Professional Documents
Culture Documents
Distrofias Musculares 2019 Mercuri
Uploaded by
maria palaciosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Distrofias Musculares 2019 Mercuri
Uploaded by
maria palaciosCopyright:
Available Formats
Seminar
Muscular dystrophies
Eugenio Mercuri, Carsten G Bönnemann, Francesco Muntoni
Muscular dystrophies are primary diseases of muscle due to mutations in more than 40 genes, which result in Lancet 2019; 394: 2025–38
dystrophic changes on muscle biopsy. Now that most of the genes responsible for these conditions have been See Editorial page 1966
identified, it is possible to accurately diagnose them and implement subtype-specific anticipatory care, as complications Pediatric Neurology Unit,
such as cardiac and respiratory muscle involvement vary greatly. This development and advances in the field of Università Cattolica del Sacro
Cuore Roma, Rome, Italy
supportive medicine have changed the standard of care, with an overall improvement in the clinical course, survival,
(Prof E Mercuri PhD); Nemo
and quality of life of affected individuals. The improved understanding of the pathogenesis of these diseases is being Clinical Centre, Fondazione
used for the development of novel therapies. In the most common form, Duchenne muscular dystrophy, a few Policlinico Universitario A
personalised therapies have recently achieved conditional approval and many more are at advanced stages of clinical Gemelli IRCCS, Rome, Italy
(Prof E Mercuri); Neuromuscular
development. In this Seminar, we concentrate on clinical manifestations, molecular pathogenesis, diagnostic strategy,
and Neurogenetic Disorders of
and therapeutic developments for this group of conditions. Childhood Section, National
Institute of Neurological
Introduction causation, together with function of the responsible Disorders and Stroke,
National Institutes of Health,
Muscular dystrophies are a group of genetically inherited proteins. The main protein classes involved are
Bethesda, MD, USA
degenerative disorders of muscle, sharing clinical extracellular matrix and basement membrane proteins, (Prof C G Bönnemann PhD);
features of progressive muscle weakness and dystrophic sarcolemma-associated proteins, enzymes or proteins Dubowitz Neuromuscular
pathological appearance on muscle biopsy.1 In a with putative enzymatic function, nuclear membrane Centre, University College
London, Great Ormond Street
Seminar2 published in 2013, we reported how a better proteins, sarcomeric proteins, endoplasmic reticulum
Institute of Child Health,
understanding of the genetic basis and mechanisms proteins, and other proteins. London, UK
underlying these disorders has allowed the scientific Congenital muscular dystrophies are typically due to (Prof F Muntoni MD); and
community to appreciate a previously not anticipated mutations in proteins located in the extracellular matrix, National Institute for Health
Research Great Ormond Street
genetic, mechanistic, and clinical heterogeneity. From or external membrane proteins or enzymes involved in Hospital Biomedical Research
a clinical perspective the definition expanded to include their post-translational modification (table 1; figure 1). Centre, London, UK
conditions with associated involvement of other Mutations in nuclear proteins typically result in (Prof F Muntoni)
organs—for example, the CNS; from a genetic Emery–Dreifuss muscular dystrophy whereas defects in Correspondence to:
perspective, a much larger number of individually rare sarcolemmal and sarcomeric proteins mostly cause limb Prof Francesco Muntoni,
Dubowitz Neuromuscular
conditions were described.3,4 At the time, the development girdle muscular dystrophies (table 2).
Centre, University College
of novel therapeutic approaches had just begun their London, Great Ormond Street
course.5–9 In this Seminar, we will discuss how the field Pathogenesis Institute of Child Health,
has advanced over the last 5 years. We will provide an Extracellular matrix and basement membrane proteins London WC1N 1EH, UK
f.muntoni@ucl.ac.uk
update on the mechanisms that can result in muscular Abnormalities in extracellular matrix and basement mem-
dystrophy and an indication on how experimental brane proteins result in the most common variants of
therapeutic approaches are rapidly advancing. congenital muscular dystrophies: collagen 6, laminin 211,
and the cellular receptor α-dystroglycan (figure 1).13
Classification Collagen 6 deficiency can be caused by both autosomal
Molecular genetic tools have allowed the identification of recessive or dominant mutations in any of the three major
more than 40 genes involved in muscular dystrophies,10,11 collagen 6 alpha-chain genes (COL6A1–3; figure 2).14–16 The
with very rare muscular dystrophy variants being con- severity ranges from the congenital muscular dystrophy
tinually identified. The classification recognises conditions variant—Ullrich congenital muscular dystrophy—to a
with early onset grouped under the congenital muscular milder form that resembles a limb girdle muscular
dystrophies, and later-onset conditions (eg, limb girdle dystrophy (Bethlem myopathy).
