Professional Documents
Culture Documents
Ekundina Full Text PDF
Uploaded by
chinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ekundina Full Text PDF
Uploaded by
chinCopyright:
Available Formats
African Journal of Cellular Pathology 4:6-12 (2015)
The Official Journal of the Society for Cellular Pathology Scientists of Nigeria
www.ajcpath.com
COMMON ARTIFACTS AND REMEDIES IN HISTOPATHOLOGY
(A REVIEW)
Ekundina VO1, Eze G2
1. Department of Medical Laboratory Science, Afe-Babalola University Ado-Ekiti, Ekiti
State, Nigeria
2. Department of Anatomy, University of Benin, Edo State, Nigeria
Corresponding Author: Ekundina VO
Email: kemvic30@gmail.com, Ekundinavo@abuad.edu.ng
Abstract
The essence of preparing a biological specimen for microscopic studies is to get
adequate and accurate medical information that is a true representation of the
specimen, be it for research or diagnostic purposes. An artifact can be defined as
unrelated, self-colored artificial feature found in tissue sections. This has been an
age long cause of misinterpretation leading to misdiagnosis to microscopists. The
processing of specimen for medical information is subject to a procedure that
results in a tissue fit for diagnosis and interpretation. The procedures themselves
are subject to human and material errors and the result is an artifact that in the
least may interfere with adequate diagnosis or at the most render the tissue so
distorted as to be undiagnosable. The need to recognize these artifacts and attempt
to overcome them is the single biggest challenge in the histopathology Laboratory.
This article focused on identifying artifacts and their potential cause so that
misinterpretation and difficulty in diagnosis can be overcome, and help
microscopist to come into definite diagnosis.
Keywords: Artifacts, Histopathologist, Microscopist, Diagnosis
INTRODUCTION
Artifact can be defined as unrelated, self-colored
artificial features found in tissue sections
(Avwioro, 2014). They occur in tissue sections
before fixation, during fixation, grossing of
specimen, tissue processing, sectioning, staining
and preservation of tissue section. Some
artifacts are easily distinguishable from normal
or diseased tissue components while some are
difficult to distinguish from such entities. In
some situations the presence of an artifact can
compromise an accurate diagnosis. Artifacts
may result in alteration of normal morphologic
and cytological features or even lead to
complete uselessness of the tissue. It is
important to know and understand about
artifacts, as learning to recognize them, can
prevent misdiagnosis. Ficarra et al., (1987),
Margarine et al (1985). These artifacts can be
minor, involving only small portion of the
specimen and therefore do not interfere with the
pathologists ability to provide an accurate
diagnosis. In some cases however, the degree of
artifactural damage is excessive or may involve
the entire specimen, rendering it suboptimal or
useless for diagnostic purposes Ficarra et al.,
(1987). Therefore, this article is to promote an
awareness of the various common artifacts
which may be encountered in histopathology, to
provide a guide for their recognition, to explain
their causes and to suggest where possible, the
means by which their occurrence can be
avoided.
TYPES OF ARTIFACT
Pre-Fixation Artifact
Pre-fixation artifacts are produced in tissues
before fixation. They may take the form of
deposits such as tattoo pigment, or result from a
surgical procedure as with laser knife damage or
crush artifact. Contaminants can also be
introduced into tissues during surgery or whilst
handling prior to, or during specimen dissection.
This type of artifact can only be avoided by
ensuring that those involved are fully aware of
the consequences of allowing a specimen to
become contaminated or otherwise damaged.
EKUNDINA AND EZE
ARTIFACTS
Examples of pre-fixation artifact include:
i.
Artifacts due to surface preparation
The excision margins of fresh surgical
specimens are sometimes marked with coloring
agents to allow appropriate orientation of the
specimen and assessment of these margins
microscopically Krishnanand et al., (2010).
Biopsy area is also prepared by using tincture
iodine. Reagents commonly used for surface
marking include Indian ink, Silver nitrate,
Alcian blue and Alcian green.
electrocautery[ Meghana and Ahmedmujib
(2007), (Seoane, 2004). This causes the surface
epithelium to be forced through the connective
tissue, producing small pseudocysts and also
causes loss of cytoplasmic and nuclear features
(Camacho et al., 2008).
