Professional Documents
Culture Documents
Multiple Sclerosis Progression Time For A New Mechanism-Driven Framework
Uploaded by
asasakopOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Multiple Sclerosis Progression Time For A New Mechanism-Driven Framework
Uploaded by
asasakopCopyright:
Available Formats
Personal View
Multiple sclerosis progression: time for a new
mechanism-driven framework
Tanja Kuhlmann, Marcello Moccia, Timothy Coetzee*, Jeffrey A Cohen*, Jorge Correale*, Jennifer Graves, Ruth Ann Marrie*, Xavier Montalban*,
V Wee Yong, Alan J Thompson,* Daniel S Reich,* on behalf of the International Advisory Committee on Clinical Trials in Multiple Sclerosis†
Lancet Neurol 2023; 22: 78–88 Traditionally, multiple sclerosis has been categorised by distinct clinical descriptors—relapsing-remitting, secondary
Published Online progressive, and primary progressive—for patient care, research, and regulatory approval of medications.
November 18, 2022 Accumulating evidence suggests that the clinical course of multiple sclerosis is better considered as a continuum,
https://doi.org/10.1016/
with contributions from concurrent pathophysiological processes that vary across individuals and over time. The
S1474-4422(22)00289-7
apparent evolution to a progressive course reflects a partial shift from predominantly localised acute injury to
See Comment page 6
widespread inflammation and neurodegeneration, coupled with failure of compensatory mechanisms, such as
*Current or former member
of the International Advisory
neuroplasticity and remyelination. Ageing increases neural susceptibility to injury and decreases resilience. These
Committee on Clinical Trials observations encourage a new consideration of the course of multiple sclerosis as a spectrum defined by the relative
in Multiple Sclerosis contributions of overlapping pathological and reparative or compensatory processes. New understanding of key
†Members of the committee mechanisms underlying progression and measures to quantify progressive pathology will potentially have important
not listed here as authors are and beneficial implications for clinical care, treatment targets, and regulatory decision-making.
listed in the appendix
Institute of Neuropathology,
University Hospital Münster,
Introduction factors, including sex, age, social and environmental
Münster, Germany Multiple sclerosis is an immune-mediated disease of the exposures, genetic factors, and disease duration.13,14
(Prof T Kuhlmann MD); CNS. The heritability of multiple sclerosis risk is Since the introduction of the Lublin–Reingold descrip
Neuroimmunology Unit, approximately 25%, with the remainder of susceptibility tors, there have been calls for development of a disease
Montreal Neurological Institute,
attributed to environmental, epigenetic, and gene–gene classification more rooted in the biological mechanisms of
McGill University, Montreal, QC,
Canada (Prof T Kuhlmann); or gene–environment interactions.1 The International multiple sclerosis. As a first step in this direction, the
Multiple Sclerosis Clinical Care Advisory Committee on Clinical Trials in Multiple International Advisory Committee on Clinical Trials in
and Research Centre, Sclerosis (appendix) categorised clinical course descriptors Multiple Sclerosis focused on clarifying the 1996 and
Department of Neurosciences,
Federico II University of Naples,
(commonly referred to as the Lublin–Reingold 2013 clinical course descriptors.15 The committee has since
Naples, Italy (M Moccia MD); classification) in 1996, with a revision in 2013.2,3 The made an effort to examine the current clinical course
National Multiple Sclerosis committee defined three clinical courses: relapsing- descriptors more compre hensively, with the goal of
Society (USA), New York, NY, remitting (acute attacks followed by recovery), primary determining an approach to development of a new
USA (T Coetzee PhD);
Department of Neurology,
progressive (gradual worsening from onset), and framework for describing the disease.16–18 Herein, we
Mellen Center for Multiple secondary progressive (relapsing-remitting at onset but present concepts and results relevant to the pathophysiology
Sclerosis Treatment and gradual worsening later in the disease course). The of injury and compen satory mechanisms in multiple
Research, Neurological Institute, descriptors provided consistency in defining patient sclerosis and summarise the tools that can be used in
Cleveland Clinic, Cleveland, OH,
USA (Prof J A Cohen MD); Fleni,
groups for natural history studies, enhanced homogeneity clinical practice, clinical trials, and research to identify the
Department of Neurology, in clinical trials, and greatly improved communication spectrum of multiple sclerosis pathology and clinical
Buenos Aires, Argentina between clinicians and patients.2,3 In the 2013 revision, progression. We consider knowledge gaps in identifying
(Prof J Correale MD); Institute of clinical and radiological disease activity and progression injury and failure of compensatory mech anisms and
Biological Chemistry and
Biophysics (IQUIFIB), CONICET/
were introduced as modifiers of the basic clinical courses indicate how these gaps could be addressed. We suggest
UBA, Buenos Aires, Argentina to better reflect treatment-relevant aspects of the disease, that clinical characterisation and treatment selection
(Prof J Correale MD); Department such as relapses.3 These refinements were incorporated should be guided by identification of disease-driving
of Neurosciences, University of into trials that led to the first approvals of drugs for pathophysiological mechanisms rather than the traditional
California, San Diego, CA, USA
(J Graves MD); Max Rady College
progressive multiple sclerosis (eg, the approval of clinical descriptors. This approach lays the groundwork for
of Medicine, Rady Faculty of siponimod for patients with active secondary progressive a future consensus-based clas sification that would
Health Sciences, University of multiple sclerosis).4,5 transform drug discovery and improve patient care.
Manitoba, Winnipeg, MB,
It seems clear now that disability progression is neither
Canada (Prof R A Marrie MD);
Multiple Sclerosis Centre dichotomous nor genetically determined.6 Rather, Mechanisms of injury
of Catalonia and Department of accumulating data suggest that patients with multiple Non-resolving inflammation
Neurology-Neuroimmunology, sclerosis share qualitatively similar (but quantitatively Focal inflammatory demyelination in the white matter is a
Hospital Universitari Vall
different) pathology features independent of clinical stereotyped process characterised by perivenular
d’Hebron, Universitat
Autònoma de Barcelona, course, including inflammation and neurodegeneration, inflammation, involving both adaptive and innate immune
Barcelona, Spain both of which are already present at disease onset.7–10 In cells, a parenchymal astrocytic and microglial reaction,
(Prof X Montalban MD); line with this observation, in patients with relapsing-onset blood–brain barrier opening, a wave of demyelination
Hotchkiss Brain Institute
multiple sclerosis, a substantial proportion of disability manifested over the course of days to weeks (sometimes
(Prof V W Yong PhD) and
Department of Clinical progression is independent from relapses.11,12 Differences corresponding to clinical relapse), and a phase of tissue
Neurosciences in disease expression can be driven by patient-specific repair that typically lasts weeks to months.19 Focal
78 www.thelancet.com/neurology Vol 22 January 2023
Personal View
Active Gadolinium Meningeal Leptomeningeal
lesions enhancement inflammation and gadolinium
and fibrosis enhancement
7-tesla gradient-
Subpial lesions echo MRI
Acute axonal Neurofilament light
damage chain in blood and CSF
Neuronal and Functional
synaptic pathology MRI
Remyelination 7-tesla T1 mapping Diffuse white PET (translocator
matter protein 18
inflammation kilodaltons)
Iron rim Paramagnetic rim
lesion
Axonal loss and Optical coherence
ence
inflammation tomography and
(optic nerve) visual evoked
potentials
Global and segmental atrophy
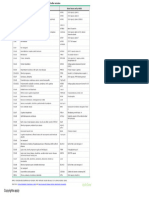
Figure 1: Mechanisms of injury and compensation and associated measures in multiple sclerosis
Early in the disease (left side of the figure), injury caused by focal lesions and associated axon damage can be compensated for by mechanisms such as remyelination. Over time, lesions in the grey and
white matter and axon damage accumulate; meningeal inflammation, diffuse microglial activation in the extralesional white matter, and slow expansion of existing lesions also become more
prominent (right side). Progression is further driven by decreased remyelination capacity and damage to neuronal networks mediated by loss of neurons and synapses. Ongoing low-level
inflammation and loss of compensatory mechanisms result in segmental and global atrophy. The histological panel depicting the optic nerve shows axon neurofilaments, whereas the inset shows
CD68+ myeloid cells. The visual evoked potential trace depicts delayed latency, indicating slow conduction related to demyelination. Neuronal and synaptic pathology can be detected by reduced
staining for NeuN, a marker for neurons (panel), and synaptophysin, a marker for synapses. The blue lines in the radiological image symbolise neuronal connectivity as detected by functional MRI.
Green arrows indicate radiological correlates of histopathological findings.
inflammation can be observed as gadolinium enhancement lesions can be detected using susceptibility-based MRI.20
on MRI, which allows identification of active disease In approximately one-quarter of lesions, inflammation can
(figure). The perivenular topography of focal inflammatory resolve despite the absence of adequate tissue repair,
www.thelancet.com/neurology Vol 22 January 2023 79
Personal View
(Prof V W Yong PhD), University leaving behind an astroglial scar.21 Residua of these tertiary lymphoid structures.48 Many (but not all) post-
of Calgary, Calgary, AB, Canada; processes can be detected in vivo using T2-weighted mortem studies have shown a spatial correspondence
Queen Square Multiple Sclerosis
Centre, Department of
hyperintensity on MRI; T1-weighted hypointensity ensues between demyelination of the underlying subpial cortex
Neuroinflammation, UCL in the case of loss of neuropil (black holes; table). and leptomeningeal inflammatory aggregates, which are
Queen Square Institute of Abrogation of new MRI lesions is a cornerstone for more prevalent in patients who had clinically progressive
Neurology, NIHR University assessing response to treatments that aim to block multiple multiple sclerosis than in those with non progressive
College London Hospitals
Biomedical Research Centre,
sclerosis relapses but has little value in predicting the clinical features.49 Despite the advent of MRI-based
Faculty of Brain Sciences, benefit of therapy for slowing of clinical progression; approaches that can identify some current or previous
University College London, however, as discussed in the next section, the residua of areas of leptomeningeal inflammation due to
London, UK focal inflammatory demyelination have emerged as key accompanying abnormalities in the blood–meningeal
(Prof A J Thompson MD);
Translational Neuroradiology
contributors to that progression.12,37,38 barrier, such techniques could reflect post-inflammatory
Section, National Institute of The existence of an ongoing intrathecal immune fibrosis and therefore are not sufficiently robust to quantify
Neurological Disorders and response is usually shown at the time of diagnosis by the accumulation of leptomeningeal inflammation over time.
