Professional Documents
Culture Documents
Gastrointestinal Drugs
Uploaded by
Abby MataCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gastrointestinal Drugs
Uploaded by
Abby MataCopyright:
Available Formats
Drugs Affecting GI Function
1)
2)
3)
ACh release (Enteric NS) binds to M1 and M3 receptors
Gastrin release - CNS activation, GI wall distention, chemicals in food
Gastrin activates ECL Histamine release
-Histamine binds to H2 in parietal cells stimulate Gs protein adenylyl cyclase activated CAMP protein kinase
activation proton pump activation H+/K+/ATPase (resp. for exchange of K+ for H+) Acid production
4) Gastric mucosa acidified to pH<3 negative feedback Antral D cells release somatostatin - inhibits gastrin by binding
to ECL and G cell
PGE2 and PGI2 bind to EP3 receptors of parietal & non-parietal mucosal epithelial cells
*cytoprotective action
*stimulates gastric mucus secretion
Abigail Mata | Phar 141
Page 1
Drugs Affecting GI Function
Drugs used to treat Gastric Acidity, PUD and GERD
Physiology of Gastric Acid Secretion
Gastrin
G or
Cholecystoki
nin-B
(CCK-B or
CCK2)
Somatostatin
(SST)
ST2
HCl and pepsinogen: principal gastric secretory products
capable of inducing mucosal injury
Basal acid production (circadian rhythm)
*highest in the evening, lowest in the morning
Cholinergic input via vagus nerve
Histaminergic input from local gastric sources
Stimulated conditions
Cephalic phase: sight, smell, taste of food
-release of Ach (1 stimulant) from CNS
Gastric phase: food enters stomach distention of GI
walls gastrin release from G cells direct/indirect
promotion of secretion of digestive juices
*direct- parietal cells induced
Intestinal phase: nutrient assimilation; antral D cells in
gastric mucosa (somatostatin) inhibits gastric
secretion
Regulatory Mechanisms of Gastric Acid Secretion
Acetylcholine (neuronal): M3 receptors (basolateral
membrane of parietal cells)
Histamine (paracrine-neighboring): H2 receptors
-Enterochromaffin-like cells adjacent to parietal cells
has H2 receptors
Gastrin (endocrine) : CCK2 (cholecystokinin)or CCK-B/G
receptors
*Parts of stomach: cardiac, fundus, body, pylorus
Regulatory
Hormones
Acetylcholine
Histamine
Receptors
M3 on
basolateral
membrane
of parietal
cells
M1 on ECL
cells
H2 on
parietal cells
Abigail Mata | Phar 141
Description
Released from
postganglionic vagal fibers
Stimulates "cephalic"
phase of acid secretion
Indirectly affects parietal
cells by increasing release
of histamine from ECL cells
in the fundus of the
stomach and of gastrin
from G cells in the gastric
antrum
Released by ECL cells (in
close proximity to parietal
cells)
Acts as a paracrine
mediator by diffusion
Most potent inducer of
acid secretion: indirectly by
inducing release of
histamine by ECL cells
Produced by antral G cells
Stimulated by CNS
activation, local distention,
& chemical components
of gastric contents
Produced by antral D cells
Inhibits gastric acid
secretion
Stimulated by
acidification of gastric
luminal pH to <3
Suppresses gastrin
release
by negative feedback
Gastric Defenses Against Acid
LES (lower
esophageal sphincter)
Secretion of mucus
layer* stimulated by PG
E2and I2
-Prevents acid reflux
-1 esophageal defense from
gastric acid
-Soluble when secreted but
quickly forms insoluble gel
protecting gastric mucosa
-Slow ion diffusion
-Protects from macromolecules
such as pepsin
-Neutralizes HCl
Secretion of
bicarbonate ions* by
superficial
gastric epithelial cells
*there should be adequate blood flow
-high metabolic demand and O2 requirement of gastric
mucosa
Drug Classes
Proton pump inhibitors (PPIs)
H2 receptor antagonists or blockers
Agents that enhance mucosal defense
Prostaglandin analogs (Misoprostol)
Sucralfate
Antacids
Other acid suppressants and cytoprotectants
Page 2
Drugs Affecting GI Function
Proton Pump Inhibitors
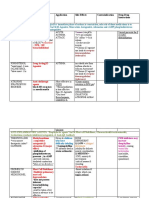
DRUG
OMEPRAZOLE
Prilosec
Losec
Hovizol
