Professional Documents
Culture Documents
1999 1 1 29 36
Uploaded by
Hadi FirmansyahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1999 1 1 29 36
Uploaded by
Hadi FirmansyahCopyright:
Available Formats
AIDS Rev 1999; 1: 29-36
HIV Protease Inhibitor-induced
Lipodystrophy Syndrome
Andrew Carr
HIV Medicine Unit, St. Vincents Hospital, Sydney, Australia
Abstract
Human immunodeficiency virus (HIV) protease inhibitor (PI) therapy can cause a
syndrome of lipodystrophy (peripheral fat wasting and/or central fat accumulation),
hyperlipidaemia and insulin resistance. Type 2 diabetes mellitus appears to be a
related, but less common, toxicity. Lipodystrophy occurs with all licensed,
potent PIs after a median of about 10 months PI therapy. Any relationship to
non-PI therapy or HIV disease appears limited. The syndrome may be due to
the inhibition of two lipid regulatory proteins that have substantial homology to the
catalytic site of HIV protease, namely cytoplasmic retinoic acid binding protein type
1 (CRABP-1) and low density lipoprotein-receptor-related protein (LRP). There are
no validated, objective diagnostic criteria at present but measurement of body fat
mass may be useful. There is no proven therapy for any component of the
syndrome. The full clinical significance of the syndrome is unknown but, in
addition to the cosmetic effect, metabolic disturbances may increase the risk of
longterm cardiovascular disease.
Key words
HIV. Lipodystrophy. Protease inhibitors. Insulin resistance. Hyperlipidaemia.
Diabetes mellitus.
Introduction
Protease inhibitors (PIs) of HIV confer virological, immunological and clinical, including survival, benefits1,2. A PI in combination with nucleoside analogue HIV reverse transcriptase inhibitors
is now standard of care antiretroviral therapy3,4.
The potency and sustained effects of combination
PI therapy have led to its widespread usage for
patients at almost every stage of disease, including primary HIV infection.
Many PI toxicities, including renal calculi and
nephropathy with indinavir, nausea, diarrhea and
perioral paraesthesiae with ritonavir, and diarrhea
with nelfinavir and soft-gel saquinavir, are not usuaCorrespondence to:
Andrew Carr
HIV Medicine Unit
St. Vincents Hospital
Sydney 2010 Australia
lly serious and resolve rapidly with discontinuation. An immune reactivation syndrome can occur
in patients with subclinical infections (eg. hepatitis
B or C, Mycobacterium avium)5-7. Excessive bleeding in haemophiliacs and portal vein thromboses,
although potentially serious, are relatively rare8,9.
These adverse effects will not be reviewed here.
Generalised wasting is a common manifestation of advanced HIV infection and is predominantly due to loss of muscle mass10,11. Until recently, however, regional fat wasting had not been
reported in patients with HIV infection nor as a
consequence of any drug therapy. We and others
noted PI recipients developing peripheral wasting, central obesity, hyperlipidaemia and diabetes
mellitus following the introduction of PI therapy
(Fig. 1, Table 1)12-15. Several groups have subsequently explored the interaction between HIV PIs,
body fat, serum lipids and insulin sensitivity.
AIDS Rev 1999; 1
Table 1. Physical and metabolic features of lipodystrophy
syndrome.
A. Physical features
One or more of the following (on physical examination or by
patient report) since commencing HIV protease inhibitor
therapy:
1. Fat wasting
face
arms
legs
buttocks
2. Fat accumulation abdomen
dorso-cervical spine (buffalo hump)
breasts (women)
3. Possible features ingrown toenails
dry skin and lips
B. Metabolic features
One or more of the following since commencing HIV
protease inhibitor therapy:
1. Hyperlipidaemia
fasting cholesterol > 5.5 mmol/L
and/or
fasting triglyceride > 2.0 mmol/L
2. Glucose intolerance fasting glucose > 6.1 mmol/L
2 hour OGTT glucose > 7.8 mmol/L
Changes should not be attributed to therapy if:
1. AIDS-defining event or other severe clinical illness in the
last 3 months.
2. Use of anabolic steroids, glucocorticosteroids, immune
modulators in the last 3 months.
A I D S R E V I E W S
Clinical features
30
In the largest study to date, we cross-sectionally
evaluated 116 HIV-infected, otherwise well, adults
receiving at least one HIV PI, 32 HIV-infected PInave patients and 47 healthy male controls12.
Lipodystrophy was defined clinically by patient report of fat wasting in one or more of face, arms or
legs with or without central obesity and confirmed
by physical examination. Patients with weight
change but without peripheral fat wasting were not
defined as having lipodystrophy. It should be emphasised, however, that there is no validated accepted definition of lipodystrophy.
Lipodystrophy was reported by 74 (64%) PI recipients after a mean 13.6 months therapy versus
1 (3%) PI-nave HIV-infected patient (P=0.0001,
Table 2). Wasting occurred with equal frequency in
all body regions, including the trunk, except the
abdomen where patients reported obesity (Fig. 1).
Lipodystrophy occurred with all potent PIs and the
median time to onset of lipodystrophy was 10
months (Fig. 2a). Lipodystrophy did not resolve in
any patient but improved in a few who switched
from ritonavir-saquinavir to indinavir. Many patients
with lipodystrophy were mistakenly assumed to
have HIV wasting syndrome with its psychological,
social and economic consequences.
