Professional Documents
Culture Documents
Contact Details Name: Hospital Telephone:: Treatment Is Urgent. Do Not Delay
Uploaded by
Caterina PrepelitaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Contact Details Name: Hospital Telephone:: Treatment Is Urgent. Do Not Delay
Uploaded by
Caterina PrepelitaCopyright:
Available Formats
Contact Details Name:
Hospital
Telephone:
This protocol has 4 pages
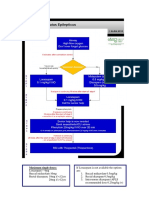
GLUTARIC ACIDURIA type 1 -ACUTE DECOMPENSATION
(Glutaryl CoA dehydrogenase deficiency, GCDH deficiency)
(standard version)
Please read carefully. Meticulous treatment is very important as there is a high risk
of neurological complications.
TREATMENT IS URGENT. DO NOT DELAY.
If the instructions do not make sense or a problem is not addressed you must discuss
your concerns with the consultant on call.
1. Background
Glutaric aciduria is an inherited disorder of the breakdown of certain amino acids, notably lysine.
Any metabolic stress can lead to serious illness, with encephalopathy - a reduced level of
consciousness and other neurological abnormalities. Following these episodes, patients often
have severe permanent neurological disability, particularly a movement disorder. However with
early aggressive treatment neurological complications can b e prevented. The damage results
from the accumulation of glutaric acid and other toxic metabolites. Patients under 6 years of age
are at most risk of neurological damage so treatment of the children must be very careful.
Treatment aims to minimise the accumulation of toxic metabolites by preventing protein
breakdown and to promote their excretion by the use of carnitine.
Decompensation is often triggered by metabolic stress such as any febrile illness, particularly
diarrhoea and vomiting, or fasting, but an obvious cause is not always apparent. The early signs
of decompensation may be subtle, such as minor changes in tone. Vomiting and diarrhoea are
common and should always be taken seriously. However, the signs may be difficult to assess
such as irritability or just not right. Always listen to parents carefully as they probably know
much more than you do.
2. Admission
Almost all patients who present to hospital will require admission. Only allow the child home if
you and the family are entirely happy and you have discussed the problems with the consultant
on call. The family must have a clear management plan and be prepared to return if the child does
not improve.
If there is any doubt at all, the child must be admitted, even if only necessary for a
short period of observation.
BIMDG 2008
BIMDG protocol Glutaric aciduria type 1 standard version
3. Initial plan and management in hospital
If the child is shocked or clearly very ill arrange for admission to ITU/High dependency unit.
If admitted to metabolic/general ward make a careful clinical assessment including blood
pressure and even if the patient does not appear encephalopathic enter a Glasgow coma score (for
details click here). This will help other staff to detect any deterioration, particularly around the
time of a change of shifts.
The following tests should be done:
BLOOD:
pH and gases
Urea and electrolytes
Glucose (laboratory and bedside strip test)
Full blood count
Blood spot acylcarnitines
Blood culture
URINE
ketones
4. Management
Treatment is urgent. Do not delay. Unless you are very confident and certain, treat with
intravenous fluids.
A. ENTERAL.
Enteral treatment should only be used occasionally and with caution.
The emergency regimen should be used. This may be given as regular drinks or through a nasogastric tube but if the patient is at risk of vomiting or is nauseated fluid should be given either
continuously or as small boluses more frequently. For more information about the emergency
oral management click here
Age (years)
0-1
1-2
2-6
6-10
>10
Glucose polymer concentration (g/100ml)*
10
15
20
20
25
Total daily volume**
150-200 ml/kg
100 ml/kg
1200-1500 ml
1500-2000 ml
2000 ml
* If necessary, seek help from your local dietitian. In an emergency a heaped 5 ml medicine spoon holds
approximately 7g of glucose polymer.
**For each drink the volume will generally be this figure divided by 12 In an emergency a heaped 5 ml
medicine spoon holds approximately 7g of glucose polymer.but if the patient is nauseated or refuses try frequent
smaller drinks or a continuous naso-gastric infusion.
Electrolytes should be added to the drinks if vomiting and/or diarrhoea is a problem using
standard rehydration mixtures following manufacturers instructions, but substituting glucose
polymer solution for water
.
