Professional Documents
Culture Documents
5601 20099 1 PB
Uploaded by
Anonymous d1CGjMTiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
5601 20099 1 PB
Uploaded by
Anonymous d1CGjMTiCopyright:
Available Formats
Original Article
Port Site and Intraperitoneal Infiltration of Local
Anesthetics in Reduction of Postoperative Pain
after Laparoscopic Cholecystectomy
Alam M S1, Hoque H W 2, Saifullah M3, Ali M O4.
Abstract simple, inexpensive and effective technique to minimize
early postoperative pain and can be practiced for elective
Laparoscopic cholecystectomy is now the gold standard
laparoscopic cholecystectomy.
technique for the treatment of gallstones disease. Although
pain after laparoscopic cholecystectomy is less intense than Introduction:
after open cholecystectomy, some patients still experience Laparoscopic cholecystectomy has become a standard
considerable discomfort during the first 24 to 72 technique for gall bladder surgery of symptomatic
postoperative hours. The aim of this study is to evaluate the cholelitheasis. The introduction of laparoscopic technique to
effect of intraperitoneal and port site instillation of local general surgery has dramatically changed our view to the
anaesthetics on pain relief in early postoperative period post operative course of patients after cholecystectomy1.
following laparoscopic cholecystectomy. Fifty patients Laparoscopic cholecystectomy has proven to reduce the
undergoing elective laparoscopic cholecystectomy were post operative pain significantly and allow a short hospital
consecutively included in this study and sample was divided stay and recovery period, which is reflected in patients
into two groups. Following removal of gallbladder, Group A earlier return to normal life and work activities2, 3. In most
received 20 ml of 0.25% bupivacaine instilled in the right of the centers patients are discharged home on the first post
sub diaphragmatic space and 20 ml of 0.25%bupivacaine in operative day. However, few series have recently shown that
divided doses at the trocar sites. The evaluation of the operation is safe and feasible even as an out patient
procedure in properly selected patients4, 5.
postoperative pain was done at fixed time interval according
to the numerical verbal scale and the dosage of narcotic Thus, pain relief and patient comfort during the early post
analgesics consumed was also recorded. Mean pain scores operative period becomes increasingly important, as the
at 6 hours and at 12 hours after surgery were 6.02 and 4.72 need for analgesic may delay discharge. Pain on the day of
respectively, in the bupivacaine group compared with 8.44 surgery is typically a diffuse abdominal pain, a more so to
the right upper quadrant and right shoulder tip6.
and 6.08 respectively in the control group (p= <0.001 and
<0.001). However, pain scores at 24hours and 48 hours Decrease in post operative pain after infiltration of local
postoperatively and incidence of shoulder tip pain did not anesthetics into the operative wound have been observed
differ significantly between the two groups. The mean total among patients who undergo herniorrhaphy and
gynecological procedures7. Continuous post operative
narcotic analgesics used in study group was 1.91 as
infusion of local anesthetic agent into the abdominal wound
compared to 2.50 in the control group respectively and was
has reduced both postoperative pain and narcotic
found to be statistically significant (p= <0.001). Infiltration requirements8.
of bupivacaine in to port site and intraperitoneal space is
Bupivacaine has a half life of 2.5 to 3.5 hours and has been
1. Dr. Mohammad Shaha Alam, MBBS, MS (Surgery), FICS (USA) reported to provide pain control for an average of 6 hours.9
Surgery Specialist, The margin of safety of the bupivacaine need for anesthesia
Coxs Bazar Medical College, Coxs Bazar, Bangladesh. is wide. At the upper limit of 2.5mg of bupivacaine per
2. Dr. Hasnat Waheedul Hoque, M.Phil(Radiology) kilogram body weight, 100mg of the drug can be used
District sadar Hospital, Coxs Bazar, Bangladesh. safely in a patient with a lean body mass of 40 kgs9.
