Professional Documents
Culture Documents
Concenso Tratamiento Miastenia 2013
Uploaded by
Francisca Fernanda Martinez SepulvedaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Concenso Tratamiento Miastenia 2013
Uploaded by
Francisca Fernanda Martinez SepulvedaCopyright:
Available Formats
VIEWS & REVIEWS
International consensus guidance for
management of myasthenia gravis
Executive summary
Donald B. Sanders, MD* ABSTRACT
Gil I. Wolfe, MD* Objective: To develop formal consensus-based guidance for the management of myasthenia
Michael Benatar, MD, gravis (MG).
PhD
Methods: In October 2013, the Myasthenia Gravis Foundation of America appointed a Task Force
Amelia Evoli, MD
to develop treatment guidance for MG, and a panel of 15 international experts was convened. The
Nils E. Gilhus, MD
RAND/UCLA appropriateness methodology was used to develop consensus guidance state-
Isabel Illa, MD
ments. Definitions were developed for goals of treatment, minimal manifestations, remission, ocu-
Nancy Kuntz, MD
lar MG, impending crisis, crisis, and refractory MG. An in-person panel meeting then determined
Janice M. Massey, MD
7 treatment topics to be addressed. Initial guidance statements were developed from literature
Arthur Melms, MD
summaries. Three rounds of anonymous e-mail votes were used to attain consensus on guidance
Hiroyuki Murai, MD
statements modified on the basis of panel input.
Michael Nicolle, MD
Jacqueline Palace, BM, Results: Guidance statements were developed for symptomatic and immunosuppressive treat-
DM ments, IV immunoglobulin and plasma exchange, management of impending and manifest myas-
David P. Richman, MD thenic crisis, thymectomy, juvenile MG, MG associated with antibodies to muscle-specific
Jan Verschuuren, MD tyrosine kinase, and MG in pregnancy.
Pushpa Narayanaswami, Conclusion: This is an international formal consensus of MG experts intended to be a guide for
MBBS, DM* clinicians caring for patients with MG worldwide. Neurology 2016;87:419425
GLOSSARY
Correspondence to AChR 5 acetylcholine receptor; ChEI 5 cholinesterase inhibitor; CTCAE 5 Common Terminology Criteria for Adverse
Dr. Sanders: Events; FDA 5 Food and Drug Administration; IS 5 immunosuppressive; IVIg 5 IV immunoglobulin; JMG 5 juvenile myas-
donald.sanders@duke.edu thenia gravis; MG 5 myasthenia gravis; MGFA 5 Myasthenia Gravis Foundation of America; MMS 5 minimal manifestation
status; MuSK 5 muscle-specific tyrosine kinase; PIS 5 Post-Intervention Status; PLEX 5 plasma exchange; RAM 5 RAND/
UCLA Appropriateness Method; RCT 5 randomized controlled trial.
Acquired myasthenia gravis (MG) is a disorder of neuromuscular transmission, resulting from
binding of autoantibodies to components of the neuromuscular junction, most commonly
the acetylcholine receptor (AChR). The incidence ranges from 0.3 to 2.8 per 100,000,1 and
it is estimated to affect more than 700,000 people worldwide.
The increasing use of immunomodulating therapies has been a major factor in improving the
prognosis for patients with MG in recent years.2 The various treatment options must be weighed
in the context of individual patient factors.
Editorial, page 350
Why do we need MG guidance treatment statements? Although there is widespread agreement on the use of many
Supplemental data treatments for MG, there is no internationally accepted standard of care. Because MG is heterogeneous, no one
at Neurology.org
*These authors contributed equally to this work.
From the Department of Neurology (D.B.S., J.M.M.), Duke University Medical Center, Durham, NC; Department of Neurology (G.I.W.), University
at Buffalo School of Medicine and Biomedical Sciences, State University of New York; Department of Neurology (M.B.), University of Miami, Miller
School of Medicine, FL; Department of Neurology (A.E.), Catholic University, Rome, Italy; Department of Clinical Medicine (N.E.G.), University of
Bergen, Norway; Department of Neurology (I.I.), Hospital Santa Creu i Sant Pau, Universitat Autnoma de Barcelona; CIBERER U762 (I.I.),
Barcelona, Spain; Departments of Pediatrics and Neurology (N.K.), Northwestern Feinberg School of Medicine, Chicago, IL; Neurologische Klinik
(A.M.), Universittsklinikum Erlangen; Hertie Institute for Clinical Research (A.M.), University of Tbingen, Germany; Department of Neurological
Therapeutics (H.M.), Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan; Department of Clinical Neurological Sciences (M.N.),
Western University, London, Canada; Department of Clinical Neurology (J.P.), John Radcliffe Hospital, Oxford University Hospitals Trust, Oxford,
UK; Department of Neurology (D.P.R.), University of California, Davis, CA; Department of Neurology (J.V.), Leiden University Medical Centre,
Leiden, the Netherlands; and Department of Neurology, Beth Israel Deaconess Medical Center/Harvard Medical School (P.N.), Boston, MA.
Go to Neurology.org for full disclosures. Funding information and disclosures deemed relevant by the authors, if any, are provided at the end of the article.
The Article Processing Charge was paid by the Myasthenia Gravis Foundation of America.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives License 4.0 (CC BY-NC-ND),
which permits downloading and sharing the work provided it is properly cited. The work cannot be changed in any way or used commercially.
2016 American Academy of Neurology 419
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
treatment approach is best for all patients. Few physi- treatment guidelines,49 supplemented by other
cians treat enough patients with MG to be comfort- literature.
able with all available treatments. Given its Guidance statements were developed for the
heterogeneity, the few randomized controlled trials following:
(RCTs) in MG have limited generalizability, while
1. Symptomatic and immunosuppressive (IS)
uncontrolled trials are limited by potential bias.
treatments
Hence, an effort to develop consensus among interna-
2. IV immunoglobulin (IVIg) and plasma exchange
tional experts was undertaken to guide clinicians
(PLEX)
worldwide on the multifaceted approach to managing
3. Impending and manifest myasthenic crisis
MG. This summary condenses the extensive back-
4. Thymectomy
ground information in the full guidance statements,
5. Juvenile MG (JMG)
available on the Neurology Web site at Neurology.org.