BIMDG 2008
BIMDG protocol Glutaric aciduria type 1 standard version
Aminoacids: As soon as available, the lysine free aminoacid mixture should be added to the
glucose polymer drinks and initially given at the rate of 1g/kg/d. If this is not tolerated, the
quantity can be reduced to 0.5 g/kg/d but for as short a period as possible. Do not delay giving
drinks if the aminoacid mixture is not immediately available. There is now laboratory evidence
that arginine alone may be effective but at present its use should be part of a research project.
Fever. If the temperature is > 38.5 C (101 F), ibuprofen should be given.(10-15 mg/kg per
dose, 3-4 doses daily). Paracetamol is not recommended because of the potential for glutathione
depletion.
.
Medicines Carnitine should be given 200 mg/kg/24h in 4 divided doses.
B. INTRAVENOUS.
This route should be used in most circumstances.
Give Glucose 200 mg/kg at once (2 ml/kg of 10% glucose or 1ml/kg of 20% glucose)
over a few minutes.
Give normal saline 10 ml/kg as a bolus immediately after the glucose unless the
peripheral circulation is poor or the patient is frankly shocked, give 20 ml/kg normal
saline instead of the 10 ml/kg.. Repeat the saline bolus if the poor circulation persists as
for a shocked non-metabolic patient.
Continue with glucose 10% at 5 ml/kg/h until next solution ready. see below
Quickly calculate the deficit and maintenance and prepare the intravenous fluids
o Deficit: estimate from clinical signs if no recent weight available
o Maintenance: Formula for calculating daily maintenance fluid volume (BNF for
children) 100ml/kg for 1st 10kg then 50 ml/kg for next 10kg then 20ml/kg thereafter,
using calculated rehydrated weight. Deduct the fluid already given from the total for
the first 24 hours.
o Give 0.45% saline/10% glucose (for instructions to make this solution click here)..
Having calculated the deficit and the maintenance, give 1/3 of the total for 24 hours over
the next 6 hours and the remainder in 18 hours. If intravenous fluids are still needed,
continue with the same solution.
Recheck the electrolytes every 24 hours if still on IV fluids.
Aminoacids: If at all possible give the lysine free aminoacid mixture orally or via naso-gastric
tube, as drinks or as a continuous infusion. Initially it can be given at the rate of 1g/kg/d. If this is
not tolerated, the quantity can be reduced to 0.5 g/kg/d but for as short a period as possible. Do
not delay giving other treatment if the mixture is not immediately available
- Carnitine should be given intravenously - 200 mg/kg/24h given as a bolus of 100 mg/kg in 30
minutes and then a slow intravenous infusion of 4 mg/k/h.
- Potassium can be added, if appropriate, once urine flow is normal and the plasma potassium
concentration is known.
BIMDG 2008
BIMDG protocol Glutaric aciduria type 1 standard version
- Arginine. There is now laboratory evidence that arginine may be effective in reducing
neurological damage but at present its use should be part of a research project.
- Hyperglycaemia can be a problem. If the blood glucose exceeds the 8 mmol/l, start an insulin
infusion using the local diabetic protocol rather than reducing the glucose intake. Strict
supervision is essential.
Fever. If the temperature is > 38.5 C (101 oF), ibuprofen (10-15 mg/kg per dose, 3-4 doses
daily) or paracetamol (use standard doses) should be given
- Treat any infection
5. Progress:
Monitoring: Reassess after 4-6 hours or earlier if there is any deterioration or no improvement
Clinical assessment should include Glasgow coma score (for details click here) and blood
pressure.
Blood tests: Blood pH and gases
Glucose (laboratory): high values can occur due to insulin resistance
Urea & electrolytes
For intravenous fluids after 24 hours please refer to the previous section.
6. Re-introduction of enteral feeds: As many more calories can be given enterally safely, feeds
should be introduced as early as possible. It is usual to give soluble glucose polymer initially
10% and increase this both volume and concentration as tolerated. It is also customary to delay
the introduction of any protein or aminoacids but this will only prolong the period of catabolism
so early re-introduction is recommended. Aminoacids should be given and increased to 2g/kg/d.
