Professional Documents
Culture Documents
00530-DEC Medical Protocol
Uploaded by
losangeles0 ratings0% found this document useful (0 votes)
26 views2 pagesThis document outlines medical protocols for assessing the health and welfare of children found at methamphetamine labs. It provides guidelines for an initial field medical assessment, immediate care if needed, a baseline exam within 24 hours, an initial follow-up visit within 30 days, and ongoing follow-up care. The protocols aim to evaluate children's general health, screen for potential toxic exposures, ensure medical and developmental monitoring, and facilitate coordination between medical, legal, and child welfare teams responding to these situations.
Original Description:
Original Title
00530-DEC%20Medical%20Protocol
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document outlines medical protocols for assessing the health and welfare of children found at methamphetamine labs. It provides guidelines for an initial field medical assessment, immediate care if needed, a baseline exam within 24 hours, an initial follow-up visit within 30 days, and ongoing follow-up care. The protocols aim to evaluate children's general health, screen for potential toxic exposures, ensure medical and developmental monitoring, and facilitate coordination between medical, legal, and child welfare teams responding to these situations.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views2 pages00530-DEC Medical Protocol
Uploaded by
losangelesThis document outlines medical protocols for assessing the health and welfare of children found at methamphetamine labs. It provides guidelines for an initial field medical assessment, immediate care if needed, a baseline exam within 24 hours, an initial follow-up visit within 30 days, and ongoing follow-up care. The protocols aim to evaluate children's general health, screen for potential toxic exposures, ensure medical and developmental monitoring, and facilitate coordination between medical, legal, and child welfare teams responding to these situations.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Medical Protocols for Children Found at Methamphetamine Labs
#1 FIELD MEDICAL ASSESSMENT PROTOCOL #3 BASELINE ASSESSMENT PROTOCOL
The field medical assessment is done to determine whether children discovered The baseline assessment exam needs to be done within 24 hours of
at the scene of a methamphetamine laboratory discovery are in need of a lab discovery to ascertain a child’s general health status. Prompt
emergency medical care. Medically trained personnel (e.g. EMT or paramedic) medical assessment is warranted due to the risk of toxicologic,
must do the assessment. If no medical personnel are available on-site, the child neurologic, respiratory, dermatologic, or other adverse affects of
must be seen at a medical facility. In either case, a medical assessment should methamphetamine lab chemical and/or stimulant or other drug
be done for each child within 2 hours of discovering children at a exposure, and the high risk of neglect/abuse.
methamphetamine lab site.
#3 STEPS
#1 STEPS 1. Obtain child’s medical history by calling parents directly for the
1. For child with obvious injury or illness, call 911 or other emergency information, or, if impossible, seek information from social
number. workers who have taken the medical history or from the child’s
2. For all children who are not obviously critical, perform field medical past medical record.
assessment consisting of: 2. Perform complete pediatric physical exam to include as much of
3. Vital signs (temperature, blood pressure, pulse, respirations) the Early Periodic Screening, Detection, and Treatment (EPSDT)
4. Pediatric Triangle of Assessment (Airway, Breathing, Circulation) exam as possible. Pay particular attention to:
5. For life-threatening findings, seek immediate medical attention. (See a. Neurologic screen
Protocol #2) Transport to a facility capable of pediatric emergency response b. Respiratory status
appropriate to findings. 3. Call Poison Control if clinically indicated (800-222-1222).
6. A child’s personal possessions should always be left at lab scene to avoid 4. Required Medical Evaluations
possible chemical/drug contamination in other settings. It is necessary to a. Temperature (otic, rectal, or oral)
remove a child’s clothing, decontaminate the child in a minimally traumatic b. Oxygen saturation levels
manner (such as warm water) and provide clean and appropriate attire prior c. Liver function tests: AST, ALT, Total Bilirubin and Alkaline
to removing them from scene. (The child’s clothing and belongings remain Phosphatase.