6. MG with antibodies to muscle-specific tyrosine
Panel constitution and method of expert consensus. In kinase (MuSK-MG)
October 2013, a Task Force of the Myasthenia 7. MG in pregnancy
Gravis Foundation of America (MGFA) convened Voting process for consensus guidance treatment
a panel of 15 international experts in MG to develop statements. We used the RAND/UCLA Appropriate-
treatment guidance statements based on formalized ness Method (RAM) for formal consensus to quantify
consensus. The panel was chosen to represent the agreement.10 RAM uses a multi-round modified
breadth of knowledge and experience and a wide vari- Delphi process to obtain a quantitative assessment
ety of opinions from MG experts internationally. that reflects the judgment of an expert group.
Development of preliminary definitions. The panel initially Appropriateness refers to the relative benefit vs
voted on definitions that formed the foundation for sub- harm of the intervention. We obtained anonymous
sequent guidance treatment statements: goals of treat- votes and feedback on each draft statement from the
ment, remission, ocular MG, impending and manifest panelists, who rated each for appropriateness on a 9-
myasthenic crises, and refractory MG. point scale (13 inappropriate, 46 uncertain, and 7
The Task Force co-chairs (D.B.S., G.I.W.) 9 appropriate). Panelists responded by e-mail to the
drafted initial definitions based on available litera- facilitator, who tallied the votes and collated the
ture.3 These were sent by e-mail to the panelists, discussions. Following each round of voting,
who were asked to vote yes or no on each, and to statements were modified by the Task Force co-
provide modifications if they did not agree. Panelists chairs and facilitator based on the panel feedback.
were instructed not to discuss the definitions among Statements that did not achieve consensus within 3
themselves, and to send their votes only to the facil- rounds were excluded.
itator (P.N.). A simple consensus was used ($80% of For statements on symptomatic and IS therapies
panelists voting yes). and thymectomy, an initial round of e-mail voting
Definitions not achieving consensus were modi- was followed by a meeting in Durham, North
fied based on the panelists suggestions and the mod- Carolina, on March 1, 2014. During this meeting,
ified definitions and discussions were shared with the statements that had undergone prior voting by
panel for subsequent voting rounds. e-mail were refined with panel input, and a second
round of voting was completed. All subsequent voting
Development of guidance treatment statements. The was by e-mail.
following were agreed upon a priori: The level of appropriateness and presence of agree-
ment were determined for each statement as per RAM.10
1. Treatment costs and availability would not be con-
sidered, as it is not possible to make international RESULTS All definitions below obtained simple con-
consensus statements specific for all countries. sensus and all guidance statements below were agreed
2. Clinical examination is assumed to have been per- upon as being appropriate by the panel. Literature
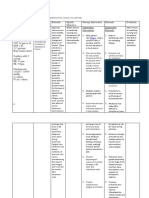
formed by physicians skilled in the evaluation of summaries and tables for medication dosing guidance
neuromuscular disease. and medication cautions are available as supplemental
3. The MGFA Clinical Classification, including data at Neurology.org.
remission, refers to the state of the patient at the
Preliminary definitions.
time of evaluation.
1. Goals for the treatment of MG. MGFA Task Force
A formal systematic review of the literature was Post-Intervention Status (PIS) classification Minimal
not performed. The Task Force co-chairs and facilita- Manifestation Status (MMS) or better,3 with no more
tor drafted initial guidance statements based on liter- than grade 1 Common Terminology Criteria for
ature cited in recent national and regional MG Adverse Events (CTCAE) medication side effects.11
420 Neurology 87 July 26, 2016
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
MMS: The patient has no symptoms or functional 2. A nonsteroidal IS agent should be used alone when
limitations from MG but has some weakness on corticosteroids are contraindicated or refused.
examination of some muscles. This class recognizes A nonsteroidal IS agent should be used initially
that some patients who otherwise meet the definition in conjunction with corticosteroids when the risk
of remission have mild weakness. of steroid side effects is high based on medical
CTCAE grade 1 medication side effects: asymp- comorbidities. A nonsteroidal IS agent should be
tomatic or only mild symptoms; intervention not added to corticosteroids when:
indicated. a. Steroid side effects, deemed significant by the
2. Definition of remission. The patient has no symp- patient or the treating physician, develop;
toms or signs of MG. Weakness of eyelid closure is b. Response to an adequate trial (table e-1) of cor-
accepted, but there is no weakness of any other mus- ticosteroids is inadequate; or
cle on careful examination. Patients taking cholines- c. The corticosteroid dose cannot be reduced due
terase inhibitors (ChEIs) every day with reasonable to symptom relapse.
evidence to support symptomatic benefit are therefore 3. Nonsteroidal IS agents that can be used in MG
excluded from this category. include azathioprine, cyclosporine, mycophenolate
3. Definition of ocular MG (based on dysfunction due to mofetil, methotrexate, and tacrolimus. The follow-
MG at a specified point in time, and not dependent upon the ing factors should be considered in selecting
duration of disease). MGFA Class I3: Any ocular muscle among these agents:
weakness. May have weakness of eye closure. a. There is widespread variation in practice with
Strength in all other facial, bulbar, and limb muscles respect to choice of IS agent since there is little
is normal. (It is recognized that some patients report literature comparing them.
fatigue when strength testing is normal. The physi- b. Expert consensus and some RCT evidence sup-
cian should use clinical judgment in attributing port the use of azathioprine as a first-line IS
fatigue to generalized MG in the absence of objec- agent in MG.
tive nonocular weakness). c. Evidence from RCTs supports the use of cyclo-
4. Definition of impending myasthenic crisis. Rapid clin- sporine in MG, but potential serious adverse
ical worsening of MG that, in the opinion of the effects and drug interactions limit its use.