muscular dystrophies). Allelic mutations in several genes
can cause onset either before or after the acquisition of
ambulation, providing a pragmatic boundary between Search strategy and selection criteria
congenital muscular dystrophies and limb girdle muscular We identified data for this Seminar from MEDLINE, Current
dystrophies. Additional common variants are Duchenne Contents, PubMed, and references from relevant articles
muscular dystrophy, Becker muscular dystrophy, Emery– using the search terms “muscular dystrophy”, “Duchenne”,
Dreifuss muscular dystrophy, and facioscapulohumeral “congenital”, “limb girdle”, “therapy”, and “care”. We only
muscular dystrophy, which were all recognised and clearly included abstracts and reports from meetings when they
described long before most of the congenital muscular related directly to previously published work. Only articles
dystrophies and limb girdle muscular dystrophies, because published in English between 2013 and 2018 were discussed.
of their unique clinical features or high incidence, or both. We also identified current clinical trials from ClinicalTrials.gov
We favour a classification recognising the major group and ClinicalTrialsRegister.eu.
of conditions, and the genes responsible for their
www.thelancet.com Vol 394 November 30, 2019 2025
Seminar
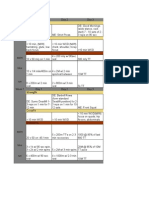
Gene Protein Disease phenotypes
Extracellular matrix proteins
6q22–23 LAMA2 Laminin subunit α-2 chain of merosin Primary merosin deficiency
21q22.3 and 2q37 COL6A1, COL6A2, Collagen type 6, subunit α-1 and 2 Ullrich congenital muscular dystrophy
COL6A3
External sarcolemmal protein
12q13 ITGA7 Integrin α-7 Integrin β-7-related congenital muscular dystrophy
Dystroglycan and glycosyltransferase enzymes
9q34.1 POMT1 Protein O-mannosyl-transferase 1 Walker-Warburg syndrome, muscle eye brain disease, congenital muscular dystrophy with cerebellar
involvement, congenital muscular dystrophy with mental retardation and microcephaly, congenital
muscular dystrophy with no mental retardation
14q24.3 POMT2 Protein O-mannosyl-transferase 2 Walker-Warburg syndrome, muscle eye brain disease, congenital muscular dystrophy with cerebellar
involvement, congenital muscular dystrophy with mental retardation and microcephaly
1q32–34 POMGNT1 Protein O-linked-mannose Walker-Warburg syndrome, muscle eye brain disease, congenital muscular dystrophy with cerebellar
β-1,2-N-acetylglucosaminyltransferase 1 involvement
19q13.3 FKRP Fukutin-related protein Walker-Warburg syndrome, muscle eye brain disease, congenital muscular dystrophy with cerebellar
involvement, congenital muscular dystrophy with mental retardation and microcephaly, congenital
muscular dystrophy with no mental retardation
9q31 FCMD Fukutin Fukuyama congenital muscular dystrophy, congenital muscular dystrophy with mental retardation,
congenital muscular dystrophy with no mental retardation
22q12.3–13.1 LARGE Glycosyltransferase-like protein Walker-Warburg syndrome, muscle eye brain disease, white matter changes
1q12–21 DPM2 and DPM3 Dolichyl-phosphate mannosyltransferase Congenital muscular dystrophy with mental retardation and severe epilepsy
polypeptide 2 and 3
7p21.2 ISPD Isoprenoid synthase domain Walker-Warburg syndrome, limb girdle muscular dystrophy
3p22.1 GTDC2 Protein O-linked-mannose Walker-Warburg syndrome
β-1,4-N-acetylglucosaminyltransferase 2
11q13.2 B3GALNT2 β-1,3-N-acetylgalactosaminyltransferase 2 Walker-Warburg syndrome, muscle eye brain disease
3p21.31 GMPPB GDP-mannose pyrophosphorylase B Congenital muscular dystrophy with mental retardation and severe epilepsy
3p21 DAG1 Dystroglycan Primary dystroglycanopathy, limb girdle muscular dystrophy with early onset and mental retardation
(normal brain MRI), allelic mutation causes congenital muscular dystrophy
8p11.21 SGK196 Protein O-mannose kinase Muscle eye brain disease
1q42 Unknown Unknown Congenital muscular dystrophy type 1B
Endoplasmic reticulum protein
1p35–36 SEPN1 Selenoprotein N1 Congenital muscular dystrophy with spinal rigidity
Nuclear envelope proteins
6q25 SYNE1 Nesprin-1 Congenital muscular dystrophy with adducted thumbs
1q21.2 LMNA Lamin-A Congenital laminopathy Emery–Dreifuss muscular dystrophy
14q23.2 SYNE2 Nesprin-2 Emery–Dreifuss muscular dystrophy
3p25.1 LUMA Transmembrane protein 43 Emery–Dreifuss muscular dystrophy
Xq28 EMD Emerin Emery–Dreifuss muscular dystrophy
Mitochondrial membrane protein
22q13 CHKB Choline kinase Mitochondrial congenital muscular dystrophy
Table 1: Congenital muscular dystrophies associated with the different protein classes