Plate 2: Surgical Artifacts: A) Forceps Artifact:
Tearing of tissue due to penetration of forceps
Plate 1: Artifacts due to surface preparation and
tattoo pigmentation: margin of a skin biopsy marked
with silver nitrate. The reagent stains the soft tissues
and has penetrated into the dermis
REMEDY
Preparation of the area of biopsy with
tincture or other colored solutions should be
cautiously used and should be clearly
mentioned along with biopsy details, as it can
interfere with tissue processing and staining
procedures.
ii.
Tattoo pigment artifact
Various colored insoluble pigments used in
producing decorative tattoos are occasionally
encountered in sections of skin. There is no
tissue reaction to the presence of deposits.
iii.
Forceps artifacts or crush/squeeze
artifacts
When the teeth of the instrument penetrate the
specimen, it results in voids or tears and
compression of surrounding tissue. Other
possible causes of artifacts during surgical
handling are:
Mechanical causes: by instruments commonly
used for biopsy procedures like hemostat and
mosquito hemostat, suction tips, Adson forceps
with or without teeth, atraumatic forceps and
Allis clamps.
Chemical causes: injection of large local
anesthetic solution in excess into the lesional
tissues and application of antiseptic medication
like Betadine solution.
Thermal cause: instruments used
coagulation and cutting electrodes
for
like
REMEDY
These artifacts can be prevented by handling
the specimen gently, avoiding applying
unnecessary force and holding the tissue in
an area away from the lesional tissue.
iv.
Fulgeration artifacts
Heat produced while using laser or
electrosurgical procedures may lead to marked
alteration in both epithelium and connective
tissue Meghana and Ahmedmujib, (2007).
Epithelial cells may appear detached and the
nuclei
assume
a
spindle,
pallisading
configuration, separation of the epithelium from
the basement membrane also occurs. The
fibrous connective tissue, fat and muscle may
show opaque, amorphous appearance.
REMEDY
This artifact can be prevented by using
knives, use low milliamperage current, use of
combination knife and electrical points.
v.
Injection artifact
Injection of large amounts of anesthetic solution
into the area to be biopsied can produce
hemorrhage with extravasations which masks
the normal cellular architecture. Injecting the
solution into the lesional tissue will cause
vaculoation of epithelium and connective tissue
and in addition causes separation of connective
tissue (Meghana and Ahmedmujib, 2007;
Seoane, 2004).
REMEDY
To avoid this, use block technique instead of
infiltration technique and inject the solution
well away from the lesional tissue. Large
quantities of local anaesthetic solution should
not be injected.
7
EKUNDINA AND EZE
vi.
Sutural artifact
Suture material is an occasional inclusion in
histological specimens. It may consist of
isolated fragments or complete fibre-bundles
cut in transverse, oblique or longitudinal planes.
(Seoane, 2004), Ramirez et al., (2007) Detail of
the fibre structure can sometimes be seen upon
careful examination of H&E-stained sections
and these silk sutures exhibit a strong
birefringence under polarized light and this can
be useful in their identification. The presence of
a suture in a histological specimen may not be
of any pathological significance but it can
damage the microtome knife leading to tears
and knife lines in sections.
ARTIFACTS
Reusable processing components (such as
tissue cassette lids), if not thoroughly
cleaned, can also carry fragments of
previous specimens.
REMEDY
Thorough rinsing of the board and
instruments between specimens or covering
the dissection board with separate paper
sheets will prevent this problem.
Plate 5-.Artifacts due to contamination. Specimenspecimen contamination: A section of cardiac muscle
with a piece of extraneous thyroid tissue present
against one surface; H&E.
Plate 3: Sutural artifact: Bifringent suture material
from stitch granuloma under Polarized light.
REMEDY
Visible sutures should be removed wherever
possible
Vii.
