Professional Documents
Culture Documents
Hemoptysis: Causes and Evaluation of Blood in the Sputum
Uploaded by
Atikah PurnamasariOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemoptysis: Causes and Evaluation of Blood in the Sputum
Uploaded by
Atikah PurnamasariCopyright:
Available Formats
39
Hemoptysis
RALPH COREY
paste" sputum . Rarely, a patient will present with pseudohemoptysis created artificially by various means .
Associated pulmonary symptoms such as chronic cough
with sputum production, change in cough, shortness of
breath on exertion, chest pain (especially of a pleuritic nature), and wheezing are also important in the evaluation of
hemoptysis . The relation between these symptoms and the
onset of hemoptysis can be quite helpful . For example, hemoptysis in lung cancer or tuberculosis usually is a late symptom preceded by weight loss, change in cough, fatigue, and
other chronic symptoms .
Other points of the history that must be addressed include previous pulmonary infections, recent blunt chest
trauma, seizures, and lower extremity pain or swelling ; exposure to such agents as cigarette smoke, alcohol, asbestos,
and tuberculosis ; use of medications (e .g ., anticoagulants) ;
and finally, systemic symptoms such as fever, weight loss,
and other bleeding problems, especially hematuria (Table
39.1) . The age of the patient is also useful in narrowing the
differential diagnosis. Cystic fibrosis is a disease of children
and young adults ; mitral stenosis, bronchial adenomas,
Goodpasture's syndrome, and primary pulmonary hypertension occur in the middle aged ; and carcinoma of the
lung is usually seen in patients over 50 years of age .
Definition
Hemoptysis is the expectoration of blood or blood-tinged spu-
tum from the lungs or tracheobronchial tree .
Technique
Hemoptysis is an important symptom that elicits fear in both
the patient and physician . Work-up for this symptom should
be undertaken immediately unless the problem is both mild
and recurrent, in which case a conservative approach may
sometimes be preferable .
A thorough history may help define not only the site but
also the cause of bleeding . When evaluating hemoptysis, the
first step is to convince yourself that the lower respiratory
tract is the source of the bleeding . Coughing is important
because nonpulmonary sources of bleeding are not usually
associated with hemoptysis . Questions regarding epistaxis
and spitting blood without coughing help rule out the upper
respiratory tract as the source of bleeding, but do not replace a thorough nose and throat examination . Further, the
physician must be convinced that the bleeding is not of
gastrointestinal origin . A history of nausea, vomiting, heartburn, and abdominal pain may be helpful, but occasionally
the differential diagnosis is difficult and requires either direct observation of the patient's hemoptysis or endoscopic
evaluation of the upper gastrointestinal tract.
The physician should quantify the amount of bleeding
that has taken place, being as specific as possible (e .g ., a
teaspoon, a cupful) . Patients and physicians usually overestimate the amount of bleeding, so nothing can replace
direct observation . The approximate rate of bleeding requires careful quantification . Because the rapidity and the
extent of the work-up depend to a large degree on the above
quantification, the importance of this aspect of the history
cannot be overemphasized .
Note if this is the first episode of hemoptysis or whether
it is a chronic and/or recurrent problem . The quantity of
past bleeding and the extent of previous evaluations are
quite helpful . Despite the fact that repeated evaluations for
recurrent hemoptysis are often advocated by experts, such
evaluations can be both expensive and unrewarding in many
patients .
One should next investigate thoroughly the material being
produced . Is the patient coughing up bright red blood or
blood clots (as in carcinoma of the lung, tuberculosis, pulmonary embolism) ; blood-streaked, purulent sputum (as in
bronchitis, bronchiectasis, or pneumonia) ; blood-tinged,
white, frothy sputum (as in congestive heart failure) ; or foulsmelling, bloody sputum (as in an anaerobic lung abscess)?
Red sputum that contains no blood is seen in a rare case of
Serratia marcescens pneumonia with its red pigmentation,
in glass sanders with sputum discolored by iron oxide, and
in ruptured hepatic amebic liver abscess with its "anchovy
Basic Science
Depending on the underlying disease, hemoptysis is a result
of several different pathologic mechanisms . Remember that
the lung contains two separate vascular systems : the pulmonary and the bronchial vessels . Hemoptysis can occur
with involvement of either.