treating physician, could lead to crisis in the short d. Although available RCT evidence does not sup-
term (days to weeks). port the use of mycophenolate and tacrolimus in
5. Definition of manifest myasthenic crisis (the concept of MG, both are widely used, and one or both are
crisis focuses on the clinical implicationsit represents a seri- recommended in several national MG treatment
ous, life-threatening, rapid worsening of MG and potential guidelines.47
airway compromise from ventilatory or bulbar dysfunction). 4. Patients with refractory MG should be referred to
MGFA Class V3: Worsening of myasthenic weakness a physician or a center with expertise in manage-
requiring intubation or noninvasive ventilation to ment of MG. In addition to the previously men-
avoid intubation, except when these measures are tioned IS agents, the following therapies may also
employed during routine postoperative management be used in refractory MG:
(the use of a feeding tube without intubation places a. Chronic IVIg and chronic PLEX (see IVIg and
the patient in MGFA Class IVB3). PLEX, no. 6);
6. Definition of refractory MG. PIS3 is unchanged or b. Cyclophosphamide;
worse after corticosteroids and at least 2 other IS c. Rituximab, for which evidence of efficacy is
agents, used in adequate doses for an adequate dura- building, but for which formal consensus could
tion, with persistent symptoms or side effects that limit not be reached.
functioning, as defined by patient and physician. 5. IS agent dosage and duration of treatment
Consensus guidance treatment statements. a. Once patients achieve treatment goals, the cor-
Symptomatic and IS treatment of MG. ticosteroid dose should be gradually tapered. In
1. Pyridostigmine should be part of the initial treat- many patients, continuing a low dose of cortico-
ment in most patients with MG. Pyridostigmine steroids long-term can help to maintain the
dose should be adjusted as needed based on symp- treatment goal.
toms. The ability to discontinue pyridostigmine can b. For nonsteroidal IS agents, once treatment goals
be an indicator that the patient has met treatment have been achieved and maintained for 6
goals and may guide the tapering of other therapies. months to 2 years, the IS dose should be tapered
Corticosteroids or IS therapy should be used in all slowly to the minimal effective amount. Dosage
patients with MG who have not met treatment goals adjustments should be made no more frequently
after an adequate trial of pyridostigmine. than every 36 months (table e-1).
Neurology 87 July 26, 2016 421
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
c. Tapering of IS drugs is associated with risk of in patients with significant respiratory or bulbar
relapse, which may necessitate upward adjust- dysfunction. Corticosteroids or other IS agents
ments in dose. The risk of relapse is higher in are often started at the same time to achieve a sus-
patients who are symptomatic, or after rapid taper. tained clinical response. (Because corticosteroids
d. It is usually necessary to maintain some immu- may cause transient worsening of myasthenic
nosuppression for many years, sometimes for weakness, it may be appropriate to wait several
life. days for PLEX or IVIg to have a beneficial effect
6. Patients must be monitored for potential adverse before starting corticosteroids).
effects and complications from IS drugs. Changing 3. Although clinical trials suggest that IVIg and PLEX
to an alternative IS agent should be considered if are equally effective in the treatment of impending
adverse effects and complications are medically sig- or manifest myasthenic crisis, expert consensus
nificant or create undue hardship for the patient. suggests that PLEX is more effective and works
more quickly. The choice between the 2 therapies
IVIg and PLEX.
depends on patient comorbidity (e.g., PLEX can-
1. PLEX and IVIg are appropriately used as short- not be used in sepsis and IVIg is contraindicated in
term treatments in patients with MG with life- hypercoagulable states, renal failure, or hypersensi-
threatening signs such as respiratory insufficiency tivity to immunoglobulin) and other factors,
or dysphagia; in preparation for surgery in patients including availability. A greater risk of hemody-
with significant bulbar dysfunction; when a rapid namic and venous access complications with PLEX
response to treatment is needed; when other treat- should also be considered in the decision (many
ments are insufficiently effective; and prior to complications of PLEX are related to route of
beginning corticosteroids if deemed necessary to access and may be minimized by using peripheral
prevent or minimize exacerbations. rather than central venous access).
2. The choice between PLEX and IVIg depends on
individual patient factors (e.g., PLEX cannot be Thymectomy in MG.
used in patients with sepsis and IVIg cannot be used 1. In non-thymomatous MG, thymectomy is per-
in renal failure) and on the availability of each. formed as an option to potentially avoid
3. IVIg and PLEX are probably equally effective in or minimize the dose or duration of immunother-
the treatment of severe generalized MG. apy, or if patients fail to respond to an initial trial of
4. The efficacy of IVIg is less certain in milder MG or immunotherapy or have intolerable side-effects
in ocular MG. from that therapy. Because of the long delay in
5. PLEX may be more effective than IVIg in MuSK- onset of effect, thymectomy for MG is an elective
MG. procedure. It should be performed when the
6. The use of IVIg as maintenance therapy can be con- patient is stable and deemed safe to undergo a pro-
sidered for patients with refractory MG or for those in cedure where postoperative pain and mechanical
whom IS agents are relatively contraindicated. factors can limit respiratory function.
2. The value of thymectomy in the treatment of pre-
Impending and
Impending and manifest myasthenic crisis.
pubertal patients with MG is unclear, but thymec-
manifest myasthenic crisis are emergent situations
tomy should be considered in children with
requiring aggressive management and supportive
generalized AChR antibodypositive MG:
care.
a. If the response to pyridostigmine and IS therapy
Although cholinergic crises are now rare, excessive
is unsatisfactory; or
ChEI cannot be completely excluded as a cause of
b. In order to avoid potential complications of IS
clinical worsening. Also, ChEIs increase airway secre-
therapy.
tions, which may exacerbate breathing difficulties.