Laminin α2, which is encoded by the LAMA2 gene, is Proteins belonging to this group give rise to Duchenne
the large chain in the laminin heterotrimer laminin 211, muscular dystrophy—the most common form in
composed of the subunits α2, β1, and γ1, which represents childhood—and its milder allelic condition known as
the main isoform in the basement membrane of muscle Becker muscular dystrophy, which is due to mutations
(figure 2). Recessive mutations in LAMA2 commonly in the X-linked dystrophin gene (figures 1, 2), and to
lead to complete loss of protein production, associated 4 autosomal recessive limb girdle muscular dystrophies
with severe congenital presentation;17 rare milder variants known as sarcoglycanopathies, each secondary to
can resemble limb girdle muscular dystrophy.18 mutations in one of four sarcoglycan genes (table 2).
The dystrophin-associated glycoprotein complex has an
Sarcolemma-associated proteins important role in stabilising the muscle fibres against
The major subcomplex in this category is the dystrophin- the mechanical forces of muscle contraction by providing
associated glycoprotein complex, which comprises a shock-absorbing connection between the cytoskeleton
dystrophin and sarcoglycans, in addition to dystroglycan. and the extracellular matrix.
2026 www.thelancet.com Vol 394 November 30, 2019
Seminar
A separate but functionally related group of sarcolemmal Extracellular matrix
proteins are dysferlin and anoctamin 5. Dysferlin has a
crucial role in the repair process of the sarcolemma,19–21 and
anoctamin 5 also contributes to this process.22–24 Dysferlin
Laminin
interacts at the sarcolemma with caveolin 3, which is
involved in a rare limb girdle muscular dystrophy variant, Myofibre
DAGC
while mutations in the polymerase I and transcript release
factor (PTRF, also known as cavin) gene, necessary for Dysferlin, ANO5 Dystrophin
Nuclear
caveolar formation, result in a secondary deficiency of envelope proteins
caveolin 3 and associated limb girdle muscular dystrophy.25,26
Nucleus
Sarcomeric proteins
Enzymes or proteins with putative enzymatic function
Defects in the glycosylation of α-dystroglycan were origi-
nally identified in several congenital muscular dystrophy Golgi and endoplasmic
reticulum glycosyltransferases
subtypes but subsequently in limb girdle muscular
dystrophies (table 1). These conditions are referred to as
dystroglycanopathies.8,27 α-dystroglycan is highly post-
translationally modified via numerous enzymatic steps.28
Binding of this cellular receptor to its muscle extracellular
Figure 1: A schematic representation of the major classes of proteins involved in muscular dystrophies
matrix partners, of which laminin is a major one (figure 1),
DAGC=dystrophin-associated glycoprotein complex. ANO5=anoctamin 5 protein.
is dependent on its proper glycosylation, and mutations in
18 proteins with demonstrated or putative enzymatic
function give rise to a dystroglycanopathy (table 1). The Sarcomeric proteins
clinical and pathological features range from limb girdle Although several of these disorders are subsumed
muscular dystrophy phenotypes to congenital muscular under the non-dystrophic congenital myopathies, recent
dystrophy with structural brain involvement,29–31 under- data also indicate involvement of sarcomeric proteins in
scoring a fundamental role of α-dystroglycan glycosylation dystrophic muscle disorders. For the giant gene titin,
not only for muscle but also basement membrane main- encoded by TTN, the full range of phenotypes is only
tenance and synaptic function of the brain.32 recently emerging, owing to the extremely large size of
Enzymes not involved in α-dystroglycan glycosylation this gene for which next-generation sequencing is
but that might have a role in muscle dystrophy have been necessary. At variance with most of the congenital mus-
reported (table 2). Calpain 3 is a Ca²+-activated neutral cular dystrophies and limb girdle muscular dystrophies,
protease. The precise pathophysiology of the corres- sarcomeric proteins-associated conditions give rise to a
ponding dystrophy, limb girdle muscular dystrophy, is still prominent or even predominantly distal distribution of
incompletely understood. muscle weakness.37,38 In some of these conditions, and in
particular TTN and MYH7,39 severe cardiomyopathy,
Nuclear membrane proteins usually dilated, can coexist, while allelic mutations in the
The nuclear envelope is composed of two membranes: same genes might lead to cardiomyopathy in isolation.