If necessary, consult your local dietitian for more details.
7. Going Home: Only allow the child home if you and the family are entirely happy and you
have discussed the problems with the consultant on call. The family must have a clear
management plan and be prepared to return if the child deteriorates.
For further information please refer to:
Saudubray J-M, van den Berghe G, Walter JH. (editors) Inborn Metabolic Diseases. Diagnosis
and treatment. 5th Edition. Springer 2012
For further information you can refer to the guidelines in: METABNET - scroll down to the long
and shortened versions.
Last reviewed in May 2013
BIMDG 2008
You might also like
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Contact Details Name: Hospital Telephone:: This Protocol Has 4 PagesDocument4 pagesContact Details Name: Hospital Telephone:: This Protocol Has 4 PagesCaterina PrepelitaNo ratings yet
- Contact Details Name: Hospital Telephone:: Carnitine Transporter Deficiency (CTD) - Acute DecompensationDocument4 pagesContact Details Name: Hospital Telephone:: Carnitine Transporter Deficiency (CTD) - Acute DecompensationCaterina PrepelitaNo ratings yet
- Metabolic Disorders LONG CHAIN FAT OXIDATION DISORDERSDocument5 pagesMetabolic Disorders LONG CHAIN FAT OXIDATION DISORDERSMahmoud khedrNo ratings yet
- Contact Details Name: Hospital Telephone:: This Protocol Has 4 PagesDocument4 pagesContact Details Name: Hospital Telephone:: This Protocol Has 4 PagesCaterina PrepelitaNo ratings yet
- This Protocol Has 4 Pages: Acute DecompensationDocument4 pagesThis Protocol Has 4 Pages: Acute DecompensationCaterina PrepelitaNo ratings yet
- 100Document14 pages100Mohammed BISHRNo ratings yet
- Gds137 Slide Diabetes Melitus Type 1Document31 pagesGds137 Slide Diabetes Melitus Type 1viscabarca543No ratings yet
- Therapeutics Question (DKA) : Answer For Q1Document4 pagesTherapeutics Question (DKA) : Answer For Q1Daniel YongNo ratings yet
- Keto LogDocument7 pagesKeto LogKim Justin InfantadoNo ratings yet
- Noor Endocrinologybase. FINALDocument62 pagesNoor Endocrinologybase. FINALschool adressNo ratings yet
- Diabetes Management ATIDocument15 pagesDiabetes Management ATIJessica ChirinoNo ratings yet
- Diabetic Ketoacidosis (DKA) : BackgroundDocument9 pagesDiabetic Ketoacidosis (DKA) : Backgroundalyssa_flores_3No ratings yet
- Insulin Initiation PPT - PPTX 2Document53 pagesInsulin Initiation PPT - PPTX 2Meno Ali100% (1)
- Captopril Drug StudyDocument7 pagesCaptopril Drug StudyKimzie Joy Basco100% (1)
- Drug StudyDocument41 pagesDrug StudyCatherine PradoNo ratings yet
- Adult Hypoglycemia Management ProtocolDocument4 pagesAdult Hypoglycemia Management ProtocolNurul MazniNo ratings yet
- Sick Day Plan For Type 2 Diabetes - TemplateDocument4 pagesSick Day Plan For Type 2 Diabetes - Templatehernandez2812No ratings yet
- Metabolic Alkalosis CausesDocument15 pagesMetabolic Alkalosis CausesRajiv Kabad100% (1)
- Glycemic ManagementDocument39 pagesGlycemic ManagementZayar HmunNo ratings yet
- Drug StudyDocument16 pagesDrug StudyJhann0% (1)
- Lisinopril PDFDocument3 pagesLisinopril PDFHannaNo ratings yet
- Endocrine CreditDocument58 pagesEndocrine CreditGiridhar SolasaNo ratings yet
- Colestipol Hydrochloride Nursing ConsiderationsDocument3 pagesColestipol Hydrochloride Nursing ConsiderationsAbby AngNo ratings yet
