Professional Documents
Culture Documents
Bonviva: The Novel Therapeutic Drug For Osteoporosis
Uploaded by
David Cahyo WibisonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bonviva: The Novel Therapeutic Drug For Osteoporosis
Uploaded by
David Cahyo WibisonoCopyright:
Available Formats
1
Bonviva : the Novel Therapeutic Drug for Osteoporosis
(A Highly Efficacious and Well Tolerated Ibandronate-150mg Once Monthly)
2008
11-752
Askandar Tjokroprawiro
Diabetes and Nutrition Center Dr.Soetomo Teaching Hospital
Airlangga University School of Medicine, Surabaya
AN OVERVIEW : FOCUS ON ONCE MONTHLY ORAL IBANDRONATE
In clinical practice, the most frequent types of osteoporosis can be categorized
into 3 types, such as: type I- osteoporosis (postmenopausal osteoporosis or PMO), type
II- osteoporosis (age-related osteoporosis or ARO), and type III-osteoporosis
(corticosteroid-induced osteoporosis or CIO).
Diabetic osteopenia and osteoporosis become major issues in daily clinical
experiences. Recent studies indicated that the probable causes of diabetic osteopenia can
be suggested and can be explained follows: AGE-modified collagen affected osteoblastic
cell differentiation and function, and this process could be responsible for osteopenia-
osteoporosis (especially in postmenopouse) in patients with diabetes mellitus.
The Treatment Update of osteoporosis can also be grouped into three
interventions: Healthy Lifestyle for osteoporosis. Prevention: Calcium Supplement 1-
1.5 g/day, and Drugs: Estrogen, Bisphosphonates, Calcitonin, Growth Hormone, SERMs,
Strontium Ranelate (SR), Vitamin D, Fluoride, PTH-PTHRP, and Symptomatic (Lumbar
Support etc).
Bisphosphonates continue to be used in treating Pagets disease and
hypercalcemia in malignancy, but new uses of drugs include prevention of
postmenopause osteoporosis, age-related osteoporosis, corticosteroid-induced
osteoporosis, and post-transplantation bone loss, and to decrease bone pain and to inhibit
of bone metastases in cancer patients. The bisphosphonates investigated in humans,
numbered in increasing order of potency can be abbreviated as E-TCP-NAORIZ-MICE:
Etidronate Tiludronate, Clodronate, Pamidronate Neridronate, Alendronate,
Olpadronate, Risedronate, Ibandronate, Zoledronate Minodronate, Incadronate,
Cimadronate, EB-1053.
Abbreviations: ACE = annual cumulative response; BALTO = bonviva alendronate trial in osteoporosis; BMD = bone
mineral density; BMF = bone marker feedback; BMS = bone material and structure; BonAdAsia = Bonviva Adherence
in Asia; BONE = ibandronate Osteoporosis in vertebral fractures in North America and Europe; BonAdAsia = BTO =
bone turn over; DIVA = dosing intra venous administration; E-TCP-NAORIZ-MICE = Etidronate Tiludronate,
Clodronate, Pamidronate Neridronate, Aledronate, Olpadronate, Risedronate, Ibandronate, Zoledronate
Minodronate, Incadronate, Cimadronate, EB-1053; FIT = fracture intervention trial; MOBILE-LTE = Monthly Oral
ibandronate In LadiEs Long Term Extension; NVFs = non-vertebral fractures; PERSIST = PERsistance Study of
Ibandronate versus alendronaTe; sCTX = serum C-telopeptide of the -chain type-1 collagen; VERT-NA = vertebral
efficacy with risedronate therapy North American; VFs = vertebral fractures.
MORNING SYMPOSIUM ON OSTEOPOROSIS
Annual Meeting of Rheumatology & Indonesian Autoimmunity Course
Jakarta, 17-20 April 2008
2
Alendronate, Risedronate and Ibandronate (most recently) have been available in
Indonesia. The novel bisphosphonate, ibandronate, shows 2-fold more potent than
risedronate, and 10.000 fold than etidronate.
Bisphosphonates have been reported successfully in preventing (prevention
effects) the bone loss in osteoporosis and have resulted in lowered fracture incidence
(treatment effects). Ibandronate is a potent nitrogen-containing bisphosphonates. It has a
strong affinity for bone mineral and potently inhibits osteoclast-mediated bone resorption.
Ibandronate is effective for the treatment of hypercalcemia of malignancy, metastatic
bone disease, postmenopausal osteoporosis, corticosteroid-induced osteoporosis, and
Pagets disease.
The target of osteoporosis treatment in the prevention of all fracture types
including both vertebral fractures (VFs) and non-vertebral fractures (NVFs). While VF is
the most common osteoporotic fracture type, NVFs, such as those of the hip, can be the
most debiliting and costly.