at the scene and are bagged as evidence.) d. Kidney function tests: BUN and Creatinine
7. If there are no pressing clinical findings, short-term shelter or other secure e. Electrolytes: Sodium, Potassium, Chloride, and Bicarbonate
placement should be implemented by child welfare personnel. f. Complete Blood Count (CBC)
g. Chest x-ray (AP and lateral)
#2 IMMEDIATE CARE PROTOCOL h. Urinalysis and urine dipstick for blood
Problems requiring immediate care are those that cannot wait 24 hours to be If not done earlier, a urine specimen should be collected.
treated at the baseline exam (discussed in Protocol #3). Immediate care must be This should be done within 12 hours of identification of the
provided as soon as possible after significant health problems are identified. child because some chemicals/drugs are eliminated in a
Care should preferably be provided within 2 hours, but not later than 4 hours short time. Urine screen and confirmatory results should be
after the child is identified at a lab site. Immediate care may be provided in a reported at any detectable level.
hospital emergency room, or pediatric or urgent care facility depending on the Optional Clinical Evaluations
severity/urgency of the problem and the time of day. If a field medical i. Complete metabolic panel (Chem 20 or equivalent)
assessment was not completed (Protocol #1), children should be taken to an j. Pulmonary function tests
immediate care facility within 2 hours for the medical assessment. k. CPK
l. Lead level (on whole blood)
#2 STEPS m. Coagulation studies
1. Perform the field medical assessment (follow Protocol #1 if not already n. Carboxyhemoglobin level
done in the field). 5. Refer for local (county department of social services/law
2. Administer tests and procedures as indicated by clinical findings. A urine enforcement) child abuse and neglect evaluation.
specimen for toxicology screening should be collected from each child 6. Conduct a developmental screen. This is an initial age-
within 12 hours of identification because some chemicals/drugs are appropriate screen, not a full-scale assessment; may need
eliminated in a short time. Use appropriate chain of evidence procedures referral to a pediatric specialist.
and request urine screen and confirmatory test results to be reported at any 7. Provide a mental health screen on all children and crisis
detectable level. intervention services as clinically indicated. These services
3. Call Poison Control if clinically indicated (800-222-1222). require a qualified pediatrician or mental health professional and
4. Follow baseline assessment (see Protocol #3) if appropriate to medical site may require a visit to a separate facility.
and time permitting or schedule baseline assessment exam to be 8. Secure the release of child(ren)’s medical records to involved
completed within 24 hours of lab discovery. agencies including child welfare worker.
5. Secure the release of the child’s medical records to all involved agencies to 9. Note: Child welfare personnel may not have immediate legal
ensure ongoing continuity of care. access to certain health care records. Every effort should be
6. Child welfare personnel should evaluate placement options and implement made to facilitate transfer of medical records, by providing
short-term shelter for the child in which they will be closely observed for information about where, when, and to whom records should be
possible developing symptoms. transferred.
9. For any positive findings, follow-up with appropriate care as necessary. #5 STEPS
ALL children must be provided long-term follow-up care (see Protocol #5) Required Components of Follow-Up Care
using specified schedule. 1. Pediatric Care Visits. The visits should occur according to
10. Long-term shelter and placement options should be evaluated and the American Academy of Pediatrics’ schedule.
implemented by child welfare worker. a. Follow-up of previously identified problems.
b. Perform comprehensive (EPSDT) physical exam and
#4 INITIAL FOLLOW-UP CARE PROTOCOL laboratory examination with particular attention to:
A visit for initial follow-up care occurs within 30 days of the baseline 1) Liver function (repeat panel at first follow-up only
assessment to reevaluate comprehensive health status of the child, identify any unless abnormal)
latent symptoms, and ensure appropriate and timely follow-up of services as the 2) Respiratory function (history of respiratory
child’s care plan and placement are established. If possible, the visit should be problems, asthma, recurrent pneumonia, check for
scheduled late in the 30-day time frame for more valid developmental and clear breath sounds).
mental health results. 3) Neurologic evaluation.
c. Perform full developmental screen.