Infarction of lung tissue with hemoptysis can occur in
numerous diseases . Pulmonary emboli often present with
hemoptysis as a result of ischemic pulmonary parenchymal
necrosis . A similar ischemic necrosis can be seen in all idiopathic vasculitides involving the pulmonary vessels, including Wegener's granulomatosis . Infections causing blood
vessel invasion with infarction include primarily Staphylococcus aureus, Pseudomonas aeruginosa, Aspergillus fumigatus,
and the phycomycetes .
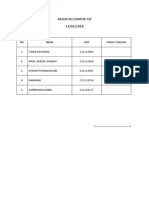
Table 39 .1
Important Points of the History in Hemoptysis
Symptoms of upper respiratory or gastrointestinal disease
Quantity and rate of bleeding
Previous hemoptysis, including extent of previous evaluations
Appearance of sputum
Other pulmonary symptoms (e .g ., chronic cough, chest pain)
Other systemic symptoms (e .g ., fever, weight loss)
Other bleeding problems
Toxic exposures, especially cigarette smoke
211
212
III . THE PULMONARY SYSTEM
Vascular engorgement with erosion is another mechanism of hemoptysis . This occurs within the bronchial capillaries in the mucosa of the tracheobronchial tree as a result
of acute infection such as viral or bacterial bronchitis, chronic
infection such as bronchiectasis, or a toxic exposure such
as cigarette smoke . The shearing force of coughing can
result in bleeding .
Local hyperemia is seen in the common bacterial pneumonias such as Streptococcus pneumonia . Vascular congestion
is followed by red hepatization of the lung where alveoli
are filled with blood-tinged fluid and bacteria to which neutrophils and fibrin are added . This results in the production
of the rust-colored, purulent sputum classically seen in
pneumococcal pneumonia . A similar situation is found in
contusion of the lung with exudation of blood and fluid
into the alveoli . Of course, the purulent nature of the sputum is absent in this situation .
Vascular engorgement of dilated bronchial vessels, along
with anastomoses between the pulmonary and bronchial
circulations, occurs in tuberculosis, bronchiectasis, lung abscesses, and cystic fibrosis . Resulting erosion and rupture
of the pulmonary capillaries or adjacent bronchial arteries
leads to hemoptysis that can be massive . Rupture of a Rasmussen's aneurysm (a dilated bronchial vessel in the wall of
a tuberculous cavity) is a relatively rare cause of hemoptysis .
Necrosis of pulmonary parenchyma can be seen in chronic
infections such as tuberculosis and in malignant tumors of
the lung . The latter can also cause bleeding by outgrowing
their blood supply with resultant tumor necrosis, as well as
by bronchial mucosal invasion (also seen in tuberculosis) .
Large vessel invasion can rarely result in massive hemoptysis .
Disruption of the pulmonary capillaries can be seen either
as a result of increased intravascular pressure (as in mitral
stenosis and left ventricular failure) or as a result of disruption of the alveolocapillary basement membrane from
the antibasement membrane antibody seen in Goodpasture's syndrome .
Aspergillomas are frequently associated with hemoptysis .
Local friction from the moving fungus ball, reactive capillary proliferation with bronchiopulmonary anastomoses, and
release of a proteolytic enzyme are all postulated as having
a role in the etiology of the bleeding .
Clinical Significance
Hemoptysis must always be considered a serious and potentially lethal complication of the underlying process . When
an aggressive approach is taken in the evaluation of hemoptysis, a cause can be determined in approximately 90% of
cases . Table 39 .2 outlines the main causes of hemoptysis .
Marked variation is seen from center to center depending
on whether inpatients or outpatients are categorized, whether
tuberculosis is prevalent, and whether one is evaluating surgical or medical patients .
The amount of bleeding is useful in the differential diagnosis of hemoptysis . More benign processes such as bronchitis and pneumonia cause the majority of all cases of
hemoptysis, but they are less common as the severity of the
bleeding increases . Massive hemoptysis is most commonly
associated with lung cancer, bleeding diathesis (e .g ., leukemia during chemotherapy, anticoagulation), cystic fibrosis, and tuberculosis .