Omepron
Protonix
Risek
ESOMEPRAZOLE
Nexium
LANSOPRAZOLE
Prevacid
Prevacid
FDT
DEXLANSOPRAZOLE
Dexilant
RABEPRAZOLE
Pariet
Aciphex
PANTOPRAZOLE
Entericcoated
contained
inside gelatin
capsules
Entericcoated
granules as
powder for
suspension
Entericcoated
tablets
Powdered
drug
combined
with sodium
bicarbonate
IV
formulations
Protonix
Pantoloc
Omeprazole
Esomeprazol
e
Lansoprazole
Lansoprazole
Pantoprazole
Rabeprazole
Omeprazole
Omeprazole
Pantoprazole
Lansoprazole
PROPERTIES AND
INDICATIONS
Most potent
suppressors of
gastric acid
secretion
All have
equivalent
efficacy at
comparable
doses
Promote
healing of gastric
and duodenal
ulcers
Treat GERD,
including erosive
esophagitis
(either
complicated or
unresponsive to
tx w/
H2-receptor
antagonists)
Mainstay in the
treatment of
pathological
hypersecretory
conditions,
including the
ZollingerEllison syndrome
(tumors in
pancreas or SI
gastrinoma)
PHARMACOLOGIC
EFFECT/MOA
Prodrugs that
require activation in
an acid
environment
Effective in acid
suppression
regardless of other
stimulating factors
(targets final step)
*80-95% diminished
daily gastric acid
secretion
SULFENAMIDE
-active metabolite
-targets secretory
canaliculi inside
parietal cells
-site of
accumulation of
prodrug (cannot
escape cell)
-binds to SH groups
of Cys of protein
pump (covalent)
inactivate PP
*irreversible
inhibition causes
prolonged action
bec. it takes time
before new PP are
synthesized
PHARMACOKINETICS
SIDE EFFECTS/CI/DI
Should be given ~30
to 60 minutes before
breakfast or the
largest meal of the
day
Nausea, diarrhea,
headache, GI
disturbance, bone
fractures (increased
w/ long-term use:
hip, wrist, spine)
Decreased
effectiveness of
clopidogrel with
omeprazole
Low vitamin B12
levels
*Vit B12 + intrinsic
factor complex
requires acid pH for
absorption
Small intestine:
rapidly absorbed,
highly protein
bound, and
extensively
metabolized by
hepatic
CYP2C19 and CYP3A4
Maximal
suppression of acid
secretion requires
several doses of PPIs
-not all PP are
simultaneously
activated
Incomplete
absorption of CaCO3
products
*alternative: Ca
citrate
Provide a prolonged
(up to 24-to 48-hour)
suppression of acid
secretion, despite the
much shorter plasma
half-lives (0.5 to 2
hours) of
parent compounds
FDA approved
for reducing risk
of duodenal ulcer
recurrence
associated with
H. pylori
infections
( D cells low
somatostatinacid)
Lansoprazole:
FDA approved for
treatment and
prevention of
recurrence of
Abigail Mata | Phar 141
Page 3
Drugs Affecting GI Function
NSAID-associated
gastric
ulcers in patients
who continue
NSAID use
H2-Receptor Antagonists
CIMETIDINE
Tagamet
RANITIDINE
Zantac
FAMOTIDINE
Pepcid
H2 Bloc
NIZATIDINE
Axid
(no
longer
marketed
)
Promote
healing of gastric
and duodenal
ulcers
Treat
uncomplicated
GERD
Prevent
occurrence of
stress ulcers
*less potent that
PPIs (70%)
-usually given at
night
-PPI (morning)
Inhibit acid
production by
reversibly
competing with
histamine for
binding
selectively to H2receptors on the
basolateral
membrane of
parietal cells, BVs,
and other sites
Predominantly
inhibit basal acid
secretion,
which accounts for
their efficacy in
suppressing
nocturnal acid
secretion
Rapidly absorbed
after oral
administration
Peak serum
concentrations within
1 to 3 hours
Absorption may be
enhanced by food or
decreased by antacids
Only small % is
protein-bound
Diarrhea,
headache,
drowsiness, fatigue,
muscular pain, and
constipation
Confusion,
delirium,
hallucinations,
slurred
speech, and
headaches
Cimetidine
Short serum half-life;
inhibits CYP450
(enzyme inhibitor)
resp for many side
effects
Cimetidine (longterm, high doses):
Women:
galactorrhea
-inhibits CYP
enzymes that
hydroxylates
estradiol)
Men: gynecomastia,
reduced sperm
count, and
impotence (due to
reduction of
testosterone binding
to androgen
receptor)
Ranitidine
Longer-acting and 510x more potent vs.
cimetidine
Famotidine
20-50x more potent
vs. cimetidine, 3-20x
vs.