- Total Parenteral NutritionDocument9 pagesTotal Parenteral NutritionsaravananNo ratings yet
- Note Exam 2Document7 pagesNote Exam 2Jamie BywaterNo ratings yet
- The Dose. Proceedings of The American College of Veterinary Internal Medicine Forum, May 2006 Kentucky, USADocument3 pagesThe Dose. Proceedings of The American College of Veterinary Internal Medicine Forum, May 2006 Kentucky, USADaniel KissNo ratings yet
- Guideline, Management of HypoglycemiaDocument5 pagesGuideline, Management of HypoglycemianellieauthorNo ratings yet
- Management of Paediatric Diabetic KetoacidosisDocument21 pagesManagement of Paediatric Diabetic KetoacidosisAsad M AminNo ratings yet
- Nursing Considerations for Patients with DiabetesDocument7 pagesNursing Considerations for Patients with Diabeteslanguha NgatiNo ratings yet
- Hypo Guidelines BrochureDocument2 pagesHypo Guidelines BrochureNellie RamosNo ratings yet
- Patient Conscious But Confused/disorientated or Aggressive and Able To SwallowDocument1 pagePatient Conscious But Confused/disorientated or Aggressive and Able To Swallowapi-192342497No ratings yet
- Medical Nutrition TherapyDocument4 pagesMedical Nutrition TherapycjgregoryNo ratings yet
- NCM 106 Learning Activities (Semis)Document12 pagesNCM 106 Learning Activities (Semis)Kimberly Abellar LatoNo ratings yet
- Joslin Diabetes Center Clinical GuideDocument16 pagesJoslin Diabetes Center Clinical GuideNikolaus TalloNo ratings yet
- Type II Diabetes: Case DefinitionDocument3 pagesType II Diabetes: Case DefinitionAnonymous kCDRRK0n9PNo ratings yet
- CH 39 Anaesthesia and Diabetes MellitusDocument6 pagesCH 39 Anaesthesia and Diabetes MellitusChristian LeepoNo ratings yet
- Age CPGDocument9 pagesAge CPGSLINo ratings yet
- DapaglifozinDocument21 pagesDapaglifozinChiyaanVikramNo ratings yet
- DiabetesMellitisChap09 SpecialPopulationsDocument12 pagesDiabetesMellitisChap09 SpecialPopulationsarmandoNo ratings yet
- ADS ADEA ANZCA NZSSD - DKA - SGLT2i - Alert - Ver July 2022Document3 pagesADS ADEA ANZCA NZSSD - DKA - SGLT2i - Alert - Ver July 2022tom.condon.02No ratings yet
- 47 TPNDocument7 pages47 TPNKhor Chin PooNo ratings yet
- Magnetic Resonance Centre: 1. DiagnosisDocument2 pagesMagnetic Resonance Centre: 1. Diagnosisbwalsh2006No ratings yet
- WHO 10-STEP MANAGEMENT OF SEVERE MALNUTRITIONDocument4 pagesWHO 10-STEP MANAGEMENT OF SEVERE MALNUTRITIONShely Karma Astuti33% (3)
- Inpatient Management of Diabetes MellitusDocument38 pagesInpatient Management of Diabetes Mellitusmsala76No ratings yet
- Informationfordoctors Revised April14Document2 pagesInformationfordoctors Revised April14Mesfin DerbewNo ratings yet
- CHAPTER 7 - Inpatient Management of Diabetes and HyperglycemiaDocument6 pagesCHAPTER 7 - Inpatient Management of Diabetes and HyperglycemiaenesNo ratings yet
- Patient profile and drug studiesDocument8 pagesPatient profile and drug studiesEspiridionNo ratings yet
- Endocrine Emergencies in PicuDocument10 pagesEndocrine Emergencies in PicuDr.MohanNo ratings yet
- BSL Management on WardsDocument2 pagesBSL Management on Wardsvigneshkumar.r3850No ratings yet
- 1-A Mother Calls You About Her 8 Years Old Son, Known Case of DM-1 Fell Comatose - She Is Not Sure If He Took The Night & Morning Dose of Insulin. You Will Advice Her ToDocument4 pages1-A Mother Calls You About Her 8 Years Old Son, Known Case of DM-1 Fell Comatose - She Is Not Sure If He Took The Night & Morning Dose of Insulin. You Will Advice Her Tomahi_elsemary7011No ratings yet