Several clinical trials oral bisphosphonates (including alendronate, risedronate
and ibandronate) have shown that daily bisphosphonate therapy increases bone mineral
density (BMD), reduces bone turnover (BTO), and reduces the risk of fractures in women
with postmenopause osteoporosis. The 3 (three) main components of bone strength are
BMD, BTO, and micro architecture and collagen of the bone (BMS).
To date, however, there are no prospective studies investigating the antifracture
efficacy of approved weekly, monthly, or quarterly bisphosphonate treatment.
The results of meta-analysis (included 8710 patients) of phase-III studies on
ibandronate (BONE, IV Fracture Prevention, MOBILE, and DIVA) and the risk of NVFs
and clinical fractures in women with postmenopausal osteoporosis were recently reported
in 2008. The marketed doses of ibandronate, 150mg once-monthly oral (Bonviva) and 3
mg quarterly intravenous (IV) injection, produce greater increases in lumbar spine BMD
than treatment with the 2.5mg oral daily dose. This meta-analysis assessed whether such
doses also reduce fracture risk relative to placebo.
Monthly oral ibandronate (Bonviva) reduces bone resorption (sCTX) within 3
months, and significantly increases lumbar spine and proximal femur BMD. Thus,
monthly oral ibandronate significantly increases BMD and significantly suppresses BTO.
Intermittent bisphosphonate regimens require higher cumulative doses in order to
achieve equal effect on BMD and BTO markers (annual cumulative response = ACE of
Bonviva : 10.8 mg, whereas for I.V 3 mg ibandronate: 12 mg).
Intermittent oral and I.V injection in doses of ibandronate have demonstrated
significant gains in BMD and similar reductions in BTO markers versus daily
ibandronate. Once-150mg monthly and 3mg I.V quarterly ibandronate show ACE 10.8mg
and ACE 12mg, respectively; both regimens have been investigated. Total dose concept :
lessons from studies with ibandronate showed that ACE of an intermittent ibandronate
regimen should be approximately 11mg.
Recent studies concluded that antifracture efficacy is highly predicted by BMD
and BTO, and also BMS (bone material and structure). BONE study demonstrated that
monthly oral ibandronate preserves trabecular micro-architecture (BMS).
Conclusions Once-monthly oral ibandronate (Bonviva) shows 3 (three)
important functions (BMD, BTO, BMS) which favor bone strength to increase
antifracture efficacy or fracture resistance.
3
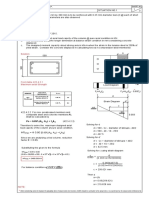
Based on annual cumulative exposure (ACE) such 4 (four) studies previously
mentioned (BONE, I.V fracture prevention, MOBILE, and DIVA) were grouped into 3
(three) dose levels.
Annual cumulative response (ACE) was defined as the annual dose (mg) x
bioavailability (0.6%, oral; 100%, IV) or placebo.
Six key NVFs (clavicle, humerus, wrist, pelvis, hip, and leg), all NVFs, and all
clinical fractures were examined.
The meta-analysis revealed that the high-dose group (ACE > 10.8mg) showed
significant reductions in the adjusted RR of (relative to placebo): key NVFs 34.4%, p =
0.032; all NVFs 29.9%, p = 0.041; clinical fracture 28.8%, p = 0.010). The high-dose
group also had significantly longer time to fracture versus placebo for key NVFs (p =
0.031), all NVFs (p = 0.025), and clinical fractures (p = 0.002).
The most recent study on the adherence of patients to the Bonviva therapeutic
regimen in Asia (BonAdAsia Study 2008, n = 596) reported the results which can be
summarized and listed below.
1. Patients: 94.6% adherent and 5.7% non-adherent patients.
2. The sCTX levels decreased significantly over time (each with p < 0.0001) over
the 3-month (50.1%) and the 6-month (51.2%) study periods.
3. Study safety profile (n = 590) : 41.1% of the patients had adverse events (87.1%
were mild, with 36.6% gastrointestinal and 29.6% muscoluskeletal. Of its are non
serious adverse events.
Conclusions Bonviva significantly decreased the sCTX, with favorable safety profile.
Patients were adherent to Bonviva intake regardless of bone marker feedback (BMF)
On the basis of the results of several studies, such as BALTO, BONE, MOBILE,
MOBILE-LTE, PERSIST, BonAdAsia, and others, which provide the efficacy and the
safety of Bonviva (150 mg ibandronate, once-monthly) as the novel therapeutic
regimen in the treatment of osteoporosis, the conclusion below is made.
Besides, the results of the below listed studies and reports support the efficacy and
tolerability of monthly oral ibandronate (Bonviva) therapy.