ranitidine
Nizatidine
Similar potency to
ranitidine; eliminated
principally by kidneys
(bioavailability ~100%)
Agents that Enhance Mucosal Defense:
Prostaglandin Analogs
Prostaglandin E2 (PGE2) and prostacyclin (PGI2)
Major PGs synthesized by the gastric mucosa
Bind to EP3 receptor on parietal cells and stimulate the Gi pathway decreased intracellular cAMP and gastric acid secretion
PGE2: cytoprotective effects (stimulation of mucin and bicarbonate secretion; increased mucosal blood flow)
DRUG
PROPERTIES AND
PHARMACOLOGIC
PHARMACOKINETICS
SIDE EFFECTS/CI/DI
INDICATIONS
EFFECT/MOA
MISOPROSTOL
Synthetic analog of PG
Degree of inhibition of Rapidly absorbed after Diarrhea, with or
Cytotec
E1
gastric acid secretion
oral administration
without abdominal
FDA approved to
is directly related to dose Rapidly and extensively pain and cramps
Abigail Mata | Phar 141
Page 4
Drugs Affecting GI Function
SUCRALFATE
Iselpin, Carafate
prevent NSAID-induced
mucosal injury
de-esterified to form
misoprostol acid
Complex of aluminum
hydroxide and sulfated
sucrose
Inhibits pepsinmediated hydrolysis of
mucosal proteins
Single dose inhibits
acid production within
30
minutes
Therapeutic effect
peaks at 60-90 minutes
and
lasts for up to 3 hours
Food and antacids
decrease the rate of
absorption
Free acid is excreted
mainly in the urine
Elimination half-life of
~20 to 40 minutes
Should be taken on an
empty stomach 1 hour
before meals
Epidermal growth
factor (EGF)
pH <4: undergoes
extensive cross-linking
to produce a viscous,
sticky polymer that
adheres to epithelial
cells and ulcer craters for
up to 6 hours
after a single dose
Effectively heals
duodenal ulcers and is
used in long-term
maintenance therapy to
prevent their recurrence
BISMUTH
SUBSALICYLATE
Pepto-Bismol
Antimicrobial in H.pylori
associated PUD
ANTACIDS
Acid-neutralizing ability
depends on capacity to
neutralize gastric HCl and
on whether the
stomach is full or empty
Sodium
Very water-soluble
Abigail Mata | Phar 141
(30%)
*dose-related,
begins w/in first 2
wks after initiation
of therapy & often
resolves
spontaneously w/in a
week
CI: IBD-misoprostol
exacerbates IBD
-Pregnancy: uterine
contractility
-taken 4x daily: limits
its use
AE: constipation
(2%)
CI: renal failure
with risk for Al
overload
DI: taken at least 2
h after
administration of
phenytoin, digoxin,
cimetidine,
ketoconazole and
fluoroquinolones
(sucralfate
decreases
absorption of these
drugs)
Additional
cytoprotective effects
(stimulation of local
production of PGs and
EGF)
Effectively heal peptic
ulcers by:
Inhibiting pepsin
activity
Increasing mucus
secretion
Interacting with
glycoproteins in necrotic
mucosal tissue and
protect the ulcer crater
Weak bases that react
with gastric acid to
form water and a salt to
diminish gastric
acidity
Also reduce pepsin
activity
Rapidly absorbed from
Alkali and sodium
Page 5
Drugs Affecting GI Function
bicarbonate
the
stomach
loads may pose a risk
for patients with
cardiac or renal
failure
Systemic alkalosis,
belching and
flatulence
(NaHCO3)
Calcium carbonate
Tums, Calsan,
Calci-Aid
Also used as calcium
supplements for
treatment
of osteoporosis
Calcium may induce
rebound acid secretion,
necessitating more
frequent administration
Combination of
Mg2+ and Al3+
hydroxides
Magaldrate,
Maalox
Symptomatic relief of
peptic ulcer disease and
GERD
Promote healing of
duodenal ulcers
Used as last-line therapy
for acute gastric ulcers
Magaldrate:
hydroxymagnesium
aluminate complex
converted rapidly in
gastric acid to
Mg(OH)2 and Al(OH)3
Simethicone
Disflatyl
+ CaCO3+ Vit D
(Esvicalforte)
+ Al and Mg
hydroxides
(Mylanta, Maalox
plus, Kremil-S)
-Provides a relatively
balanced and sustained
neutralizing capacity
Surfactant added in
antacid preparations that
may decrease foaming
and hence esophageal
reflux
-Poorly absorbed
(sustained antacid
effect)
-Mg (fast acting)
-Al (slow acting)
Na content for
hypertensive or HF
patients
Release of CO2
from bicarbonateand carbonatecontaining antacids
can cause belching,
nausea, abdominal
distention, and
flatulence
Constipation (Al
hydroxide)
Diarrhea (Mg
hydroxide)
Hypophosphatemia
(Al-containing)
Accumulation of
cations in renal
insufficiency
Antimicrobial Agents