3. Dr. Mohammad Saifullah, FCPS (Surgery)
Dhaka Medical College, Dhaka, Bangladesh. Controversy exists on source of pain after laparoscopic
procedures. Some clinicians maintain that the placement of
4. Dr. Md. Omar Ali, FCPS (Surgery), FICS (USA)
Dhaka Medical College, Dhaka, Bangladesh. trocars through the abdominal wall is the primary source,
whereas other believes that most pain arises from
2009 Volume 22 Number 01
24
ORIGINAL ARTICLE
intraperitoneal dissection10. Variable analgesic effects of fixed time interval at 6hrs, 12hrs, 24hrs, and 48hrs
periportal infiltration of local anesthetics, intraperitoneal respectively. Presence of shoulder pain was also assessed
spraying above the gall bladder, and instillation into the during the same interval.
subdiaphramatic space and into the subhepetic space
Patients were given narcotic analgesic intramuscularly
covering the area of the hepatoduodenal ligament have been
(pethidine 50mg+ phenargan 25mg) on requirement and the
reported. Some of them failed to show any benefit11.
total number of doses of narcotic analgesia used was
Our study is designed to evaluate the effect of combined recorded in a proforma. Statistical analysis of the data was
intraperitoneal and port site infiltration of bupivacaine for done using SPSS software programmed. Independent t
pain relief following laparoscopic cholecystectomy. test and chi square test were used for statistical analysis.
Differences were considered significant at a probability
Methodology:
level less than 0.05.
This is a prospective, consecutive study conducted in the
Results
General Surgery Unit-II of Dhaka Medical College Hospital
for six month. Patients scheduled to undergo elective A total of 50 patients participated in the study. The male to
laparoscopic cholecystectomy during March 2006 to August female ratio was 1: 4 in the study group and 1:4 in control
2006, were included in this study. There were fifty patients group. There were 80% of females in both study and control
who participated in this study, with twenty-five patients in group. Twenty-five patients (20 women & 5men) with mean
each arm. All the patients gave informed consent and met (SD) age 36.92(13.24) years received Bupivacaine. The
the following criteria: adult patient [above 16 years] with control group comprised 25 patients (20 women, 5 men)
ASA Class 1(a normally healthy individual) and 2(a patient with mean age 40.92 (13.11) years.
with mild to moderate systemic disease), who were
The gas pressure in the bupivacaine group was median
undergoing planned elective procedure for symptomatic gall
(SD) 12.12 mmHg (0.92) and that of control was 13.08
stone disease. Patient with choledocholithiasis, placement
mmHg (0.70) and was not found to be statistically
of drain intraoperatively and any previous upper abdominal
significant.
surgery were not included in the study. All patients were
explained about the basis of study and informed consent Intensity of pain was assessed at fixed time intervals at 6
was obtained. hrs, 12hrs, 24hrs and 48 hrs postoperatively. The Mean
(SD) score ranged from 2.68 (0.47) to 6.08 (0.40) for
All patients were screened preoperatively with the help of
the bupivacaine group and from 2.44 (0.51) to 8.44(0.51)
anesthetist and explained about the use of Numerical Rating
for the control group. (Table-I)
Scale (NRS) for pain employed in this study. The scale
ranged from 0-10, with 1 being the mildest pain the patient Table I: Mean pain Scores for study and control group
ever had and 10 being the most severe pain, zero counts for
Mean ( SD) Pain Scores* postoperatively for patients
no pain12.
given Bupivacaine compared with those not receiving
Patients were randomized into the study arm and control Bupivacaine (control)
arm using the random number table. In all cases induction,
maintain and reversal of anesthesia was achieved by Postop Assessment Bupivacaine Control p value
standard protocol. time group group
Pneumoperitoneum was produced by insufflations of carbon 6hrs 6.08(0.40) 8.44(0.51) <0.001*
dioxide with the method of open laparoscopes using Hassans 12hrs 4.72(0.61) 6.08(0.64) <0.001*
canula and port laparoscopes was carried out with carried out
24hrs 3.44(0.51) 3.40(0.50) 0.780
with gas pressure maintained between 12-14mm Hg.
48hrs 2.68(0.47) 2.44(0.51) 0.091
After delivery of the gall bladder 20 ml of 0.5% bupivacaine
solution was instilled in the right sub diaphragmatic space [Ranged from 0 (no pain) to 10 (severe pain) ]
and another 20ml was infiltrated into the port sites (6ml was * Highly significant
infiltrated through the abdominal wall around each midline At 6 hours postoperatively the Mean (SD) pain score of
port site and 4ml administered in the similar fashion at the Bupivacaine group was found to be 6.08(0.40) as
lateral port sites). compared to Control group 8.44(0.51) and it was found to
In all cases, residual carbon dioxide was evacuated at the be having p value of <0.001.
end of the procedure by compressing the abdomen before Therefore, Bupivacaine provided a substantial reduction of
closure of ports. pain intensity during the first 6 hours postoperatively and
The time of arrival in the postoperative ward was defined as this was found to be statistically highly significant. At 12
zero hour postoperatively. Pain intensity was measured at hours postoperatively, although the Mean (SD) was
2009 Volume 22 Number 01
25
ORIGINAL ARTICLE
4.72(0.61) of study group in compare to 6.08(0.64) of the analgesics. 14
Control group, it was found to be having p value <0.001.