PLEX and IVIg are the mainstay of management For children diagnosed with seronegative general-
in myasthenic crisis. ized MG, the possibility of a congenital myasthenic
syndrome or other neuromuscular condition should
1. Impending crisis requires hospital admission and
be entertained, and evaluation at a center specializing
close observation of respiratory and bulbar func-
in neuromuscular diseases is of value prior to
tion, with the ability to transfer to an intensive care
thymectomy.
unit if it progresses to manifest crisis. Myasthenic
crisis requires admission to an intensive care or 3. With rare exceptions, all patients with MG with
step-down unit to monitor for or manage respira- thymoma should undergo surgery to remove the
tory failure and bulbar dysfunction. tumor. Removal of the thymoma is performed to
2. PLEX and IVIg are used as short-term treatment rid the patient of the tumor and may not produce
for impending and manifest myasthenic crisis and improvement in MG. All thymus tissue should be
422 Neurology 87 July 26, 2016
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
removed along with the tumor. Further treatment MG in pregnancy.
of thymoma will be dictated by histologic classifi- 1. Planning for pregnancy should be instituted well in
cation and degree of surgical excision. Incom- advance to allow time for optimization of myasthenic
pletely resected thymomas should be managed clinical status and to minimize risks to the fetus.
after surgery with an interdisciplinary treatment 2. Multidisciplinary communication among relevant
approach (radiotherapy, chemotherapy). specialists should occur throughout pregnancy,
4. In elderly or multimorbid patients with thymoma, during delivery, and in the postpartum period.
palliative radiation therapy can be considered in 3. Provided that their myasthenia is under good con-
the appropriate clinical setting. Small thymomas trol before pregnancy, the majority of women can
may be followed without treatment unless they be reassured that they will remain stable through-
are enlarging or become symptomatic. out pregnancy. If worsening occurs, it may be
5. Endoscopic and robotic approaches to thymectomy more likely during the first few months after
are increasingly performed and have a good track delivery.
record for safety in experienced centers. Data from 4. Oral pyridostigmine is the first-line treatment dur-
randomized, controlled comparison studies are not ing pregnancy. IV ChEIs may produce uterine con-
available. Based on comparisons across studies, less tractions and should not be used during pregnancy.
invasive thymectomy approaches appear to yield 5. Thymectomy should be postponed until after preg-
similar results to more aggressive approaches. nancy as benefit is unlikely to occur during
6. Thymectomy may be considered in patients with pregnancy.
generalized MG without detectable AChR anti- 6. Chest CT without contrast can be performed safely
bodies if they fail to respond adequately to IS ther- during pregnancy, although the risks of radiation
apy, or to avoid/minimize intolerable adverse to the fetus need to be carefully considered. Unless
effects from IS therapy. Current evidence does there is a compelling indication, postponement of
not support an indication for thymectomy in pa- diagnostic CT until after delivery is preferable.
tients with MuSK, LRP4, or agrin antibodies. 7. Prednisone is the IS agent of choice during
Juvenile MG (see also Thymectomy in MG, no. 2).
pregnancy.
8. Current information indicates that azathioprine
1. Children with acquired autoimmune ocular MG
and cyclosporine are relatively safe in expectant
are more likely than adults to go into spontaneous
mothers who are not satisfactorily controlled with
remission. Thus, young children with only ocular
or cannot tolerate corticosteroids. Current evidence
symptoms of MG can be treated initially with pyr-
idostigmine. Immunotherapy can be initiated if indicates that mycophenolate mofetil and metho-
goals of therapy are not met. trexate increase the risk of teratogenicity and are
2. Children are at particular risk of steroid side effects, contraindicated during pregnancy. (These agents
including growth failure, poor bone mineralization, previously carried Food and Drug Administration
and susceptibility to infection, due in part to a delay [FDA] Category C (cyclosporine), D (azathioprine
in live vaccinations. Long-term treatment with cor- and mycophenolate mofetil), and X (methotrexate)
ticosteroids should use the lowest effective dose ratings. The FDA has recently discontinued this
to minimize side effects. rating system, and replaced it with a summary of
3. Maintenance PLEX or IVIg are alternatives to IS the risks of using a drug during pregnancy and
drugs in JMG. breastfeeding, along with supporting data and rel-
evant information to help health care providers
MG with MuSK antibodies. make prescribing and counseling decisions12).
1. Many patients with MuSK-MG respond poorly to Although this statement achieved consensus, there was
ChEIs, and conventional pyridostigmine doses fre- a strong minority opinion against the use of azathio-
quently induce side effects. prine in pregnancy. Azathioprine is the nonsteroidal
2. Patients with MuSK-MG appear to respond well to IS of choice for MG in pregnancy in Europe but is
corticosteroids and to many steroid-sparing IS considered high risk in the United States. This differ-
agents. They tend to remain dependent on predni- ence is based on a small number of animal studies and
sone despite concomitant treatment with steroid- case reports.
sparing agents. 9. PLEX or IVIg are useful when a prompt, although
3. MuSK-MG responds well to PLEX, while IVIg temporary, response is required during pregnancy.
seems to be less effective. Careful consideration of both maternal and fetal
4. Rituximab should be considered as an early thera- issues, weighing the risks of these treatments
peutic option in patients with MuSK-MG who have against the requirement for use during pregnancy
an unsatisfactory response to initial immunotherapy. and their potential benefits, is required.
Neurology 87 July 26, 2016 423
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
10. Spontaneous vaginal delivery should be the the manuscript for important intellectual content. I. Illa: acquisition
of data, critical revision of the manuscript for important intellectual
objective and is actively encouraged.
content. N. Kuntz: acquisition of data, drafting/revising the manuscript,
11. Magnesium sulfate is not recommended for critical revision of the manuscript for important intellectual content.
management of eclampsia in MG because of J.M. Massey: acquisition of data, drafting/revising the manuscript, crit-
its neuromuscular blocking effects; barbiturates ical revision of the manuscript for important intellectual content.