Stroke, National Institutes of presence of CNS-specific oligoclonal bands.39 In the Finally, diffuse microglial activation and multifocal
Health, Bethesda, MD, USA
(Prof D S Reich MD)
acute phase, activation of microglia and infiltrates of microglial nodules in the extralesional white matter have
Correspondence to:
macrophages and lymphocytes accompany demyelination been reported in post-mortem tissue from patients with
Prof Tanja Kuhlmann, Institute and plaque formation.40,41 However, these inflammatory multiple sclerosis, especially in patients who had
of Neuropathology, University mechanisms do not resolve in approximately 20% of progressive multiple sclerosis (figure 1).10,50 The causes
Hospital Münster, lesions.19 Inflammation becomes more organised, as and consequences of this diffuse (and occasionally
48149 Münster, Germany
tanja.kuhlmann@
evidenced by accumulation of tissue-resident CD8+ profound) microglial activation are poorly understood.
ukmuenster.de memory cells and monocyte populations fostering Similarly, whether microglial nodules represent areas
or inflammatory changes in brain-resident cells (astrocytes of incipient but aborted focal demyelination, reaction to
Prof Daniel S Reich, Translational and microglia), and chronic tissue damage and local tissue perturbation, or something else, is unclear.51
Neuroradiology Section, remodelling.9,40,42 These characteristics are especially PET studies using radioligands that bind to activated
National Institute of prominent in mixed active and inactive lesions, a recent microglia and astrocytes have provided some in vivo
Neurological Disorders and
term that subsumes previous descriptions of chronic evidence for widespread microglial involvement,
Stroke, National Institutes of
Health, Bethesda 20892, MD, active, smouldering, and slowly expanding lesions; many although data generated by these scans are often noisy,
USA (but not all) such lesions are identifiable on high-field MRI spatial localisation is poor, and cellular specificity is
daniel.reich@nih.gov because they accumulate iron-laden phagocytes at the edge imperfect (table).52 These same PET radioligands can
See Online for appendix of the lesion, bordering the normal-appearing white matter identify some mixed active and inactive white matter
(the so-called paramagnetic rim sign; figure 1).19,43 In vivo lesions and have been used for this purpose in clinical
MRI studies have confirmed speculations based on post- trials.53–55 Given the new appreciation of the extent of glial
mortem studies that paramagnetic rim lesions can enlarge and neuronal heterogeneity in the CNS, an important
slowly into previously healthy perilesional tissue, mani research goal is to improve the cellular specificity of
festing as low-grade demyeli nation and transection of molecular imaging techniques.
axons passing through or near lesions.43,44 Axon transection Non-resolving inflammation not only drives injury but
results in retrograde and anterograde axon degeneration, might also prevent repair. An open and crucial question
with potentially detri mental effects on separate but is whether inflammation needs to resolve before tissue
anatomically connected areas of the brain. Therefore, it is repair can commence. The development of sensitive and
not surprising that having a large number of paramagnetic specific non-invasive imaging markers that detect non-
rim lesions is associated with accelerated disability resolving inflammation, such as the paramagnetic rim
accumulation.44 Data show that the paramagnetic rim sign sign, along with future development of robust CSF and
can disappear over a period of years, raising the possibility blood biomarkers of the same processes, might allow
that chronic focal white matter inflammation might be this question to be answered. Similar approaches could
susceptible to therapeutic modulation.45,46 Changes in elucidate the importance of non-resolving inflammation,
paramagnetic rim lesions are included as outcome for clinical progression of multiple sclerosis and any
measures in ongoing and newly designed multiple potential group or individual effect on that inflammation
sclerosis clinical trials as potential correlates or predictors of existing or future disease-modifying therapies.
of multiple sclerosis progression and response to therapy.
A separate MRI approach combines data from the entire Neurodegeneration
time course of a clinical trial to capture the slow Inflammation is closely linked to axon and neuron injury
enlargement of multiple sclerosis lesions (so-called slowly in patients with multiple sclerosis. Axon damage is
evolving lesions), but whether and how these changes are already prominent at the earliest lesion stages, whereas
related to chronic inflammation is uncertain.47 neuronal loss can start early but becomes more obvious
Another important site of chronic inflammation is the in tissue samples from patients with progressive disease
leptomeninges (figure 1), in which innate and adaptive (figure 1).56,57 As a consequence primarily of axon damage,
immune cells can aggregate and occasionally organise into neurofilament light chain is released into the interstitial
80 www.thelancet.com/neurology Vol 22 January 2023
Personal View
Clinical outcome Stage of use* Source
Inflamation
White matter inflammation
MRI for lesion volume and count (T2-FLAIR, Gd+) Relapse (count, time to, Clinical practice Filippi et al (2019)22
and annualised rate)
MRI for central vein sign (T2*) Relapse Clinical practice Al-Louzi et al (2022)23
MRI for paramagnetic (iron) rim lesions (T2* phase, QSM) Disability progression Clinical practice Filippi et al (2019)22
Grey matter inflammation
MRI for lesion count and volume (T2*, STIR, PSIR, PD, MPRAGE) Relapse, disability progression Clinical practice Moccia et al (2017)24
Spinal cord inflammation
MRI for lesion count and volume (T2*, STIR, PSIR, PD, MPRAGE) Relapse, disability progression Clinical practice Moccia et al (2017)24
Optic nerve inflammation
MRI for lesion count and volume (STIR) Optic neuritis, changes in Clinical practice Kolappan et al (2009)25
visual acuity
Optical coherence tomography (pRNFL) Changes in visual acuity Clinical practice Sotirchos et al (2020)26
Leptomeningeal inflammation
MRI (post-gadolinium 3D T2-FLAIR) Disability progression Clinical trials Choi et al (2012)27
Microglia and astrocytes
PET (TSPO, acetate) Disability progression Clinical research Moccia et al (2017)28
Neurodegeneration
Neuro-axonal damage
Blood or CSF (neurofilament light chain concentrations) Relapse, disability progression Clinical trials Khalil et al (2018)29
MRI (AD and FA DTI, ODI/NDI) Disability progression Clinical trials Bagnato et al (2020)30
Magnetic resonance spectroscopy (GABA, choline) Unknown Clinical research Moccia et al (2017)28
PET (GABA, choline) Unknown Clinical research Moccia et al (2017)28
Neuro-axonal loss
MRI for intralesional axonal loss (T1 black holes) Disability progression Clinical practice Filippi et al (2019)22
MRI for global and regional brain atrophy (3DT1) Disability progression Clinical trials Eshaghi et al (2021)16
MRI for spinal cord atrophy (3DT1) Disability progression Clinical trials Moccia et al (2019)31
Optical coherence tomography for optic nerve atrophy (GCL, pRNFL) Low contrast visual acuity Clinical trials Sotirchos et al (2020)26
PET for synapse loss Unknown Clinical research Moccia et al (2017)28
Molecular mechanisms of injury: oxidative stress and mitochondrial dysfunction
Energy failure
Magnetic resonance spectroscopy (NAA, creatine, phosphocreatine) Disability progression Clinical research Moccia M et al (2017)28
Metabolic imbalance
Sodium imaging Disability progression Clinical research Eisele et al (2021)32
Magnetic resonance spectroscopy (glutamate, glutamine, glutathione) Disability progression Clinical research Choi et al (2018)33
Blood or CSF (oxidation products) Disability progression Clinical research Pegoretti et al (2020)34
Failure of compensatory mechanisms
Demyelination and remyelination
Visual evoked potentials Changes in visual acuity Clinical practice Green et al (2017)35
MRI (MT, MWF, RD DTI, MP2RAGE) Disability progression Clinical trials Bagnato et al (2020)30
PET (amyloid) Disability progression Clinical research Moccia et al (2017)28
Neuroplasticity
Functional MRI (BOLD) Disability progression Clinical trials Loitfelder et al (2014)36
7T=7 tesla. AD=axial diffusivity. BOLD=blood oxygen level dependent. DIR=double inversion recovery. DTI=diffusion tensor imaging. FA=fractional anisotropy.
fMRI=functional MRI. GABA=gamma-aminobutyric acid. GCL= ganglion cell layer. Gd+=gadolinium enhancing. MP(2)RAGE=magnetisation prepared (2) rapid
acquisition(s) of gradient echo. MRI=magnetic resonance imaging. MRS=magnetic resonance spectroscopy. MT=magnetisation transfer. MWF=myelin water fraction.
NAA=N-acetylaspartate. OCT=optical coherence tomography. ODI/NDI=orientation dispersion index/neurite density index. PD=proton density weighted imaging.
PET=positron emission tomography. pRNFL=peripapillary retinal nerve fibre layer. PSIR=phase-sensitive inversion recovery. QSM=quantitative susceptibility mapping.
RD=radial diffusivity. STIR=short tau inversion recovery. T2-FLAIR=T2 fluid-attenuated inversion recovery. TSPO=translocator protein 18kDa. VEP=visual evoked
potentials. *Stage of use is defined as clinical research if measurement is limited to non-interventional studies (eg, observational, proof-of-concept, retrospective) in
specialised centres; clinical trials if measurement is applied also to interventional studies (eg, treatment response) in multiple centres with central processing and clinical
practice if measurement is currently part of standard care.