Controversy exists about the principal source of pain after
It is evident that Bupivacaine did provide a substantial laparoscopic procedure. Some clinicians mentioned that
reduction of pain intensity during the first 12 hrs placement of trocars through the abdominal wall is the
postoperatively. There was no significant difference in the primary source; whereas others believe that most pain arises
intensity of pain at 24hrs and 48hrs respectively. The mean
from intraperitoneal dissection and insufflations of CO2
ranged between 2.68 to 3.44 in the bupivacaine group and
resulting in distension of abdominal wall and prolonged
2.44 to 3.40 in the control group. Two patients in the study
elevation of diaphragm15. Early pain after laparoscopic
group and 3 patients belonging to the control arm
experienced shoulder tip pain and it was statistically not cholecystectomy is a complex process and includes different
significant (p=0.646). pain components secondary to different pain mechanisms,
such as surgical trauma to the abdominal wall, intra-
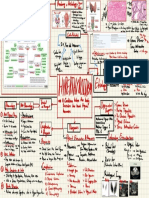
Fig 1: Opoid analgesics requirement in both group of abdominal trauma secondary to the gall bladder removal,
patients abdominal distention, pneumoperitoneum using carbon
dioxide etc. Therefore pain should be treated multimodally16.
25 We studied the effect of combined somatovisceral
(intraperitoneal and port site) instillation of local anesthesia
for analgesia after laparoscopic cholecystectomy.
20 In our study, over all pain (incisional and visceral) is
reduced. Shoulder pain also reduced. In previous
randomized control trial studies where incisional local
15
anesthetics were used for analgesia Alexander17 and Sarac18
Number found reduction in the intensity of pain and opoid
14 requirement whereas Ure19 did not found pain to be reduced,
10
when local anesthetics were infiltrated into the abdominal
wall.
5 8 Our study showed modest overall analgesic effect whereas
there was a statistically significant difference during the first
3 6 and 12 hours. Cuniffe20 showed a significant decrease in
0 shoulder tip pain after intraperitoneal bupivacaine. Our
1 2 3
present study did not show any significant reduction in
Doses shoulder tip pain and it was consistent with the findings of
Chandrigar21 and Szem12. Bisgaard22 and Michaloliakou23
control examined the effect of combined multiregional incisional
study and intraperitoneal local anesthetic blockade in two RCTs.
The total narcotic requirement in study group was mean Michaloiakou23 reported a significant reduction in overall
(SD) 1.91(0.61) while that in control group was 2.50 pain during the first 24 hours postoperatively. Our study also
(0.51). Eight patients (32%) in the bupivacaine group showed a significant difference in pain intensity in the early
required only one dose of opiod analgesic. Fourteen (56%) postoperative period. Bisgaard22 showed a significant
patients in study group received two doses of opiod reduction in overall pain and narcotic requirements, however
analgesic whereas 11(44%) patients received those doses in there was no significant effect on shoulder tip pain and it
control group. Fourteen patients (56%) in control arm had was consistent with our present study.
three doses of narcotic analgesic in compare to only 3
patients (12%) in the Bupivacaine group who required total We found a large variation in pain scores at each of the
of three doses (Fig-I) and it was found to be statistically assessment times. Aside from individual difference in pain
significant [p= <0.001]. perception, several other patient and technical factors may
have affected the scores. Despite of large variation in the
Discussion: pain scores, we did detect differences in mean pain scores
Although Minimal Invasive Surgery is characterized by between the bupivacaine and control group during the 6
reduced pain, it is not painless. Thirteen Patients undergoing hours and 12 hours postoperative assessment. Mean pain
Laparoscopic cholecystectomy suffer considerable pain on scores at 6 hours and 12 hours were found to be statistically
the day of surgery though frequently requires narcotic significant.
2009 Volume 22 Number 01
26
ORIGINAL ARTICLE
Although we expected the effect of the local anesthetic to study of pain level and analgesic requirement after
wear off after the period of 6-8hours, there was no increase laparoscopic and open cholecystectomy. Surg Laparosc
in the pain score at the 3rd pain assessment at 24hours Endosc 1994;4:139-41.
postoperatively in the patients who received bupivacaine.