Dual energy X-ray absorptiometry (DEXA) confirmed the clinical findings12,16. PI recipients had
comparable body weight and fat free mass but
significantly lower fat mass overall and in each
body region except the central abdomen than
both PI-nave patients and healthy males. Importantly, PI-nave patients had similar total and cen-
tral fat mass to controls. The estimated loss in
body fat/month during the first year of PI therapy
was 0.40 kg/month12.
The main risk factor for lipodystrophy (apart
from PI therapy) was longer duration of PI therapy
(Fig. 1). After a mean 22 months follow-up the
prevalence of lipodystrophy in our PI cohort had
increased to 83%; using a patient-rated severity
scale (that concurred with DEXA), lipodystrophy
was severe overall in only 11%17. Peripheral
lipodystrophy was observed in 25% of patients receiving indinavir for 1 year12. Another cohort study
found cumulative rates of 3, 11, 29, 63 and 75%
after 6, 12, 18, 24 and 30 months PI therapy, respectively18. Lipodystrophy has not been found to
be associated with CD4+ lymphocyte counts, HIV
RNA levels or use of other drugs including other
classes of antiretrovirals.
Miller et al showed that the abdominal distension in patients receiving indinavir was due to accumulation of visceral fat, with stable or declining
levels of subcutaneous abdominal fat14. Further,
they found that this accumulation occurred in
those receiving at least 6 months therapy. Hengel
reported a group of PI recipients with multiple lipomata19; it is possible, of course, that this represents fat wasting surrounding a pre-existing invisible lipoma.
There are several reports of fatty enlargement of
the dorso-cervical fat pad (buffalo hump) in HIVinfected patients, although some patients were not
receiving PIs and so the relationship of buffalo
hump to PI therapy is unclear15,20-22. Buffalo hump
appears less common than wasting or abdominal
obesity17.
Women and children receiving protease inhibitors also develop lipodystrophy. An additional
feature in women is breast hypertrophy23-26.
Whether there are other differences in prevalence
rates or severity between men and women or between ethnic groups is unknown. Controlled,
prospective, longterm prevalence studies have not
been reported.
There have been small numbers of reports of patients not receiving PIs with physical features of
lipodystrophy12,14,25; the aetiology in these patients
is unclear.
Metabolic features
Advanced HIV infection is associated with low
serum cholesterol levels and mild hypertriglyceridaemia10. PI therapy is associated with significant
disturbances in both lipid and glucose metabolism12,14,27-40. In turn, patients with lipodystrophy
have more abnormal lipid and glucose metabolism
than those without lipodystrophy, confirming that
the metabolic and clinical disturbances are two
components of the one syndrome12.
Combined hyperlipidaemia was identified in both
phase-1 studies of the protease inhibitor ritonavir1,41.
This developed within weeks and persisted for the
duration of therapy. Interestingly, no phase 2 or 3
studies of any PI systematically evaluated lipid or glu-
Andrew Carr: HIV Protease Inhibitor-induced Lipodystrophy Syndrome
cose metabolism. Numerous studies have now confirmed that combined hyperlipidaemia is common
with all potent PIs and persists in those remaining on
therapy17. The effect of PI withdrawal is unknown.
Several reports have identified diabetes with PI
therapy12,28-30. In previously non-diabetic patients, the
clinical presentation was usually asymptomatic and
non-ketotic (i.e. type-2 diabetes) and in long standing, type-1 diabetics, daily insulin requirements increased within weeks of commencing therapy. Serum
insulin, C-peptide, insulin secretion and insulin resistance all increase12,30, and proportionally to lipodystrophy severity17. Type-2 diabetes was thought to be
uncommon (0.1 to 1%), but systematic studies using
A I D S R E V I E W S
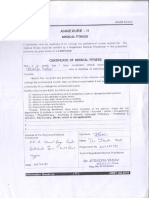
Fig. 1. Characteristic physical features of the lipodystrophy syndrome in several patients receiving HIV protease inhibitors. There is
fat wasting of the face (a) legs (b) and buttocks (c) and fat accumulation in the abdomen (d), breasts (e) and dorso-cervical fat
pad (f).
31
AIDS Rev 1999; 1
Table 2. Possible therapeutic strategies.
Problem
Possible therapy
(example)
Comments
Fat wasting
anabolic steroids
growth hormone
testosterone
glitazones
troglitazone
rexinoid
cis-9-RA
anabolic for muscle not fat
increases insulin resistance
anabolic for muscle not fat
PPAR- agonist (? anabolic for fat)
potential P450 interaction (? increased risk of troglitazone-induced
hepatitis)
RXR agonist (? anabolic for fat)
atorvastatin
clofibrate
? intralesional for buffalo hump
could exacerbate peripheral fat wasting
could exacerbate peripheral fat wasting
potential P450 interaction (? increased risk for statin-induced myositis)
-
Fat accumulation
Hyperlipidaemia
Insulin resistance
Diabetes mellitus
growth hormone
low fat diet
increased exercise
statins
fibrates
diet
exercise
diet
exercise
oral hypoglycaemics
insulin
treat as for type 2 diabetes mellitus in general population
sulphonylureas
For all manifestations, unproven options include:
switching from ritonavir-saquinavir to indinavir or nelfinavir
cessation of all protease inhibitors
Patients should be monitored for cardiovascular symptoms and signs
A I D S R E V I E W S
Potential cardiovascular risk factors should be addressed:
32
hypertension, smoking, physical inactivity
oral glucose tolerance testing found a prevalence of
6 to 9% with a further 16% of patients in one study
having impaired glucose tolerance17,30. Type-2 diabetes in the general population usually results from
both insulin resistance and impaired insulin secretion.