Table: Pathological mechanisms of multiple sclerosis progression and approaches to measure them
www.thelancet.com/neurology Vol 22 January 2023 81
Personal View
space and subsequently enters the CSF and peripheral oxidised DNA—can induce injury of axons, neurons,
blood (table).29 Neurofilament light chain concentration dendrites, and oligodendroglia in multiple sclerosis
has been directly associated with relapses and clinical lesions.68–70 Excessive iron deposition in CNS parenchyma
progression, is now routinely included in clinical trials as has been hypothesised to be a source of oxidative stress in
an outcome measure, and is moving closer to use in multiple sclerosis, and iron has been noted to accumulate
clinical practice. Neurofilament light chain will likely be in deep grey matter nuclei by susceptibility-based MRI and
important as a prognostic biomarker to monitor patients in macrophages and microglia in the rim of mixed active
with multiple sclerosis for progression, disease activity, and inactive lesions.22 The pro-oxidative environment is
and treatment efficacy.58 At the molecular level, demye aggravated by relative deficiency of protective brain
lination leads to dysfunction and anomalous distribution glutathione in progressive multiple sclerosis, as might be
of ion channels along the axons. One consequence of detected in vivo by glutathione spectroscopy.33
aberrant function of ion channels is accumulation of Mitochondria are also perturbed in multiple sclerosis.
intra-axonal calcium, which can stimulate catabolism Following demyelination, mitochondria move from the
and trigger intra-axonal proteolytic degradation.59–61 cell soma to the demyelinated axon; however, the peak of
Altered ion channel distribution is difficult to detect in this potentially beneficial mitochondrial response is
clinical practice, but a few MRI studies in patients with reached only after axonal degeneration has begun.71
multiple sclerosis have shown that the tissue sodium Chronic demyelination, iron accumulation, and oxidative
concentration is elevated in acute and chronic lesions injury can further produce dysfunctional mitochondria,
compared with areas of extralesional white matter, which accumulate over time.72 Dys functional kinesins
suggesting widespread or focal ion imbalance.32,62 (motor proteins responsible for axonal transport of
At the metabolic level, myelin contributes to axon and mitochondria) also impair export of mitochondria from
neuron survival.63 Astrocytes transfer metabolites to the soma into the axon, further contributing to axonal
oligodendrocytes, which in turn support neuroaxonal energy failure and injury. In post-mortem tissue from
metabolism.64 These metabolic changes can in principle patients with progressive multiple sclerosis, the density
be studied using magnetic resonance spectroscopy and of neurons deficient in respiratory complex IV is elevated
PET, although use of these methods is limited to small throughout the grey matter, and there are multiple
numbers of patients in proof-of-concept studies; broader deletions of mitochondrial DNA in individual neurons
use would require standardisation of image acquisition resembling those seen with ageing. Dysfunctional
and processing, and substantial improvements in signal- mitochondria might not complete oxidative phosphory
to-noise ratio.65 lation, leading to energy failure, a state of virtual hypoxia,
Although cellular, molecular, and metabolic mech and amplification of oxidative injury through electron
anisms of neuroaxonal damage are still difficult to leakage in axons and neurons, which could contribute to
measure, the resulting global and regional brain neuronal network failure and disease progression.73
atrophy—detectable from early in the disease course— Energy failure can in practice be assayed in vivo using
has been associated with a heightened risk of progressive magnetic resonance spectroscopy, but a com bination
disability accumulation. Accelerated brain atrophy has of laboratory and imaging techniques that can
been associated with long-term disability progression reliably assess ongoing oxidative injury and mito
independent of relapse activity (so-called silent chondrial dysfunction in lesions is needed (table).
progression).66 Atrophy indices have been utilised as As such, evidence of associations between molecular
primary outcome measures in phase 2 clinical trials in mechanisms of injury and multiple sclerosis progression
patients with progressive multiple sclerosis. Brain and mostly comes from small proof-of-concept studies, and
spinal cord volume measurements are beginning to be standardisation of methods will be necessary for imple
available for clinical practice and will benefit from mentation in clinical trials and practice.
standardised acquisition protocols and analysis methods
(table).67 Axon loss, mostly from inflammatory demyeli Failure of compensatory mechanisms
nation in the optic nerve, is reflected in thinning of the Remyelination
retinal nerve fibre and ganglion cell layers on optical Myelin is required for saltatory conduction of action
coherence tomography, which is in turn correlated with potentials, to supply trophic factors for axons, and to
brain atrophy and disability accumulation (figure 1).26 protect axons against the inflammatory milieu. Remyeli
nation is a spontaneous repair process in which new
Oxidative stress and mitochondrial dysfunction myelin sheaths are formed after a demyelinating event
Oxidative stress and mitochondrial dysfunction, which (figure 1).21,74 Compared with native myelin, repaired
contribute to glial and neuronal injury, axonal energy myelin is characterised by shorter and thinner myelin
failure, and loss of neuronal network function, could be sheaths, resulting in slower action potential conduction.75,76
key molecular mechanisms driving disease progression. The extent of remyelination varies across and within
High levels of oxidative stress in the CNS—as determined individuals and might be influenced by lesion location,
by lipid peroxides, their breakdown aldehydes, and extent and composition of inflammation, age, genetic
82 www.thelancet.com/neurology Vol 22 January 2023
Personal View
factors, disease duration, and potentially other factors yet and more severe disability, compared with healthy
to be identified.77,78 A higher proportion of remyelinated controls.89 Acute and chronic inflammation not only
lesions is associated with slower disease progression.51,79 cause CNS damage, which stimulates reorganisation, but
MRI studies suggest that remyelination starts quickly also probably interfere with the processes required for
after the onset of demyelination and continues over functional reorganisation.56 Preservation of functional
approximately 6 months.80 Whether remyelination can connectivity also depends on cognitive reserve, despite
continue beyond 6 months is uncertain but of tremendous accumulation of structural damage, suggesting that such
importance. reserve can directly affect neuroplasticity potential.90 The
In animal models of demyelination, proliferation and magnitude of functional reorganisation correlates with
migration of oligodendrocyte progenitor cells and their the extent of lesional and extralesional damage. In
differentiation into mature myelinating oligodendrocytes patients with preserved motor function, greater lesion
are required for successful remyelination. In inactive volume and microstructural damage are associated with
and mixed active and inactive lesions, oligodendrocyte widespread activation of brain areas, suggesting that
progenitor cells are present, albeit in reduced numbers reorganisation is compensatory. However, the degree of
and uneven distribution, whereas mature oligo recovery relates to the specific pattern of functional
dendrocytes are almost completely lost.81,82 These findings changes, rather than to their extent, indicating that
suggest that impaired oligodendrocyte differentiation compensation might in some instances be maladaptive.56
contributes to remyelination failure in progressive The severity of multiple sclerosis-related CNS damage
multiple sclerosis.76,77 Studies suggest that not only as assessed clinically and by MRI is an important factor
oligodendrocyte progenitor cells but also mature affecting quantitative and qualitative aspects of functional
oligodendrocytes might contribute to successful lesion reorganisation, interacting with age at disease onset,
remyelination and that the reasons for remyelination disease duration, and disease-modifying therapy.91 Other
failure in multiple sclerosis could be diverse and depend important factors, such as age, sex, comorbidities, and
on disease duration, lesion stage, and lesion location.45,74,83,84 health behaviours (eg, smoking and exercise) influence
Several methods can assess remyelination clinically the capacity for compensatory reorganisation.92–94
even though they are not routinely used in clinical practice One explanation for the emergence of progressive
(table). Longitudinal voxel-based magnetisation transfer disability worsening in multiple sclerosis is the accu
MRI has been used to quantify remyelination in several mulation of irreversible damage exceeding the capacity
clinical trials; however, inflammation, oedema, and axon of the CNS to compensate. Future longitudinal studies
loss can also influence the measurement.85 T1 mapping at should integrate functional MRI findings with clinical
7-tesla MRI allows partial differentiation of demyelinated and neuropsychological measures and other methods
and remyelinated white matter lesions (figure 1).86 Myelin that assess neural networks structurally (eg, diffusion
water fraction imaging is another technique currently tensor imaging and ultra-high-field anatomical imaging)
used to identify myelin changes in the human brain.87 and functionally (eg, magnetoencephalography). Aspects
Radiotracers that also label amyloid (eg, [11C]PIB) are of functional MRI acquisition parameters and analysis
sensitive to myelin, and longitudinal data raise the need to be refined and standardised. Additionally,
possibility that this method allows detection of both a better understanding of the network characteristics
demyelination and remyelination in patients with multiple that are most clinically relevant is required.56 Most
sclerosis.79,88 Visual evoked potentials have been extensively importantly, among the changes associated with motor
used to assess demyelination and remyelination, both and cognitive disability worsening, it is essential to
in clinical practice and as a primary outcome in proof- distinguish the changes that are clinically irrelevant,
of-concept clinical trials evaluating the potential of
those that are appropriate but inadequate to compensate
remyelination-promoting compounds.35 for accu mulating CNS damage, and those that are
maladaptive.
Neuroplasticity
Neuroplasticity and functional reorganisation in response The role of ageing in multiple sclerosis
to damage are intrinsic properties of the CNS. Mech Older chronological age is robustly associated with non-
anisms include molecular changes, synaptogenesis, relapse-related progression. Progressive multiple sclerosis
alteration of synaptic function, and dendrite and axon is very rare in children, and progression from onset occurs
sprouting. Reorganisation of neural networks can be seen in less than 1% of children versus around 10% of adults
in people with multiple sclerosis by task-oriented and diagnosed with multiple sclerosis.95 In adults, older age at
resting state functional MRI (figure 1, table). Motor, diagnosis is associated with faster accumulation of
sensory, visual, and particularly cognitive functions ambulatory disability, which is currently a defining feature
(processing speed and efficiency, attention, memory, and of progressive multiple sclerosis, and greater cognitive
executive function) are associated with widespread and impairment.96,97
bilateral brain activation in patients with multiple The prototypical biological marker of ageing is telomere
sclerosis, especially those with longer disease duration attrition, and leukocyte telomere length is a reliable marker
www.thelancet.com/neurology Vol 22 January 2023 83
Personal View
of telomere length from different cell types throughout the capacity for functional recovery from inflam matory
body.98 In a cohort of over 500 people with multiple injury. By contrast, better physical outcome from multiple
sclerosis, attrition of leukocyte telomere length was sclerosis attacks in children compared with adults has
associated with greater disability in both cross-sectional been attributed to high functional reserve and capacity for
and longitudinal analyses independent of disease duration plasticity.105
and chronological age.99 Although the association of Systemic ageing leads to increased burden of comorbid
telomere length with multiple sclerosis subtype has not illnesses, including vascular disease, which could
been shown to be causal, there is strong biological further hasten development of multiple sclerosis
plausibility that processes downstream of telomere ambulatory disability.106 Although the mechanisms by
attrition, including the DNA damage response and cellular which vascular disease worsens progression are not fully
senescence, contribute to disability progression. Intrigu elucidated, injury to brain white matter is a likely
ingly, senescence of lymphocyte subsets has been linked to contributor.107
multiple sclerosis pathology.100–102 Reproductive ageing can also affect multiple sclerosis
Senescence of different CNS cell subtypes, which might progression. Whereas women are at increased risk for
be accelerated due to the disease itself, might also affect developing multiple sclerosis, men with multiple sclerosis
progression. Senescent microglia can both promote can have earlier and faster disability development.96,97
chronic secretion of inflammatory cytokines and Several studies suggest that progressive multiple sclerosis
contribute to an inhibitory environment for remyelination, pathology and disability accelerate in the perimenopausal
due to their decreased phagocytic activity. Senescent period.108 Potential mechanisms for an association of
astrocytes are detrimental to synaptic plasticity, blood– ovarian functional decline with progressive multiple
brain barrier function, and the metabolic balance of sclerosis pathology include the loss of neuroprotective
neighbouring neurons.103,104 Overall, ageing has been effects of oestrogens and immune changes in the
associated with declining neural plasticity and less perimenopausal period. Loss of sex-specific steroid
Biological measures
Pathological Blood MRI Functional Magnetic PET Optical Visual
speciments and CSF MRI resonance coherence evoked
biomarkers spectroscopy tomography potentials
To measure
• Biological sex
• Infections Injury and compensatory mechanisms
• Genetics Mediate Inflammation Demyelination Axonal Mitochondrial Oxidative Ca2+ and Remyelination Neuroplasticity
• Race degeneration injury stress glutamate
• Ethnicity excitotoxicity
• Microbiome
• Comorbidities and
medications Contribute to
• Disease modifying
therapies
Mediate
• Health behaviours Clinical expression
(eg, diet and exercise)
• Social determinants
of health To measure
Clinical measures
Disability scales Patient reported outcomes
Exposure to Biological Prodromal Clinical presentation Clinical course and evolution
risk factors onset of period
disease
Reserve and repair Biological ageing
Figure 2: Assessments relevant to a mechanism-driven framework for multiple sclerosis progression
Multiple sclerosis progression reflects a combination of mechanisms of injury and compensation (red box) that exist contemporaneously and contribute to clinical expression. The activation of
mechanisms of injury marks the biological onset of the disease and initiates the prodromal period (the period between the start of disease mechanisms and the start of detectable signs or symptoms).