3. Kunz R, Berger D, Berger HG.Laparoscopic
For the control group pain scores peaked immediately and cholecystectomy versus mini-lap cholecystectomy: a
were maximum during the first 6-8hours after the surgical prospective randomized trial.Surg Endosc 1994;8:504.
procedure and there after declined to the level comparable to
4. Mjaland O, Reader J, Aesboe V, Trondsen E, Buanes
that for the bupivacaine group by the third assessment at
T. Out patient laparoscopic cholecystectomy. Br J Surg
24hours postoperatively. Therefore, the main effect of
1997;84:958-961.
bupivacaine in this study seems to have been in amelioration
of pain peak occurring during the initial 6 hours after the 5. KeulmansY, Eshuis J,de Haes H, de Wit LT, Gouma
surgical procedure. We did find an appreciable difference in DJ:Laparoscopic cholecystectomy:daycare versus
total narcotic analgesics requirement between the control clinical observation.Ann Surg1998;228:734-740.
and bupivacaine group and this was consistent with the
6. Spittal MJ, Hunter SJ. A comparison of bupivacaine
findings that of Bisgaard22 in a randomized control study.
instillation and inguinal field block for pain control
If laparoscopic cholecystectomy is to be a routine after herniorrhaphy. Ann R Coll Surg Engl 1992;74:85-
ambulatory surgical procedure, the pain experienced by the 88.
patients during early postoperative period must be
7. Bays RA, Barry L. The use of bupivacaine in elective
addressed. Our study showed that Infiltration of bupivacaine
inguinal herniorrhaphy as a fast and safe technique for
into the port site and intraperitoneal instillation diminishes
relief of postoperative pain. Surg Gynecol Obstetric
the peak of pain occurring during the first 6 hours after the
1991;57:548-52.
surgical procedure and significantly reduces the need for
narcotic analgesics. 8. Thomas DF, Lambert WG. The direct perfusion of
surgical wounds with local anesthetics solution: an
Any reduction in such pain is relevant, particularly if it is
approach to postoperative pain. Ann R Coll Surg Engl
statistically significant, whether the lower pain score
1983;65,226-9.
translated into increased patients comfort and compliance is
questionable. However, at whatever level they functioned 9. Szem JW, Hydo L A double blind evaluation of
they did so more comfortably. intraperitoneal bupivacaine vs saline for the
reduction of postoperative pain and nausea after
Thus, this simple, inexpensive, effective technique improves
laparoscopic cholecystectomy. Surg Endos 1996;
the postoperative period in-hospital course and can be 10:44-48.
practiced routinely in all elective laparoscopic
cholecystectomy. 10. Rademaker BM, Kalkman CJ.Intraperitoneal local
anesthetics after laparoscopic cholecystectomy:
Conclusion effects on postoperative pain, metabolic responses and
lung function. Br J Anaes 1994;72:263-6.
Laparoscopic cholecystectomy in now the gold standard for
the treatment of gall stones disease when a careful, correct 11. Mouret P. from the first laparoscopic cholecystectomy
technique is employed, though pain after laparoscopic to the frontiers of laparoscopic surgery, the future
cholecystectomy is multifactorial; our study showed port prospectives. Dig Surg 1991;81:124-125
site, intraperitoneal infiltration of local anesthetics for post
12. Mouton WG, Bessell JR Pain after laparoscopy. Surg
operative pain relief is, in this context, an effective
Endoscopy; 1999;13:106-108.
alternative method for early pain control and minimize the
need of opoid analgesics and the technique is very simple, 13. Alexander JI, Hull MGR. Adbominal pain after
easily applicable. laproscopy: the value of a gas drain. Br J Obstet
Gynaecol 1987;94:26-269.
References:
14. Fredman B, Olsfanger D. Residual
1. Simpson JP, savarise MT, Moore J: Out patients
pneumoperitoneum: a cause of postoperative pain after
laparoscopic cholecystectomy: What predicts the
laparoscopic cholecystectomy. Can J Surg 1996;39:26-
need for admission? Am Surg 1999;65:525-528.
30.