- Question For EndoDocument30 pagesQuestion For EndoArti SharmaNo ratings yet
- Theophylline Dosing & Side EffectsDocument3 pagesTheophylline Dosing & Side EffectsWindy Gigiers SeptianiNo ratings yet
- Diabetes Cases: Nahda College Program of Pharmacy Department of Clinical Pharmacy 2020-2021Document23 pagesDiabetes Cases: Nahda College Program of Pharmacy Department of Clinical Pharmacy 2020-2021Basil DomiNo ratings yet
- L Tiple: Përgjigje-Kumar&Clark 'S Clinical MedicineDocument10 pagesL Tiple: Përgjigje-Kumar&Clark 'S Clinical MedicineNreca TokjonaNo ratings yet
- Status Epilepticus - APLSDocument3 pagesStatus Epilepticus - APLSMuhammadafif SholehuddinNo ratings yet
- Nephrotic 2008Document7 pagesNephrotic 2008Herni PurbaNo ratings yet
- Midterms LecDocument276 pagesMidterms LecmyNo ratings yet
- Insulin Therapy Initiation and AdjustmentDocument28 pagesInsulin Therapy Initiation and AdjustmentOsama AlmuqrinNo ratings yet
- ER KHv2 31 215051 22 05 2013 PDFDocument4 pagesER KHv2 31 215051 22 05 2013 PDFCaterina PrepelitaNo ratings yet
- Event1 Jurnalul Pediatrului Supliment 1 2011Document30 pagesEvent1 Jurnalul Pediatrului Supliment 1 2011Caterina PrepelitaNo ratings yet
- Marik Covid Protocol SummaryDocument2 pagesMarik Covid Protocol SummaryCaterina PrepelitaNo ratings yet
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangNo ratings yet
- Contact Details Name: Hospital Telephone:: This Protocol Has 5 PagesDocument5 pagesContact Details Name: Hospital Telephone:: This Protocol Has 5 PagesCaterina PrepelitaNo ratings yet
- ER Ketone v1 31 482224 22 05 2013 PDFDocument4 pagesER Ketone v1 31 482224 22 05 2013 PDFCaterina PrepelitaNo ratings yet
- ER GSD3 v1 31 249136 22 05 2013 PDFDocument4 pagesER GSD3 v1 31 249136 22 05 2013 PDFCaterina PrepelitaNo ratings yet
- Contact Details Name: Hospital Telephone:: This Protocol Has 5 PagesDocument5 pagesContact Details Name: Hospital Telephone:: This Protocol Has 5 PagesCaterina PrepelitaNo ratings yet
- ER A&ECitrin1 119909 22 05 2013Document1 pageER A&ECitrin1 119909 22 05 2013Caterina PrepelitaNo ratings yet
- Cyclical Vomitingv1 235142 22 05 2013Document1 pageCyclical Vomitingv1 235142 22 05 2013Caterina PrepelitaNo ratings yet
- Antibiotic eDocument10 pagesAntibiotic ebvl78No ratings yet
- FebrileDocument7 pagesFebrileCaterina PrepelitaNo ratings yet
- Treatment of MitovondrialDocument16 pagesTreatment of MitovondrialCaterina PrepelitaNo ratings yet
- Aerobic VaginitisDocument4 pagesAerobic VaginitisCaterina PrepelitaNo ratings yet
- 389 FullDocument8 pages389 FullpipimseptianaNo ratings yet
- Packaging Information Hematology Reagent - Diluent: W-31D: Page 1 of 4Document28 pagesPackaging Information Hematology Reagent - Diluent: W-31D: Page 1 of 4A Wahid KemalNo ratings yet
- Catalogo de Regillas D Eretorno Titus de AluminioDocument46 pagesCatalogo de Regillas D Eretorno Titus de AluminiojoravicaNo ratings yet
- NDT PDFDocument0 pagesNDT PDFAnthony CyrilNo ratings yet
- Asme Sec Viii D1 C PT UhtDocument14 pagesAsme Sec Viii D1 C PT Uhtkcp1986No ratings yet
- NABL 108 - National Accreditation Board for Testing and Calibration Laboratories Criteria for Non-Destructive Testing LaboratoriesDocument25 pagesNABL 108 - National Accreditation Board for Testing and Calibration Laboratories Criteria for Non-Destructive Testing LaboratoriesKishore Nayak kNo ratings yet