A more complete (but by no means exhaustive) list of
causes is given in Table 39 .3 and helps one formulate an
Table 39 .2
Major Causes of Hemoptysis
Cause
Bronchitis
Bronchiectasis
Pneumonia
Lung abscess
Tuberculosis
Lung cancer
Congestive
heart
failure
Other'
Unknown
Major
(>200 cc/24 hr)
Massive
(>1000 cc/24 hr)
50%
0-5
10
0-5
3-5
10-15
25%
0-15
0-5
0-5
3-70
20
0-7%
0-5
1-2
0-5
3-70
30
0-5
10
10
0-5
20-40
10
1-2
10-50
10
All
Includes anticoagulation, leukemia, metastatic neoplasm, and cystic
fibrosis .
approach to the physical examination . A young healthy
woman with chronic hemoptysis may well have a bronchial
adenoma, but the same patient presenting with dyspnea and
hemoptysis may have mitral stenosis or primary pulmonary
hypertension ; mucocutaneous telangiectasis are often seen
in Osler-Weber-Rendu syndrome ; putrid sputum in an alcoholic or seizure patient points toward a lung abscess . Streak
hemoptysis in a chronic smoker is often due to bronchitis,
but carcinoma of the lung must always be ruled out, especially when the patient has associated symptoms such as
weight loss . Chronic cough with fever and weight loss complicated by hemoptysis can be seen both in tuberculosis and
bronchiectasis, although the latter often has more marked
sputum production . A systemic disease resulting in hemoptysis points toward a vasculitis or Goodpasture's syndrome .
Therapy depends on the underlying process and the rate
of hemoptysis . Amounts greater than 1000 ml in 24 hours
calls for an aggressive diagnostic approach . The risk of dying
with this degree of hemoptysis, however, rests primarily on
the underlying disease . Bronchitis and bronchiectasis have
a low mortality even with this amount of bleeding, whereas
patients with tuberculosis, lung cancer, and lung abscesses
Table 39 .3
Common Causes of Hemoptysis
Arteriovenous malformations
Bleeding diathesis
Bronchial adenoma
Bronchiectasis
Bronchitis
Bronchogenic carcinoma
Cystic fibrosis
Goodpasture's syndrome
Leukemia
Lung abscess
Metastatic neoplasm
Mycetoma
Pneumoconiosis
Pneumonia
Primary pulmonary hypertension
Pulmonary edema due to left ventricular failure or mitral
stenosis
Pulmonary infarction
Trauma
Tuberculosis
Wegener's granulomatosis
39 . HEMOPTYSIS
have a higher risk . Therapy is controversial and is usually
nonsurgical except in a small group of patients with a resectable lesion on chest roentgenogram and respiratory or
hemodynamic failure .
References
Abbot OA . The clinical significance of pulmonary hemorrhage : a
study of 1316 patients with chest disease . Dis Chest 1948 ; 14 :82442 .
Bobrowitz ID, Ramakrishna S, Shim Y-S . Comparison of medical
vs . surgical treatment of major hemoptysis . Arch Intern Med
1983 ; 143 :1343-46 .
213
Conlan AA, Hurwitz SS, Krige L, et al . Massive hemoptysis : review
of 123 cases . J Thorac Cardiovasc Surg 1983 ;85 :120-24 .
Corey R, Hla KM : Major and massive hemoptysis : A reassessment
of conservative management . Am J Med Sci 1987 ;294 :301-309 .
Liebow AA, Hales MR, Lindskog GE . Enlargement of the bronchial
arteries and then anastomosis with the pulmonary arteries in
bronchiectasis . Am J Pathol 1949 ;25 :211-20 .
Rasmussen V . On hemoptysis, especially when fatal in its anatomical
and clinical aspects . Edinburgh Med J 1868 ;14 :384-85 .
Statement by the Committee on Therapy . Management of hemoptysis . Am Rev Respir Dis 1966 ;93 :471-74.
Wolfe JD, Simmons DH . Hemoptysis : diagnosis and management .
West J Med 1977 ;127 :383-90 .