The balance of the mechanisms of injury together with those of repair jointly determines clinical expression throughout the disease course. The age-associated decrease in reserve and repair capacity
also influences clinical progression. Development of clinical and biological measures with high sensitivity and specificity is required to continuously monitor the clinical presentation of the disease and
identify relevant injury and compensatory mechanisms in individuals. Potential mediators (light blue box on the left) exert positive and negative influences on injury and compensatory mechanisms
and thus affect clinical expression throughout the disease course. The list of mediators is illustrative rather than comprehensive.
84 www.thelancet.com/neurology Vol 22 January 2023
Personal View
production might explain the phenomenon of women
with multiple sclerosis appearing to catch up with men in Search strategy and selection criteria
terms of disability in later decades of life. References for this Personal View were identified by searches
of articles published in English in PubMed between
Conclusions and future directions Jan 1, 2012, and April 1, 2022, and references from relevant
Despite substantial gains in knowledge of multiple articles. The search terms “multiple sclerosis”, “inflammation”,
sclerosis pathophysiology and the proliferation of treat “neurodegeneration”, “mitochondrial dysfunction”,
ments to forestall multiple sclerosis relapses, halting and “oxidative stress”, and “remyelination”, “neuronal networks”,
reversing disease progression are unmet needs. To address “neural plasticity”, “aging”, “imaging”, and “OCT” were used.
these needs, it is essential to move from clinically based to The final reference list was generated based on relevance to
biologically based definitions of multiple sclerosis the topics covered in this Personal View.
progression, and to develop and validate tools that can
reliably assess and track relevant disease biology in clinical
settings. Data suggest that disability progression is not ensuring a smooth transition from the current state to a
caused by one uniform disease mechanism but instead future framework is non-trivial but crucial given its
results from a combination of several mechanisms, which importance for patients.
play out variably across patients and within individual We are cognisant that a new framework, albeit necessary
patients over time (figure 2). Indeed, over time, for developing biologically-based treatment approaches
mechanisms of injury such as those discussed in this and algorithms, would require validation in clinical and
Personal View (non-resolving inflammation, neurode research settings. Coordinated efforts of stakeholders
generation, oxidative stress, and mitochondrial dysfunc (eg, researchers, funders, health authorities, and patient
tion) can occur separately or in various combinations in organisations) will be key. Focused efforts will then be
the same individual, and together with failure of com needed to integrate the new framework into clinical trials
pensatory mechanisms (eg, remyelination and neuro and practice, and to transition away from the legacy
plasticity), all interacting with ageing, to define the clinical framework used by regulatory agencies and health
picture across the disease course. Multiple sclerosis authorities for drug approvals. Comprehensive patient
researchers must develop methods to identify and education efforts will also be required. As such,
quantify these mechanisms on the patient level, and development of a roadmap for implementation of any
incorporate the relevant measures into both clinical trials new framework will be a key future focus of the
and clinical practice. Achieving this goal will require International Advisory Committee on Clinical Trials in
correlative clinical–radiological–pathological studies of Multiple Sclerosis.
people with fast versus slow disease progression, Contributors
independent of relapses and active lesions on MRI, and All authors contributed to the conceptualisation, drafting, and review
longitudinal studies correlating imaging and other of the manuscript. TK, MM, TC, and DSR edited and finalised the
manuscript. The members of the International Advisory Committee
paraclinical tools with disease progression as measured on Clinical Trials in Multiple Sclerosis (appendix) reviewed and
using state-of-the-art techniques (eg, clinical, cognitive, endorsed the manuscript.
and digital tools, and blood and CSF biomarkers).109–112 Declaration of interests
In keeping with current trends throughout medicine, we TK received research funding from the German Research Foundation,
envision a future in which clinical benefit accrues directly Interdisciplinary Centre for Clinical Studies (IZKF) Münster, National
from biomarker-based, biologically informed treatment Multiple Sclerosis Society (USA), European Leukodystrophy Association,
Progressive MS Alliance, European Commission (H2020-MSCA-
decisions. The concepts described in this Personal View ITN-2018), and Novartis; and received compensation for serving on a
are a first step towards a new framework that eliminates scientific advisory board (Novartis) and speaker honoraria from Novartis
the current phenomenological classification of patients and Roche. MM has received research grants from MAGNIMS-
using relapsing-remitting, secondary progressive, and ECTRIMS, Multiple Sclerosis Society UK, and Merck; consulting fees
from Ipsen, BMS Celgene, Biogen, Sanofi-Genzyme, Roche, and Merck;
primary progressive descriptors.3 However, until the honoraria for lectures from Merck, Roche, and Sanofi-Genzyme; and
underlying mechanisms and how they interact to drive support for attending meetings from Merck, Biogen, and Sanofi-
progression are better understood, we expect that any new Genzyme. TC is an employee of the National Multiple Sclerosis Society
framework will require additional modification over time. (USA), which is one of the sponsors of the International Advisory
Committee on Clinical Trials in Multiple Sclerosis. JAC has received
Adoption of biologically based definitions of multiple personal compensation for consulting for Biogen, Bristol-Myers Squibb,
sclerosis progression will be operationally challenging, as Convelo, Genentech, Janssen, NervGen, Novartis, and PSI; for speaking
the existing descriptors are deeply embedded in clinical for H3 Communications; and for serving as an editor of the
Multiple Sclerosis Journal. JC has received grants or contracts from
research and health-care systems. Patients rely on the
Biogen, Merck and UC San Francisco; and has received payments or
descriptors to understand their disease journey and honoraria for lectures, speaker bureaus, or presentations from Biogen,
inform health-care decisions. Furthermore, regulatory Merck, Sanofi Genzyme, Novartis, Bristol-Myers, and Roche;
authorities have integrated the descriptors, albeit with participation on Data Safety Monitoring Boards or Advisory Boards from
Novartis, Merck, Sanofi Genzyme, and Biogen. JG has received grant
complicated and differing interpretations, in approval
and contract research support from the National Multiple Sclerosis
documents for multiple sclerosis treatments. As such,
www.thelancet.com/neurology Vol 22 January 2023 85
Personal View
Society (USA), Biogen, and Octave Biosciences; serves on a steering 5 Kappos L, Bar-Or A, Cree BAC, et al. Siponimod versus placebo in
committee for a trial supported by Novartis; has received speaker fees secondary progressive multiple sclerosis (EXPAND): a double-blind,
from Alexion and BMS; and served on an advisory board for Genentech. randomised, phase 3 study. Lancet 2018; 391: 1263–73.
XM received speaking honoraria and travel expenses for participation 6 Fitzgerald KC, Kim K, Smith MD, et al. Early complement genes
in scientific meetings; has been a steering committee member of clinical are associated with visual system degeneration in multiple sclerosis.
trials or participated in advisory boards of clinical trials with Abbvie, Brain 2019; 142: 2722–36.
Actelion, Alexion, Biogen, Bristol-Myers Squibb/Celgene, EMD Serono, 7 Magliozzi R, Howell OW, Nicholas R, et al. Inflammatory
Genzyme, Hoffmann-La Roche, Sandoz, Immunic, Janssen intrathecal profiles and cortical damage in multiple sclerosis.
Pharmaceuticals, Medday, Merck, Mylan, Nervgen, Novartis, Ann Neurol 2018; 83: 739–55.
Sanofi-Genzyme, Teva Pharmaceuticals, TG Therapeutics, Excemed, 8 Moccia M, van de Pavert S, Eshaghi A, et al. Pathologic correlates
Multiple Sclerosis International Federation, and National Multiple of the magnetization transfer ratio in multiple sclerosis. Neurology
2020; 95: e2965–76.
Sclerosis Society (USA). RAM receives research funding from Biogen
Idec and Roche; and is the chair of the Medical Advisory Committee of 9 Absinta M, Maric D, Gharagozloo M, et al. A lymphocyte-microglia-
astrocyte axis in chronic active multiple sclerosis. Nature 2021;
the Multiple Sclerosis Society of Canada. VWY is funded by research
597: 709–14.
grants from the Multiple Sclerosis Society of Canada, the Canadian
10 Yong HYF, Yong VW. Mechanism-based criteria to improve
Institutes of Health Research, Canadian Cancer Society, and Genentech;
therapeutic outcomes in progressive multiple sclerosis.
has received speaker honoraria from Biogen, EMD Serono, Novartis, Nat Rev Neurol 2022; 18: 40–55.