Optimal therapy for patients with PUD (both duodenal and gastric ulcers) who are infected with Helicobacter pylori
TRIPLE THERAPY
PPI + Metronidazole/Amoxicillin +
Clarithromycin
QUADRUPLE THERAPY
Bismuth Subsalicylate +
Metronidazole + Tetracycline + PPI
Other Acid Suppressants and Cytoprotectants
DRUG
M1 Muscarinic
Receptor Antagonists
PIRENZEPINE
Abigail Mata | Phar 141
PROPERTIES AND INDICATIONS
-40-50% suppression
PHARMACOLOGIC EFFECT/MOA
SIDE EFFECTS/CI/DI
-significant undesirable
anticholinergic effect
-risk of blood disorders
-poor efficacy
Page 6
Drugs Affecting GI Function
TELENZEPINE
REBAMIPIDE Mucosta
Used for ulcer therapy (100mg)
ECABET Gastrom
also used for ulcer therapy in
Japan
Derivative of glycyrrhizic acid
found in licorice root
-Used for ulcer therapy in Europe
CARBENOXOLONE
Appears to exert a
cytoprotective effect both by
increasing PG generation in
gastric mucosa and by
scavenging reactive oxygen
species
Appears to increase the
formation of PGE2and PGI2
Unclear mechanism; may alter
the composition and
quantity of mucin
Hypokalemia and
hypertension due to
excessive mineralocorticoid
receptor activation
-Inhibits type I isozyme of 11-B
hydroxysteroid dehydrogenase
protects mineralocorticoid
receptor activation by cortisol in
the distal nephron
DRUGS USED FOR BOWEL MOTILITY DISORDERS
Drug classes:
Prokinetic agents and antiemetics
Laxatives
Antidiarrheals
Dopamine in GIT
Serotonin (5-HT)
Present in significant amounts in the GIT
Inhibitory effects on motility: reduction of LES and
intragastric pressures
Mediated by D2-dopaminergicreceptors
Result from suppression of Ach release from myenteric
motor neurons
>90% of total 5-HT in the body exists in GIT
Produced by ECL cells and rapidly released in response to
chemical and mechanical stimulation
Triggers the peristaltic reflex
5-HT1stimulation of the gastric fundus release
of nitric oxide and reduces smooth muscle tone
5-HT4stimulation of excitatory motor neurons enhanced Ach
release at the NMJ
5-HT3and 5-HT4receptors facilitate interneuronal signaling
Prokinetic Agents and Antiemetics
Medications that enhance coordinated GI motility and transit of material in the GI tract
Appear to enhance the release of excitatory neurotransmitter at the nerve-muscle junction without interfering with the
normal physiological pattern and rhythm of motility
2 TYPES
5-HT3 RECEPTOR BLOCKERS
DOPAMINE RECEPTOR ANTAGONISTS
Ondansetron (Zofran); Granisetron (Kytril); Palonosetron (Aloxi);
Metoclopramide, Domperidone, Phenothiazines,
Butyrophenones
Dolasetron(Anzemet)
Prokinetic Agents and Antiemetics
Substituted benzamides
Derivatives of PABA
Structurally related to procainamide
Additional advantage of relieving nausea and vomiting by antagonism of dopamine receptors in CTZ (high brain center for
vomiting)
Abigail Mata | Phar 141
Page 7
Drugs Affecting GI Function
DRUG
I. METOCLOPRAMIDE
Reglan, Plasil
Domperidone
Phenothiazines
PROPERTIES AND
INDICATIONS
Ameliorate nausea and
vomiting that often
accompany GI
dysmotility syndromes
Improve gastric
emptying in
symptomatic patients
with gastroparesis
(paralysis of GIT)
IV: adjunctive measure
in medical or
diagnostic procedures
(e.g., intestinal
intubation or contrast
radiography of the GIT)
Treatment of
chemotherapy-induced
emesis (as well as
prophylaxis of
anticipatory vomiting
CTZ)
OFF-LABEL USE:
Treatment of persistent
hiccups
II. DOMPERIDONE
Motilium
PHARMACOLOGIC
EFFECT/MOA
5-HT4-receptor agonism,
vagal and central 5HT3-antagonism, and
possible sensitization of
muscarinic receptors on
smooth muscle
Increases LES tone and
stimulates antral and
small intestinal
contractions
PHARMACOKINETICS
SIDE EFFECTS/CI/DI
Extrapyramidal
effects
Dystonias
(uncoordinated
movement) and
parkinsonian-like
symptoms (TRAP
tremor, rigidity,
akinesia, postural
instability)
Tardive dyskinesia
(slow abnormal
movement; may be
irreversible)
Galactorrhea
*confined effect in upper
digestive tract; no colonic
effect
Treatment:
Anticholinergics
Antihistamines
Predominantly
antagonizes the dopamine
D2 receptor without major
involvement of other
Receptors
Does not readily cross
BBB to cause
extrapyramidal side
effects
No significant effects on
lower GI motility
III. PHENOTHIAZINES
Prochlorperazine
Comprazine
IV.