#4 STEPS d. Perform mental health evaluation (requires a qualified
1. Follow-up of any abnormal baseline test results. mental health professional, pediatrician, licensed
2. Perform developmental examination (using instruments such as the therapist, child psychologist or licensed child mental
Denver, Gesell, and Bayley) as indicated by the developmental screen in health professional).
Protocol #3. 2. Plan follow-up and treatment or adjust existing treatment for
3. Conduct mental health history and evaluation (requires a qualified pediatric any medical problems identified. Medical records should
professional). continue to accompany the child’s course of care.
4. If abnormal findings on any of the above, schedule intervention and follow- 3. Adequacy of child’s shelter/placement situation should be
up as appropriate to the findings; then proceed with long-term follow-up reviewed by child welfare worker and modified as necessary.
protocol (see Protocol #5). If no abnormal findings, schedule visits per long- 4. Plan follow-up strategies for developmental, mental health or
term follow-up protocol (Protocol #5). placement problems identified.
5. Adequacy of child’s shelter/placement situation should be reviewed by child
welfare worker and modified if necessary. Optional Enhancements of Follow-up Care
1. Conduct pediatric care visits including developmental screen
#5 LONG-TERM FOLLOW-UP CARE PROTOCOL and mental health evaluation at 6, 12, and 18 months post-
Long-term follow-up care is designed to 1) monitor physical, emotional, and baseline assessment.
developmental health, 2) identify possible late developing problems related to 2. Conduct home visits by pediatrically trained PHN or other
the methamphetamine environment, and 3) provide appropriate intervention. At nurse, at 3, 9, 15, and 18 months post-baseline assessment.
minimum, a pediatric visit is required 12 months after the baseline Ensure that home visits occur between the pediatric clinic
assessment. Children considered to be Drug Endangered Children (DEC) cases visits until the last visit at 18 months.
should receive follow-up services a minimum of 18 months post identification.
IF YOUR COMMUNITY HAS ADDITIONAL
For further information contact:
Kathryn Wells, MD, FAAP SPECIFIC INSTRUCTIONS AND/OR LOCAL
Medical Director, Denver Family Crisis Center PHONE NUMBERS, AFFIX THE ATTACHED
2929 W. 10th Ave.
Denver, CO 80204
POUCH, INSERT INSTRUCTIONS AND
Phone: (720) 944-3747 – Fax: (720) 944-3710 PLACE IN THIS SPACE
e-mail: kathryn.wells@dhha.org
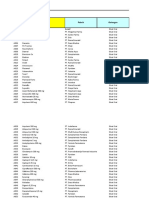
This protocol was modified slightly from the original DEC Protocol that was Color Code of Agency Responsibility:
developed by the DEC Resource Center for the purpose of improving multi- HAZMAT/Law Enforcement/Fire
agency response to children found in clandestine methamphetamine labs. The Emergency Medical Personnel
DEC Resource Center, The Children’s Hospital and The Kempe Children’s
Center disclaim liability for outcomes from use of this protocol or misuse of the Social Services
sequential steps herein. Physicians
You might also like
- Rules and Regulations Implementing R.A. 9288 Otherwise Known As The "Newborn Screening Act of 2004" Important ConceptsDocument2 pagesRules and Regulations Implementing R.A. 9288 Otherwise Known As The "Newborn Screening Act of 2004" Important ConceptsDELLNo ratings yet