A. Melms: acquisition of data, critical revision of the manuscript for
or phenytoin usually provide adequate important intellectual content. H. Murai: acquisition of data, critical
treatment. revision of the manuscript for important intellectual content. J. Palace:
12. All babies born to myasthenic mothers should acquisition of data, drafting/revising the manuscript, critical revision of
the manuscript for important intellectual content. M. Nicolle: acquisi-
be examined for evidence of transient myas-
tion of data, drafting/revising the manuscript, critical revision of the
thenic weakness, even if the mothers myasthe- manuscript for important intellectual content. D.P. Richman: acquisi-
nia is well-controlled, and should have rapid tion of data, critical revision of the manuscript for important intellec-
access to neonatal critical care support. tual content. J. Verschuuren: acquisition of data, critical revision of the
manuscript for important intellectual content. P. Narayanaswami:
study concept and design, acquisition of data, analysis or interpretation
DISCUSSION We have developed international guid- of data, drafting/revising the manuscript, critical revision of the man-
ance statements for the management of JMG and uscript for important intellectual content, study supervision.
adult MG. We utilized recent national guidelines and
a regional European guideline to assemble a foundation ACKNOWLEDGMENT
of literature, supplementing their comprehensive litera- The authors thank MGFA Board member Jurgen Venitz, MD, PhD, for
providing insight from the patients perspective.
ture reviews with additional articles identified by panel-
ists. After reaching agreement on the treatment goals,
a 3-round anonymous modified Delphi voting process STUDY FUNDING
Supported by a grant from the Myasthenia Gravis Foundation of America
was used to obtain consensus on guidance statements. (MGFA).
A limitation of consensus-based processes is that
subconscious or conscious selection of like-minded DISCLOSURE
panel members may result in opinions that are not rep- D. Sanders: consultant for Accordant Health Services, Cytokinetics,
resentative of MG experts. This issue was addressed by GlaxoSmithKline, and Jacobus Pharmaceutical Co. G. Wolfe: advisory
board for Grifols, Baxter, CSL Behring, and Syntimmune; and research
selecting an international panel with variations in prac-
support from Alexion. M. Benatar: research support from the FDA
tice and by using a formal consensus process. (R01FD003710), NIH (U01NS084495), and Alexion. A. Evoli: scien-
Recognizing the variability of practice patterns and tific award jury member for Grifols. N. Gilhus: speakers honoraria from
availability of treatment modalities, these statements Octopharma, Baxter, and Merck Serono. I. Illa: research funding from
Grifols and speaking fees and travel grants from Genzyme and Pfizer; and
are not absolute recommendations for management, consultant for Alexion, UCB, and Grifols. N. Kuntz and J. Massey report
but are intended as a guide for the clinician. They no disclosures relevant to the manuscript. A. Melms: advisory board,
are also not intended for establishing payment poli- UCB. H. Murai: research funding from Biogen, Novartis, Bayer, Tanabe
Mitsubishi, and the Japan Blood Products Organization. J. Palace: con-
cies or drug tiering by payers.
sultant for Merck Serono, Biogen Idec, Novartis, Teva, Chugai Pharma,
This is a living document that will require updates Alexion, and Bayer Schering; research funding from Merck Serono, No-
as the MG treatment theater continues to evolve. vartis, Biogen Idec, and Bayer Schering. M. Nicolle reports no disclosures
Despite the limitations of consensus-based methods, relevant to the manuscript. D. Richman: research funding from the
Muscular Dystrophy Association, Myasthenia Gravis Foundation of
these guidance statements reflect an up-to-date expert
California, and the Myasthenia Gravis Foundation of Illinois. J. Verschuuren:
consensus to guide clinicians worldwide who strive to research support by NIH, FP7 European grant (#602420), consultant for
optimize function and quality of life for their patients Tyr pharma, and arGEN-X. The LUMC receives royalties from IBL for
with MG, especially for those who practice in parts of antibody tests. P. Narayanaswami: serves on the Medical and Scientific
Advisory Board, Myasthenia Gravis Foundation of America (MGFA),
the world that do not have the resources to develop and Medical Advisory Board, MGFA, New England Chapter. Go to
local treatment guidelines. Any future trial of treat- Neurology.org for full disclosures.
ment that provides relevant information will merit
review of these guidance statements. Received August 25, 2015. Accepted in final form February 19, 2016.
REFERENCES
AUTHOR CONTRIBUTIONS 1. Deenen JCW, Horlings CGC, Verschuuren JJGM,
D.B. Sanders: study concept and design, grant application and manage- Verbeek ALM. The epidemiology of neuromuscular
ment, acquisition of data, analysis or interpretation of data, drafting/ disorders: a comprehensive overview of the literature.
revising the manuscript, critical revision of the manuscript for important J Neuromuscul Dis 2015;2:7385.
intellectual content, study supervision. G.I. Wolfe: study concept and
2. Grob D, Brunner NG, Namba T, Pagala M. Lifetime course
design, acquisition of data, analysis or interpretation of data, drafting/
of myasthenia gravis. Muscle Nerve 2008;37:141149.
revising the manuscript, critical revision of the manuscript for important
intellectual content, study supervision. M. Benatar: acquisition of data,
3. Jaretzki A III, Barohn RB, Ernstoff RM, et al. Myasthenia
drafting/revising the manuscript, critical revision of the manuscript for gravis: recommendations for clinical research standards:
important intellectual content. A. Evoli: acquisition of data, drafting/ Task Force of the Medical Scientific Advisory Board
revising the manuscript, critical revision of the manuscript for important of the Myasthenia Gravis Foundation of America.
intellectual content. N.E. Gilhus: acquisition of data, critical revision of Neurology 2000;55:1623.
424 Neurology 87 July 26, 2016
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
4. Wiendl H. Diagnostik und Therapie der Myasthenia gravis working group. J Neurol Neurosurg Psychiatry 2014;85:
und des Lambert-Eaton-Syndroms [online]. Available at: 538543.
http://www.dgn.org/leitlinien/11-leitlinien-der-dgn/3005-ll- 9. Skeie GO, Apostolski S, Evoli A, et al. Guidelines for
68-ll-diagnostik-und-therapie-der-myasthenia-gravis-und- treatment of autoimmune neuromuscular transmission
des-lambert-eaton-syndroms. Accessed August 14, 2015. disorders. Eur J Neurol 2010;17:893902.
