdiatrique, Hpital Pellegrin Enfants (Bordeaux,
France) in patients diagnosed with trichothiodystrophy].
At birth, the clinical frontier of the most severe forms with
the so-called Harlequin fetus or kratome malin by French
authors, is now more blurred, as systemic retinoids have
allowed such patients to survive the neonatal period.3 In the
least severe forms, X-linked hypohidrotic ectodermal dysplasia
should be discussed if associated clinical dysmorphic features
are found, because overheating the baby may have tragic
consequences.
Why is the ichthyotic phenotype at its peak at birth? One
possible explanation is the absence of an airliquid interface in
utero that does not allow the epidermal differentiation
programme to progress to its complete development, which is
seen in normal human cultured epidermis maintained in
immersion. This may exacerbate the consequence of some
inherited epidermal differentiation anomalies.
The practical consequences for paediatric management
are manifold. A collodion baby is the equivalent of a highly
premature baby in terms of epidermal barrier, with a high
transepidermal water loss and a major risk of dehydration and
hypothermia.4 The baby must be admitted to the intensive care
unit to prevent this risk. Placement in a humidified incubator is
still considered as the most important decision, even though
susceptible to an increased risk of skin colonization with
harmful microbes. The incubator should be set at 90100%
hygrometry. The role of emollients is discussed in the Rotterdam
paper where they were found to increase the risk of infection.
At the Unit de Dermatologie Pdiatrique, Hpital Pellegrin
2002 European Academy of Dermatology and Venereology
JDV_478.fm Page 437 Tuesday, September 10, 2002 5:13 PM
Editorial 437
Enfants (Bordeaux, France) we bathe the child daily with
diluted chlorhexidine, followed by a rinse and then sterile petrolatum is used twice daily, which favours the shedding of
membranes and limits water loss. The discipline of hand
washing and the other measures to limit exposure to infections
routinely used in the intensive care unit are mandatory. The use
of intravenous lines and blood sampling should be severely
restricted to avoid further skin damage and the risk of systemic
infections. The weight of the child is the best clinical indicator
for the adaptation of nutriments and fluid intake. However, in
severe cases, in particular Nethertons syndrome (rarely clearly
documented at birth as a collodion baby), when hypernatraemic
dehydration is life threatening, an umbilical artery catheter may
be necessary.
The prophylactic use of antibiotics is not recommended. A
multisite assessment of the cutaneous microflora should be
done initially and monitored on a regular basis or when needed,
and cutaneous or systemic infections detected early and treated
appropriately. Ophthalmological management of ectropion is
important for the prevention of conjunctivitis and keratitis. The
management of pain should not be forgotten. A water bed is
useful and the prophylactic use of mild antalgics before daily
bathing and skin care is appropriate. Sedation with opioids may
be indicated when handling the child is very painful. The use of
retinoids may be considered when the shedding of the collodion
membrane is much delayed (after 3 weeks), because of the
infectious risk associated with the humidified milieu in
the incubator, and mostly because of the intrinsic severity of
the underlying ichthyosis. In that case, acitretin may be given at
0.5 0.75 mg/ kg per day.5
Eventually, one of the most challenging problems is to
communicate with the family of a first child born with this
syndrome. The long-term prognosis is difficult to address at
birth, and the compromised skin status of the child is difficult
to understand for the family. A very prudent approach is
mandatory to avoid further anxiety and a sense of guilt in the
parents, and to help them dealing with this distressing episode.
Coping develops quite naturally when the parents are allowed
to participate in the care of their baby. Prenatal diagnosis can
be discussed later in severe phenotypes.6,7
References
1 Larrgue M, Ottavy N, Bressieux JM, Lorette G. Bb collodion:
trente deux nouvelles observations. Ann Dermatol Venereol 1986;
113: 773 785.
2 Hohl D, Aeschlimann D, Huber M. In vitro and rapid in situ transglutaminase assays for congenital ichthyoses a comparative study.
J Invest Dermatol 1998; 110: 268 271.
3 Haftek M, Cambazard F, Dhouailly D et al. A longitudinal study of a
harlequin infant presenting clinically as non-bullous congenital
ichthyosiform erythroderma. Br J Dermatol 1996; 135: 448 453.
4 Buyse L, Graves C, Marks R et al. Collodion baby dehydration: the
danger of high transepidermal water loss. Br J Dermatol 1993; 129:
86 88.
5 Lacour M, Mehta-Nikhar B, Atherton DJ, Harper JI. An appraisal of
acitretin therapy in children with inherited disorders of keratinization.
Br J Dermatol 1996; 134: 1023 1029.
6 Pigg M, Gedde-Dahl T Jr, Cox DW et al. Haplotype association and
mutation analysis of the transglutaminase 1 gene for prenatal exclusion
of lamellar ichthyosis. Prenat Diagn 2000; 20: 132137.
7 Schorderet DF, Huber M, Laurini RN et al. Prenatal diagnosis of
lamellar ichthyosis by direct mutational analysis of the keratinocyte
transglutaminase gene. Prenat Diagn 1997; 17: 483 486.