BUTYROPHENONES
Droperidol Inapsine
Haloperidol Haldol
Serenace
Treatment of
chemotherapy-induced
emesis (i.e.,
low or moderately
emetogenic
chemotherapeutic
agents
Moderately effective
antiemetics
Increasing dose
improves antiemetic
activity
Hypotension,
restlessness, EPS,
sedation
Droperidol: used for
sedation in endoscopy
and surgery (+ opiates or
BZDs); cause QT
prolongation
5-HT3 Receptor Blockers
DRUG
ONDANSETRON
Zofran
Abigail Mata | Phar 141
PROPERTIES AND
INDICATIONS
PHARMACOLOGIC
EFFECT/MOA
Selectively block 5HT3 receptors in the
PHARMACOKINETICS/DOSING
-Can be administered as a
single dose prior to
SIDE EFFECTS/CI/DI
Headache as
common SE
Page 8
Drugs Affecting GI Function
visceral vagal afferent
fibers and CTZ in the
brain
GRANISETRON
Kytril
PALONOSETRON
Aloxi
chemotherapy (IV or PO);
efficacious against all grades
of emetogenic therapy
- Longer duration of action
DOLASETRON
Anzemet
Substance P/neurokinin-1 Receptor Blocker
DRUG
APREPITANT
Emend
PROPERTIES AND INDICATIONS
Only indicated for highly or
moderately emetogenic
chemotherapy regimens
PHARMACOKINETICS/DOSING
PO administration with
dexamethasone and
palonosetron
SIDE EFFECTS/CI/DI
Constipation and fatigue
as major SEs
LAXATIVES
Commonly used for constipation to accelerate the movement of food through the GIT
May cause electrolyte imbalances when used chronically
Increase potential for loss of pharmacologic activity of poorly absorbed, delayed-acting, and ER oral drugs by accelerating
intestinal transit time
All except lubiprostone have risk of dependency for the user
IRRITANTS and STIMULANTS
DRUG
Senna
PROPERTIES AND INDICATIONS
Active ingredient is a group of
sennosides
(anthraquinone glycosides)
Bisacodyl
+ docusate-containing stool
softener: useful in
treating opioid-induced constipation
Potent stimulant of the colon
available as
suppositories and enteric-coated
tablets
Castor Oil
Abortifacient
Hydrophilic colloids from
indigestible parts of fruits and
vegetables
Magnesium
citrate
Magnesium
hydroxide
Sodium
phosphate
Electrolyte solutions containing
PEG: used as
colonic lavage solutions to prepare
the gut for
radiologic or endoscopic procedures
PHARMACOLOGIC EFFECT/MOA
Causes evacuation of the bowels
within 8 to 10 hours
Causes water and electrolyte
secretion into the bowel
Acts directly on nerve fibers in the
colonic mucosa
Broken down in the small intestine
to
ricinoleic acid (very irritating to the
stomach and promptly increases
peristalsis)
Form gels in the large intestine,
causing water
retention and intestinal distension,
thereby
increasing peristaltic activity
Nonabsorbable salts that hold
water in the
intestine by osmosis, causing bowel
distention which increases intestinal
activity and
produces defecation in a few hours
SIDE EFFECTS/CI/DI
Abdominal cramps and
potential for atonic colon
with prolonged use
Food interaction: basic
food, milk
Causes GI irritation
CI in pregnancy
Used cautiously in
immobile patients
-potential to cause intestinal
obstruction
*less abdominal cramps and gas
Abigail Mata | Phar 141
Page 9
Drugs Affecting GI Function
Lactulose
Duphalac
Semi-synthetic disaccharide sugar
that cannot be hydrolyzed by
intestinal enzymes
Docusate
sodium
Often used for prophylaxis rather
than acute treatment
Oral doses are degraded in the
colon by colonic bacteria into lactic,
formic, and acetic acids increases
osmotic pressure fluid
accumulation, colon distention, soft
stools, and defecation
Surface-active agents that become
emulsified with stool, producing
softer feces and ease of passage
Not to be taken
concomitantly with mineral
oil
Docusate
calcium
Docusate
potassium
Lubricant Laxatives
Mineral oil
Glycerin
suppositories
Mineral oil to be taken orally in an
upright position to prevent aspiration
and lipid & lipoid pneumonia
Act by facilitating the passage of
hard stools
Chloride Channel Activators
Lubiprostone
Used in the treatment of chronic
constipation
Activates chloride channels to
increase fluid secretion in the
intestinal lumen
Nausea as common SE
Metabolism occurs quickly in the
stomach and jejunum
ANTIDIARRHEALS
Causes of diarrhea
Increased osmotic load within the intestine, resulting in retention of water within the lumen
Excessive secretion of electrolytes and water into the intestinal lumen
Exudation of protein and fluid from the mucosa
Altered intestinal motility resulting in rapid transit and decreased fluid absorption