Roche, and Sanofi-Genzyme; and is the recipient of unrestricted
11 Lublin FD, Häring DA, Ganjgahi H, et al. How patients with
educational grants from Biogen, EMD Serono, Novartis, Roche, multiple sclerosis acquire disability. Brain 2022; 145: 3147–3161.
Sanofi-Genzyme, and Teva Canada to support educational activities of
12 Kappos L, Wolinsky JS, Giovannoni G, et al. Contribution of
the Alberta MS Network, which he directs. AJT reports personal fees as relapse-independent progression vs relapse-associated worsening
an editorial board member for The Lancet Neurology receiving a free to overall confirmed disability accumulation in typical relapsing
subscription; is Editor-in-Chief for the Multiple Sclerosis Journal receiving multiple sclerosis in a pooled analysis of 2 randomized clinical
an honorarium from SAGE Publications; receives support from the trials. JAMA Neurol 2020; 77: 1132–40.
UCLH NIHR Biomedical Research Centre; and receives support for 13 Fransen NL, Crusius JBA, Smolders J, et al. Post-mortem multiple
travel as Chair of the Scientific Advisory Committee and International sclerosis lesion pathology is influenced by single nucleotide
Progressive MS Alliance from the National MS Society (USA) as polymorphisms. Brain Pathol 2020; 30: 106–19.
member, National Multiple Sclerosis Society (USA) Research Programs 14 Vandebergh M, Andlauer TFM, Zhou Y, et al. Genetic variation in
Advisory Committee, and as a Board member of the European Charcot WNT9B increases relapse hazard in multiple sclerosis. Ann Neurol
Foundation; has received payment in the past 36 months (paid to the 2021; 89: 884–94.
UCL) from Eisai and from the German Aerospace Centre, Health 15 Lublin FD, Coetzee T, Cohen JA, Marrie RA, Thompson AJ.
Research (ERA-NET NEURON); has received fees or support for travel The 2013 clinical course descriptors for multiple sclerosis:
from Hoffman La Roche, Novartis, and CanProCo SAB; had received a clarification. Neurology 2020; 94: 1088–92.
honoraria or support for travel from EXCEMED and Almirall; has 16 Eshaghi A, Young AL, Wijeratne PA, et al. Identifying multiple
received support for travel to PACTRIMS and has received support for sclerosis subtypes using unsupervised machine learning and MRI
travel to the Multiple Sclerosis Society of Canada; unpaid roles include data. Nat Commun 2021; 12: 2078.
as a Guarantor of BRAIN, Trustee of the National Brain Appeal (National 17 De Meo E, Portaccio E, Giorgio A, et al. Identifying the distinct
Hospital for Neurology and Neurosurgery), and as Chair of the Scientific cognitive phenotypes in multiple sclerosis. JAMA Neurol 2021;
Ambassadors, ‘STOP MS’ Appeal Board (Multiple Sclerosis Society UK). 78: 414–25.
DSR reports personal fees from Bounds Law Group LLC, grants from 18 Tsagkas C, Parmar K, Pezold S, et al. Classification of multiple
sclerosis based on patterns of CNS regional atrophy covariance.
Vertex, grants from Sanofi-Genzyme, grants from Abata Therapeutics,
Hum Brain Mapp 2021; 42: 2399–415.
outside the submitted work; has a patent system and method of
19 Absinta M, Sati P, Reich DS. Advanced MRI and staging of multiple
automatically detecting tissue abnormalities (US Patent 9,607,392)
sclerosis lesions. Nat Rev Neurol 2016; 12: 358–68.
issued, a patent method of analysing multisequence MRI data for
20 Solomon AJ. Progress towards a diagnostic biomarker for MS:
analysing brain abnormalities in a subject (US Patent 9,888,876) issued,
central vein sign. Mult Scler 2020; 26: 394–96.
a patent Automatic identification of subjects at risk of multiple sclerosis
21 Frischer JM, Weigand SD, Guo Y, et al. Clinical and pathological
(US Patent application 16/254,710) issued, and a patent high-resolution
insights into the dynamic nature of the white matter multiple
cerebrospinal fluid-suppressed T2*-weighted magnetic resonance sclerosis plaque. Ann Neurol 2015; 78: 710–21.
imaging of cortical lesions (US Patent application 62/838,578) pending.
22 Filippi M, Brück W, Chard D, et al. Association between
Acknowledgments pathological and MRI findings in multiple sclerosis. Lancet Neurol
The writing of this Personal View was supported by the German 2019; 18: 198–210.
Research Foundation (SFB128 B07, Ku1477/11–1) to TK, and the 23 Al-Louzi O, Letchuman V, Manukyan S, et al. Central vein sign profile
Intramural Research Program of NINDS to DSR. We thank of newly developing lesions in multiple sclerosis: a 3-year longitudinal
Antonio Carotenuto (Federico II University of Naples, Italy) for their study. Neurol Neuroimmunol Neuroinflamm 2022; 9: e1120.
help with the figures. AJT acknowledges support from the UCLH 24 Moccia M, de Stefano N, Barkhof F. Imaging outcome measures
NIHR Biomedical Research Centre. The work of the International for progressive multiple sclerosis trials. Mult Scler 2017;
Advisory Committee on Clinical Trials in Multiple Sclerosis is jointly 23: 1614–26.
sponsored by the European Committee for Treatments and Research in 25 Kolappan M, Henderson AP, Jenkins TM, et al. Assessing structure
Multiple Sclerosis and the National Multiple Sclerosis Society (USA). and function of the afferent visual pathway in multiple sclerosis and
associated optic neuritis. J Neurol 2009; 256: 305–19.
References 26 Sotirchos ES, Gonzalez Caldito N, Filippatou A, et al. Progressive
1 Olsson T, Barcellos LF, Alfredsson L. Interactions between genetic, multiple sclerosis is associated with faster and specific retinal layer
lifestyle and environmental risk factors for multiple sclerosis. atrophy. Ann Neurol 2020; 87: 885–96.
Nat Rev Neurol 2017; 13: 25–36. 27 Choi SR, Howell OW, Carassiti D, et al. Meningeal inflammation
2 Lublin FD, Reingold SC. Defining the clinical course of multiple plays a role in the pathology of primary progressive multiple
sclerosis: results of an international survey. Neurology 1996; sclerosis. Brain 2012; 135: 2935–37.
46: 907–11. 28 Moccia M, Ciccarelli O. Molecular and metabolic imaging in
3 Lublin FD, Reingold SC, Cohen JA, et al. Defining the clinical course multiple sclerosis. Neuroimaging Clin N Am 2017; 27: 343–356.
of multiple sclerosis: the 2013 revisions. Neurology 2014; 83: 278–86. 29 Khalil M, Teunissen CE, Otto M, et al. Neurofilaments as
4 Montalban X, Hauser SL, Kappos L, et al. Ocrelizumab versus biomarkers in neurological disorders. Nat Rev Neurol 2018;
placebo in primary progressive multiple sclerosis. N Engl J Med 14: 577–89.
2017; 376: 209–20.
86 www.thelancet.com/neurology Vol 22 January 2023
Personal View
30 Bagnato F, Gauthier SA, Laule C, et al. Imaging mechanisms of 53 Kaunzner UW, Kang Y, Zhang S, et al. Quantitative susceptibility
disease progression in multiple sclerosis: beyond brain atrophy. mapping identifies inflammation in a subset of chronic multiple
J Neuroimaging 2020; 30: 251–266. sclerosis lesions. Brain 2019; 142: 133–45.
31 Moccia M, Prados F, Filippi M, et al. Longitudinal spinal cord 54 Kaunzner UW, Kang Y, Monohan E, et al. Reduction of PK11195
atrophy in multiple sclerosis using the generalized boundary shift uptake observed in multiple sclerosis lesions after natalizumab
integral. Ann Neurol 2019; 86: 704-13. initiation. Mult Scler Relat Disord 2017; 15: 27–33.
32 Eisele P, Kraemer M, Dabringhaus A, et al. Characterization of 55 Sucksdorff M, Rissanen E, Tuisku J, et al. Evaluation of the effect
chronic active multiple sclerosis lesions with sodium (²³Na) of fingolimod treatment on microglial activation using serial PET
magnetic resonance imaging-preliminary observations. Eur J Neurol imaging in multiple sclerosis. J Nucl Med 2017; 58: 1646–51.
2021; 28: 2392–95. 56 Chard DT, Alahmadi AAS, Audoin B, et al. Mind the gap: from
33 Choi IY, Lee P, Adany P, et al. In vivo evidence of oxidative stress in neurons to networks to outcomes in multiple sclerosis.
brains of patients with progressive multiple sclerosis. Mult Scler Nat Rev Neurol 2021; 17: 173–84.
2018; 24: 1029–38. 57 Zoupi L, Booker SA, Eigel D, et al. Selective vulnerability of inhibitory
34 Pegoretti V, Swanson KA, Bethea JR, Probert L, Eisel ULM, networks in multiple sclerosis. Acta Neuropathol 2021; 141: 415–29.
Fischer R. Inflammation and oxidative stress in multiple sclerosis: 58 Bittner S, Oh J, Havrdová EK, Tintoré M, Zipp F. The potential
consequences for therapy development. Oxid Med Cell Longev 2020; of serum neurofilament as biomarker for multiple sclerosis.
2020: 7191080. Brain 2021; 144: 2954–63.
35 Green AJ, Gelfand JM, Cree BA, et al. Clemastine fumarate as 59 Stys PK. General mechanisms of axonal damage and its prevention.
a remyelinating therapy for multiple sclerosis (ReBUILD): J Neurol Sci 2005; 233: 3–13.
a randomised, controlled, double-blind, crossover trial. Lancet 2017; 60 Witte ME, Schumacher AM, Mahler CF, et al. Calcium influx
390: 2481–89. through plasma-membrane nanoruptures drives axon degeneration
36 Loitfelder M, Fazekas F, Koschutnig K, et al. Brain activity changes in a model of multiple sclerosis. Neuron 2019; 101: 615–624.e5.
in cognitive networks in relapsing-remitting multiple 61 Estacion M, Vohra BP, Liu S, et al. Ca2+ toxicity due to reverse
sclerosis - insights from a longitudinal FMRI study. PLoS One Na+/Ca2+ exchange contributes to degeneration of neurites of
2014; 9: e93715. DRG neurons induced by a neuropathy-associated Nav1.7 mutation.