- Resource Guide - Model Nbs PolicyDocument7 pagesResource Guide - Model Nbs PolicyagelesswapNo ratings yet
- Postmortem Findings In COVID-19 Patients & Mental Health Issues In The Era Of COVID-19: Clinical Updates in COVID-19From EverandPostmortem Findings In COVID-19 Patients & Mental Health Issues In The Era Of COVID-19: Clinical Updates in COVID-19No ratings yet
- Background : BDH Polices & Procedures On Universal Newborn ScreeningDocument21 pagesBackground : BDH Polices & Procedures On Universal Newborn ScreeningJnana YumnaNo ratings yet
- 5 November 2022 Nurses Program of ExaminationDocument4 pages5 November 2022 Nurses Program of ExaminationDumangeng, Claire G.No ratings yet
- Newborn ScreeningDocument18 pagesNewborn ScreeningKayNo ratings yet
- Otomicroscopy (Adult, Peds)Document4 pagesOtomicroscopy (Adult, Peds)Carmen EneaNo ratings yet
- Physical Examinations I (JoVE)Document119 pagesPhysical Examinations I (JoVE)Thasya RenaNo ratings yet
- Types of AssessmentDocument27 pagesTypes of AssessmentLai KuanlinNo ratings yet
- Wound Debridement (Adult, Neonatal, Peds) PDFDocument4 pagesWound Debridement (Adult, Neonatal, Peds) PDFPangestu KelvinNo ratings yet
- Newborn CompetencyDocument3 pagesNewborn CompetencyGail LeslieNo ratings yet
- Brain Death Protocol - Up PGHDocument18 pagesBrain Death Protocol - Up PGHKristian CadienteNo ratings yet
- Protocol Synopsis Sample Sheet (HW)Document6 pagesProtocol Synopsis Sample Sheet (HW)rockmanx182No ratings yet
- CU 5 Normal Diagnostic and Laboratory FindingsDocument12 pagesCU 5 Normal Diagnostic and Laboratory FindingsIana CastigadorNo ratings yet
- Dictation Discharge Summary TemplateDocument19 pagesDictation Discharge Summary TemplateBobby ReddyNo ratings yet
- Clinical Objectives GuidelinesDocument11 pagesClinical Objectives GuidelinesprowritttersNo ratings yet
- Nicu Discharge GuidelinesDocument8 pagesNicu Discharge Guidelinessophia mendiolaNo ratings yet
- Exam Progam MAY 2022 PNLE (Nursing)Document4 pagesExam Progam MAY 2022 PNLE (Nursing)Victoria Castillo TamayoNo ratings yet
- IN PRC CAR (Baguio City) Philippine Nurse Licensure Examination (Pnle)Document63 pagesIN PRC CAR (Baguio City) Philippine Nurse Licensure Examination (Pnle)PRC BaguioNo ratings yet
- Newborn ScreeningDocument13 pagesNewborn ScreeningACOB, Jamil C.No ratings yet
- Nursing DiagnosisDocument4 pagesNursing DiagnosisAngela SaavedraNo ratings yet
- Revalida ToolDocument12 pagesRevalida ToolShaira SariaNo ratings yet
- Checklist DeliveryDocument3 pagesChecklist DeliveryChristian Paul PerezNo ratings yet
- NCMA219 - W8 - Newborn ScreeningDocument10 pagesNCMA219 - W8 - Newborn ScreeningKayNo ratings yet
- Ethical Issues in Clinical ResearchDocument23 pagesEthical Issues in Clinical ResearchDaxesh PatelNo ratings yet
- Ra 9288 Basis For Questionnaire PDFDocument22 pagesRa 9288 Basis For Questionnaire PDFHolden Mandapat ValdezNo ratings yet
- s006 Animal Health and Environmental SurveillanceDocument7 pagess006 Animal Health and Environmental SurveillanceYogi HerdiansyahNo ratings yet
- New Born ScreeningDocument70 pagesNew Born ScreeningChiro Rouy Malaluan100% (2)
- Bio136 186unit4Document48 pagesBio136 186unit4jhon pauloNo ratings yet
- Micropara FINALSDocument286 pagesMicropara FINALSjhon pauloNo ratings yet
- Paediatric Forensic Medical ExaminationDocument7 pagesPaediatric Forensic Medical ExaminationYwagar YwagarNo ratings yet