This may explain why lipodystrophy is more common
with PI therapy than hyperglycaemia.
It should be noted that neither PI use nor presence of lipodystrophy has been associated with
significant differences in liver function, or in plasma
leptin, testosterone, sex hormone binding globulin,
prolactin, cortisol, C3 or tumour necrosis factoralpha levels12,15. Additionally, dexamethasone suppression tests are normal15.
The early differential effect of ritonavir-saquinavir
versus indinavir or nelfinavir might arise because
PIs have differential capacities to cause this syndrome or may merely represent the use of more
than one PI. The relative contributions of ritonavir
and saquinavir has not been assessed, although
the syndrome was not reported when hard-gel
saquinavir was the only widely available PI.
Whether soft-gel saquinavir, amprenavir, or nonpeptidomimetic protease inhibitors such as
tipranivir cause lipodystrophy is not known.
Comparison of indinavir, ritonavirsaquinavir and nelfinavir
There have been two reports of patients receiving PIs developing ischaemic heart disease42,43.
However, a causal link has not been demonstrated
and there are no data estimating prevalence or risk
factors of cardiovascular disease in patients receiving PIs or non-PI therapy. Some cases have occurred in patients with other risk factors, and others in
those who had received PI therapy for a very short
period and therefore are more likely to represent a
prothrombotic effect of PI therapy rather than an atherosclerotic effect.
Patients with diabetes mellitus or impaired glucose tolerance are at increased risk for microvascular diabetic disease such as retinopathy, neuropathy and nephropathy over a 5-year period44.
Patients on longterm stable PI therapy should probably be monitored for these conditions.
Both the clinical and metabolic features of the
syndrome are more abnormal in patients receiving
ritonavir-saquinavir when compared to those receiving indinavir, at least early in therapy (Table 2;
Fig. 2b)12,25,31. Several studies have reported that
nelfinavir has similar effects to indinavir early in
therapy17,25. However, with prolonged therapy (a
mean 22 months), all features of the syndrome (except for hypertriglyceridaemia) became similar regardless of PI type, suggesting that fat changes
have finite limits that are merely reached earlier with
ritonavir-saquinavir17. One early report suggested
that diabetes associated with indinavir may improve
in some patients who switch to nelfinavir37.
Cardiovascular disease and protease
inhibitors
Andrew Carr: HIV Protease Inhibitor-induced Lipodystrophy Syndrome
Diagnosis
Patient report appeared useful for diagnosis of
lipodystrophy as self-reported presence or absence of fat wasting related to body fat mass using
DEXA12. Nevertheless, given the large variability in
body fat in the general and HIV-infected populations, mean body fat appeared insufficient for diagnosis of all cases. Metabolic abnormalities may also
be useful diagnostically17. Changes in body fat and
metabolic parameters following commencement of
PI therapy may well improve diagnosis, but this has
not been demonstrated. As there is no gold diagnostic standard for diagnosing lipodystrophy, diagnostic criteria may eventually resemble those for
diseases such as rheumatoid arthritis and systemic
lupus erythematosis, where presence of a minimum
number of clinical and laboratory abnormalities will
confirm the diagnosis. Consensus guidelines are
clearly needed.
Treatment
There is no proven therapy for any component of
the syndrome. Options worthy of investigation are
summarised in Table 2, based on anecdotal and
case reports. Some options have theoretical handicaps which may prevent their routine use. Also, it
is not known whether hyperlipidaemia or insulin resistance in the absence of glucose intolerance
should be treated, nor at what level. Treatment of
lipids alone may not affect cardiovascular risk if insulin resistance is not also addressed (and vice
versa). Factors that would affect a decision to treat
Pathogenesis
All HIV PIs have high affinity for the catalytic site
of HIV protease and so might induce this syndrome
by binding and inhibiting an homologous human
protein(s) involved in lipid metabolism47. A 12
amino acid sequence (aa 19 to 30) spanning the
catalytic region of HIV protease has homologies at
the protein level of 63 percent with a region incorporating a lipid binding domain in the low density
lipoprotein-receptor-related protein (LRP) and of
58 percent with a C-terminal region of the cytoplasmic retinoic acid binding protein type 1
(CRABP-1).
CRABP-1 binds all intracellular RA and presents
A I D S R E V I E W S
Fig. 2. Times to development of lipodystrophy for all patients
receiving protease inhibitors (a) and those receiving
indinavir or ritonavir-saquinavir (b). Lipodystrophy developed
significantly earlier in those receiving ritonavir-saquinavir
(P=0.013).
(Reprinted from ref.12 with permission).
would include the patient status, the likelihood that
PI therapy would be ongoing, the severity of any
feature, and the presence of other cardiovascular
risk factors (Table 3).
The role of diet and exercise have not been evaluated. Although increased exercise or a very restrictive diet might theoretically reduce central fat
accumulation, lipids and insulin resistance, this
might be at the expense of increased peripheral fat
wasting. Certainly, no diet should interfere with PI
drug absorption or overall patient wellbeing.
Some agents may be problematic. Anabolic
steroids are anabolic for muscle not fat, although increased muscle mass may partially disguise fat
loss. Intralesional growth hormone appeared to reduce the size of buffalo humps in 2 patients45, but
can exacerbate insulin resistance if given parenterally and so precipitate diabetes. The statins (lipid
lowering agents) and glitazones (insulin sensitisers
and possible peripheral adipocyte growth factors see below) are metabolised by cytochrome P450
3A (which is inhibited by PIs) and so their use with
PIs could increased the risks for myositis and hepatitis, respectively. Brief reports suggest that gemfibrozil and atorvastatin may be safe and have
some efficacy in lowering lipids32,46.