You might also like
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- A. B.R. Thomson, E. A. Shaffer-First Principles of Gastroenterology and Hepatology-CreateSpace Independent Publishing Platform (2012) PDFDocument826 pagesA. B.R. Thomson, E. A. Shaffer-First Principles of Gastroenterology and Hepatology-CreateSpace Independent Publishing Platform (2012) PDFAtikah PurnamasariNo ratings yet
- MandalaDocument80 pagesMandalavanag99152100% (1)
- The Clinical Assessment of Infants, Preschoolers and Their Families - IACAPAPDocument22 pagesThe Clinical Assessment of Infants, Preschoolers and Their Families - IACAPAPcpardilhãoNo ratings yet
- Hemoptysis 1Document27 pagesHemoptysis 1Aida SiregarNo ratings yet
- Mental and Emotional Health PowerpointDocument36 pagesMental and Emotional Health PowerpointYen Aduana86% (7)
- HemoptysisDocument35 pagesHemoptysisElad MizrahiNo ratings yet
- PneumothoraxDocument36 pagesPneumothoraxEira Lopez60% (5)
- Usepa 2014Document16 pagesUsepa 2014walidNo ratings yet
- Classification of MalocclusionDocument8 pagesClassification of MalocclusionDevata RaviNo ratings yet
- Food PoisoningDocument11 pagesFood PoisoningLeanne Teh100% (1)
- Pulmonary Embolism Guide: Causes, Symptoms & DiagnosisDocument60 pagesPulmonary Embolism Guide: Causes, Symptoms & DiagnosisRafika RaraNo ratings yet
- Five Animal FrolicsDocument46 pagesFive Animal FrolicsGhitiu50% (2)
- Abnormal Uterine Bleeding Causes and TreatmentDocument29 pagesAbnormal Uterine Bleeding Causes and TreatmentJed Mostajo100% (2)
- Askep Emboli Paru - Edema Paru - Cor PulmonalDocument63 pagesAskep Emboli Paru - Edema Paru - Cor PulmonalDhevy Sa'PhuttRyyNo ratings yet
- AlprazolamDocument2 pagesAlprazolamGLen CaniedoNo ratings yet
- Hemoptysis 1216302404643775 8Document33 pagesHemoptysis 1216302404643775 8abdul sahidNo ratings yet
- Brush Up On Your Drug Calculation SkillsDocument12 pagesBrush Up On Your Drug Calculation SkillsMichael Baylon DueñasNo ratings yet
- AM Cert Disability FMLA GLA 10981 PDFDocument5 pagesAM Cert Disability FMLA GLA 10981 PDFEsteven Michal Al-Merlin Wallace Ceelah El BeyNo ratings yet
- Pulmonary Tuberculosis Case PresentationDocument71 pagesPulmonary Tuberculosis Case PresentationSimeonDomingoTorresSy100% (4)
- Chronic Obstructive Disease by HibaDocument38 pagesChronic Obstructive Disease by HibahibaNo ratings yet
- Hirschsprung Disease FarieDocument38 pagesHirschsprung Disease FarieFarie Farihan67% (3)
- Acute Respiratory Distress SyndromeDocument36 pagesAcute Respiratory Distress Syndromedr9348345000No ratings yet
- Hemoptysis vs Haematemesis GuideDocument45 pagesHemoptysis vs Haematemesis GuideAlan Dwi SetiawanNo ratings yet
- Pneumoniae, Haemophilus Influenzae, or Moraxella Catarrhalis, IncreasingDocument4 pagesPneumoniae, Haemophilus Influenzae, or Moraxella Catarrhalis, IncreasingParth BhayanaNo ratings yet
- Practice Essentials of Pulmonary ThromboembolismDocument39 pagesPractice Essentials of Pulmonary ThromboembolismEzzat Abdelhafeez SalemNo ratings yet
- Cor Pulmonale (Pneumoconiosis)Document23 pagesCor Pulmonale (Pneumoconiosis)Sai charithaNo ratings yet
- Cor PulmonaleDocument14 pagesCor PulmonaleEvangelin MelvinNo ratings yet
- Introduction to Cor Pulmonale: Causes, Symptoms, and DiagnosisDocument15 pagesIntroduction to Cor Pulmonale: Causes, Symptoms, and DiagnosisRizky Zulfa Afrida100% (1)
- Approach 2 PDFDocument55 pagesApproach 2 PDFdoc_next_doorNo ratings yet