- Checklist Newborn Competency 2022Document3 pagesChecklist Newborn Competency 2022みずNo ratings yet
- Diagnostic ProceduresDocument10 pagesDiagnostic Proceduresmc gallegoNo ratings yet
- CHO Pop QuizDocument2 pagesCHO Pop QuizCarloAragon100% (3)
- Clinical ChemistryDocument23 pagesClinical ChemistryRezzy Mae Panadero OraNo ratings yet
- Bone Marrow AspirationDocument6 pagesBone Marrow AspirationSai PardhuNo ratings yet
- Republic of The Philippines Professional Regulation Commission ManilaDocument3 pagesRepublic of The Philippines Professional Regulation Commission ManilaTheSummitExpress0% (1)
- NURSE 07-2021 Room AssignmentDocument118 pagesNURSE 07-2021 Room AssignmentPRC BaguioNo ratings yet
- A. IntroductionDocument24 pagesA. IntroductionAhmad Kurnia SandhiNo ratings yet
- Permethrin Topical Cream RLD 019855 RC08-17Document7 pagesPermethrin Topical Cream RLD 019855 RC08-17Ritesh RastogiNo ratings yet
- Newborn ScreeningDocument22 pagesNewborn ScreeningSirc PatrickNo ratings yet
- Closed Door Coaching Histopat Mtlaws Ethics 2021 PDFDocument5 pagesClosed Door Coaching Histopat Mtlaws Ethics 2021 PDFAnne MorenoNo ratings yet
- Tentative List of Qualified Examinees For The February 3 & 4, 2022 Respiratory Therapists Licensure Examination in Baguio CityDocument9 pagesTentative List of Qualified Examinees For The February 3 & 4, 2022 Respiratory Therapists Licensure Examination in Baguio CityPRC BaguioNo ratings yet
- Guidelines For DischargeDocument30 pagesGuidelines For DischargeJose GiertzNo ratings yet
- How Vaccines Are MadeDocument37 pagesHow Vaccines Are MadeMary_Spiro67% (3)
- Valoración PreanestesicaDocument5 pagesValoración PreanestesicaSebastian Hdez BolañosNo ratings yet
- Research ReportDocument13 pagesResearch ReportAllza AllNo ratings yet
- Clinical ObjectivesDocument1 pageClinical ObjectivesMuhammad AdilNo ratings yet
- CebuDocument201 pagesCebusantosmauriceleeNo ratings yet
- Current Standard Operating ProcedureDocument3 pagesCurrent Standard Operating ProcedureRhu LibonNo ratings yet
- Clinic Flow P&PDocument2 pagesClinic Flow P&Psahar hussinNo ratings yet
- Introduction NNUDocument3 pagesIntroduction NNUZuna QaziNo ratings yet
- Efikasi AzitromisinDocument4 pagesEfikasi AzitromisinNadia DesiNo ratings yet
- Schedule y PPT EDITTED ONEDocument38 pagesSchedule y PPT EDITTED ONEKesetha100% (2)
- Removal of External Ventricular Drainage Catheter or Intracranial Pressure Device (Adult, Peds)Document4 pagesRemoval of External Ventricular Drainage Catheter or Intracranial Pressure Device (Adult, Peds)Dot DitNo ratings yet
- PMLS Lesson 4Document3 pagesPMLS Lesson 4Void MelromarcNo ratings yet
- 2 Mod Issue Brief Finalupdatedlogo Policy Oct2017 SMDocument2 pages2 Mod Issue Brief Finalupdatedlogo Policy Oct2017 SMJohnryl FranciscoNo ratings yet
- NURSING PROCEDURES FOR CHN Converted 1Document25 pagesNURSING PROCEDURES FOR CHN Converted 1Genki Fay B. Lequigan100% (1)
- Omb Bulletin No. 06-01Document2 pagesOmb Bulletin No. 06-01losangeles100% (1)
- 02358-b04-02 Supp1Document7 pages02358-b04-02 Supp1losangelesNo ratings yet
- Executive Office of The President Executive Office of The PresidentDocument4 pagesExecutive Office of The President Executive Office of The Presidentlosangeles100% (1)
- 02368-b06-01 CorrectionDocument1 page02368-b06-01 Correctionlosangeles100% (1)
- 02359-b04-03 AppendixDocument146 pages02359-b04-03 AppendixlosangelesNo ratings yet