Visit the EADV website at: www.eadv.org
2002 European Academy of Dermatology and Venereology JEADV (2002) 16, 436 437
You might also like
- Medical Journals Year in Body Mods 2012 12-30-12Document24 pagesMedical Journals Year in Body Mods 2012 12-30-12Hadi FirmansyahNo ratings yet
- Lower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANDocument3 pagesLower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANHadi FirmansyahNo ratings yet
- Medical Journals Year in Body Mods 2012 12-30-12Document24 pagesMedical Journals Year in Body Mods 2012 12-30-12Hadi FirmansyahNo ratings yet
- Bleomycin and The SkinDocument8 pagesBleomycin and The SkinHadi FirmansyahNo ratings yet
- 10 5923 J Surgery 20140301 03 PDFDocument4 pages10 5923 J Surgery 20140301 03 PDFJacobMsangNo ratings yet
- White Piedra in A Mother and DaughterDocument3 pagesWhite Piedra in A Mother and DaughterHadi FirmansyahNo ratings yet
- Bleomycin in The Treatment of Keloids and Hypertrophic Scars by Multiple Needle PuncturesDocument10 pagesBleomycin in The Treatment of Keloids and Hypertrophic Scars by Multiple Needle PuncturesHadi FirmansyahNo ratings yet
- Chae Et Al-2015-Journal of Cosmetic DermatologyDocument7 pagesChae Et Al-2015-Journal of Cosmetic DermatologyHadi FirmansyahNo ratings yet
- Co-Isolation of Trichosporon Inkin and CandidaDocument8 pagesCo-Isolation of Trichosporon Inkin and CandidaHadi FirmansyahNo ratings yet
- Treatment of Keloids and Hypertrophic ScarsDocument9 pagesTreatment of Keloids and Hypertrophic ScarsHadi FirmansyahNo ratings yet
- Wilske B. Epidemiology and Diagnosis of Lyme Borreliosis 2005Document12 pagesWilske B. Epidemiology and Diagnosis of Lyme Borreliosis 2005Hadi FirmansyahNo ratings yet
- JorgenDocument5 pagesJorgenHadi FirmansyahNo ratings yet
- Verrucous Lepromatous Leprosy A Rare Form ofDocument4 pagesVerrucous Lepromatous Leprosy A Rare Form ofHadi FirmansyahNo ratings yet
- Fatal Metastatic Cutaneous Squamous Cell Carcinoma Evolving From A Localized Verrucous Epidermal NevusDocument11 pagesFatal Metastatic Cutaneous Squamous Cell Carcinoma Evolving From A Localized Verrucous Epidermal NevusHadi FirmansyahNo ratings yet
- A Case of Basal Cell Carcinoma Arising in Epidermal Nevus: CameoDocument3 pagesA Case of Basal Cell Carcinoma Arising in Epidermal Nevus: CameoHadi FirmansyahNo ratings yet
- Collodion Baby and Loricrin Keratoderma: A Case Report and Mutation AnalysisDocument5 pagesCollodion Baby and Loricrin Keratoderma: A Case Report and Mutation AnalysisHadi FirmansyahNo ratings yet
- Lepromatous Leprosy A Case Simulating VerrucousDocument5 pagesLepromatous Leprosy A Case Simulating VerrucousHadi FirmansyahNo ratings yet
- New Developments in Ochronosis: Review of The LiteratureDocument6 pagesNew Developments in Ochronosis: Review of The LiteratureHadi FirmansyahNo ratings yet
- Xerosis CutisDocument6 pagesXerosis CutisHadi FirmansyahNo ratings yet
- Cutaneous Annular Sarcoidosis Developing On A Background of Exogenous Ochronosis: A Report of Two Cases and Review of The LiteratureDocument5 pagesCutaneous Annular Sarcoidosis Developing On A Background of Exogenous Ochronosis: A Report of Two Cases and Review of The LiteratureHadi FirmansyahNo ratings yet
- Thayer Martin Agar Procedure 08Document1 pageThayer Martin Agar Procedure 08Hadi FirmansyahNo ratings yet
- Xerosis CutisDocument6 pagesXerosis CutisHadi FirmansyahNo ratings yet
- Dermatologica Sinica: Cheng-Han Lee, Yi-Chun Chen, Yung-Tsu Cho, Chia-Ying Chang, Chia-Yu ChuDocument5 pagesDermatologica Sinica: Cheng-Han Lee, Yi-Chun Chen, Yung-Tsu Cho, Chia-Ying Chang, Chia-Yu ChuHadi FirmansyahNo ratings yet
- 1999 1 1 29 36Document8 pages1999 1 1 29 36Hadi FirmansyahNo ratings yet
- JorgenDocument5 pagesJorgenHadi FirmansyahNo ratings yet
- New Developments in Ochronosis: Review of The LiteratureDocument6 pagesNew Developments in Ochronosis: Review of The LiteratureHadi FirmansyahNo ratings yet