- Cor Pulmonale: Right Heart Failure Due to Lung DiseaseDocument62 pagesCor Pulmonale: Right Heart Failure Due to Lung DiseaseAlbert NixonNo ratings yet
- ARDSDocument23 pagesARDSDumora FatmaNo ratings yet
- HemoptysisDocument3 pagesHemoptysisjerwin01041No ratings yet
- Pleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)Document10 pagesPleural Effusion in Adults—Etiology, Diagnosis, and Treatment (24.05.2019)lordiroh1No ratings yet
- Sclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaleDocument2 pagesSclerodactyly, and Telangiectasis) Syndrome Accompany-: Cor PulmonaledivinaNo ratings yet
- Respiratory Step 2 CK NoteDocument41 pagesRespiratory Step 2 CK NoteXboyx MahdiNo ratings yet
- Hemoptysis EditedDocument11 pagesHemoptysis EditedRashed ShatnawiNo ratings yet
- Pulmonary ThromboembolismDocument4 pagesPulmonary ThromboembolismValerrie NgenoNo ratings yet
- PE Diagnosis & TreatmentDocument3 pagesPE Diagnosis & TreatmentHeidi M FischerNo ratings yet
- Pathophysiology: Pulmonary Embolus Hypoalbuminemia CirrhosisDocument42 pagesPathophysiology: Pulmonary Embolus Hypoalbuminemia CirrhosisLala Aya-ayNo ratings yet
- Everything You Need to Know About Chronic Cor PulmonaleDocument7 pagesEverything You Need to Know About Chronic Cor PulmonaleAnastasia Eka PuteriNo ratings yet
- Pulmonary Edema - StatPearls - NCBI BookshelfDocument7 pagesPulmonary Edema - StatPearls - NCBI BookshelfriyanasirNo ratings yet
- Pulmonary Edema: Causes, Symptoms and Treatment of 'Water in the LungsDocument23 pagesPulmonary Edema: Causes, Symptoms and Treatment of 'Water in the LungsLouella RamosNo ratings yet
- COPD and Chronic Cor PulmonaleDocument6 pagesCOPD and Chronic Cor PulmonaleMiranty Aditya HadiniNo ratings yet
- Pulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional EditionDocument25 pagesPulmonary Embolism (PE) - Pulmonary Disorders - MSD Manual Professional Editionpeterpavel112No ratings yet
- Respiratory diseases guideDocument71 pagesRespiratory diseases guideZafir SharifNo ratings yet
- History and Physical Examination: EvaluationDocument3 pagesHistory and Physical Examination: EvaluationDore NanNo ratings yet
- Cor Pulmonale GuideDocument9 pagesCor Pulmonale GuideMaríaDelPilarAguilarNo ratings yet
- Pulmonary HypertensionDocument9 pagesPulmonary HypertensionDesriani Anisa YakubNo ratings yet
- 5. Hemoptysis 讲稿Document4 pages5. Hemoptysis 讲稿mirabel IvanaliNo ratings yet
- Respiratory Diseases ExplainedDocument7 pagesRespiratory Diseases Explainedjon0725No ratings yet
- Asessemnt of Lower Respiratory 506Document4 pagesAsessemnt of Lower Respiratory 506هدوء النسمةNo ratings yet
- Cor Pulmonale by Prof. Dr. Rasheed Abd El Khalek M. DDocument45 pagesCor Pulmonale by Prof. Dr. Rasheed Abd El Khalek M. DvaishnaviNo ratings yet
- Wardclass-Cardiac Tamponade and Pleural EffusionDocument13 pagesWardclass-Cardiac Tamponade and Pleural EffusionCyrusNo ratings yet
- 15 - Approach To Pleural EffusionDocument48 pages15 - Approach To Pleural EffusionBhanu KumarNo ratings yet
- Systemic Disorders of The LungDocument74 pagesSystemic Disorders of The Lungjhay-r reyesNo ratings yet
- Classification of Respiratory FailureDocument8 pagesClassification of Respiratory Failurerau_rauNo ratings yet
- Lungs 3Document60 pagesLungs 3Surya L KNo ratings yet
- Pe in HospitalDocument5 pagesPe in HospitalAbdiaziz WalhadNo ratings yet
- Signs, Causes and Treatment of Pleural EffusionsDocument4 pagesSigns, Causes and Treatment of Pleural EffusionsJvspapa ShilohNo ratings yet
