Professional Documents
Culture Documents
The Pulse Oximeter
The Pulse Oximeter
Uploaded by
Roberto TeekersinghCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Pulse Oximeter
The Pulse Oximeter
Uploaded by
Roberto TeekersinghCopyright:
Available Formats
LECTURE/PRESENTATION DATE: 05TH November 2015
TOPIC : THE PULSE OXIMETER/OXIMETRY
Pulse oximetry is a procedure used to measure the oxygen level (or oxygen saturation) in
the blood. It is considered to be a non-invasive, painless, and a general indicator of oxygen
delivery to the peripheral tissues (such as the finger, earlobe, or nose).
HOW DOES PULSE OXIMETRY WORK
Oxygen in the air is breathed into the lungs. The oxygen then passes into the blood where the
majority of the oxygen attaches to haemoglobin (a protein located inside the red blood cell) for
transport in the bloodstream. The oxygenated blood circulates to the tissues.
Pulse oximetry technology utilizes the light absorptive characteristics of haemoglobin and the
pulsating nature of blood flow in the arteries to aid in determining the oxygenation status in the
body. First, there is a colour difference between arterial haemoglobin saturated with oxygen,
which is bright red, and venous haemoglobin without oxygen, which is darker.
Second, with each pulsation or heartbeat there is a slight increase in the volume of blood flowing
through the arteries. Because of the increase of blood volume, albeit small, there is an associated
increase in oxygen-rich haemoglobin. This represents the maximum amount of oxygen-rich
haemoglobin pulsating through the blood vessels.
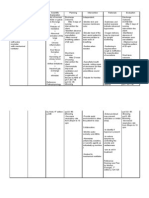
A clip-like device called a probe is placed on a body part, such as a finger or ear lobe, to measure
the blood that is still carrying or is saturated with oxygen. The probe houses a light source, a light
detector, and a microprocessor, which compares and calculates the differences in the oxygen-rich
versus oxygen-poor haemoglobin. One side of the probe has a light source with two different types
of light, infrared and red, which are transmitted through the finger to the light detector side of the
probe. The oxygen-rich haemoglobin absorbs more of the infrared light and the haemoglobin
without oxygen absorbs more of the red light. The microprocessor calculates the differences and
converts the information to a digital readout. This information helps the responder assess the
amount of oxygen being carried in the blood and evaluate the need for supplemental oxygen.It is
also useful in measuring your pulse rate.
Use of pulse oximetry in cases of smoke or carbon monoxide inhalation is not helpful because oximetry
cannot distinguish between normal oxygen saturation in the haemoglobin and the
carboxyhaemoglobin saturation of haemoglobin that occurs with inhalation of smoke or carbon
dioxide.
Certain factors or conditions may interfere with the results of the test. These include, but are not
limited to, the following:
Decreased blood flow to the peripheral vessels
Light shining directly on the oximetry probe
Movement of the area to which the probe is attached
Severe anemia (decreased red blood cells)
Extreme warmth or coolness of the area to which the probe is attached
Excessive sweating of the area to which the probe is attached
WHAT DOES SpO2 MEAN? WHAT IS A NORMAL SpO2 LEVEL?
SpO2 stands for peripheral capillary oxygen saturation, an estimate of the amount of oxygen in the
blood. More specifically, it is the percentage of oxygenated haemoglobin (haemoglobin containing
oxygen) compared to the total amount of haemoglobin in the blood (oxygenated and non-oxygenated
haemoglobin).SpO2 is an estimate of arterial oxygen saturation, or SaO2, which refers to the amount
of oxygenated haemoglobin in the blood.Haemoglobin is a protein that carries oxygen in the blood. It
is found inside red blood cells and gives them their red colour.
For a regular healthy person, the normal blood oxygen saturation level (SpO2) should be around
94% to 99%. For patients with mild respiratory diseases, the SpO2 should be 90% or above.
Supplementary oxygen should be used if SpO2 level falls below 90%, which is unacceptable for a
prolonged period of time.
HYPOXIA OR HYPOXEMIA
When your body doesn't have enough oxygen, you could get hypoxemia or hypoxia. These are
dangerous conditions. Without oxygen, your brain,liver, and other organs can be damaged just
minutes after symptoms start.