Surgery (excision or liposuction) has been performed on some patients with severe fat accumulation, although fat may reaccumulate within a matter
of months. There is no report of surgery for fat wasting, an approach used for some forms of congential lipodystrophy.
One theoretical treatment option is PI withdrawal
or substitution. It should be emphasised, however,
that it is not known whether lipodystrophy is reversible if PI therapy is withdrawn. Several studies
are currently evaluating this strategy, using newer
nucleoside analogues and non-nucleoside agents.
Non-PI strategies may well fail in future for other
reasons, however. Therefore, even if non-PI strategies are successful, it is essential that therapies
that prevent the syndrome in those commencing
PIs be developed. Cessation of PIs should be considered for patients who have failed therapy if there
is evidence of lipodystrophy or insulin resistance.
The data mentioned above suggests that substitution with another PI is not likely to be effective for a
large proportion of patients.
33
AIDS Rev 1999; 1
Table 3. Factors that might influence treatment of metabolic
abnormalities.
A I D S R E V I E W S
1. Patient status CD4 count
HIV RNA
prior AIDS
2. Likelihood that PI therapy would be ongoing (non-PI therapy
possible but switching not proven to be effective in
suppressing viral load nor in reversing metabolic
disturbances)
3. Presence of both hyperlipidaemia and impaired glucose
tolerance
4. Diabetic symptoms
5. Pancreatitis related to hyperlipidaemia
6. Presence of known cardiovascular risk factors smoking
hypertension
family history
34
RA to cytochrome P450 3A isoforms that catalyse
RA conversion to cis-9-RA (Fig. 3). Cis-9-RA is the
sole ligand of the retinoid X receptor (RXR) which in
adipocyte nuclei functions as a heterodimer with
peroxisome proliferator activated receptor type
gamma (PPAR-). Ligand binding to RXR or PPAR-
inhibits adipocyte apoptosis and upregulates
adipocyte differentiation and proliferation and
PPAR- is preferentially expressed in peripheral versus central fat. Of note, RXR or PPAR- agonists improve abnormal insulin sensitivity and hyperlipidaemia, and result in peripheral fat accumulation.
CRABP-1 has multiple RA binding residues. HIV
PIs may, therefore, bind this homologous region
within CRABP-1 and so inhibit the binding of RA to
its binding pocket. Reduced cis-9-RA production
would lead to reduced RXR activity and hence to
reduced differentiation and increased apoptosis of
peripheral adipocytes. Both circumstances lead to
hyperlipidaemia via reduced triglyceride storage
and lipid release into the circulation. Necrosis
seems less likely than apoptosis as the condition is
painless12-15.
Cytochrome P450 3A is the sole enzyme that
converts RA to cis-9-RA. HIV PIs are potent inhibitors of cytochrome P450 3A. Indeed, lipodystrophy was worst in those receiving ritonavir12, the
most potent cytochrome P450 3A inhibitor of the PIs.
LRP is an hepatic receptor important for postprandial chylomicron clearance. LRP is complexed
on capillary endothelium with lipoprotein lipase
(LPL), which cleaves fatty acids from circulating
triglycerides, permitting free fatty acid entry into
adipocytes for storage as fat. The homologous region in LRP contains a probable lipid binding domain. PI binding of LRP could, therefore, exacerbate hyperlipidaemia.
Central adipocytes (including perhaps those of
the breast and dorso-cervical fat pad) are more
metabolically active than peripheral adipocytes. In
the presence of impaired peripheral fat storage and
hyperlipidaemia, central fat accumulation may occur by default. In the presence of oestrogen, lipid
would also be sequestered in the breasts. Hyper-
lipidaemia also causes insulin resistance, by interference with post-receptor insulin signalling, competition between glucose and lipid oxidation pathways in skeletal muscle or inhibition of glycogen
synthase.
CRABP-2 has 97 percent homology with CRABP1 and is predominantly expressed in epidermis.
Other adverse events of PI therapy, such as dermatitis, dry lips and nail dystrophy may, therefore,
be a consequence of inhibited RA metabolism in
the integument. LRP is also the primary clearance
receptor for endogenous proteases including tissue
plasminogen activator, a natural anti-coagulant. Increased bleeding in hemophiliacs receiving PIs
suggests that PIs do inhibit LRP function, in this
case its uptake of tissue plasminogen activator.
Future research
Prospective studies are in progress to further
assess the syndromes incidence and severity, and
to determine if any clinical or biochemical parameter predicts the syndrome. Studies of lipodystrophy
in women and children receiving PIs and its reversibility upon ceasing or switching antiretroviral
regimens are required. In vitro and in vivo studies
are required to explore the above hypothesis. A relevant animal model would be welcome.
Longer term follow-up is required to assess
whether vascular complications of insulin resistance and hyperlipidaemia will develop and if there
is any significant morbidity associated with long
term, severe fat depletion.
Newer HIV PIs that do not cause lipodystrophy,
hyperlipidaemia and insulin resistance are required. Candidates include PIs that bind neither
CRABP-1 nor LRP, particularly the non-peptidic PIs.
Summary
The lipodystrophy syndrome is common with prolonged PI therapy. Hyperlipidaemia and impaired
glucose tolerance may lead to longterm micro and
macrovascular disease. Nevertheless, patients with
advanced HIV disease clearly benefit from PIs in
terms of disease progression, survival2 and reversal
of some opportunistic infections48. Any survival advantage in early HIV disease is unproven, however,
although biologically plausible and widely advocated 3,4. Non-PI therapy may be as potent as PI
combination therapy49 and needs to be explored as
a therapeutic option for HIV infection, particularly
early disease.