Artifacts due to contamination
Certain artifacts can be due to contamination:
(a) Starch artifact due to contamination of
specimen with starch powder used as
lubricant in surgical glove. These starch
granules are retractile, glassy, ply, PAS
positive bodies generally 5-20mm in
diameter. They have spore like
structures with dark central area which
could be misinterpreted as a pyknotic
nucleus or as one undergoing mitosis,
Plate 4 (Artifacts due to contamination). Starch
granules: Starch granules in a typical starch
granuloma stained with H&E and Polarized light
(b) Specimen-specimen
contamination
artifact probably occurs during dissection
where tissue from a previous specimen is
transferred via the instruments used (such as
scalpel blades) or from fragments which
remain on the dissecting board surface.
(c )
Foreign body contamination artifact
often makes the interpretation of the specimen
quite difficult. These artifacts are encountered as
a contaminant arising from paper, cotton gauze
or a cork board used during specimen
preparation. They are usually found on the
surface of the specimen but can be implanted
mechanically during dissection (Ficarra et al.,
1987: Krishnanand et al., 2001)
Plate 6-.Artifacts due to contamination. Foreign body
contamination: Cellulose in an H&E-stained section
and under Polarized light.
REMEDY
Artifact due to contaminations can be
prevented by careful manipulation of
specimen at every step of preparation and
cleaning dissecting board after treating each
specimen.
FIXATION ARTIFACTS
Although fixation is necessary to avoid
diffusion of soluble tissue components and
decomposition, it by itself constitutes a major
cause of artifact. If the procedure is not carried
out under optimal conditions, if fixative does
not have proper access to the tissues, or because
of the nature and quality of the particular
8
EKUNDINA AND EZE
reagent used, artifact can occur. (McInnes,
2005:Weir, 1976). The most commonly used
fixative is 10% formalin. The concentration of
the formalin, contamination and prolong
fixation time leads to difficulty in sectioning of
the specimen. Fixation artifacts arise due to
formalin, mercuric chloride and picric acid used
in various fixative agents which causes BrownBlack granular and yellow stains distributed
randomly throughout the tissues. (Samar et al.,
2014)
Plate 7. Fixation Artifact. Pigment artifact: Deposits
of formalin pigments are brown here in H&E Stain
REMEDY
Treat sections with saturated alcoholic picric
acid solution or prevent it by fixing in
buffered formalin
i. Shrinkage artifacts: During fixation,
tissues change in size. This is due to
inhibition of cellular respiration and
changes in membrane permeability. As a
result tissues that are attached in life may be
pulled away from each other, leaving empty
spaces (McInnes E 2005), this is a very
common artifact. Some of the non protein
precipitants cause swelling of tissue
following fixation in formalin.
REMEDY
Shrinkage artifact can be prevented by using
compound fixatives compensating for
disadvantages of individual fixatives as seen
in Bouins fluid.
ii. Streaming artifacts: This is an important
type of artifact due to diffusion of unfixed
material to give false localization by coming
to rest in same place other than its original
location. A well known example of this is
glycogen.
REMEDY
Fixation of tissue for glycogen study should
be prompt as there is an initial sharp loss of
glycogen in postmortem solution and it
should be carried out at 4 degrees in 80%
alcohol
ARTIFACTS
Plate. 8 streaming of glycogen, Seen in hepatic tissue
iii. Diffusion artifacts: Materials may
sometimes diffuse out of the tissue. Apart
from large molecules, small molecules like
inorganic ions and biogenic amines can be
lost from tissue. For example; when cut end
of adrenal gland tissue are placed in iodate
for iodate reaction, late cholamines can be
seen leaving the tissue as a red cloud of
aminochromes. (Samar et al., 2014)
iv. Artifacts due to microwave fixation:
Optimum temperature for microwave
fixation is 45-55 oC. Under heating results
in poor section quality whereas overheating
above
65oC
produces
vacuolation,
overstained cytoplasm and pyknotic nuclei
Remedy: Maintain optimal temperature
during this procedure
v. Artifacts during freeze-drying - ice crystal
artifacts: During fixation using freeze
drying method, the tissue must be plunged
into isopentane cooled to -160 to -180 oC
with liquid nitrogen immediately. Low
temperature is important because unless the
whole tissue is frozen, large ice crystals are
formed
causing
disruption
artifacts
(Thomson A 2007). This artifact causes
total distortion of the tissue and diagnostic
difficulty.