- BronchiectasisDocument6 pagesBronchiectasisdrpaviNo ratings yet
- Disorders of Pleura: Diagnosis and TreatmentDocument32 pagesDisorders of Pleura: Diagnosis and TreatmentnikhilNo ratings yet
- CorpulmonalefinalDocument37 pagesCorpulmonalefinalRay ReyesNo ratings yet
- Risk Factors, Med and NSG MGTDocument5 pagesRisk Factors, Med and NSG MGTHania PolangiNo ratings yet
- Respiration CH 43.Dr SarahDocument59 pagesRespiration CH 43.Dr Sarahaiman siddiquiNo ratings yet
- Non-Cardiogenic Pulmonary EdemaDocument7 pagesNon-Cardiogenic Pulmonary EdemadarmariantoNo ratings yet
- Acute Pulmonary ThromboembolismDocument37 pagesAcute Pulmonary ThromboembolismОльга КоваленкоNo ratings yet
- PleurisyDocument41 pagesPleurisyNishan SubediNo ratings yet
- PleuritisDocument48 pagesPleuritisMuhammad FhaliqNo ratings yet
- Acute Dyspnoea and Haemoptysis My Notes Add Jimmy's PDF Notes On & OrganiseDocument171 pagesAcute Dyspnoea and Haemoptysis My Notes Add Jimmy's PDF Notes On & OrganisewwwrgrobinNo ratings yet
- Massive Hemoptysis: Resident Grand RoundsDocument7 pagesMassive Hemoptysis: Resident Grand RoundsEko CahyonoNo ratings yet
- Metod Terapiya Lechebnoe Delo Fakul'tet Inostranyx Studentov-006Document29 pagesMetod Terapiya Lechebnoe Delo Fakul'tet Inostranyx Studentov-006Nishani SatiyaseelanNo ratings yet
- Approach to a Patient with Haemoptysis and Normal Chest X-RayDocument9 pagesApproach to a Patient with Haemoptysis and Normal Chest X-Raydoc_next_doorNo ratings yet
- Hemoptysis Causes and TreatmentDocument27 pagesHemoptysis Causes and TreatmentRuby FirdausNo ratings yet
- Washing Machine: Owner'S ManualDocument84 pagesWashing Machine: Owner'S ManualAtikah PurnamasariNo ratings yet
- Washing Machine: Owner'S ManualDocument84 pagesWashing Machine: Owner'S ManualAtikah PurnamasariNo ratings yet
- W2.1.20210117.76 2Document1 pageW2.1.20210117.76 2Atikah PurnamasariNo ratings yet
- SafariDocument13 pagesSafariAtikah PurnamasariNo ratings yet
- Miss Atikah Purnamasari SuaibDocument2 pagesMiss Atikah Purnamasari SuaibAtikah PurnamasariNo ratings yet
- W2.2.20200824.36 2Document1 pageW2.2.20200824.36 2Atikah PurnamasariNo ratings yet
- Marhaban Ya RamadhanDocument1 pageMarhaban Ya RamadhanAtikah PurnamasariNo ratings yet
- Washing Machine: Owner'S ManualDocument84 pagesWashing Machine: Owner'S ManualAtikah PurnamasariNo ratings yet
- W2.2.20200824.36 2Document1 pageW2.2.20200824.36 2Atikah PurnamasariNo ratings yet
- W2.2.20200824.36 2Document1 pageW2.2.20200824.36 2Atikah PurnamasariNo ratings yet
- 18 Heartpart1 Basiccongestiveheartfailure 110919083613 Phpapp01Document43 pages18 Heartpart1 Basiccongestiveheartfailure 110919083613 Phpapp01Atikah PurnamasariNo ratings yet
- W2 3 20211022 76Document1 pageW2 3 20211022 76Atikah PurnamasariNo ratings yet
- Nonsurgical management of extradural hematomas in childrenDocument14 pagesNonsurgical management of extradural hematomas in childrenAtikah PurnamasariNo ratings yet
- Temporal Lobe 2Document7 pagesTemporal Lobe 2Atikah PurnamasariNo ratings yet
- Casereport KLP 4Document31 pagesCasereport KLP 4Atikah PurnamasariNo ratings yet
- OksigenDocument56 pagesOksigenAtikah PurnamasariNo ratings yet
- Sustainable Cities and Society: Malek Al-ChalabiDocument4 pagesSustainable Cities and Society: Malek Al-ChalabiAtikah PurnamasariNo ratings yet