The manner in which this syndrome has been
identified highlights the need for more thorough interpretation of pre-licensing data and for more
thorough post marketing surveillance of agents approved under accelerated licensing processes. Understanding the underlying mechanisms should
lead to treatment strategies and to the design of
new PIs that do not cause this syndrome
Andrew Carr: HIV Protease Inhibitor-induced Lipodystrophy Syndrome
References
1. Danner S, Carr A, Leonard J, et al. Safety, pharmacokinetics
and preliminary efficacy of ritonavir, an inhibitor of HIV-1 protease. N Engl J Med 1995; 333: 1528-33.
2. Hammer S, Squires K, Hughes M, et al. A controlled trial of two
nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. N Engl J Med 1997; 337: 725-33.
3. Carpenter C, Fischl M, Hammer S, et al. Antiretroviral therapy for
HIV infection in 1997: updated recommendations of the International AIDS Society - USA panel. JAMA 1998; 280: 78-86.
4. Gazzard B, Moyle G, on behalf of the BHIVA Guidelines Writing
Committee. 1998 revision to the British HIV Association Guidelines for Antiretroviral Treatment of HIV Seropositive Individuals.
Lancet 1998; 352: 314-6.
5. Carr A, Cooper D. Restoration of immunity to chronic hepatitis B
infection in HIV-infected patient on protease inhibitor (letter).
Lancet 1997; 349: 995-6.
6. Race E, Adelson-Mitty J, Kriegel G, et al. Focal mycobacterial
lymphadenitis following initiation of protease-inhibitor therapy in
patients with advanced HIV-1 disease. Lancet 1998; 351: 252-5.
7. French M, Lenzo N, John M, et al. Immune restoration disease
after treatment of immunodeficient HIV-infected patients with
potent anti-retroviral therapy. In: Abstracts of the 12th World
AIDS Conference, Geneva, June, 1998 (abstract 22323).
8. Deeks S, Smith M, Holodny M, et al. HIV-1 Protease inhibitors:
a review for clinicians. JAMA 1997; 277: 145-53.
9. Carr A, Brown D, Cooper D. Portal vein thrombosis in patients
receiving indinavir (letter). AIDS 1997; 11: 1657-8.
10. Grunfeld C, Feingold K. Metabolic disturbances and wasting in
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
the acquired immunodeficiency syndrome. N Engl J Med 1992;
327: 329-37.
Paton N, Macallan D, Jebb S, et al. Longtitudinal changes in
body composition measured with a variety of methods in patients with AIDS. J Acquir Immune Defic Syndr Hum Retrovirol
1997; 14: 119-27.
Carr A, Samaras K, Burton S, et al. A Syndrome of peripheral
lipodystrophy, hyperlipidaemia and insulin resistance in patients
receiving HIV protease inhibitors. AIDS 1998; 12: F51-8.
Viraben R, Aquilina C. Indinavir-associated Lipodystrophy. AIDS
1998; 12: F37-9.
Miller K, Jones E, Yanovski J, et al. Visceral abdominal-fat accumulation associated with use of indinavir. Lancet 1998; 351: 871-5.
Lo J, Mulligan K, Tai V, et al. Buffalo hump in men with HIV-1
infection. Lancet 1998; 351: 867-70.
Bonjoch A, Veny A, Johnston S, et al. Body composition measurements by anthropometry and bioelectrical impedance to
evaluate redistribution of body fat in HIV-positive patients on antiretroviral treatment. In: Abstracts of the 37th ICAAC, San
Diego, September, 1998 (abstract 1-94).
Carr A, Samaras K, Thorisdottir A, et al. Prevalence and severity of protease inhibitor-induced lipodystrophy and insulin resistance. In: Abstracts of the 12th World AIDS Conference, Geneva, June, 1998 (abstract 22323).
Veny A, Bonjoch A, Romeu J, et al. Cumulative risk for developing protease inhibitor-associated lipodystrophy in HIV-infected
patients. In: Abstracts of the 37th ICAAC, San Diego, September, 1998 (abstract 1-92).
Hengel R, Watts N, Lennox J. Multiple symmetrical lipomatosis
associated with protease inhibitors. Lancet 1997; 350: 1596.
Roth V, Kravcik S, Angel J. Development of cervical fat pads
A I D S R E V I E W S
Fig. 3. Proposed mechanism of HIV protease inhibitor (PI)-induced peripheral lipodystrophy, hyperlipidaemia, central obesity,
breast hypertrophy and insulin resistance.
Sites of protease inhibitor action are represented by solid bars, dashed arrows and encircled numerals. The primary event is
impaired generation of cis-9-retinoic acid (cis-9-RA) from retinoic acid (RA), either by direct binding to cytoplasmic retinoic acid
binding protein type 1 (CRABP-1)1 or by inhibition of cytochrome P450 3A isoforms that metabolise RA to cis-9-RA2. This leads to
reduced retinoid X receptor (RXR) stimulation and so to apoptosis and impaired differentiation of peripheral adipocytes, with lipid
release and/or reduced lipid storage. Inhibition of low density lipoprotein receptor-related protein (LRP) would lead to reduced
cleavage of fatty acids from circulating triglycerides by the LRP-lipoprotein lipase (LPL) complex on vascular endothelium3 and
reduced hepatic uptake of chylomicrons4. The resulting hyperlipidaemia would lead to some fat redistribution to the abdomen (and
in the breasts under the influence of oestrogen) and to insulin resistance, with secondary type 2 diabetes mellitus in susceptible
individuals. Inhibition of CRABP-2 would result in ectodermal dysplasia (ingrown toenails, dry lips and skin)5. Inhibition of LRP
would also block uptake of tissue plasminogen activator (tPA) and so lead to increased bleeding in haemophiliacs6.