DRUG
PROPERTIES AND INDICATIONS
PHARMACOLOGIC EFFECT/MOA
Bulk-forming and Hydroscopic Agents
Methylcellulose
Hydrophilic and poorly
May work as gels to modify stool texture and viscosity and to
Citrucel
fermentable colloids or polymers produce a perception of decreased stool fluidity
that absorb water and increase
Adsorb intestinal toxins or microorganisms
Aluminum hydroxide stool
and/or by coating or protecting the intestinal mucosa
Alternagel
Bulk
Bile Acid Sequestrants
Cholestyramine
Colestipol
Colesevalam
Crystal complex consisting of trivalent
Low pH of the stomach: drug reacts with HCl to
Bismuth
bismuth and salicylate suspended in a mixture form bismuth oxychloride and salicylic acid
subsalicylate
of
Pepto-Bismol
magnesium aluminum silicate clay
Antisecretory, anti-inflammatory, and
antimicrobial effects
Prevention and treatment of traveler's
diarrhea;
other forms of episodic diarrhea and acute
gastroenteritis
Antimotility and Antisecretory Agents
Abigail Mata | Phar 141
Page 10
Drugs Affecting GI Function
Opioids
Loperamide
Diphenoxylate and difenoxin
Octreotide and somatostatin
Opioids
Loperamide
Lormide
Lomotil
Imodium
An orally active
antidiarrheal agent with receptor activity agent and
penetrates the CNS poorly
Effective against
traveler's diarrhea, used
either alone or in
combination with
antimicrobial agents
(trimethoprim,
cotrimoxazole,or a
fluoroquinolone)
Effects on intestinal
motility (receptors),
intestinal secretion
(dreceptors), or
absorption ( and d
receptors)
Increases small
intestinal and mouth-tocecum transit times
Increases anal sphincter
tone
Usual adult dose: 4 mg
initially followed by 2 mg
after each subsequent
loose stool, up to 16 mg
per day
40 to 50 times more
potent than morphine as
an antidiarrheal
Must be discontinued if
no clinical improvement in
acute diarrhea within 48 h
Overdosagecan
result in CNS
depression
(especially in
children) and
paralytic ileus less
movement of
intestines
Used as adjunct
treatment in almost all
forms of chronic diarrheal
disease
Diphenoxylate
Octreotide &
Somatostatin
Lacks significant abuse
potential
Related structurally to
meperidine; more
potent than morphine as
antidiarrheal
Rapidly deesterified to
difenoxin
Both can produce CNS
effects when used in
higher doses (40 to 60
mg per day)
*see previous handouts
(hormones)
Abigail Mata | Phar 141
Page 11
You might also like
- Drugs Used in Gastrointestinal Diseases FinalDocument30 pagesDrugs Used in Gastrointestinal Diseases FinalFaridah Yuwono 28No ratings yet
- Pharmacology ReviewDocument172 pagesPharmacology ReviewJan Patrick Arrieta100% (1)
- Emergency Contraception and Emergency Contraceptive Pills (ECPs)Document39 pagesEmergency Contraception and Emergency Contraceptive Pills (ECPs)cafemed100% (1)
- Anti Inflammatory DrugsDocument82 pagesAnti Inflammatory DrugsShardendu MishraNo ratings yet
- Pharmacology2 (Drug Receptors & Pharmacodynamics)Document58 pagesPharmacology2 (Drug Receptors & Pharmacodynamics)Durge Raj Ghalan100% (2)
- Pharmacology of The GIT System: CIC Ragasa, RN-MDDocument70 pagesPharmacology of The GIT System: CIC Ragasa, RN-MDCarmencita Ileen Ragasa - AhmedNo ratings yet
- Cardiovascular Agents ReviewerDocument18 pagesCardiovascular Agents ReviewerJoycel CeñidozaNo ratings yet
- Chapter 13 PharmacologyDocument35 pagesChapter 13 PharmacologyEdelrose LapitanNo ratings yet
- Pharma CNS DRUGS Part 1Document13 pagesPharma CNS DRUGS Part 1reference booksNo ratings yet
- NCM 107 1.2Document2 pagesNCM 107 1.2Clint Mikael EulatrizNo ratings yet
- Anti-Infectives and AntibioticsDocument38 pagesAnti-Infectives and AntibioticsKarel Lu0% (1)
- Cardiotonic Medications: Drugs Used To For Patients Experiencing Heart FailureDocument28 pagesCardiotonic Medications: Drugs Used To For Patients Experiencing Heart FailureMoxie MacadoNo ratings yet
- PHRM 246: MR Thabiso Tlaila Department of Pharmacology Discipline of Pharmaceutical Sciences University of Kwazulu-NatalDocument38 pagesPHRM 246: MR Thabiso Tlaila Department of Pharmacology Discipline of Pharmaceutical Sciences University of Kwazulu-NatalSindile MchunuNo ratings yet
- Drugs For Immune SystemDocument75 pagesDrugs For Immune SystemDhonat FlashNo ratings yet
- GIT DrugsDocument180 pagesGIT DrugsMaria Linevel Balderamos Dalida100% (1)
- Anti-Infective Pharmacology ReviewerDocument5 pagesAnti-Infective Pharmacology ReviewerArianne Pearl PrimeroNo ratings yet