- Absen Kelompok 4 B 23/01/2018: NIM Tanda TanganDocument1 pageAbsen Kelompok 4 B 23/01/2018: NIM Tanda TanganAtikah PurnamasariNo ratings yet
- Manual CSL-Medicolegal - 2 Wound Description02Document12 pagesManual CSL-Medicolegal - 2 Wound Description02Atikah PurnamasariNo ratings yet
- Journal 1 UrologyDocument8 pagesJournal 1 UrologyAtikah PurnamasariNo ratings yet
- Ds Sindroma Nefrotik EditedDocument46 pagesDs Sindroma Nefrotik EditedAtikah PurnamasariNo ratings yet
- Terapi Oksigen KPPIKDocument42 pagesTerapi Oksigen KPPIKAtikah PurnamasariNo ratings yet
- Advanced Trauma Life SupportDocument34 pagesAdvanced Trauma Life SupportAtikah PurnamasariNo ratings yet
- CHF Guidelines EscDocument85 pagesCHF Guidelines EscAtikah PurnamasariNo ratings yet
- ACPA - Resource - Guide - 2015 - Final Edited PDFDocument135 pagesACPA - Resource - Guide - 2015 - Final Edited PDFAtikah PurnamasariNo ratings yet
- Nerve Injury Repair and Healing GuideDocument34 pagesNerve Injury Repair and Healing GuideAtikah PurnamasariNo ratings yet
- Heart Failure 2Document12 pagesHeart Failure 2Atikah PurnamasariNo ratings yet
- Sika Grout 214 (HE)Document3 pagesSika Grout 214 (HE)aselabollegalaNo ratings yet
- Stretching - Inservice - Final Eddie PizzoDocument18 pagesStretching - Inservice - Final Eddie PizzoMatthew PuglieseNo ratings yet
- AMRUT Mission for Indian CitiesDocument7 pagesAMRUT Mission for Indian CitiesPragya ChattreeNo ratings yet
- Pharmacology of The GITDocument31 pagesPharmacology of The GITmarviecute22No ratings yet
- EXPAREL Prescribing InformationDocument17 pagesEXPAREL Prescribing InformationcignalNo ratings yet
- Painting Pictures of Success Initiates Inner Process of ElevationDocument57 pagesPainting Pictures of Success Initiates Inner Process of ElevationrerenNo ratings yet
- Effect of Plyometric Exercise Depth Jump and Knee Tuck Jump To The Result A Far Kick Athlete Football Player at SMP Negeri 2 Kasihan, BantulDocument2 pagesEffect of Plyometric Exercise Depth Jump and Knee Tuck Jump To The Result A Far Kick Athlete Football Player at SMP Negeri 2 Kasihan, BantuladamNo ratings yet
- Li2021 - COVID-19 - Performance Study of Microplastic Inhalation Risk Posed by Wearing MasksDocument9 pagesLi2021 - COVID-19 - Performance Study of Microplastic Inhalation Risk Posed by Wearing MasksStepan81No ratings yet
- Adverse Effects of Points AcupunctureDocument2 pagesAdverse Effects of Points AcupunctureGermán Mariano Torrez GNo ratings yet
- Fetal Therapy: Hyaline Membrane DiseaseDocument5 pagesFetal Therapy: Hyaline Membrane DiseaseDelphy VargheseNo ratings yet
- Supportive Care in Clinical ToxicologyDocument13 pagesSupportive Care in Clinical ToxicologyKausal VermaNo ratings yet
- Mga OorderinDocument7 pagesMga OorderinMary Ann Tobias VeraNo ratings yet
- An Abusive Father and The Effects On A Young WomanDocument2 pagesAn Abusive Father and The Effects On A Young WomanJennalyn CasapaoNo ratings yet
- More Volume Is Not Always BetterDocument48 pagesMore Volume Is Not Always BetterGuyNo ratings yet
- Admission and Discharge of A Client in Psychiatric UnitDocument18 pagesAdmission and Discharge of A Client in Psychiatric UnitMahipal singh pacharNo ratings yet
- A Suggested Protocol For The Endocrine Postoperative Management of Patients Undergoing Pituitary SurgeryDocument11 pagesA Suggested Protocol For The Endocrine Postoperative Management of Patients Undergoing Pituitary Surgerymiguel saba sabaNo ratings yet
- Epsom MapDocument1 pageEpsom Mapandrewmmwilmot0% (1)