5. Fuhr P, Gold R, Hohlfeld R, et al. Diagnostik und 10. Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/U-
therapie der myasthenia gravis und des Lambert-Eaton Syn- CLA Appropriateness Method Users Manual. Santa
droms. In: Diener HC, Weimar C, Deuschl G, et al, eds. Monica, CA: RAND Corporation; 2001.
Leitlinien fr Diagnostik und Therapie in der Neurologie, 11. US Department of Health and Human Services. Common
5th ed. Stuttgart: Thieme; 2012:830856. Terminology Criteria for Adverse Events (CTCAE) v4.03
6. Murai H. Japanese clinical guidelines for myasthenia gravis: [online]. Available at: http://evs.nci.nih.gov/ftp1/CTCAE/
putting into practice. Clin Exp Neuroimmunol 2015;6:2131. CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf.
7. Sussman J, Farrugia ME, Maddison P, Hill M, Leite MI, Accessed May 25, 2016.
Hilton-Jones D. Myasthenia gravis: association of British 12. US Food and Drug Administration. Pregnancy and Lactation
Neurologists management guidelines. Pract Neurol 2015; Final Rule [online]. Available at: http://www.fda.gov/Drugs/
15:199206. DevelopmentApprovalProcess/DevelopmentResources/
8. Norwood F, Dhanjal M, Hill M, et al. Myasthenia in preg- Labeling/ucm093307.htm. Accessed November 11,
nancy: best practice guidelines from a UK multispecialty 2015.
This Weeks Neurology Podcast
International consensus guidance for management of myasthenia
gravis: Executive summary (see p. 419)
This podcast begins and closes with Dr. Robert Gross, Editor-in-
Chief, briefly discussing highlighted articles from the July 26,
2016, issue of Neurology. In the second segment, Dr. Ted Burns
talks with Dr. Donald Sanders about the international consensus
guidance for the management of myasthenia gravis. Dr. Ilena
George reads the e-Pearl of the week about progressive multifocal
leukoencephalopathy. Dr. Tesha Monteith focuses his interview
with Dr. Richard Lipton on his Neurology Year in Review plenary
session at the AAN Annual Meeting discussing headache.
Disclosures can be found at Neurology.org.
At Neurology.org, click on RSS in the Neurology Podcast box to listen to the most recent
podcast and subscribe to the RSS feed.
CME Opportunity: Listen to this weeks Neurology Podcast and earn 0.5 AMA PRA Category
1 CME Credits by answering the multiple-choice questions in the online Podcast quiz.
Get Connected. Stay Connected.
Connect with the American Academy of Neurologys popular social media channels to stay up-to-
date on the latest news and breakthroughs in neurology, and network with peers and neurology
thought leaders. Visit AAN.com/Connect.
Neurology 87 July 26, 2016 425
2016 American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Neuropharmacotherapy in Critical IllnessFrom EverandNeuropharmacotherapy in Critical IllnessGretchen BrophyNo ratings yet
- International Consensus Guidance For Management of Myasthenia GravisDocument8 pagesInternational Consensus Guidance For Management of Myasthenia GravisWindy SengiNo ratings yet
- International Concensus Guidelines MGDocument9 pagesInternational Concensus Guidelines MGWinsome Chloe Rara-BuñoNo ratings yet
- International Consensus Guidance For Management of Myasthenia GravisDocument10 pagesInternational Consensus Guidance For Management of Myasthenia GravisChon ChiNo ratings yet
- Developing Treatment Guidelines For Myasthenia GravisDocument7 pagesDeveloping Treatment Guidelines For Myasthenia GravismoneurNo ratings yet
- Practice Guideline Update Summary: Vaccine-Preventable Infections and Immunization in Multiple SclerosisDocument13 pagesPractice Guideline Update Summary: Vaccine-Preventable Infections and Immunization in Multiple SclerosisChon ChiNo ratings yet
- Nihms 818661Document40 pagesNihms 818661cloudxsimplifyNo ratings yet
- Meningiomas: Knowledge Base, Treatment Outcomes, and Uncertainties. A RANO ReviewDocument20 pagesMeningiomas: Knowledge Base, Treatment Outcomes, and Uncertainties. A RANO ReviewLuwiNo ratings yet
- ECAM2013 Trat FMSDocument7 pagesECAM2013 Trat FMStxankleroNo ratings yet
- Molecular TherapeuticDocument14 pagesMolecular TherapeuticGiselle Vasquez LuceroNo ratings yet
- MOCA PEDS 2021 Required ReadingDocument26 pagesMOCA PEDS 2021 Required Readingerica100% (1)
- EuroMyasthenia Newsletter 18 FinalDocument11 pagesEuroMyasthenia Newsletter 18 FinalMaria NigelNo ratings yet
- Weller Et Al-2021-Nature Reviews Clinical OncologyDocument17 pagesWeller Et Al-2021-Nature Reviews Clinical OncologyRaul Matute MartinNo ratings yet
- 2016 AHS Manejo de Migraña en EMGDocument30 pages2016 AHS Manejo de Migraña en EMGSolange Vargas LiclaNo ratings yet
- NeurologyDocument11 pagesNeurologyCarlos PonceNo ratings yet
- Guideline TBI BTF Edisi 4Document10 pagesGuideline TBI BTF Edisi 4Franklin L. SinanuNo ratings yet
- Characterizing Opioid Use in A US Population With MigraineDocument12 pagesCharacterizing Opioid Use in A US Population With MigraineVagner PinheiroNo ratings yet
- Considerations For Development of Therapies For Cutaneous NeurofibromaDocument11 pagesConsiderations For Development of Therapies For Cutaneous NeurofibromanadilaayukarisaNo ratings yet