2. Kum CK, Wong CW, Goh MY, Ti TK. Comparative
15. Sarac AM. Baykan N The effect and timing of local
2009 Volume 22 Number 01
27
ORIGINAL ARTICLE
anaesthesia in laparoscopic cholecystectomy. Surg laparos 20. Cunniffe Mogador MA a prspective randomezed of
Endos 1996;6:362-366. intraoperative bupivacaine irrigation for management
of shoulder tip pain following laparoscopy. Am J Surg
16. Dubner R: Neuronal plasticity and pain following 1998;176:258- 261.
peripheral tissue inflammation or nerve injury.
Proceedings of the VIth world congress on pain. Edited 21. Chandigar T, Hedges AR. Intraperitoneal bupivacaine
by Bond MR, Charlton JE, Woolf CJ. Amsterdam, for effective pain relief after laparoscopic
Elsevier, 1991;263-76. cholecystectomy. Ann R Coll Rurg Engl 1993;75: 437-
439.
17. Alexander JI, Hull MGR. Adbominal pain after
laproscopy: the value of a gas drain. Br J Obstet 22. Bisgaard T, Klarskov B. Multiregional local
Gynaecol 1987;94:26-269. anaesthetic infiltration during laparoscopic
cholecystectomy in patients receiving prophylactic
18. Sarac AM. Baykan N The effect and timing of local multimodal analgesea: a randomezed, double blinded,
anaesthesia in laparoscopic cholecystectomy. Surg placebo controlled study. Anaes Anal 1999;89:1017-
laparos Endos 1996; 6:362-366. 1024
19. Ure BM,Troidl H.Preincisional local anaesthesia with 23. Michaloliakou C, Chung F. Preoperative multimodal
bupivacaine after laparoscopic cholecystectomy. A analgesia facilitates recovery after ambulatory
double blind RCT. Surg Endos 1993;7:482-488. laparoscopic cholecystectomy. Anaes Anal 1996;
82:44-51.
2009 Volume 22 Number 01
28
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Noor PDFDocument826 pagesNoor PDFAnonymous d1CGjMTi100% (1)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Plutonium, Lead-210, and Carbon Isotopes in TDocument7 pagesPlutonium, Lead-210, and Carbon Isotopes in TAnonymous d1CGjMTiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Global Circulation of Radiocerium Isotopes From The May 14, 1965, Nuclear ExplosioDocument8 pagesGlobal Circulation of Radiocerium Isotopes From The May 14, 1965, Nuclear ExplosioAnonymous d1CGjMTiNo ratings yet
- PSM Old Questions (UM 2,) : KZM (Final Part I, 6/2018)Document9 pagesPSM Old Questions (UM 2,) : KZM (Final Part I, 6/2018)Anonymous d1CGjMTiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Royal College of Obstetricians and Gynaecologists Evidence-Based Clinical Guidelines Guideline Summary No. 2: The Initial Investigation and Management of The Infertile CoupleDocument10 pagesRoyal College of Obstetricians and Gynaecologists Evidence-Based Clinical Guidelines Guideline Summary No. 2: The Initial Investigation and Management of The Infertile CoupleAnonymous d1CGjMTiNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Geology of Burma (DGSE)Document126 pagesGeology of Burma (DGSE)Anonymous d1CGjMTi100% (3)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Geology of Burma (DGSE)Document126 pagesGeology of Burma (DGSE)Anonymous d1CGjMTi100% (3)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- UM 1 Mock 2 16.8.18Document18 pagesUM 1 Mock 2 16.8.18Anonymous d1CGjMTiNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- UM 1 Mock 2 16.8.18Document18 pagesUM 1 Mock 2 16.8.18Anonymous d1CGjMTiNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Review Article: Transversus Abdominis Plane Block: An Updated Review of Anatomy and TechniquesDocument12 pagesReview Article: Transversus Abdominis Plane Block: An Updated Review of Anatomy and TechniquesAnonymous d1CGjMTiNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Marta Et Al (2015)Document8 pagesMarta Et Al (2015)Anonymous d1CGjMTiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 00038Document11 pages00038Anonymous d1CGjMTiNo ratings yet