37 Bodini B, Chard D, Altmann DR, et al. White and gray matter J Neurophysiol 2015; 114: 1554–64.
damage in primary progressive MS: the chicken or the egg? 62 Inglese M, Madelin G, Oesingmann N, et al. Brain tissue sodium
Neurology 2016; 86: 170–76. concentration in multiple sclerosis: a sodium imaging study at
38 Lublin F, Miller DH, Freedman MS, et al. Oral fingolimod in primary 3 tesla. Brain 2010; 133: 847–57.
progressive multiple sclerosis (INFORMS): a phase 3, randomised, 63 Fünfschilling U, Supplie LM, Mahad D, et al. Glycolytic
double-blind, placebo-controlled trial. Lancet 2016; 387: 1075–84. oligodendrocytes maintain myelin and long-term axonal integrity.
39 Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple Nature 2012; 485: 517–21.
sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 64 Brown AM, Baltan Tekkök S, Ransom BR. Energy transfer from
2018; 17: 162–73. astrocytes to axons: the role of CNS glycogen. Neurochem Int 2004;
40 Fransen NL, Hsiao CC, van der Poel M, et al. Tissue-resident 45: 529–36.
memory T cells invade the brain parenchyma in multiple sclerosis 65 Moccia M, Ciccarelli O. Molecular and metabolic imaging in
white matter lesions. Brain 2020; 143: 1714–30. multiple sclerosis. Neuroimaging Clin N Am 2017; 27: 343–56.
41 Schirmer L, Velmeshev D, Holmqvist S, et al. Neuronal 66 Cree BAC, Hollenbach JA, Bove R, et al. Silent progression in
vulnerability and multilineage diversity in multiple sclerosis. disease activity-free relapsing multiple sclerosis. Ann Neurol 2019;
Nature 2019; 573: 75–82. 85: 653–66.
42 Wheeler MA, Clark IC, Tjon EC, et al. MAFG-driven astrocytes 67 Wattjes MP, Ciccarelli O, Reich DS, et al. 2021 MAGNIMS-CMSC-
promote CNS inflammation. Nature 2020; 578: 593–99. NAIMS consensus recommendations on the use of MRI in patients
43 Dal-Bianco A, Grabner G, Kronnerwetter C, et al. Slow expansion with multiple sclerosis. Lancet Neurol 2021; 20: 653–70.
of multiple sclerosis iron rim lesions: pathology and 7 T magnetic 68 Lassmann H, van Horssen J. Oxidative stress and its impact on
resonance imaging. Acta Neuropathol 2017; 133: 25–42. neurons and glia in multiple sclerosis lesions. Biochim Biophys Acta
44 Absinta M, Sati P, Masuzzo F, et al. Association of chronic active 2016; 1862: 506–10.
multiple sclerosis lesions with disability in vivo. JAMA Neurol 2019; 69 Haider L, Zrzavy T, Hametner S, et al. The topograpy of
76: 1474–83. demyelination and neurodegeneration in the multiple sclerosis
45 Dal-Bianco A, Grabner G, Kronnerwetter C, et al. Long-term brain. Brain 2016; 139: 807–15.
evolution of multiple sclerosis iron rim lesions in 7 T MRI. 70 Haider L, Simeonidou C, Steinberger G, et al. Multiple sclerosis
Brain 2021; 144: 833–47. deep grey matter: the relation between demyelination,
46 Zinger N, Ponath G, Sweeney E, et al. Dimethyl fumarate reduces neurodegeneration, inflammation and iron.
inflammation in chronic active multiple sclerosis lesions. J Neurol Neurosurg Psychiatry 2014; 85: 1386–95.
Neurol Neuroimmunol Neuroinflamm 2022; 9: e1138. 71 Licht-Mayer S, Campbell GR, Canizares M, et al. Enhanced axonal
47 Elliott C, Wolinsky JS, Hauser SL, et al. Slowly expanding/ response of mitochondria to demyelination offers neuroprotection:
evolving lesions as a magnetic resonance imaging marker of implications for multiple sclerosis. Acta Neuropathol 2020;
chronic active multiple sclerosis lesions. Mult Scler 2019; 140: 143–67.
25: 1915–25. 72 Campbell G, Mahad DJ. Mitochondrial dysfunction and axon
48 Lassmann H. Multiple sclerosis pathology. degeneration in progressive multiple sclerosis. FEBS Lett 2018;
Cold Spring Harb Perspect Med 2018; 8: a028936. 592: 1113–21.
49 Howell OW, Reeves CA, Nicholas R, et al. Meningeal inflammation 73 Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in
is widespread and linked to cortical pathology in multiple sclerosis. progressive multiple sclerosis. Lancet Neurol 2015; 14: 183–93.
Brain 2011; 134: 2755–71. 74 Heß K, Starost L, Kieran NW, et al. Lesion stage-dependent causes for
50 Kutzelnigg A, Lucchinetti CF, Stadelmann C, et al. Cortical impaired remyelination in MS. Acta Neuropathol 2020; 140: 359–75.
demyelination and diffuse white matter injury in multiple sclerosis. 75 Stangel M, Kuhlmann T, Matthews PM, Kilpatrick TJ. Achievements
Brain 2005; 128: 2705–12. and obstacles of remyelinating therapies in multiple sclerosis.
51 Luchetti S, Fransen NL, van Eden CG, Ramaglia V, Mason M, Nat Rev Neurol 2017; 13: 742–54.
Huitinga I. Progressive multiple sclerosis patients show substantial 76 Franklin RJM, Ffrench-Constant C. Regenerating CNS myelin—from
lesion activity that correlates with clinical disease severity and sex: mechanisms to experimental medicines. Nat Rev Neurosci 2017;
a retrospective autopsy cohort analysis. Acta Neuropathol 2018; 18: 753–69.
135: 511–28.
77 Goldschmidt T, Antel J, König FB, Brück W, Kuhlmann T.
52 Högel H, Rissanen E, Vuorimaa A, Airas L. Positron emission Remyelination capacity of the MS brain decreases with disease
tomography imaging in evaluation of MS pathology in vivo. chronicity. Neurology 2009; 72: 1914–21.
Mult Scler 2018; 24: 1399–412.
www.thelancet.com/neurology Vol 22 January 2023 87
Personal View
78 Chang A, Staugaitis SM, Dutta R, et al. Cortical remyelination: a new 95 Harding KE, Liang K, Cossburn MD, et al. Long-term outcome
target for repair therapies in multiple sclerosis. Ann Neurol 2012; of paediatric-onset multiple sclerosis: a population-based study.
72: 918–26. J Neurol Neurosurg Psychiatry 2013; 84: 141–47.
79 Bodini B, Veronese M, García-Lorenzo D, et al. Dynamic imaging 96 Kalincik T, Vivek V, Jokubaitis V, et al. Sex as a determinant of
of individual remyelination profiles in multiple sclerosis. Ann Neurol relapse incidence and progressive course of multiple sclerosis.
2016; 79: 726–38. Brain 2013; 136: 3609–17.
80 Chen JT, Collins DL, Atkins HL, Freedman MS, Arnold DL. 97 Confavreux C, Vukusic S. Age at disability milestones in multiple
Magnetization transfer ratio evolution with demyelination and sclerosis. Brain 2006; 129: 595–605.
remyelination in multiple sclerosis lesions. Ann Neurol 2008; 98 Demanelis K, Jasmine F, Chen LS, et al. Determinants of telomere
63: 254–62. length across human tissues. Science 2020; 369: eaaz6876.
81 Chang A, Tourtellotte WW, Rudick R, Trapp BD. Premyelinating 99 Krysko KM, Henry RG, Cree BAC, et al. Telomere length is
oligodendrocytes in chronic lesions of multiple sclerosis. associated with disability progression in multiple sclerosis.
N Engl J Med 2002; 346: 165–73. Ann Neurol 2019; 86: 671–82.
82 Kuhlmann T, Miron V, Cui Q, Wegner C, Antel J, Brück W. 100 Claes N, Fraussen J, Vanheusden M, et al. Age-associated B cells
Differentiation block of oligodendroglial progenitor cells as a cause with proinflammatory characteristics are expanded in a proportion
for remyelination failure in chronic multiple sclerosis. Brain 2008; of multiple sclerosis patients. J Immunol 2016; 197: 4576–83.
131: 1749–58. 101 Thewissen M, Linsen L, Somers V, Geusens P, Raus J, Stinissen P.
83 Yeung MSY, Djelloul M, Steiner E, et al. Dynamics of oligodendrocyte Premature immunosenescence in rheumatoid arthritis and
generation in multiple sclerosis. Nature 2019; 566: 538–42. multiple sclerosis patients. Ann N Y Acad Sci 2005; 1051: 255–62.
84 Jäkel S, Agirre E, Mendanha Falcão A, et al. Altered human 102 Thewissen M, Somers V, Venken K, et al. Analyses of
oligodendrocyte heterogeneity in multiple sclerosis. Nature 2019; immunosenescent markers in patients with autoimmune disease.
566: 543–47. Clin Immunol 2007; 123: 209–18.
85 Cadavid D, Mellion M, Hupperts R, et al. Safety and efficacy of 103 Correale J, Farez MF. The role of astrocytes in multiple sclerosis
opicinumab in patients with relapsing multiple sclerosis progression. Front Neurol 2015; 6: 180.
(SYNERGY): a randomised, placebo-controlled, phase 2 trial. 104 Oost W, Talma N, Meilof JF, Laman JD. Targeting senescence to
Lancet Neurol 2019; 18: 845–56. delay progression of multiple sclerosis. J Mol Med 2018; 96: 1153–66.
86 Kolb H, Absinta M, Beck ES, et al. 7T MRI differentiates 105 Rocca MA, Absinta M, Ghezzi A, Moiola L, Comi G, Filippi M.
remyelinated from demyelinated multiple sclerosis lesions. Is a preserved functional reserve a mechanism limiting clinical
Ann Neurol 2021; 90: 612–26. impairment in pediatric MS patients? Hum Brain Mapp 2009;
87 Elkady AM, Wu Z, Leppert IR, Arnold DL, Narayanan S, Rudko DA. 30: 2844–51.
Assessing the differential sensitivities of wave-CAIPI ViSTa myelin 106 Marrie RA, Rudick R, Horwitz R, et al. Vascular comorbidity is
water fraction and magnetization transfer saturation for efficiently associated with more rapid disability progression in multiple
quantifying tissue damage in MS. Mult Scler Relat Disord 2021; sclerosis. Neurology 2010; 74: 1041–47.