1. Monthly oral 150 mg ibandronate provides consistent gains in BMD after 3 years
or treatment (2 years in MOBILE plus 1 year in MOBILE-LTE) with a tolerability
profile similar to the daily regimen.
2. The MOBILE-LTE study revealed progressive improvements in efficacy with oral
150mg ibandronate when administered monthly.
3. Rapid suppression of serum CTX (sCTX) within 3 (three) days of treatment
initiation with monthly oral 150 mg ibandronate.
4. MOBILE-LTE results: Median sCTX levels remained within the premenopausal
range after 3 years and were reduced by 52.0% (100mg arm) and 64.9% (150 mg
arm) compared with the MOBILE study baseline.
5. A meta-analysis of individual patients data showed significant reduction in non-
vertebral fracture will high-versus low-dose ibandronate.
6. Monthly oral ibandronate preserves trabecular micro-architecture: micro-
computed tomography findings from the BONE study.
7. Ibandronate-induced reduction of bone turnover marker predicts antifracture
efficacy. Bone strength = BMD + BTO + Bone microarchitecture structure.
8. Ibandronate-induced BMD gains are related to vertebral antifracture efficacy.
4
9. The data show that 150 mg monthly ibandronate provides consistent gains in
BMD in postmenopausal women with osteoporosis. This evidence, plus the
favorable tolerability profile and greater persistence with monthly ibandronate
versus weekly regiments support the clinical benefits.
10. Conclusion of the BALTO study: significantly more women with PMO preferred
once-monthly 150 mg ibandronate therapy to once-weekly alendronate therapy,
and found the once-monthly regimen to be more convenient.
Taken together (not comparative study), RRR (%) for the new vertebral fracture at 3
years, Bonviva 2.5 mg/day (BONE study, RRR 62%) is superior than alendronate 5-10
mg/day (FIT, 47%) and risedronate 5 mg/day (VERT-NA, 41%). For non-vertebral
fracture efficacy in high-risk patients, ibandronate showed 69% RRR.
Conclusions Ibandronate is a potent 3rd generation nitrogen-containing
bisphosphonate. This novel bisphosphonate shows twice fold more potent than
risedronate, and ten fold more potent than alendronate. This drug has shown its high
efficacy to increase BMD, to reduce BTO, to improve BMS, and to reduce the risk of
vertebral fractures (RRR 62%) in PMO; for non-vertebral fracture, ibandronate showed
69% RRR. The MOBILE study long term extension (MOBILE-LTE) has demonstrated
the progressive improvements in efficacy with 150mg oral ibandronate (Bonviva) when
administered once monthly. Bonviva at dose level of ACE > 10.8 mg, the marketed 150
mg once-monthly oral, shows highly efficacious and well tolerated bisphosphonate.
Bonviva may provide significant vertebral and non-vertebral and clinical efficacy;
patients will be more convenience and have more quality of life while taking once
monthly ibandronate than daily or weekly bisphosphonate.
-oOo-
You might also like
- RTL Surabaya-Workshop EnumeratorDocument18 pagesRTL Surabaya-Workshop EnumeratorDavid Cahyo WibisonoNo ratings yet
- Ask - 0812Document11 pagesAsk - 0812David Cahyo WibisonoNo ratings yet
- Ask - 0804iDocument15 pagesAsk - 0804iDavid Cahyo WibisonoNo ratings yet
- BacLink 2.excel, Text Files, Other ApplicationsDocument35 pagesBacLink 2.excel, Text Files, Other Applicationsvn_ny84bio021666No ratings yet
- Makalah DiabetesDocument16 pagesMakalah DiabetesDavid Cahyo WibisonoNo ratings yet
- Infection or InflammationDocument7 pagesInfection or InflammationDavid Cahyo WibisonoNo ratings yet
- Inflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDocument26 pagesInflammation: Inflammation Is A Protective Response, The Goal of Which Is To EliminateDavid Cahyo WibisonoNo ratings yet
- Resistensi AntibiotikaDocument55 pagesResistensi AntibiotikaDavid Cahyo WibisonoNo ratings yet
- Periodontal (Gum) Disease - Dentist Delray Beach, FL - Dental Education LibraryDocument3 pagesPeriodontal (Gum) Disease - Dentist Delray Beach, FL - Dental Education LibraryDavid Cahyo WibisonoNo ratings yet