- Executive Office of The PresidentDocument23 pagesExecutive Office of The Presidentlosangeles100% (1)
- Executive Office of The President Executive Office of The PresidentDocument13 pagesExecutive Office of The President Executive Office of The Presidentlosangeles100% (1)
- b04 04Document16 pagesb04 04losangeles100% (1)
- Executive Office of The President: Attachment BDocument5 pagesExecutive Office of The President: Attachment Blosangeles100% (1)
- 02360-b04-03 AttachmentDocument5 pages02360-b04-03 AttachmentlosangelesNo ratings yet
- Major Savings and Reforms in The President's 2008 Budget: EbruaryDocument211 pagesMajor Savings and Reforms in The President's 2008 Budget: EbruarylosangelesNo ratings yet
- Bulletin No. 00 - 03 To The Heads of Executive Departments and Establishments SubjectDocument13 pagesBulletin No. 00 - 03 To The Heads of Executive Departments and Establishments SubjectlosangelesNo ratings yet
- Executive Office of The PresidentDocument20 pagesExecutive Office of The PresidentlosangelesNo ratings yet
- 02352-b03-04 AttachDocument141 pages02352-b03-04 AttachlosangelesNo ratings yet
- Executive Office of The President: What Are The Legal Authorities Under Which OMB Is Requiring Agency Action?Document3 pagesExecutive Office of The President: What Are The Legal Authorities Under Which OMB Is Requiring Agency Action?losangelesNo ratings yet
- Executive Office of The President Executive Office of The PresidentDocument5 pagesExecutive Office of The President Executive Office of The PresidentlosangelesNo ratings yet
- Attachment BDocument4 pagesAttachment BlosangelesNo ratings yet
- 02338-Expanding Egov 2005Document12 pages02338-Expanding Egov 2005losangelesNo ratings yet
- SpecDocument424 pagesSpeclosangelesNo ratings yet
- Director Rob Portman February 5, 2007Document8 pagesDirector Rob Portman February 5, 2007losangelesNo ratings yet
- Program Assessment Rating Tool (PART) 2008 Budget: This PDF Is Also Available in Excel Format atDocument31 pagesProgram Assessment Rating Tool (PART) 2008 Budget: This PDF Is Also Available in Excel Format atlosangelesNo ratings yet
- Object Class Analysis: Budget of The U.S. GovernmentDocument128 pagesObject Class Analysis: Budget of The U.S. GovernmentlosangelesNo ratings yet
- TreasuryDocument4 pagesTreasurylosangelesNo ratings yet
- HistDocument336 pagesHistlosangeles100% (1)
- Department of Transportation: Since 2001, The AdministrationDocument5 pagesDepartment of Transportation: Since 2001, The AdministrationlosangelesNo ratings yet
- CLSI Laboratory Documents Development and Control Approved Guideline NAT L COMM CLINICAL LAB STANDARDS 2006 PDFDocument100 pagesCLSI Laboratory Documents Development and Control Approved Guideline NAT L COMM CLINICAL LAB STANDARDS 2006 PDFErvin RodriguezNo ratings yet
- (ISPS Book Series) Yrjö O. Alanen, Manuel González de Chávez, Ann-Louise S. Silver, Brian Martindale - Psychotherapeutic Approaches To Schizophrenic Psychoses - Past, Present and Future-Routledge (20Document419 pages(ISPS Book Series) Yrjö O. Alanen, Manuel González de Chávez, Ann-Louise S. Silver, Brian Martindale - Psychotherapeutic Approaches To Schizophrenic Psychoses - Past, Present and Future-Routledge (20Manuel100% (1)
- IS 4049-Part-IDocument5 pagesIS 4049-Part-ISrinivas KadivetiNo ratings yet
- Om Deutz 1013 PDFDocument104 pagesOm Deutz 1013 PDFEbrahim Sabouri100% (1)