Vi Artifacts due to prolonged fixation: Prolong
fixation causes secondary shrinkage and
hardening which leads to separation of portion
of tissues giving the appearance of empty
spaces.
Vii Artifacts during post fixation treatment:
Tissue that are fixed in chrome if not washed for
24 hours in running tap water could produce
chromeoxide pigment
TISSUE PROCESSING ARTIFACTS
Tissue processing is designed to remove all
extractable water from tissue, replacing it with a
support medium that provides sufficient rigidity
to enable sectioning of the tissue without
damage or distortion and artifacts are produced
at each step if proper care and procedures are
9
EKUNDINA AND EZE
ARTIFACTS
not followed. Examples of tissue processing
artifact include the following.
i.
Artifacts During Dehydration:
Artifacts can be
dehydration due to
encountered
Artifacts Due to Poor Processing:
Extensive loss of architectural details and
clarity within loose connective tissue may
reflect inadequate fixation. These can be
caused by faults in tissue processing: such
as too short processing cycle, inappropriate
choice of reagents, use of exhausted
reagents or error in replacing solvents.
Krishnanand et al., (2010), Grizzle et al.,
(2001)
v.
during
1. Improper gradient of dehydration, if the
concentration gradient between the fluid
inside and outside the tissue is excessive,
diffusion current cross the cell membranes
during fluid exchange thus resulting to
increase in possibility of cell distortion
(Margarine et al., 1985) (McInnes E 2005)
2. Over dehydration makes the tissue hard,
brittle and shrunken causing difficulty while
cutting and also interfere with staining
properties of section (Grizzle et al., 2001)
3. Under or Incomplete dehydration results
in improper infiltration of paraffin and block
made is difficult to section thus leading to
distorted or fragmented tissue sections
which causes artifactural features.
ii.
microtome, tearing of section thereby
making microscopic study of tissue difficult.
ARTIFACT DUE TO MICROTOMY AND
SECTION MOUNTING
i.
Artifacts Related To Microtomy:
Various forms of mechanical damage produced
during section cutting and flotation, together
with a range of contaminants from a variety of
sources are commonly encountered in sections.
Artifacts During Clearing:
Artifacts may arise due to over and
under clearing of tissue causing
excessive hardening, and thus obstruct
paraffin impregnation of tissue making
it difficult to cut during sectioning.
Krishnanand et al., ( 2010), Margarine
et al., ( 1985)
Artifacts During Impregnation:
The function of wax impregnation is to
remove clearing agent (wax solvent) from
the tissue and for it to be completely
permeated by the paraffin wax which is
subsequently allowed to harden to produce
a block from which sections are cut. The
artifact produced during this procedure is
Crystallization: The thicker the tissue, the
more clearing agent it absorbs and hence it
requires multiple change of molten wax to
be completely impregnated. Contamination
of molten wax by clearing agent causes
incomplete impregnation leading to
crumbling and crystallization during
sectioning (Samar et al., 2014)
iii.
ii.
Artifacts Related to Tissue Floating on
Water Bath:
Mainly three types of artifacts can result from
floating:
(a). Air Bubble Entrapment: trapped water
bubble under section, occurs due to poor
floatation technique where sections are dropped
rather than pull gently across the water surface
or due to bubbles already present in water bath
dislodged by the slide and rise up under the
section. These air bubbles trapped in a section
after flotation and mounting can collapse on
drying, leaving zones which cracks and fails to
adhere properly to the slide.
(b). Increase temperature of water bath results
into expansion of tissue beyond its limit and
Parched Earth (crackes) effect is noted.
(c) Floaters Artifacts are pieces of tissues that
appear on slide that do not belong there, they are
mainly extraneous to the floated section and
these results mainly from unclean floating bath.
Artifacts During Embedding:
Artifacts due to improper orientation are
frequently encountered during embedding
procedures which will lead to damage to
iv.
10
EKUNDINA AND EZE
ARTIFACTS
microorganisms, airborne fibres, cellulose fibres
and dirt particles.
STAINING ARTIFACTS
i.