- Pharmacology Mock Exam MCQDocument8 pagesPharmacology Mock Exam MCQanaeshklNo ratings yet
- Factors Affecting Drug ActionDocument3 pagesFactors Affecting Drug ActionHempriya Tomar0% (1)
- Introduction To CNS PharmacologyDocument9 pagesIntroduction To CNS PharmacologyAbraham Daniel Campo Cruz100% (1)
- Nutrition and Malnutrition Resource UnitDocument22 pagesNutrition and Malnutrition Resource UnitMitch GatdulaNo ratings yet
- Drugs acting on the Cardiovascular SystemDocument18 pagesDrugs acting on the Cardiovascular SystemIbrahem AlNo ratings yet
- GI Pharmacology OverviewDocument24 pagesGI Pharmacology OverviewjenniferluzonNo ratings yet
- Drugs For GI DisordersDocument5 pagesDrugs For GI DisordersAalap ShahNo ratings yet
- Pharmacology: By: Nerissa Cabañero Laiza PinedaDocument121 pagesPharmacology: By: Nerissa Cabañero Laiza PinedaJacq CalaycayNo ratings yet
- Module 1.1 Presentation (B2)Document15 pagesModule 1.1 Presentation (B2)Jan Lianne BernalesNo ratings yet
- Appendix A: National Unified Health Research Agenda A. DiagnosticsDocument10 pagesAppendix A: National Unified Health Research Agenda A. DiagnosticsKit ChampNo ratings yet
- Chapter 09 AntibioticsDocument77 pagesChapter 09 AntibioticsAngela Joy AmparadoNo ratings yet
- Pharmacotherapy of Diabetes MellitusDocument8 pagesPharmacotherapy of Diabetes MellitusSheryl Layne Lao-SebrioNo ratings yet
- Ursing Care of Client With CancerDocument51 pagesUrsing Care of Client With CancerJimmelyn PalosNo ratings yet
- Autonomic Nervous System: Parasympathetic and Sympathetic DivisionsDocument107 pagesAutonomic Nervous System: Parasympathetic and Sympathetic DivisionsMaria Mercedes LeivaNo ratings yet
- 1.introduction To PharmacologyDocument127 pages1.introduction To PharmacologyblacknurseNo ratings yet
- Anti InfectivesDocument126 pagesAnti Infectiveseunice lachicaNo ratings yet
- Introduction to Key Concepts in PharmacologyDocument30 pagesIntroduction to Key Concepts in PharmacologyCandy crush100% (1)
- Sexually Transmitted InfectionsDocument34 pagesSexually Transmitted InfectionsMariana Creciun100% (1)
- Pharmacology of Gastrointestinal SystemDocument4 pagesPharmacology of Gastrointestinal SystemZaira KimNo ratings yet
- Drug Name Mechanism Application Side Effects Contraindication Drug-Drug InteractionsDocument3 pagesDrug Name Mechanism Application Side Effects Contraindication Drug-Drug Interactionsazhar hussinNo ratings yet
- Gastrointestinal DrugsDocument2 pagesGastrointestinal DrugsJannah Mikhaela Alibay VillarinNo ratings yet
- NCM 106.2 3Document3 pagesNCM 106.2 3Marielle ChuaNo ratings yet
- Drug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityDocument2 pagesDrug Study: Name Mechanism of Action Indication/Contraindication Side Effects Nursing ResponsibilityJoshua DavantesNo ratings yet
- Huntington DiseaseDocument10 pagesHuntington Diseaseapi-498055661No ratings yet
- Albacio Eddiva Dapli-An Magwilang MaspilDocument138 pagesAlbacio Eddiva Dapli-An Magwilang MaspilJustineNo ratings yet
- Mental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessDocument41 pagesMental Health Nursing II NURS 2310: Unit 1 Basic Concepts of Mental Health and Mental IllnessRocky Domingo LazaroNo ratings yet
- NotesDocument14 pagesNotesJan Rey L. TejereroNo ratings yet
- Autonomic Nervous System DrugsDocument111 pagesAutonomic Nervous System DrugsCres Padua QuinzonNo ratings yet
- Pharma ExamDocument7 pagesPharma ExamGeno Adrian T PampangaNo ratings yet
- Case HistoryDocument8 pagesCase HistoryjabeensarwarNo ratings yet
- Antiviral AgentsDocument14 pagesAntiviral AgentsKate MendozaNo ratings yet
- Pharmacology Section on Antibiotics, Antivirals and AntifungalsDocument5 pagesPharmacology Section on Antibiotics, Antivirals and AntifungalsPathalee ThalpavilaNo ratings yet
- Drugs Acting On Cardiovascular SystemDocument7 pagesDrugs Acting On Cardiovascular SystemAnwar Ul HaqueNo ratings yet
- TB in ChildrenDocument26 pagesTB in ChildrenReagan PatriarcaNo ratings yet
- Anti InflammatoryDocument41 pagesAnti InflammatoryKakai Ablanque LopozNo ratings yet
- Anti-TB Drugs: Mechanisms & Treatment PhasesDocument35 pagesAnti-TB Drugs: Mechanisms & Treatment PhasesZijieNo ratings yet
- Health Education PlanDocument10 pagesHealth Education PlanJulienne Sanchez-SalazarNo ratings yet
- Medical AbbreviationsDocument5 pagesMedical AbbreviationsReuelHengNo ratings yet