- Patch Test FDEDocument8 pagesPatch Test FDEHadi FirmansyahNo ratings yet
- Can P Rio Biotics Prevent VaginitisDocument2 pagesCan P Rio Biotics Prevent VaginitisHadi FirmansyahNo ratings yet
- 1486 - Vitamin D PaperDocument9 pages1486 - Vitamin D PaperHadi FirmansyahNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Webrep - Cgi 4Document1 pageWebrep - Cgi 4viridiana bonillaNo ratings yet
- HS - I Don't Feel Weel TodayDocument10 pagesHS - I Don't Feel Weel Todaychie NbaNo ratings yet
- Artesunato MefloquinaDocument11 pagesArtesunato MefloquinaDavid CerrónNo ratings yet
- Resbakuna - Comirnaty PoU Deck For Site Training and Education-FINAL-013122Document53 pagesResbakuna - Comirnaty PoU Deck For Site Training and Education-FINAL-013122toledanagerald516No ratings yet
- Community Project Proposal (Rabbi Petallar)Document2 pagesCommunity Project Proposal (Rabbi Petallar)Gerald Riate100% (1)
- Antibiotic Prophylaxis in Pediatric Odontology. An UpdateDocument6 pagesAntibiotic Prophylaxis in Pediatric Odontology. An UpdateJavier Farias VeraNo ratings yet
- SCREENING FOR DISEASEDocument15 pagesSCREENING FOR DISEASEDr. Radhay ShyamNo ratings yet
- Vaccine Guide - Randall NeustaedterDocument6 pagesVaccine Guide - Randall NeustaedterttreksNo ratings yet
- Awareness of Mother With Baby PacifierDocument10 pagesAwareness of Mother With Baby PacifierIJAR JOURNALNo ratings yet
- COA OB WardDocument17 pagesCOA OB WardChristian PasiliaoNo ratings yet
- Pamphlet TemplateDocument2 pagesPamphlet TemplateZoe ColemanNo ratings yet
- Fluids and Electrolytes in ElderlyDocument7 pagesFluids and Electrolytes in ElderlyDithaNo ratings yet
- Patient Care StudyDocument49 pagesPatient Care StudyKwabena AmankwaNo ratings yet
- Cabizares Handle CaseDocument8 pagesCabizares Handle CaseMae AbabonNo ratings yet
- Basic Principles of Nursing EthicsDocument2 pagesBasic Principles of Nursing Ethicsalena volinaNo ratings yet
- Asante Teaching Hospital Activity Based CostingDocument3 pagesAsante Teaching Hospital Activity Based CostingMuskanNo ratings yet
- Revised SNCU Mentoring ChecklistDocument6 pagesRevised SNCU Mentoring Checklistrani26octNo ratings yet
- 248-Article Text-614-1-10-20210714Document7 pages248-Article Text-614-1-10-20210714Abl ApriliaaNo ratings yet
- ASTHMADocument16 pagesASTHMAAyesigwa Gerald96100% (1)
- USMLE Images For The BoardsDocument297 pagesUSMLE Images For The BoardsMulham Etki100% (3)
- CDI Module 19: Behavior Change Communication: ©jhpiego Corporation The Johns Hopkins UniversityDocument34 pagesCDI Module 19: Behavior Change Communication: ©jhpiego Corporation The Johns Hopkins University420192420192No ratings yet
- History Patient - Co.ukDocument14 pagesHistory Patient - Co.ukiuytrerNo ratings yet
- Ncma217 Performancetask#5 TinioDocument7 pagesNcma217 Performancetask#5 TinioAndhee Mae TinioNo ratings yet
- World Health OrganizationDocument18 pagesWorld Health OrganizationsulyNo ratings yet
- MSEB - Claim - Form 2016 MahaGencoDocument2 pagesMSEB - Claim - Form 2016 MahaGencoAnonymous pKsr5vNo ratings yet
- Medical Act outlines requirements for medical practiceDocument13 pagesMedical Act outlines requirements for medical practiceCornelio AlfonsoNo ratings yet
- Global Epidemiology of Hepatitis B Virus (HBV) Infection: Elizabeth W. Hwang, MD, Ramsey Cheung, MDDocument7 pagesGlobal Epidemiology of Hepatitis B Virus (HBV) Infection: Elizabeth W. Hwang, MD, Ramsey Cheung, MDivan gartikaNo ratings yet
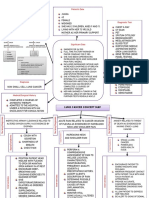
- Lung Cancer Concept Map-Group 2Document2 pagesLung Cancer Concept Map-Group 2Maria Cristina100% (2)
- The Hospital Formulary: Bilal Hassan M.Phil PharmaceuticsDocument11 pagesThe Hospital Formulary: Bilal Hassan M.Phil PharmaceuticsShafaqat Ghani Shafaqat GhaniNo ratings yet
- MT 1 NurseDocument36 pagesMT 1 NurseShipra dhingraNo ratings yet