Artifacts due to residual wax:
Plate 10 water bubble trapped in section
Artifacts in water bath: Air bubble entrapment;
Section of lymph node showing circular darkly
stained areas with pale centers and surrounding radial
cracks. These faults indicate collapsed bubble
artifact; H&E Stain.
iii.
Artifacts related to oven/hot plate:
The temperature setting of the oven/hot plate
should be approximately that of the melting
point of paraffin. This type of artifact arises due
to increase in temperature beyond melting point
of paraffin. If the oven is too hot there may be
distortion to the cells causing dark pyknotic
nuclei or nuclear bubbling. Cells appear to be
completely devoid of nuclear details.
iv.
Artifacts During Lifting of Tissue
Sections:
Artifacts such as Tissue Folds can be produce
when tissue adheres to the under surface of the
blade, seen most commonly with fatty tissues
and mainly seen due to dull blade. They can be
avoided by transferring the sections to a new
water bath or by passing light of Bunsen burner
over the section and also by adding small
amount of detergent may be helpful. Tissue
Tearing is produced when tissue adheres to the
undersurface of the blade. This is mainly seen
due to dull blade, these tearing can be avoided
by using clean and replaced blade.
Residual wax in a section will prevent
penetration of both aqueous and alcoholic dye
solutions leaving areas totally devoid of stain.
Traces of residual wax have a subtle effect on
nuclear staining producing small patches in
sections where nuclei appear muddy and lack
detail (Krishnanand et al., 2010; Wynnchuk,
1990)
Plate 12 Artifact due to residual wax
REMEDY
Prolonged xylene treatment and re-staining
will overcome this problem
ii.
Artifacts due to contaminated staining
solution
Staining solutions can be contaminated by
microorganisms, dust/ foreign particle and
could serve as a potential cause of
misdiagnosis.
Artifacts due to stain deposits:
Undissolved and precipitated stain will lead to
deposits on sections.
v.
Artifacts due to incomplete or unstained
areas:
Inadequately
filled
staining
dish
or
accumulation of staining solution at the top of
slide will cause such artifacts. Grizzle et al.,
(2001)
Plate 11: Artifacts during lifting of tissues: Tissue
folds; H&E Stain.
v.
Artifacts due to section adhesive and
mounting:
Thick coat of section adhesive will take the stain
and background stain may be detected resulting
in irregular, poor quality sections. Mounted,
unstained section left uncovered can be
contaminated with various materials such as
Plate .13 Artifacts due to incomplete staining
MOUNTING ARTIFACTS
During mounting, air bubble entrapment,
residual water and excessive use of mounting
media will bring artifactural changes. These
11
EKUNDINA AND EZE
changes can be avoided if proper mounting
technique is incorporated.
MICROSCOPY ARTIFACTS
Dust particles, impurities which can be internal
or external present on slide will bring
artifactural changes. Fatty films are observed
due to unclean lenses or greasy deposits on
eyepieces due to eyelashes will results in foggy
appearance.
ARTIFACTS
Camacho FA, Jornet PL, Torres M J, Orduna A
(2008). Analysis of the histopathological
artifacts in punch biopsies of the normal oral
mucosa. Med Oral Patol Oral Cir Bucal.
13(10):E636-9. .
Ficarra G, Clintock B, Hansen L (1987).
Artifacts created during oral biopsy procedures.
J Craniomaxillofac Surg. 15(1):34-7.
Remedy
Ensure that microscopes are well kept and
regularly maintained
Grizzle WE, Stockard C, Billings P (2001). The
effects of tissue processing variables other than
fixation on histochemical staining and
immunohistochemical detection of antigens. J
Histotechnology. 24(3):213219.
Section Preservation Artifacts
This include majorly drying artifact and
bleaching artifact
Krishnanand P, Kamath V, Nagaraja A. (2010).
Artefacts in Oral Mucosal Biopsies A Review.
Orofac Sci, 2(1); 57-62.
Margarine JE, Natiella J, Vaughan CD (1985).
Artifacts in oral biopsy specimen. J Oral
Maxillofac Surg. Mar;43(3):163-72.