- Oral Biomarkers in The Diagnosis and Progression of Periodontal PDFDocument8 pagesOral Biomarkers in The Diagnosis and Progression of Periodontal PDFAmrí David BarbozaNo ratings yet
- Nature Publishing Group PDFDocument11 pagesNature Publishing Group PDFDavid Cahyo WibisonoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Group 3 Safety Issues in ICTDocument15 pagesGroup 3 Safety Issues in ICTRoseAnnNo ratings yet
- Toaz - Info Super Coolant Af Nac PRDocument6 pagesToaz - Info Super Coolant Af Nac PRsugi yantoNo ratings yet
- Step-by-Step Planning for Escalators and Moving WalksDocument21 pagesStep-by-Step Planning for Escalators and Moving WalksYusup SNo ratings yet
- To Study The Open Circuit/Core Losses of Single Phase TransformerDocument5 pagesTo Study The Open Circuit/Core Losses of Single Phase TransformerTanzeel UR RehmanNo ratings yet
- Easytronic Micro II 28 05 2010 08 35 20 Revision 05 Controller 1 PDFDocument10 pagesEasytronic Micro II 28 05 2010 08 35 20 Revision 05 Controller 1 PDFСергей Заика100% (1)
- JW1782BDocument13 pagesJW1782BGustavo AlonsoNo ratings yet
- Learning Activity Sheet In: Computer Systems ServicingDocument12 pagesLearning Activity Sheet In: Computer Systems ServicingCarvalds 0315No ratings yet
- HYBRIFLEX® RRH Hybrid Cable Solution 12 X 24, 6AWG, Low-Inductance, Single-Mode Fiber, DLC Connectors Top and Bottom, 240 FTDocument3 pagesHYBRIFLEX® RRH Hybrid Cable Solution 12 X 24, 6AWG, Low-Inductance, Single-Mode Fiber, DLC Connectors Top and Bottom, 240 FTNoame Pauline SimbajonNo ratings yet
- Company ProfileDocument10 pagesCompany Profile1anupma0No ratings yet
- Measuring: TranslateDocument5 pagesMeasuring: Translatechelsea romaidaNo ratings yet
- Real-Time Reservoir Operation For Irrigation: P. P. Mujumdar and T. S. V. RameshDocument8 pagesReal-Time Reservoir Operation For Irrigation: P. P. Mujumdar and T. S. V. RameshGetachew BekeleNo ratings yet
- Behavior of Connected and Unconnected Back-to-Back Walls For Bridge ApproachesDocument10 pagesBehavior of Connected and Unconnected Back-to-Back Walls For Bridge Approachessalar salarNo ratings yet
- Implant Dentistry - The Most Promising Discipline of Dentistry PDFDocument488 pagesImplant Dentistry - The Most Promising Discipline of Dentistry PDFnaresh sharmaNo ratings yet
- NAS810 Protection of Fluid Lines & EquipDocument1 pageNAS810 Protection of Fluid Lines & EquipfdhgjklNo ratings yet
- Industrial Training IntroductionDocument1 pageIndustrial Training Introductionsgurjar07No ratings yet
- Asme Section II A Sa-435 Sa-435mDocument4 pagesAsme Section II A Sa-435 Sa-435mAnonymous GhPzn1xNo ratings yet
- Saa6d170e-5 HPCR Egr Sen00190-04Document415 pagesSaa6d170e-5 HPCR Egr Sen00190-04Ahmad Mubarok100% (4)
- Hooded Scarf Project From Warm Knits, Cool GiftsDocument4 pagesHooded Scarf Project From Warm Knits, Cool GiftsCrafterNews33% (3)
- Model Business Plan Mango Pineapple Banana 1 1 1Document86 pagesModel Business Plan Mango Pineapple Banana 1 1 1ebubec92% (13)
- Sample Final OutputDocument3 pagesSample Final OutputRey Dominique VillarNo ratings yet
- Curriculum MapDocument3 pagesCurriculum MapSem PerezNo ratings yet
- Food DirectoryDocument20 pagesFood Directoryyugam kakaNo ratings yet
- Comprehension Y9aDocument9 pagesComprehension Y9angwenping5No ratings yet
- Australian F1 SUBMACHINE GUNDocument4 pagesAustralian F1 SUBMACHINE GUNCaprikorn100% (4)
- ASPE Data Book Volume 1 & 2 - Attachment For Pump Head CalculationDocument2 pagesASPE Data Book Volume 1 & 2 - Attachment For Pump Head CalculationibnrafeeqNo ratings yet
- Hepatitis - Seminary WorkDocument15 pagesHepatitis - Seminary WorkDraganaNo ratings yet
- Mathematics JEE Main Chapter Wise DPPDocument513 pagesMathematics JEE Main Chapter Wise DPPMurali100% (1)
- ACS Appl. Energy Mater. 5 (2022) 367-379 PDFDocument13 pagesACS Appl. Energy Mater. 5 (2022) 367-379 PDFEdgar QuintanillaNo ratings yet
- ABC Oilfield Services Emergency Drill RecordDocument1 pageABC Oilfield Services Emergency Drill RecordJaijeev PaliNo ratings yet
- Drug Metabolism in Fetus and NewbornsDocument20 pagesDrug Metabolism in Fetus and NewbornsBikash SahNo ratings yet