Hypoxemia (low oxygen in your blood) can cause hypoxia (low oxygen in your tissues) when your blood
doesn't carry enough oxygen to your tissues to meet your body's needs. The word hypoxia is
sometimes used to describe both problems.Some causes are,but not limited to are COPD (Chronic
Obstructive Pulmonary Disease), Pulmonary Edema,Anaemia,Asthma,Bronchitis, Emphysema, and
heart disease.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ChesttubesDocument30 pagesChesttubesapi-2692977900% (1)
- Atelectasis EditedDocument40 pagesAtelectasis EditedAimee Gutierrez100% (1)
- Restrictive Lung DiseaseDocument21 pagesRestrictive Lung DiseaseSerena MogniNo ratings yet
- Acute Respiratory FailureDocument34 pagesAcute Respiratory FailureStuDIEng100% (1)
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas Exchangecuicuita100% (3)
- Chest Tube ThoracostomyDocument6 pagesChest Tube ThoracostomyRhea Lyn LamosteNo ratings yet
- ThoracentesisDocument10 pagesThoracentesisGabriel Friedman100% (1)
- Scientific Book Jicccim 2018Document171 pagesScientific Book Jicccim 2018ngwinda90No ratings yet
- Impaired Gas ExchangeDocument2 pagesImpaired Gas Exchangeiloveanne87% (30)
- Physiology of Mechanical VentilationDocument28 pagesPhysiology of Mechanical VentilationBaswaraj Tandur100% (1)
- Application of High-Fow Nasal CannulaDocument7 pagesApplication of High-Fow Nasal CannulaCLAUDIANo ratings yet
- Daftar Pustaka PDFDocument3 pagesDaftar Pustaka PDFRatih Ayu PNo ratings yet
- Date and Time Focus: D - Received Patient On BedDocument2 pagesDate and Time Focus: D - Received Patient On BedGraphaiene Neika WacasNo ratings yet
- Diagnostic in Pulmonary Emergency and Respiratory Problem 2020 PDFDocument43 pagesDiagnostic in Pulmonary Emergency and Respiratory Problem 2020 PDFIzka P RahmaniaNo ratings yet
- COPD Case StudyDocument3 pagesCOPD Case Studyshazel chiasaokwuNo ratings yet
- Pharm Resp Mcqs PDFDocument8 pagesPharm Resp Mcqs PDFVikashgtmNo ratings yet
- ICU No Nama Alat Merk TypeDocument2 pagesICU No Nama Alat Merk TypeRamadhan FebriNo ratings yet
- SDL R VS OldDocument6 pagesSDL R VS Oldsejal3vijNo ratings yet
- Ers 2015Document358 pagesErs 2015Dejan ŽujovićNo ratings yet
- 2) Respiratory - Acute Lung Failure - 202243.15374-CCRN-1505-01 - MANAGEMENT OF CCHC - RESPIRATORYDocument5 pages2) Respiratory - Acute Lung Failure - 202243.15374-CCRN-1505-01 - MANAGEMENT OF CCHC - RESPIRATORYafshin nikraveshNo ratings yet
- Acute Respiratory FailureDocument13 pagesAcute Respiratory FailureKartikaNo ratings yet
- Oxygen Assessment ToolDocument6 pagesOxygen Assessment Toolshinoj poyanadanNo ratings yet
- Flyer Konker Pdpi 2023 23082023Document30 pagesFlyer Konker Pdpi 2023 23082023suci mesaNo ratings yet
- Kuliah Pakar 2 Dyspnea PBLDocument35 pagesKuliah Pakar 2 Dyspnea PBLTrisya AksaraNo ratings yet
- Positive End Expiratory PressureDocument5 pagesPositive End Expiratory PressureIrving H Torres LopezNo ratings yet
- Hafizah Hoshni PneumothoraxDocument47 pagesHafizah Hoshni PneumothoraxhafizahhoshniNo ratings yet
- Mindray Ventilator SynoVent E5 BrochureDocument4 pagesMindray Ventilator SynoVent E5 BrochureKoalaNo ratings yet
- NBRC Nps Test Content AreasDocument19 pagesNBRC Nps Test Content AreasMarla Karina Urbach0% (1)
- Respiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyDocument9 pagesRespiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyanaNo ratings yet
- SS Mawar FixDocument42 pagesSS Mawar FixFransnedo EXONo ratings yet