56: 103309.
107 Geraldes R, Esiri MM, DeLuca GC, Palace J. Age-related small
88 Auvity S, Tonietto M, Caillé F, et al. Repurposing radiotracers for vessel disease: a potential contributor to neurodegeneration in
myelin imaging: a study comparing 18F-florbetaben, 18F-florbetapir, multiple sclerosis. Brain Pathol 2017; 27: 707–22.
18F-flutemetamol,11C-MeDAS, and 11C-PiB.
108 Graves JS, Henry RG, Cree BAC, et al. Ovarian aging is associated
Eur J Nucl Med Mol Imaging 2020; 47: 490–501.
with gray matter volume and disability in women with MS.
89 Rimkus CM, Schoonheim MM, Steenwijk MD, et al. Gray matter Neurology 2018; 90: e254–60.
networks and cognitive impairment in multiple sclerosis. Mult Scler
109 McKay KA, Bedri SK, Manouchehrinia A, et al. Reduction in
2019; 25: 382–91.
cognitive processing speed surrounding multiple sclerosis relapse.
90 Fuchs TA, Benedict RHB, Bartnik A, et al. Preserved network Ann Neurol 2022; 91: 417–23.
functional connectivity underlies cognitive reserve in multiple
110 Moccia M, Lanzillo R, Palladino R, et al. Cognitive impairment at
sclerosis. Hum Brain Mapp 2019; 40: 5231–41.
diagnosis predicts 10-year multiple sclerosis progression. Mult Scler
91 Rocca MA, Colombo B, Falini A, et al. Cortical adaptation in patients 2016; 22: 659–67.
with MS: a cross-sectional functional MRI study of disease
111 Dillenseger A, Weidemann ML, Trentzsch K, et al. Digital
phenotypes. Lancet Neurol 2005; 4: 618–26.
biomarkers in multiple sclerosis. Brain Sci 2021; 11: 1519.
92 Schoonheim MM, Hulst HE, Landi D, et al. Gender-related
112 De Angelis M, Lavorgna L, Carotenuto A, et al. Digital technology
differences in functional connectivity in multiple sclerosis. Mult Scler
in clinical trials for multiple sclerosis: systematic review. J Clin Med
2012; 18: 164–73.
2021; 10: 2328.
93 Sumowski JF, Wylie GR, Deluca J, Chiaravalloti N. Intellectual
enrichment is linked to cerebral efficiency in multiple sclerosis: Copyright © 2022 Elsevier Ltd. All rights reserved.
functional magnetic resonance imaging evidence for cognitive
reserve. Brain 2010; 133: 362–74.
94 Sandroff BM, Jones CD, Baird JF, Motl RW. Systematic review on
exercise training as a neuroplasticity-inducing behavior in multiple
sclerosis. Neurorehabil Neural Repair 2020; 34: 575–88.
88 www.thelancet.com/neurology Vol 22 January 2023
You might also like
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Lancet Sclerosi MultiplaDocument15 pagesLancet Sclerosi MultiplaMr. LNo ratings yet
- Effect of Photobiomodulation in MultiplesclerosisDocument4 pagesEffect of Photobiomodulation in MultiplesclerosisMuhammad Imam NoorNo ratings yet
- Multiple Sclerosis Lancet 2018Document15 pagesMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoNo ratings yet
- Personal View: Graham Teasdale, Andrew Maas, Fiona Lecky, Geoff Rey Manley, Nino Stocchetti, Gordon MurrayDocument11 pagesPersonal View: Graham Teasdale, Andrew Maas, Fiona Lecky, Geoff Rey Manley, Nino Stocchetti, Gordon MurrayMariana PeredaNo ratings yet
- Tratamiento de La Neurocisticercosis Revision CritDocument9 pagesTratamiento de La Neurocisticercosis Revision CritKarem Santos HinostrozaNo ratings yet
- Differential Diagnosis of Suspected Multiple Sclerosis - An Updated Consensus ApproachDocument15 pagesDifferential Diagnosis of Suspected Multiple Sclerosis - An Updated Consensus ApproachInthe MOON youNo ratings yet
- Diagnosis of Multiple Sclerosis Progress and ChallengesDocument11 pagesDiagnosis of Multiple Sclerosis Progress and Challengessarawu9911No ratings yet
- Glasgow Come ScaleDocument11 pagesGlasgow Come ScaleMaria Jose Gonzalez SarangoNo ratings yet
- Develop Med Child Neuro - 2019 - Duignan - Paediatric Multiple Sclerosis A New Era in Diagnosis and TreatmentDocument12 pagesDevelop Med Child Neuro - 2019 - Duignan - Paediatric Multiple Sclerosis A New Era in Diagnosis and TreatmentFelipe Beltrán TorresNo ratings yet
- Journal Reading - Progressive Multiple SclerosisDocument20 pagesJournal Reading - Progressive Multiple SclerosisMuhammad Imam NoorNo ratings yet
- Frohman 2006Document11 pagesFrohman 2006Alfredo Enrique Marin AliagaNo ratings yet
- Esclerosis Tuberosa 6Document18 pagesEsclerosis Tuberosa 6Santiago CeliNo ratings yet
- SeminarDocument20 pagesSeminarricardojosesotofontalvoNo ratings yet
- Tani 2014Document4 pagesTani 2014Besiel Buendia J.No ratings yet
- Multiple Sclerosis and Exercice A Literature ReviewDocument5 pagesMultiple Sclerosis and Exercice A Literature ReviewBelén María Vega AladueñaNo ratings yet
- NIH Public AccessDocument30 pagesNIH Public AccessElfrida FernandesNo ratings yet
- PARANEOPLASTICDocument8 pagesPARANEOPLASTICMuhammad Imran MirzaNo ratings yet
- ECMM Guidelines For MucormycosisDocument17 pagesECMM Guidelines For MucormycosisSaurabh AgrawalNo ratings yet
- Krupp 2007Document7 pagesKrupp 2007Linda CoronadoNo ratings yet
- fnagi-15-1184435Document15 pagesfnagi-15-1184435maria fensterseiferNo ratings yet
- 3 Pages Review-Mcdonald2018Document3 pages3 Pages Review-Mcdonald2018Riyan PratamaNo ratings yet
- Enfermedad MitocondrialDocument12 pagesEnfermedad MitocondrialOsvaldo CortésNo ratings yet
- Neurological Disease in Lupus: Toward A Personalized Medicine ApproachDocument12 pagesNeurological Disease in Lupus: Toward A Personalized Medicine ApproachjerejerejereNo ratings yet
- Kumar Et Al. - 2016 - International Myeloma Working Group Consensus CritDocument19 pagesKumar Et Al. - 2016 - International Myeloma Working Group Consensus CritCarina MoitaNo ratings yet
- 2021 09 24 21264020v1 FullDocument25 pages2021 09 24 21264020v1 FullElfina NataliaNo ratings yet
- Int J Dermatology - 2023 - Nihal - Treatment Options for Necrobiosis Lipoidica a Systematic ReviewDocument9 pagesInt J Dermatology - 2023 - Nihal - Treatment Options for Necrobiosis Lipoidica a Systematic Reviewevelyn.minichNo ratings yet
- Diagnostics: Isolated Cognitive Decline in Neurologically Stable Patients With Multiple SclerosisDocument13 pagesDiagnostics: Isolated Cognitive Decline in Neurologically Stable Patients With Multiple SclerosisVidushi ChhabraNo ratings yet
- WHO Central Nervous System Tumor Classification PDFDocument18 pagesWHO Central Nervous System Tumor Classification PDFAdli Wafi JabbarNo ratings yet
- Progressive Multiple SclerosissDocument10 pagesProgressive Multiple SclerosissMuhammad Imam NoorNo ratings yet
- Systemic - Sclerosis Nature Review 2014Document22 pagesSystemic - Sclerosis Nature Review 2014CT TANNo ratings yet
- Diabetic Neuropathy: What Does The Future Hold?Document7 pagesDiabetic Neuropathy: What Does The Future Hold?O. floriceNo ratings yet
- Diagnosis of Multiple Sclerosis - 2017 Revisions of McDonald PDFDocument13 pagesDiagnosis of Multiple Sclerosis - 2017 Revisions of McDonald PDFricky rdnNo ratings yet
- Newborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersDocument11 pagesNewborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- WHO 2016 Brain Tumor ClassificationDocument18 pagesWHO 2016 Brain Tumor ClassificationMu ZNo ratings yet
- LancetDocument9 pagesLancetRenju KuriakoseNo ratings yet
- Nanomaterials For Drug Delivery AssignmentDocument8 pagesNanomaterials For Drug Delivery AssignmentABDUL NAWAS K STUDENT - EEENo ratings yet
- Monti 2020Document8 pagesMonti 2020Ian MannNo ratings yet
- Fneur 12 639315Document13 pagesFneur 12 639315Muhammad Naqvi Al FarisiNo ratings yet
- Primer: Multiple SclerosisDocument27 pagesPrimer: Multiple SclerosisYabokuxtoriNo ratings yet
- International Myeloma Working Group Consensus Criteria For Response and Minimal Residual Disease Assessment in Multiple Myeloma LancetOncol-Aug2016Document19 pagesInternational Myeloma Working Group Consensus Criteria For Response and Minimal Residual Disease Assessment in Multiple Myeloma LancetOncol-Aug2016Andy LNo ratings yet
- Multiple SclerosisDocument22 pagesMultiple SclerosisInthe MOON youNo ratings yet
- Distrofias Musculares 2019 MercuriDocument14 pagesDistrofias Musculares 2019 Mercurimaria palaciosNo ratings yet
- 2017 Infectious Diseases Society of America's Clinical Practice Guidelines For Healthcare-Associated Ventriculitis and MeningitisDocument32 pages2017 Infectious Diseases Society of America's Clinical Practice Guidelines For Healthcare-Associated Ventriculitis and MeningitisMatus AlbertoNo ratings yet
- PIIS2213858721002357Document29 pagesPIIS2213858721002357Bladimir CentenoNo ratings yet