- EANO Guideline On The Diagnosis and Management ofDocument14 pagesEANO Guideline On The Diagnosis and Management ofJames E. WalkerNo ratings yet
- Sturge Weber GuidelineDocument18 pagesSturge Weber Guidelinemartin.ruda93No ratings yet
- Pi Is 002561961500378 XDocument12 pagesPi Is 002561961500378 XTatiana IonascuNo ratings yet
- 2017 Treatment Outcomes for Metastatic Melanoma of Unknown Primary in the New Era- A Single-Institution Study and Review of the LiteratureDocument10 pages2017 Treatment Outcomes for Metastatic Melanoma of Unknown Primary in the New Era- A Single-Institution Study and Review of the LiteratureAndrés WunderwaldNo ratings yet
- Anticonvulsant Prophylaxis Brin Tumors 2000Document10 pagesAnticonvulsant Prophylaxis Brin Tumors 2000Mariajose RubalcavaNo ratings yet
- Psychopharmacological Options For Adult Patients WDocument2 pagesPsychopharmacological Options For Adult Patients WViviana DuarteNo ratings yet
- AACE2013 HyperthyroidylDocument65 pagesAACE2013 HyperthyroidylHan KethyanethNo ratings yet
- Niemann 37Document19 pagesNiemann 37banitavlad5No ratings yet
- Massage For Mechanical Neck Disorders: A Systematic ReviewDocument10 pagesMassage For Mechanical Neck Disorders: A Systematic ReviewOana RuxandraNo ratings yet
- Howard JF Et Al Lancet Neurology 2021 ADAPT Publication With SupplementDocument34 pagesHoward JF Et Al Lancet Neurology 2021 ADAPT Publication With SupplementSusana RocheNo ratings yet
- Dongsheng Duan, Jerry R. Mendell - Muscle Gene Therapy-Springer International Publishing (2019)Document804 pagesDongsheng Duan, Jerry R. Mendell - Muscle Gene Therapy-Springer International Publishing (2019)Sorin DinuNo ratings yet
- Neurosurg Focus Article Pe14Document7 pagesNeurosurg Focus Article Pe14jojost14No ratings yet
- NEUROLOGY2014621771Document13 pagesNEUROLOGY2014621771Alexandra SerbanNo ratings yet
- Renal GIDocument1 pageRenal GIBryan NguyenNo ratings yet
- Dialnet AprovechamientoDeResiduosOrganicosAgricolasYForest 5633579 PDFDocument15 pagesDialnet AprovechamientoDeResiduosOrganicosAgricolasYForest 5633579 PDFEDGAR DÍAZ URDANETANo ratings yet
- Thoracic Spine Manipulation For The Management of Mechanical Neck Pain: A Systematic Review and Meta-AnalysisDocument28 pagesThoracic Spine Manipulation For The Management of Mechanical Neck Pain: A Systematic Review and Meta-AnalysisskNo ratings yet
- Maas 2007Document11 pagesMaas 2007Caroline FelicianoNo ratings yet
- Mercuri 2017Document13 pagesMercuri 2017akshayajainaNo ratings yet
- Systemic Immunomodulating Therapies For Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis A Systematic Review and Meta-AnalysisDocument9 pagesSystemic Immunomodulating Therapies For Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis A Systematic Review and Meta-AnalysisSri DarmayaniNo ratings yet
- Multiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkDocument11 pagesMultiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkasasakopNo ratings yet
- 1Document11 pages1Valentina Cortes MoralesNo ratings yet
- Sugammadex For Reversal of Rocuronium-Induced Neuromuscular Blockade in Pediatric PatientsDocument7 pagesSugammadex For Reversal of Rocuronium-Induced Neuromuscular Blockade in Pediatric PatientsAllonsiny GutierrezNo ratings yet
- Consensus Evidence-Based Clinical Practice Recommendations For The Management of FibromyalgiaDocument11 pagesConsensus Evidence-Based Clinical Practice Recommendations For The Management of FibromyalgiaLisa GonçalvesNo ratings yet
- Epilepsia - 2021 - Rosenow - Relative Importance of Clinical Outcomes and Safety Risks of Antiseizure MedicationDocument12 pagesEpilepsia - 2021 - Rosenow - Relative Importance of Clinical Outcomes and Safety Risks of Antiseizure MedicationririsNo ratings yet
- A Systematic Review of Treatments For Mild Traumatic Brain InjuryDocument3 pagesA Systematic Review of Treatments For Mild Traumatic Brain InjurySergio Machado NeurocientistaNo ratings yet
- 9.1 An Approach To Identifying Headache Patients That Require Neuroimaging (Curr, Inst and Pedagogy 2019)Document6 pages9.1 An Approach To Identifying Headache Patients That Require Neuroimaging (Curr, Inst and Pedagogy 2019)Katherine RodríguezNo ratings yet
- Ref 1Document7 pagesRef 1Tiago BaraNo ratings yet
- A Narrative Review of Defensive Medical Practice in PsychiatryDocument1 pageA Narrative Review of Defensive Medical Practice in PsychiatryyehfanweiNo ratings yet
- Persistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisDocument16 pagesPersistence and Switching Patterns of Oral Migraine Prophylactic Medications Among Patients With Chronic Migraine: A Retrospective Claims AnalysisAzam alausyNo ratings yet
- Brain Cancer Progression A Retrospective.7Document9 pagesBrain Cancer Progression A Retrospective.7Hamzeh AlsalhiNo ratings yet
- 1 s2.0 S0272638617307813 MainDocument18 pages1 s2.0 S0272638617307813 MainArtivoNo ratings yet