(Modified from ref. 38 with permission).
35
AIDS Rev 1999; 1
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
A I D S R E V I E W S
36.
36
following therapy with human immunodeficiency virus type 1
protease inhibitors. Clin Infect Dis 1998; 27: 65-7.
Miller K, Daly P, Sentochnik D, et al. Pseudo-cushings syndrome in human immunodeficiency virus-infected patients. Clin
Infect Dis 1998; 27: 68-72.
Striker R. Localized adipose tissue hypertrophy in patients receiving human immunodeficiency virus protease inhibitors. Clin
Infect Dis 1998; 27: 218-9.
Herry I, Bernard L, de Truchis P, Perronne C. Hypertrophy of the
breasts in a patient treated with indinavir (letter). Clin Infect Dis
1997; 25: 937-8.
Dong K, Flynn M, Dickinson B, et al. Changes in body habitus in
HIV+ women after initiation of protease inhibitor therapy. In: Abstract of the 12th World AIDS Conference, Geneva, June, 1998
(abstract 12373).
Gervasoni C, Ridolfo AL, Trifiro G, et al. Redistribution of body fat
in HIV-infected women undergoing combined antiretroviral therapy: Clinical immunological, and Metabolic Analyses. In: Abstracts
of the 37th ICAAC, San Diego, September, 1998 (abstract 1-93).
Regan AM, Babl FE. Abnormal body fat accumulations in HIVinfected children on antiretroviral therapy. In: Abstract of the 37th
ICAAC, San Diego, September, 1998 (abstract 1-86).
Mulligan K, Tai VW, Algren H, et al. Evidence of unique metabolic effects of protease inhibitors. In: Abstract of the 5th Conference on Retroviruses and Opportunistic Infections, Chicago,
February, 1998, (abstract 414).
Lumpkin M. Reports of diabetes and hyperglycaemia in patients receiving protease inhibitors for the treatment of human immunodeficiency virus infection. FDA Public Health Advisory, June 11, 1997.
Dube M, Johnson D, Currier J, et al. Protease inhibitor-associated hyperglycaemia (letter). Lancet 1997; 350: 713-4.
Walli R, Herfort O, Michl G, et al. Treatment with protease inhibitors associated with peripheral insulin resistance and impaired glucose tolerance in HIV-1-infected patients. AIDS 1998;
12: F167-74.
Nelson M, Moyle G, Newell A, et al. The incidence of hyperlipidaemia with protease inhibitors. In: Abstracts of the 37th ICAAC,
San Diego, September, 1998 (abstract 1-87).
Hewitt R, Shelton L. Gemifibrozil effectivity lowers protease inhibitor-associated hypertriglyceridemia in HIV-1+ patients. In:
Abstracts of the 37th ICAAC, San Diego, September, 1998 (abstract 1-88).
Yarasheski KE, Tebas P, Sigmund CM, et al. Insulin resistance
in HIV-protease inhibitor-associated diabetes. In: Abstracts of
the 37th ICAAC, San Diego, September, 1998 (abstract 1-90).
Rothstein A, Caldwell R, Allmon C, et al. Investigation of protease Inhibitor-associated hypercholesterolemia in a universitybased HIV Clinic. In: Abstracts of the 37th ICAAC, San Diego,
September, 1998 (abstract 1-91).
Green R, Raghavan S, Levin K, et al. Change in weight, body
composition, and serum lipids prior to and after initiation of protease inhibitors. In: Abstracts of the 37th ICAAC, San Diego,
September, 1998 (abstract 1-94).
Keruly J, Mehta S, Chaisson R, et al. Incidence of and factors
associated with the development of hypercholesterolemia and
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
hyperglycemia in HIV-infected patients using a protease Inhibitor. In: Abstracts of the 37th ICAAC, San Diego, September,
1998 (abstract 1-95).
Dube M, Johnson D, Currier J, et al. Protease inhibitor-associated hyperglycaemia: results of switching from indinavir to nelfinavir. In: Abstract of the 12th World AIDS Conference, Geneva,
June, 1998 (abstract 32172).
Papadopoulos A, Evangelopoulou E, Nicolaidi N, et al. Serum
lipid changes in HIV-infected patients under combination therapy containing a protease inhibitor. In: Abstract of the 12th World
AIDS Conference, Geneva, June, 1998 (abstract 60018).
Vancouwenberghe C, King JH, Gordon J, et al. Clinical investigation of the incidence and severity of elevated cholesterol and
triglycerides in AIDS patients receiving protease inhibitor therapy. In: Abstracts of the 37th ICAAC, San Diego, September,
1998 (abstract 1-69).
Bernasconi E, Carota A, Megenta L, et al. Metabolic changes in
HIV-infected patients treated with protease inhibito therapy. In:
Abstract of the 12th World AIDS Conference, Geneva, June,
1998 (abstract 12375).
Markowitz M, Saag M, Powderly W, et al. A preliminary study of
ritonavir, an inhibitor of HIV-1 protease, to treat HIV-1 infection.
N Engl J Med 1995; 333: 1534-8.