- Neuroimaging techniques assess inflammation in multiple sclerosisDocument41 pagesNeuroimaging techniques assess inflammation in multiple sclerosisLISA PERESNo ratings yet
- 668 FullDocument10 pages668 FullfranciscoNo ratings yet
- Guidelines For Healthcare-Associated VentriculitisDocument32 pagesGuidelines For Healthcare-Associated VentriculitisDaniel Martínez CruzNo ratings yet
- Duchenne Guidelines - Part 1Document17 pagesDuchenne Guidelines - Part 1guilherme.chaparimNo ratings yet
- Sepsis-Pathophysiology and Therapeutic ConceptsDocument22 pagesSepsis-Pathophysiology and Therapeutic ConceptsJuan ZamoraNo ratings yet
- 1032 FTPDocument7 pages1032 FTPGembyok KarnadiNo ratings yet
- Seminar: Christopher P Denton, Dinesh KhannaDocument15 pagesSeminar: Christopher P Denton, Dinesh KhannavieeveeNo ratings yet
- An Algorithm Approach To Diagnosing Bilateral Parotid EnlargementDocument8 pagesAn Algorithm Approach To Diagnosing Bilateral Parotid Enlargementalzeroelzain123No ratings yet
- Ev Estado de ConcienciaDocument18 pagesEv Estado de ConcienciaFabiolaNo ratings yet
- Inflammatory Cortical Demyelination in Early Multiple SclerosisDocument10 pagesInflammatory Cortical Demyelination in Early Multiple SclerosisWulan AzmiNo ratings yet
- Multiple Sclerosis, A Treatable DiseaseDocument7 pagesMultiple Sclerosis, A Treatable DiseaseMuhammad Imam NoorNo ratings yet
- 14 MsDocument18 pages14 MsMendila FerryNo ratings yet
- Rheumatoid Arthritis Lancet 2009Document14 pagesRheumatoid Arthritis Lancet 2009pispi_896094No ratings yet
- Perez-Cerdá - Inflammation Neurodegeneration Multiple SclerosisDocument8 pagesPerez-Cerdá - Inflammation Neurodegeneration Multiple SclerosisinesNo ratings yet
- Neuromuscular Disorders Presenting in NewbornsDocument1 pageNeuromuscular Disorders Presenting in NewbornsasasakopNo ratings yet
- Complications of MPSDocument1 pageComplications of MPSasasakopNo ratings yet
- Causes of Optic NeuropathyDocument1 pageCauses of Optic NeuropathyasasakopNo ratings yet
- Diagnostic Criteria ADEM in ChildrenDocument1 pageDiagnostic Criteria ADEM in ChildrenasasakopNo ratings yet
- MRI and Neuropathology of AHLDocument1 pageMRI and Neuropathology of AHLasasakopNo ratings yet
- MRI of CIS Presenting As Optic NeuritisDocument1 pageMRI of CIS Presenting As Optic NeuritisasasakopNo ratings yet
- Cervicogenic HeadacheDocument32 pagesCervicogenic HeadacheasasakopNo ratings yet
- NMOSD Diagnostic Criteria For AdultsDocument1 pageNMOSD Diagnostic Criteria For AdultsasasakopNo ratings yet
- Findings Atypical For NMOSDDocument1 pageFindings Atypical For NMOSDasasakopNo ratings yet
- Fahrs Disease and Aspergers Syndrome inDocument27 pagesFahrs Disease and Aspergers Syndrome inSaran RalucaNo ratings yet
- MRI Optic NeuritisDocument1 pageMRI Optic NeuritisasasakopNo ratings yet
- Characteristics of SCA TypesDocument1 pageCharacteristics of SCA TypesasasakopNo ratings yet
- Neurology and The KidneyDocument12 pagesNeurology and The KidneyasasakopNo ratings yet
- Concise Pocket Medical Dictionary 2edDocument715 pagesConcise Pocket Medical Dictionary 2edSai harshaNo ratings yet
- Advantage of Modified MRI Protocol For HDocument148 pagesAdvantage of Modified MRI Protocol For HasasakopNo ratings yet
- Wernickes Encephalopathy Following HyperDocument44 pagesWernickes Encephalopathy Following HyperasasakopNo ratings yet
- Posterior Reversible Encephalopathy SyndDocument7 pagesPosterior Reversible Encephalopathy SyndasasakopNo ratings yet
- A Fatal Case of Al Encephalopathi in A Patient With Severe Chronic Renal Failure Not On Dialysis PDFDocument3 pagesA Fatal Case of Al Encephalopathi in A Patient With Severe Chronic Renal Failure Not On Dialysis PDFasasakopNo ratings yet
- Pitfalls in Cervical Spine SurgeryDocument301 pagesPitfalls in Cervical Spine Surgerymrz200No ratings yet
- Arterijskovenski Malformati-Dijagnosticke Poteskoce Prikaz Dva SlucajaDocument8 pagesArterijskovenski Malformati-Dijagnosticke Poteskoce Prikaz Dva SlucajaasasakopNo ratings yet
- Halucinations in Patients With ParkinsonDocument189 pagesHalucinations in Patients With ParkinsonasasakopNo ratings yet
- Anti LGL1 Limbic EncephalitisDocument4 pagesAnti LGL1 Limbic EncephalitisasasakopNo ratings yet
- Affective Disorders: Clinical Picture, Diagnosis and Therapeutic PrinciplesDocument45 pagesAffective Disorders: Clinical Picture, Diagnosis and Therapeutic Principlesasasakop100% (1)
- Lipds and CarbohydratesDocument4 pagesLipds and CarbohydratesMilenaNo ratings yet
- Lactate Dehydrogenas E: Clinical Chemistry Post-Laboratory DiscussionDocument21 pagesLactate Dehydrogenas E: Clinical Chemistry Post-Laboratory DiscussionValdez Francis ZaccheauNo ratings yet
- (Series in Radiology 24) Raad H. Mohiaddin MD, MSC, Donald B. Longmore FRCS, FRCR (Auth.) - MRI Atlas of Normal Anatomy-Springer Netherlands (1992)Document200 pages(Series in Radiology 24) Raad H. Mohiaddin MD, MSC, Donald B. Longmore FRCS, FRCR (Auth.) - MRI Atlas of Normal Anatomy-Springer Netherlands (1992)Tina SNo ratings yet
- Case Based Learning#3Document4 pagesCase Based Learning#3Imran khanNo ratings yet
- (The Natural History of The Crustacea) Les Watling, Martin Thiel (Eds.) - Functional Morphology and Diversity. 1-Oxford University Press (2013)Document515 pages(The Natural History of The Crustacea) Les Watling, Martin Thiel (Eds.) - Functional Morphology and Diversity. 1-Oxford University Press (2013)Yamaly Barragán MarínNo ratings yet
- Orthodontics AssignmentDocument4 pagesOrthodontics AssignmentTasneem SaleemNo ratings yet
- BONAVERA CountDocument15 pagesBONAVERA CountpsychejaneNo ratings yet
- VS TLN 27547 2208 3Document12 pagesVS TLN 27547 2208 3Deni ArdianNo ratings yet
- Glenoid Fossa RemodellingDocument59 pagesGlenoid Fossa RemodellingArnabNo ratings yet
- Biological Science Canadian 2Nd Edition Freeman Solutions Manual Full Chapter PDFDocument38 pagesBiological Science Canadian 2Nd Edition Freeman Solutions Manual Full Chapter PDFkieranthang03m100% (14)
- From Wikipedia, The Free Encyclopedia: Jump To:, For Other Uses, SeeDocument19 pagesFrom Wikipedia, The Free Encyclopedia: Jump To:, For Other Uses, Seenassamerg23No ratings yet
- Osmosis: Major Fluid CompartmentDocument9 pagesOsmosis: Major Fluid CompartmentMarielle ChuaNo ratings yet
- Fundamentals of the Human Body: HomeostasisDocument34 pagesFundamentals of the Human Body: HomeostasisLiana ChanNo ratings yet
- Cookeville Regional Medical Center Severe Sepsis/Septic Shock Clinical PathwayDocument4 pagesCookeville Regional Medical Center Severe Sepsis/Septic Shock Clinical PathwayArnelli HutagalungNo ratings yet
- English 2-09-Structure Transisiton QuestionsDocument8 pagesEnglish 2-09-Structure Transisiton QuestionsDing DongNo ratings yet
- Visualization Peaceful MeadowDocument2 pagesVisualization Peaceful MeadowSagaya AmithaNo ratings yet
- Updated NMAT Study Guide by Astro Dok PDFDocument36 pagesUpdated NMAT Study Guide by Astro Dok PDFJeremy Calderon100% (1)
- Psychology of HorrorDocument29 pagesPsychology of HorrorKurumi ShimuraNo ratings yet
- PHM 3471 Merged Week (1-6)Document303 pagesPHM 3471 Merged Week (1-6)Lisa MuthiniNo ratings yet
- Electrodiagnostic ProceduresDocument3 pagesElectrodiagnostic Proceduresakheel ahammedNo ratings yet
- Animal Diversity and ClassificationDocument45 pagesAnimal Diversity and ClassificationSafiqa Tasfia100% (1)
- Download ebook Neuroanatomy Text And Atlas Pdf full chapter pdfDocument67 pagesDownload ebook Neuroanatomy Text And Atlas Pdf full chapter pdfsue.zuniga537100% (19)
- C:/Users/Prima Agung Laksono/Pictures/tugas DR NP/Philips-Goldway-G30E-G40E-preconfigured-Patient - Monitors PDFDocument10 pagesC:/Users/Prima Agung Laksono/Pictures/tugas DR NP/Philips-Goldway-G30E-G40E-preconfigured-Patient - Monitors PDFPrima Agung LNo ratings yet
- Words of Listening Level 5 U3Document15 pagesWords of Listening Level 5 U3Obaid KhanNo ratings yet
- Fdocuments - in - Digestion of Starch by Salivary AmylaseDocument13 pagesFdocuments - in - Digestion of Starch by Salivary AmylaseGSI BHUBANESWAR100% (1)
- Neet Wizz Bio Class 12Document89 pagesNeet Wizz Bio Class 12Aarthi T. UNo ratings yet
- ProteaseDocument18 pagesProteasePriyaNo ratings yet
- Medical Surgical Nursing Module 14Document31 pagesMedical Surgical Nursing Module 14weissNo ratings yet
- Module 2-The Biology of MotivationDocument42 pagesModule 2-The Biology of MotivationPadmaja PradeepNo ratings yet
- ICCAT Manual BETDocument25 pagesICCAT Manual BETRUBÉN CASTIÑEIRA PÉREZNo ratings yet