- JAM 2018 Biotechnology - BTDocument15 pagesJAM 2018 Biotechnology - BTSuman duttaNo ratings yet
- Designing of A TPH Fire Tube Boiler: December 2019Document25 pagesDesigning of A TPH Fire Tube Boiler: December 2019Hélder PascoalNo ratings yet
- Stability ComparisonDocument4 pagesStability Comparisonkunalprabhu148No ratings yet
- FWC Air Cooled Exchanger PDFDocument49 pagesFWC Air Cooled Exchanger PDFdinakaranpatelNo ratings yet
- Hydroprocessing Reactor and Process Design To Optimize Performance (Topsoe - 1998)Document18 pagesHydroprocessing Reactor and Process Design To Optimize Performance (Topsoe - 1998)yliangcaNo ratings yet
- Van Den Hul Pricelist 2009 2010Document49 pagesVan Den Hul Pricelist 2009 2010Ama BlekNo ratings yet
- 3D Printing Technology in Drug Delivery: Recent Progress and ApplicationDocument10 pages3D Printing Technology in Drug Delivery: Recent Progress and ApplicationAngela DelarmenteNo ratings yet
- AMSOIL Synthetic SAE 15W40 Heavy Duty Diesel Marine Motor Oil AMEDocument2 pagesAMSOIL Synthetic SAE 15W40 Heavy Duty Diesel Marine Motor Oil AMEamsoildealerNo ratings yet
- Chem Exam Review SheetsDocument6 pagesChem Exam Review SheetsAljho AljhoNo ratings yet
- Restriction EnzymesDocument17 pagesRestriction EnzymesSatyam AryaNo ratings yet
- Lecture-1. Introduction To Pharmacology-1Document26 pagesLecture-1. Introduction To Pharmacology-1AbdulahiNo ratings yet
- Opportunities For Lightweight Vehicles Using Advanced Plastics and CompositesDocument416 pagesOpportunities For Lightweight Vehicles Using Advanced Plastics and CompositesAltairEnlighten100% (1)
- Quality Training 2014Document20 pagesQuality Training 2014somai4qualityNo ratings yet
- Transition Metals HomeworkDocument17 pagesTransition Metals Homeworkkingman14No ratings yet
- Amity Institute of Pharmacy: B Pharm Ist Semester Pharmaceutical Analysis Pawan Kumar GuptaDocument35 pagesAmity Institute of Pharmacy: B Pharm Ist Semester Pharmaceutical Analysis Pawan Kumar Guptapawan kumar guptaNo ratings yet
- D) 3 AlcoholDocument9 pagesD) 3 AlcoholJessicaNo ratings yet
- E3 BernoulliDocument16 pagesE3 BernoullikishoreNo ratings yet
- Semiconductor Manufacturing ProcessDocument51 pagesSemiconductor Manufacturing Processmanoj3e9329100% (1)
- A Special Selection From Infinite Energy Magazine: Selected Articles From Issues 1 - 45 March/April 1995 - September/October 2002Document117 pagesA Special Selection From Infinite Energy Magazine: Selected Articles From Issues 1 - 45 March/April 1995 - September/October 2002DsgmmmmNo ratings yet
- Maximum Residue Limits For Pesticides - Health CanadaDocument3 pagesMaximum Residue Limits For Pesticides - Health CanadaJose Luis Aguero ParedesNo ratings yet
- PHOTOCHEMISTRYDocument5 pagesPHOTOCHEMISTRYyuki_akitsuNo ratings yet
- Textile Finishing: Shrinkagecontrol: Fabric ScienceDocument18 pagesTextile Finishing: Shrinkagecontrol: Fabric ScienceAnushka Singh100% (2)
- Slump TestDocument4 pagesSlump TestJec SepradoNo ratings yet
- Lecture 24 PDFDocument10 pagesLecture 24 PDFBhavesh Dilip ChanchlaniNo ratings yet
- Terminalia Tomentosa Research DiabetesDocument4 pagesTerminalia Tomentosa Research DiabetesErshad Shafi AhmedNo ratings yet