- Mills & Tamnes, 2014.methods and Considerations For Longitudinal Structural Brain Imaging Analysis Across DevelopmentDocument10 pagesMills & Tamnes, 2014.methods and Considerations For Longitudinal Structural Brain Imaging Analysis Across DevelopmentSu AjaNo ratings yet
- Formolo D. A., Et Al. (2019) - Deep Brain Stimulation For Obesity ReviewDocument13 pagesFormolo D. A., Et Al. (2019) - Deep Brain Stimulation For Obesity ReviewHiago MeloNo ratings yet
- NeurosurgeryDocument9 pagesNeurosurgeryGiuseppe CampanaNo ratings yet
- Risma 3Document17 pagesRisma 3Safira Sal SabillaNo ratings yet
- Effectiveness of Global Postural Re-Education For Treatment of Spinal Disorders A Meta-AnalysisDocument10 pagesEffectiveness of Global Postural Re-Education For Treatment of Spinal Disorders A Meta-AnalysisraquelbibiNo ratings yet
- Neurocrit Care-Critical Care Management of Patients Following ASHDocument30 pagesNeurocrit Care-Critical Care Management of Patients Following ASHEyE UVNo ratings yet
- SaudiJKidneyDisTranspl22110-3529284 094812Document8 pagesSaudiJKidneyDisTranspl22110-3529284 094812shiloinNo ratings yet
- Diagnosis and Management of Spinal Muscular Atrophy: Part 1: Recommendations For Diagnosis, Rehabilitation, Orthopedic and Nutritional CareDocument13 pagesDiagnosis and Management of Spinal Muscular Atrophy: Part 1: Recommendations For Diagnosis, Rehabilitation, Orthopedic and Nutritional CareValentina GiraldoNo ratings yet
- Neuro OncologyDocument10 pagesNeuro OncologylarissaNo ratings yet
- Clinical Policy For The Initial Approach To Patients Presenting With A Chief Complaint of Seizure Who Are Not in Status EpilepticusDocument19 pagesClinical Policy For The Initial Approach To Patients Presenting With A Chief Complaint of Seizure Who Are Not in Status EpilepticusVivin KarlinaNo ratings yet
- Palliative care and end-of-life care in adults with malignant brain tumorsDocument10 pagesPalliative care and end-of-life care in adults with malignant brain tumorsLaras Adythia PratiwiNo ratings yet
- Vaccinations For ChildrenDocument6 pagesVaccinations For Childrenapi-358040298No ratings yet
- CefuroximeDocument14 pagesCefuroximeBentoys StreetNo ratings yet
- Xylocaine Jelly Cil enDocument4 pagesXylocaine Jelly Cil enRavi KumarNo ratings yet
- Adverse Effects of FillersDocument9 pagesAdverse Effects of FillersElizabeth TovittoNo ratings yet
- Case Report TBDocument3 pagesCase Report TBNurul Izzati Mohd HanifiahNo ratings yet
- Iop-Lowering Medication Review: How To Address Face Mask-Associated Dry EyeDocument36 pagesIop-Lowering Medication Review: How To Address Face Mask-Associated Dry EyeEklas RahmanNo ratings yet
- Patient Charter-DMAI NABHDocument3 pagesPatient Charter-DMAI NABHMoin MedicansNo ratings yet
- The Drug Development ProcessDocument7 pagesThe Drug Development ProcessSACHIN BHASKAR NARKHEDE100% (1)
- False UnicornDocument3 pagesFalse UnicornNutrimakeNo ratings yet
- Naranjo AlgorithmDocument3 pagesNaranjo AlgorithmmilkymilkyNo ratings yet
- DR Drug StudyDocument6 pagesDR Drug Studyslashmortred100% (5)
- Appebon With IronDocument2 pagesAppebon With IronLindsay Grace MandarioNo ratings yet
- Health - November 2015Document116 pagesHealth - November 2015alejandronealNo ratings yet
- NCP - FatigueDocument3 pagesNCP - Fatigueitsmeaya100% (1)
- The Edom PharmacDocument90 pagesThe Edom PharmackhoachiNo ratings yet
- Chapter 4: Implementing The Pharmacists' Patient Care ProcessDocument15 pagesChapter 4: Implementing The Pharmacists' Patient Care ProcessLouise TheunisNo ratings yet
- Fucidin (R) OintmentDocument4 pagesFucidin (R) OintmentAmy AdamsNo ratings yet
- IV Therapy Course Outline for Licensed Practical NursesDocument34 pagesIV Therapy Course Outline for Licensed Practical NursesEleganceinblk0% (1)
- Root Cause in Healthcare PDFDocument28 pagesRoot Cause in Healthcare PDFcpears56100% (2)
- Concept Map Case Study E2Document5 pagesConcept Map Case Study E2api-283004290No ratings yet
- Chapter 16 - Oncology - Nursing Management in Cancer CareDocument10 pagesChapter 16 - Oncology - Nursing Management in Cancer CareSavanna Chambers100% (2)
- Assignment 02 PharmacologyDocument4 pagesAssignment 02 PharmacologyOink TopusNo ratings yet
- DDC MA Nursing - Input Process Output ModelDocument15 pagesDDC MA Nursing - Input Process Output ModelBlaiseNo ratings yet
- Structured Observation Guide for Drug Use StudiesDocument16 pagesStructured Observation Guide for Drug Use Studiesisele1977No ratings yet
- Ivermectin ResearchDocument9 pagesIvermectin ResearchMohd Adam0% (1)
- Listening Mark Scheme: Question Answer Question AnswerDocument10 pagesListening Mark Scheme: Question Answer Question AnswerlilalilakNo ratings yet
- Assignment 1 - PHARMACOLOGYDocument4 pagesAssignment 1 - PHARMACOLOGYJewel SebastianNo ratings yet
- Health Risks of Drinking Hibiscus TeaDocument4 pagesHealth Risks of Drinking Hibiscus TeaAishwarya BharathNo ratings yet
- Adverse Drug Interaction in Dental PracticeDocument8 pagesAdverse Drug Interaction in Dental PracticeSusanna TsoNo ratings yet
- The Cancer Solution by DR ROBERT E. WILLNER M.D., Ph.D.Document210 pagesThe Cancer Solution by DR ROBERT E. WILLNER M.D., Ph.D.johnscu912396% (26)