Henry K, Melroe H, Huebsch J, et al. Severe premature coronary artery disease with protease inhibitors. Lancet 1998; 351:
1328.
Behrens G, Schimdt H, Meyer D, et al. Vascular complications
associated with HIV protease inhibitors. Lancet 1998; 351: 1958.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1998;
21: S5-19.
Torres R. Treatment of dorsocervial fat pads and truncal adiposity with recombinant growth hormone in patients with AIDS
maintained on HAART. In: Abstract of the 12th World AIDS Conference, Geneva, June, 1998 (abstract 32164).
Henry K, Melroe H, Huebesch J, et al. Atorvastatin and gemfibrozil for protease inhibitor-related lipid abnormalities. Lancet
1998; 352: 1031.
Carr A, Samaras K, Chisholm D, et al. Pathogenesis of HIV Protease inhibitor-associated syndrome of peripheral lipodystrophy,
hyperlipidaemia and insulin resistance. Lancet 1998; 351: 1881-3.
Carr A, Marriott D, Field A, et al. Combination antiretroviral therapy of HIV-associated microsporidiosis and cryptosporidiosis.
Lancet 1998; 351: 256-61.
Staszewski S, Morales-Ramirez J, Flanigan T, et al. A Phase
II, multicenter, randomized, open-label study to compare the
antiretroviral activity and tolerability of efavirenz + indinavir,
versus efavirenz + zidovudine + lamivudine, versus indinavir
+ zidovudine + lamivudine at 24 weeks. In: Abstracts of the
12th World AIDS Conference, Geneva, June, 1998 (abstract
22336).
You might also like
- Medical Journals Year in Body Mods 2012 12-30-12Document24 pagesMedical Journals Year in Body Mods 2012 12-30-12Hadi FirmansyahNo ratings yet
- Lower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANDocument3 pagesLower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANHadi FirmansyahNo ratings yet
- Medical Journals Year in Body Mods 2012 12-30-12Document24 pagesMedical Journals Year in Body Mods 2012 12-30-12Hadi FirmansyahNo ratings yet
- Bleomycin and The SkinDocument8 pagesBleomycin and The SkinHadi FirmansyahNo ratings yet
- 10 5923 J Surgery 20140301 03 PDFDocument4 pages10 5923 J Surgery 20140301 03 PDFJacobMsangNo ratings yet
- White Piedra in A Mother and DaughterDocument3 pagesWhite Piedra in A Mother and DaughterHadi FirmansyahNo ratings yet
- Bleomycin in The Treatment of Keloids and Hypertrophic Scars by Multiple Needle PuncturesDocument10 pagesBleomycin in The Treatment of Keloids and Hypertrophic Scars by Multiple Needle PuncturesHadi FirmansyahNo ratings yet
- Chae Et Al-2015-Journal of Cosmetic DermatologyDocument7 pagesChae Et Al-2015-Journal of Cosmetic DermatologyHadi FirmansyahNo ratings yet
- Co-Isolation of Trichosporon Inkin and CandidaDocument8 pagesCo-Isolation of Trichosporon Inkin and CandidaHadi FirmansyahNo ratings yet
- Treatment of Keloids and Hypertrophic ScarsDocument9 pagesTreatment of Keloids and Hypertrophic ScarsHadi FirmansyahNo ratings yet
- Wilske B. Epidemiology and Diagnosis of Lyme Borreliosis 2005Document12 pagesWilske B. Epidemiology and Diagnosis of Lyme Borreliosis 2005Hadi FirmansyahNo ratings yet
- JorgenDocument5 pagesJorgenHadi FirmansyahNo ratings yet
- Verrucous Lepromatous Leprosy A Rare Form ofDocument4 pagesVerrucous Lepromatous Leprosy A Rare Form ofHadi FirmansyahNo ratings yet
- Fatal Metastatic Cutaneous Squamous Cell Carcinoma Evolving From A Localized Verrucous Epidermal NevusDocument11 pagesFatal Metastatic Cutaneous Squamous Cell Carcinoma Evolving From A Localized Verrucous Epidermal NevusHadi FirmansyahNo ratings yet
- A Case of Basal Cell Carcinoma Arising in Epidermal Nevus: CameoDocument3 pagesA Case of Basal Cell Carcinoma Arising in Epidermal Nevus: CameoHadi FirmansyahNo ratings yet
- DocumentDocument3 pagesDocumentHadi FirmansyahNo ratings yet
- Lepromatous Leprosy A Case Simulating VerrucousDocument5 pagesLepromatous Leprosy A Case Simulating VerrucousHadi FirmansyahNo ratings yet
- New Developments in Ochronosis: Review of The LiteratureDocument6 pagesNew Developments in Ochronosis: Review of The LiteratureHadi FirmansyahNo ratings yet
- Xerosis CutisDocument6 pagesXerosis CutisHadi FirmansyahNo ratings yet
- Cutaneous Annular Sarcoidosis Developing On A Background of Exogenous Ochronosis: A Report of Two Cases and Review of The LiteratureDocument5 pagesCutaneous Annular Sarcoidosis Developing On A Background of Exogenous Ochronosis: A Report of Two Cases and Review of The LiteratureHadi FirmansyahNo ratings yet
- Thayer Martin Agar Procedure 08Document1 pageThayer Martin Agar Procedure 08Hadi FirmansyahNo ratings yet