McInnes E. (2005). Artefacts in histopathology
Comp Clin Path. 13:100108.
Plate. 14 bleaching present due to exposure of
stained section to light.
SUMMARY
The processing of specimen for adequate
medical information is subject to a procedural
protocol that results in a tissue fit for diagnosis
and interpretation. The procedures themselves
are subject to human, reagents and material
errors which may result in artifact that in the
least may interfere with adequate diagnosis or at
the most render the tissue so distorted as to be
undiagnosable. The need to recognize these
artifacts and attempt to overcome them is the
single biggest challenge in the histopathology
Laboratory. This review article focused on
identifying artifacts, their potential cause and
remedies so that misinterpretation and difficulty
in diagnosis can be overcome and help
microscopist to come into definite diagnosis.
REFERENCES
Avwioro OG, Histochemistry and tissue
pathology principles and techniques, third
edition, claverianum press Nigeria ltd 2014 pg
119
Meghana SM,
Ahmedmujib BR. (2007).
Surgical artefacts in oral biopsy specimens:
Punch biopsy compared to conventional scalpel
biopsy. J Oral Maxillofac Pathol 11:11-14.
Ramrez AM, Silvestre E, Juan M. (2007). Oral
biopsy in dental practice. Med Oral Patol Oral
Cir Bucal. 12(7):E504-10.
Samar K, Manisha T, Megha J, and Ami D
(2014). Artifacts in Histopathology: A Potential
Cause of Misinterpretation RRJDS. 2 (2), 23-31
Seoane C, Ramirez J (2004). Artefacts in oral
incisional biopsies in general dental practice: a
pathology audit. Oral Diseases. 10, 113117.
Thomson A, Wallace W. Fixation artefact in an
intra-operative frozen section: a potential cause
of misinterpretation. Journal of Cardiothoracic
Surgery. 2007.
Weir JC, Weathers RA. (1976). Fixation
artifacts simulating acantholytic disease. Oral
Surg Oral Med Oral Pathol. 41 (1):105-8.
Wynnchuk M. (1990). An artifact of H&E
staining: The problem and its solution. The J
Histotechnol 13:193-198.
12
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Spooky Scary SkeletonDocument6 pagesSpooky Scary SkeletonPiano Covers0% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
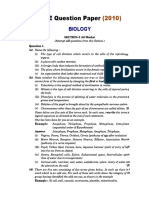
- ICSE QUESTION PAPER Biology 2010 Class 10 PDFDocument11 pagesICSE QUESTION PAPER Biology 2010 Class 10 PDFLokesh MalikNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- List of Companies (FSC) 2015Document12 pagesList of Companies (FSC) 2015chinNo ratings yet
- Immunology Exam Q's With AnswersDocument26 pagesImmunology Exam Q's With AnswersHavardKrovel87% (55)
- Second Periodical Test Science 6Document12 pagesSecond Periodical Test Science 6Hardy Misagal100% (1)
- 1 Крок 1 ЛС KROK 2007 2017 English BiochemistryDocument480 pages1 Крок 1 ЛС KROK 2007 2017 English BiochemistryAbhani MøhitNo ratings yet
- GaussProblemsSolutions 001Document3 pagesGaussProblemsSolutions 001chinNo ratings yet
- Liver CirrhosisDocument20 pagesLiver CirrhosischinNo ratings yet
- Chronic/ Repetitive Injury Aorta Coronary Popliteal ICA Circle of WillisDocument4 pagesChronic/ Repetitive Injury Aorta Coronary Popliteal ICA Circle of WillischinNo ratings yet
- UDPG1673 - Tutorial 3 - 201601Document3 pagesUDPG1673 - Tutorial 3 - 201601chinNo ratings yet
- References: of The Lung: An Update. (Online) Available atDocument2 pagesReferences: of The Lung: An Update. (Online) Available atchinNo ratings yet