- DocumentDocument6 pagesDocumentAnonymous d1CGjMTiNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- (Pageoph Topical Volumes) Raúl Madariaga, Agustín Udías (Auth.), Agustín Udías, Elisa Buforn (Eds.) - Source Mechanism and Seismotectonics-Birkhäuser Basel (1991)Document211 pages(Pageoph Topical Volumes) Raúl Madariaga, Agustín Udías (Auth.), Agustín Udías, Elisa Buforn (Eds.) - Source Mechanism and Seismotectonics-Birkhäuser Basel (1991)Anonymous d1CGjMTiNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Crash Cart ICU EMRDocument5 pagesCrash Cart ICU EMRRetteri KUMARANNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 01f2 - ICD vs. DSM - APA PDFDocument1 page01f2 - ICD vs. DSM - APA PDFfuturistzgNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Visiting A DoctorDocument12 pagesVisiting A DoctorНаталіяNo ratings yet
- PTB Case-StudyDocument64 pagesPTB Case-StudyBeverly DatuNo ratings yet
- Essential DrugsDocument10 pagesEssential DrugsZarish IftikharNo ratings yet
- Mindmap METENDocument1 pageMindmap METENIpulCoolNo ratings yet
- Emmess Books Catalogue: Nursing & Allied Health SciencesDocument32 pagesEmmess Books Catalogue: Nursing & Allied Health SciencesMIR SARTAJ0% (3)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Detailed Study On Infertility Its Causes and TreatmentDocument2 pagesDetailed Study On Infertility Its Causes and TreatmentBibhuti bhusan MondalNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Patient Safety WHO CurriculumDocument46 pagesPatient Safety WHO CurriculumCalvin Chowder WittelsbachNo ratings yet
- HYPERALDOSTERONISMDocument7 pagesHYPERALDOSTERONISMMarnee Justine ColladoNo ratings yet
- Midazolam Drug Study SaclotDocument1 pageMidazolam Drug Study SaclotMaybelle Cababat Saclot100% (1)
- Nakahara Et Al 2023 Assessment of Myocardial 18f FDG Uptake at Pet CT in Asymptomatic Sars Cov 2 Vaccinated andDocument65 pagesNakahara Et Al 2023 Assessment of Myocardial 18f FDG Uptake at Pet CT in Asymptomatic Sars Cov 2 Vaccinated andgandalf74No ratings yet
- Acupuntura Protocolo Endometriose PDFDocument8 pagesAcupuntura Protocolo Endometriose PDFGraziele GuimaraesNo ratings yet
- Lab 2 - Birth Spacing Policy in OmanDocument39 pagesLab 2 - Birth Spacing Policy in OmanMeme 1234No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- CH-UH Media Statement Re Healthcare 11-30-2020Document2 pagesCH-UH Media Statement Re Healthcare 11-30-2020WKYC.comNo ratings yet
- MTY1215 Hematology 2 (Lec) HandoutsDocument7 pagesMTY1215 Hematology 2 (Lec) HandoutsDarren Gabriel NicolasNo ratings yet
- Telepharmacy ResearchDocument8 pagesTelepharmacy Researchugwuja marcyNo ratings yet
- SOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticDocument5 pagesSOFA (Sequential Organ Failure Assessment) and PELOD (Pediatric LogisticvidyahamzahNo ratings yet
- Anesthesia in The FutureDocument11 pagesAnesthesia in The FuturesayednourNo ratings yet
- UntitledDocument337 pagesUntitledGulzar AhmadNo ratings yet
- Drug Study..Document4 pagesDrug Study..Micah SalesNo ratings yet
- Prevalence of Helicobacter Pylori Infection AmongDocument77 pagesPrevalence of Helicobacter Pylori Infection AmongAbigailNo ratings yet
- 60 Revision MCQs For ProsDocument9 pages60 Revision MCQs For ProsUsman Ali AkbarNo ratings yet
- Eating Disorders: by Pius KigamwaDocument20 pagesEating Disorders: by Pius KigamwaRahul Kumar DiwakarNo ratings yet
- Perioperative Patient CareDocument6 pagesPerioperative Patient CareClark LlameraNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Resume Template PharmacistDocument1 pageResume Template PharmacistHammad AslamNo ratings yet
- Family Centered CareDocument7 pagesFamily Centered CareSirisha ChelvaNo ratings yet
- Nursing Care Plan Breast CancerDocument1 pageNursing Care Plan Breast CancerAhmed SalahNo ratings yet
- Laporan 10 Penyakit Terbesar Rawat Inap Bulan Januari 2022: Rawat Inap LT 1 Rawat Inap LT 2 Rawat Inap Perina-NiccuDocument4 pagesLaporan 10 Penyakit Terbesar Rawat Inap Bulan Januari 2022: Rawat Inap LT 1 Rawat Inap LT 2 Rawat Inap Perina-NiccuAhmad MunifNo ratings yet
- Ca BladderDocument11 pagesCa Bladdersalsabil aurellNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)