- Xerosis CutisDocument6 pagesXerosis CutisHadi FirmansyahNo ratings yet
- Dermatologica Sinica: Cheng-Han Lee, Yi-Chun Chen, Yung-Tsu Cho, Chia-Ying Chang, Chia-Yu ChuDocument5 pagesDermatologica Sinica: Cheng-Han Lee, Yi-Chun Chen, Yung-Tsu Cho, Chia-Ying Chang, Chia-Yu ChuHadi FirmansyahNo ratings yet
- Collodion Baby and Loricrin Keratoderma: A Case Report and Mutation AnalysisDocument5 pagesCollodion Baby and Loricrin Keratoderma: A Case Report and Mutation AnalysisHadi FirmansyahNo ratings yet
- JorgenDocument5 pagesJorgenHadi FirmansyahNo ratings yet
- New Developments in Ochronosis: Review of The LiteratureDocument6 pagesNew Developments in Ochronosis: Review of The LiteratureHadi FirmansyahNo ratings yet
- Patch Test FDEDocument8 pagesPatch Test FDEHadi FirmansyahNo ratings yet
- Can P Rio Biotics Prevent VaginitisDocument2 pagesCan P Rio Biotics Prevent VaginitisHadi FirmansyahNo ratings yet
- 1486 - Vitamin D PaperDocument9 pages1486 - Vitamin D PaperHadi FirmansyahNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Follow The Instructions For R.I.C.EDocument2 pagesFollow The Instructions For R.I.C.Eayatolla ayatollaTMNo ratings yet
- New Recommendations According To 2022 ILCOR CoSTDocument1 pageNew Recommendations According To 2022 ILCOR CoSTMineTagraNo ratings yet
- Hepatitis PreventionDocument3 pagesHepatitis PreventionazisbustariNo ratings yet
- DHP W. TableDocument21 pagesDHP W. Tablejenika studiesNo ratings yet
- Improve Circulation and Oxygenation During CPR with CPVDocument8 pagesImprove Circulation and Oxygenation During CPR with CPVCode ValmirNo ratings yet
- Hospital Medicine Maintenance of Certification Examination Blueprint - American Board of Internal MedicineDocument4 pagesHospital Medicine Maintenance of Certification Examination Blueprint - American Board of Internal MedicineabimorgNo ratings yet
- Assignment1-UnaniMedicine Dosage LabellingDocument12 pagesAssignment1-UnaniMedicine Dosage LabellingFarhat JahanNo ratings yet
- Encyclopedia of Diseases and Disorders (Gnv64)Document482 pagesEncyclopedia of Diseases and Disorders (Gnv64)Florin Ciobanu100% (12)
- Classification of Congenital Heart DiseasesDocument16 pagesClassification of Congenital Heart DiseasesdoctorriyasNo ratings yet
- Prevalence and Risk Factors of Inguinal Hernia Study in A Semi-Urban Area in Rayalaseema, Andhra PradeshDocument4 pagesPrevalence and Risk Factors of Inguinal Hernia Study in A Semi-Urban Area in Rayalaseema, Andhra Pradeshsamsara vrindaNo ratings yet
- Reis Da Silva 2023 Falls Assessment and Prevention in The Nursing Home and CommunityDocument5 pagesReis Da Silva 2023 Falls Assessment and Prevention in The Nursing Home and CommunityTiago SilvaNo ratings yet
- Referensi No 7Document5 pagesReferensi No 7Bagus Wanda HabibullahNo ratings yet
- Chapter 24 HomeworkDocument9 pagesChapter 24 HomeworkKvn4N6No ratings yet
- Erba Actime - APTTDocument2 pagesErba Actime - APTTthinh.ho2No ratings yet
- Mills 1975Document6 pagesMills 1975Nida AtmimNo ratings yet
- Dental Caries VandhuDocument53 pagesDental Caries Vandhujunaid junuNo ratings yet
- Asbestosis StatPearls NCBIBookshelfDocument11 pagesAsbestosis StatPearls NCBIBookshelfAjeng RahmawatiNo ratings yet
- MORINGO Plus and CellerikDocument38 pagesMORINGO Plus and CellerikARIF PATEL100% (2)
- Medical CcertificateDocument1 pageMedical CcertificateNirmala YadavNo ratings yet
- Admission Form 2935Document6 pagesAdmission Form 2935Erica KatzNo ratings yet
- Ambu BagDocument12 pagesAmbu BagAejaz Ahmad100% (1)
- Abnormal Psychology 6th Edition Nolen-Hoeksema Solutions Manual 1Document26 pagesAbnormal Psychology 6th Edition Nolen-Hoeksema Solutions Manual 1jamie100% (31)
- Nurse Practitioner VS Physical TherapistsDocument5 pagesNurse Practitioner VS Physical Therapistspdet1No ratings yet
- Reumatoid KELOMPOK 8Document11 pagesReumatoid KELOMPOK 8Ida FarizaNo ratings yet
- BFISDocument1 pageBFISEverestNo ratings yet
- Comprehensive Geriatric AssessmentDocument87 pagesComprehensive Geriatric AssessmentNurrahmanita AzizaNo ratings yet
- Special Topic: Erika N. Davis, B.S., and Kevin C. Chung, M.D., M.SDocument6 pagesSpecial Topic: Erika N. Davis, B.S., and Kevin C. Chung, M.D., M.ScryystinaNo ratings yet
- Human Papilloma Virus Vaccine For Cervical Cancer PreventionDocument9 pagesHuman Papilloma Virus Vaccine For Cervical Cancer Preventionsayeef khanNo ratings yet
- Dermoscopy of Inflamed Seborrheic KeratosisDocument9 pagesDermoscopy of Inflamed Seborrheic KeratosisFreddy RojasNo ratings yet