- Learning Guide No 5Document19 pagesLearning Guide No 5Menal JemalNo ratings yet
- Wire Rope Inspection ProgramDocument2 pagesWire Rope Inspection Programسيد جابر البعاجNo ratings yet
- Region Iii - Central Luzon Padapada National High SchoolDocument2 pagesRegion Iii - Central Luzon Padapada National High SchoolRotipNo ratings yet
- Microbes in Human Welfare PDFDocument2 pagesMicrobes in Human Welfare PDFshodhan shettyNo ratings yet
- Plasma Arc Machining (Pam) : Mechanical Engineering Department I.I.T Guwahati-781039 E-Mail: Manasdas@iitg - Ernet.inDocument15 pagesPlasma Arc Machining (Pam) : Mechanical Engineering Department I.I.T Guwahati-781039 E-Mail: Manasdas@iitg - Ernet.inSrinivasanNo ratings yet
- Withania DSC PDFDocument6 pagesWithania DSC PDFEfsha KhanNo ratings yet
- Krispy Kreme Doughnut Recipe - Immaculate BitesDocument2 pagesKrispy Kreme Doughnut Recipe - Immaculate Bitesdaisydrops6No ratings yet
- Occlusal Appliance TherapyDocument14 pagesOcclusal Appliance TherapyNam BuiNo ratings yet
- Poverty and Children's Personal RelationshipsDocument87 pagesPoverty and Children's Personal RelationshipsJoe OgleNo ratings yet
- BlahDocument8 pagesBlahkwood84100% (1)
- B737-800 Air ConditioningDocument7 pagesB737-800 Air ConditioningReynaldoNo ratings yet
- 1Manuscript-BSN-3y2-1A-CEDILLO-222 11111Document32 pages1Manuscript-BSN-3y2-1A-CEDILLO-222 11111SHARMAINE ANNE POLICIOSNo ratings yet
- Photosynthesis PastPaper QuestionsDocument24 pagesPhotosynthesis PastPaper QuestionsEva SugarNo ratings yet
- Tryout Consent Form - 2014 - Sign and ReturnDocument2 pagesTryout Consent Form - 2014 - Sign and ReturnSanjeevan BaraNo ratings yet
- The Mental MeltdownDocument5 pagesThe Mental Meltdownapi-460020991No ratings yet
- Airport - WikipediaDocument109 pagesAirport - WikipediaAadarsh LamaNo ratings yet
- Demolition/Removal Permit Application Form: Planning, Property and Development DepartmentDocument3 pagesDemolition/Removal Permit Application Form: Planning, Property and Development DepartmentAl7amdlellahNo ratings yet
- EESC 111 Worksheets Module 5Document5 pagesEESC 111 Worksheets Module 5Keira O'HowNo ratings yet
- 2nd Term Study Guide 4th Grade Feb 2024 Cambridge ObjectivesDocument8 pages2nd Term Study Guide 4th Grade Feb 2024 Cambridge Objectivessofi.cardenas1968No ratings yet
- 5070 s14 QP 11Document16 pages5070 s14 QP 11OsamaRahimNo ratings yet
- Baxshin LABORATORY: Diagnostic Test and AnalysisDocument1 pageBaxshin LABORATORY: Diagnostic Test and AnalysisJabary HassanNo ratings yet
- HSN-Lube 2007 PDFDocument45 pagesHSN-Lube 2007 PDFCecilio Valderrama100% (3)
- LYON Conditions of Secondment 3500EUR enDocument4 pagesLYON Conditions of Secondment 3500EUR enabdu1lahNo ratings yet
- Celitron ISS 25L - Product Spec Sheet V 2.1 enDocument9 pagesCelitron ISS 25L - Product Spec Sheet V 2.1 enyogadwiprasetyo8_161No ratings yet
- Industrial Visit ReportDocument8 pagesIndustrial Visit ReportAnuragBoraNo ratings yet
- Data Obat VMedisDocument53 pagesData Obat VMedismica faradillaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (34)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIFrom EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIRating: 4 out of 5 stars4/5 (20)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4.5 out of 5 stars4.5/5 (6)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)