- Adult Nursing Immune FunctionDocument103 pagesAdult Nursing Immune FunctionEstherThompsonNo ratings yet
- Drugs Affecting The Gastrointestinal SystemDocument4 pagesDrugs Affecting The Gastrointestinal SystemJerica Jaz F. Vergara100% (1)
- TB TreatmentDocument58 pagesTB TreatmentNdayisaba CorneilleNo ratings yet
- Central Nervous System Pharmacology: Elly Nurus SakinahDocument64 pagesCentral Nervous System Pharmacology: Elly Nurus Sakinahkareem92No ratings yet
- Anti Emetics 141109072529 Conversion Gate02Document23 pagesAnti Emetics 141109072529 Conversion Gate02sanoozarmNo ratings yet
- Autonomic Nervous System: Skin / Gut Skeletal MuscleDocument7 pagesAutonomic Nervous System: Skin / Gut Skeletal MuscleAbby MataNo ratings yet
- USP Limit Test For LeadDocument2 pagesUSP Limit Test For LeadAbby MataNo ratings yet
- Sensations and Sensory Pathways General Senses Test Procedure Normal Result Abnormal Result Clinical InterpretationDocument5 pagesSensations and Sensory Pathways General Senses Test Procedure Normal Result Abnormal Result Clinical InterpretationAbby MataNo ratings yet
- Hypertension and Anti-Hypertensive DrugsDocument12 pagesHypertension and Anti-Hypertensive DrugsAbby Mata100% (1)
- Cholelithiasis AnaphysioDocument12 pagesCholelithiasis AnaphysioAbby MataNo ratings yet
- REDOXDocument27 pagesREDOXAbby MataNo ratings yet
- Carbohydrate identification testsDocument3 pagesCarbohydrate identification testsAbby Mata100% (1)
- Xanax Information-Sheet 2018-002Document2 pagesXanax Information-Sheet 2018-002Alexa HuffmanNo ratings yet
- Administering Subcutaneous InjectionDocument6 pagesAdministering Subcutaneous InjectionAnggrian Clara DewiNo ratings yet
- Analysis of NATCO Vs BAYER Pharma Case by Ankit SinghDocument18 pagesAnalysis of NATCO Vs BAYER Pharma Case by Ankit SinghAnkit Singh50% (4)
- Swcavilt 11103Document3 pagesSwcavilt 11103Sadik AmbaniNo ratings yet
- National Drug Policy 1995Document13 pagesNational Drug Policy 1995Madhu Sudhan PandeyaNo ratings yet
- Tylenol for mild to moderate painDocument2 pagesTylenol for mild to moderate painKristi WrayNo ratings yet
- Ch1 Intro To DrugsDocument23 pagesCh1 Intro To DrugsLalita SutcharitkulNo ratings yet
- Pharmaceutical Formulations III Pharm DQuestion BankDocument7 pagesPharmaceutical Formulations III Pharm DQuestion BankAnanda VijayasarathyNo ratings yet
- Formularium OBAT KlinikDocument13 pagesFormularium OBAT KlinikSathyani ParmitaNo ratings yet
- Abott LaboratoriesDocument41 pagesAbott Laboratoriesnishant_gupta_22No ratings yet
- Usp 2008 P 2 Supplement 3Document166 pagesUsp 2008 P 2 Supplement 3EstiPramestiningtyas100% (1)
- Asthma MedicationDocument6 pagesAsthma Medicationmomina arshidNo ratings yet
- Acyclovir antiviral drug overviewDocument3 pagesAcyclovir antiviral drug overviewLisaNo ratings yet
- LEAM ProtocolDocument6 pagesLEAM ProtocolShaza ElkourashyNo ratings yet
- Acetaminophen ToxicityDocument14 pagesAcetaminophen ToxicityEdel CarlosNo ratings yet
- Do Not CrushDocument16 pagesDo Not CrushDouglas Greg CookNo ratings yet
- Entire Pharm ClassDocument173 pagesEntire Pharm ClassnancyNo ratings yet
- Format Inject Stock Obat FOI 2017Document32 pagesFormat Inject Stock Obat FOI 2017Rani HadinataNo ratings yet
- 07 26 17Document24 pages07 26 17WoodsNo ratings yet
- Clinical PharmacyDocument38 pagesClinical PharmacyBalakrishna Thalamanchi100% (1)
- Omeprazole (Losec, Prilosec)Document1 pageOmeprazole (Losec, Prilosec)Jocelyn RiveraNo ratings yet
- PONV 30 Mar 2010 AmitDocument46 pagesPONV 30 Mar 2010 AmitAmit KochetaNo ratings yet
- What Are Drug Utilization Reviews (Dur) : Why Durs Are ImportantDocument3 pagesWhat Are Drug Utilization Reviews (Dur) : Why Durs Are ImportantthegroovyNo ratings yet
- Vesicular Palmoplantar EczemaDocument16 pagesVesicular Palmoplantar EczemakcipitNo ratings yet
- Normal Values HR RR BPDocument28 pagesNormal Values HR RR BPKthrine CrronNo ratings yet
- Report Regarding DepressionDocument18 pagesReport Regarding Depressiontech masterNo ratings yet
- Caffeine Piece in WiredDocument4 pagesCaffeine Piece in Wiredthird3planetNo ratings yet
- Drugs Acting On The Endocrine SystemDocument90 pagesDrugs Acting On The Endocrine SystemKATHERINE GRACE JOSENo ratings yet
- Antiepileptic DrugsDocument39 pagesAntiepileptic Drugsking_goldNo ratings yet
- Package InsertDocument2 pagesPackage InsertcherokeeNo ratings yet