- Arachidonic Acid MetabolitesDocument1 pageArachidonic Acid MetaboliteschinNo ratings yet
- Cover PageDocument1 pageCover PagechinNo ratings yet
- Cover PageDocument1 pageCover PagechinNo ratings yet
- UDDD2223 Neurobiology Tutorial 3: Universiti Tunku Abdul RahmanDocument1 pageUDDD2223 Neurobiology Tutorial 3: Universiti Tunku Abdul RahmanchinNo ratings yet
- Tutorial 4 Jan 2016 QPDocument2 pagesTutorial 4 Jan 2016 QPchinNo ratings yet
- LicenseDocument6 pagesLicensechin50% (2)
- UDPG1673 - Tutorial 7 - 201601Document4 pagesUDPG1673 - Tutorial 7 - 201601chinNo ratings yet
- IB Singh Vol-2Document387 pagesIB Singh Vol-2dannyNo ratings yet
- Chap 8Document17 pagesChap 8Shane EsparasNo ratings yet
- Muscle PhysiologyDocument64 pagesMuscle Physiologylynn.dargham2No ratings yet
- Rain Natomy: Adapted From Human Anatomy & Physiology by Marieb and Hoehn (9 Ed.)Document16 pagesRain Natomy: Adapted From Human Anatomy & Physiology by Marieb and Hoehn (9 Ed.)vibs1994No ratings yet
- Disorders of Red Blood CellsDocument27 pagesDisorders of Red Blood Cellskirti sharmaNo ratings yet
- Study Guide For Introduction To Maternity and Pediatric Nursing 5th Edition Leifer Test BankDocument36 pagesStudy Guide For Introduction To Maternity and Pediatric Nursing 5th Edition Leifer Test Banknephriteprimelyqihx100% (21)
- Cephalometric Lecture-1Document45 pagesCephalometric Lecture-1Batman 02053No ratings yet
- Tissue Renewal and Repair RegenerationDocument13 pagesTissue Renewal and Repair Regenerationمحسن حدوان عليخانNo ratings yet
- Physiology of Reproduction in Women IDocument34 pagesPhysiology of Reproduction in Women Iapi-196413370% (1)
- Floyd17 TB Ch12Document5 pagesFloyd17 TB Ch12sdjuknicNo ratings yet
- NERVOUS SYSTEM (IB-DP BIOLOGY) - Multiple Choice Type QuestionsDocument5 pagesNERVOUS SYSTEM (IB-DP BIOLOGY) - Multiple Choice Type QuestionsVishnu SharmaNo ratings yet
- ScienceGeography3ResourceSample PDFDocument9 pagesScienceGeography3ResourceSample PDFmargantoniNo ratings yet
- 2020 Pathology Compilation Questions by TopicsDocument7 pages2020 Pathology Compilation Questions by Topicsrupertgrint2000No ratings yet
- CH 8 Digestive System: StructuresDocument18 pagesCH 8 Digestive System: StructuresBheru LalNo ratings yet
- Pigeon DissectionDocument10 pagesPigeon DissectionAnonymous 3NmUUDtNo ratings yet
- 2013 BAA - Glossary of Common Medical Prefixes and Suffixes For BAA and BLSDocument5 pages2013 BAA - Glossary of Common Medical Prefixes and Suffixes For BAA and BLSM GavinNo ratings yet
- 5 - The Visual System and Mechanisms of PerceptionDocument13 pages5 - The Visual System and Mechanisms of PerceptionElmer SalazarNo ratings yet
- MVW 020Document9 pagesMVW 020SofyanNo ratings yet
- 10 TH Science Practical Guide EM PDFDocument15 pages10 TH Science Practical Guide EM PDFSRI VISHNUNo ratings yet
- Cavidades Corporales AnatomiaDocument4 pagesCavidades Corporales AnatomiaBOKOR5000No ratings yet
- ArteriDocument1 pageArterifakira tanzilNo ratings yet
- Astrocyte: Structure & FunctionDocument7 pagesAstrocyte: Structure & Functionمحمود الموسويNo ratings yet
- Study Guide: Cytokines Associated With Innate ImmunityDocument12 pagesStudy Guide: Cytokines Associated With Innate ImmunityxxxxxxxNo ratings yet
- ThyroidDocument7 pagesThyroidverawoNo ratings yet
- Locomotion and MovementDocument9 pagesLocomotion and MovementVishal JoshiNo ratings yet