the outer and the inner nuclear membranes, which
interact with the underlying nuclear lamina. Mutations in Endoplasmic reticulum proteins
proteins localised in the nuclear envelope, including Mutations in the protein encoded by the TRAPPC11 gene,
lamin A/C, emerin, nesprin 1 and 2, and TMEM43 a subunit of the transport particle protein complex, have
(LUMA) have been implicated in conditions that share been reported both in a form of limb girdle muscular
a progressive muscular dystrophy phenotype named dystrophy (LGMD2S)40 and congenital muscular
Emery–Dreifuss muscular dystrophy.33,34 Mutations in dystrophy with cerebellar involvement.41 Mutations in
another nuclear membrane protein, matrin 3, have been another protein expressed both at the endoplasmic
described in a distal myopathy with vocal cord paralysis.35 reticulum and the sarcolemma (blood vessel epicardial
Remarkable divergence of phenotypes exists because of substance or POPDC1) result in an autosomal recessive
allelic mutations in these genes, suggesting discrete limb girdle muscular dystrophy characterised by slowly
roles of different protein domains.36 The most striking progressive weakness and cardiac arrhythmias.42
example are mutations in lamin A/C, which can give
rise to Emery–Dreifuss muscular dystrophy, isolated Other proteins
cardiomyopathy with conduction system disease, limb Facioscapulohumeral muscular dystrophy-1 is one of
girdle muscular dystrophy with lipodystrophy, lipodys- the most common autosomal dominant adult muscular
trophy with mandibuloacral dysplasia, congenital muscu- dystrophies. Both cellular localisation and presumed
lar dystrophy, peripheral neuropathy, lethal restrictive function of the defective protein cannot easily fit in our
dermopathy, and Hutchinson–Gilford progeria. classification scheme. The causative gene defect was
www.thelancet.com Vol 394 November 30, 2019 2027
Seminar
Inheritance Locus Gene Protein Main localisation
LGMD type 1A (myofibrillar myopathy) AD 5q31 MYOT Myotilin Sarcomeric-associated protein (Z disc)
LGMD type 1B (Emery–Dreifuss musclar dystrophy) AD 1q21.2 LMNA Lamin A/C Nuclear lamina-associated protein
LGMD type 1C (rippling muscle disease) AD 3p25 CAV3 Caveolin-3 Sarcolemmal-associated protein
LGMD type 1D (D1 DNAJB6-related LGMD) AD 7q DNAJB6 Co-chaperone DNAJB6 Sarcomeric-associated protein (Z disc)
LGMD type 1E (myofibrillar myopathy) AD 6q23 DES Desmin Intermediate filament protein
LGMD type 1F (D2 TNP03-related LGMD) AD 7q32 TNPO3 Transportin-3 Nucleus
LGMD type 1G (D3 HNRNPDL-related LGMD) AD 4p21 HNRDL Heterogeneous nuclear ribonucleoprotein D-like Nucleus
protein
LGMD type 1H AD 3p23–25 Unknown Unknown Not confirmed
LGMD type 1L (D4 calpain3-related LGMD) AD 15q15.1 CAPN3 Calpain-3 Myofibril-associated proteins
LGMD type 2A (R1 calpain3-related LGMD) AR 15q15.1 CAPN3 Calpain-3 Myofibril-associated proteins
LGMD type 2B (R2 dysferlin-related LGMD) AR 2p13 DYSF Dysferlin Sarcolemmal-associated protein
LGMD type 2C (R5 γ-sarcoglycan-related LGMD) AR 13q12 SGCG γ-sarcoglycan Sarcolemmal-associated protein
LGMD type 2D (R3 α-sarcoglycan-related LGMD) AR 17q12–q21.33 SGCA α-sarcoglycan Sarcolemmal-associated protein
LGMD type 2E (R4 β-sarcoglycan-related LGMD) AR 4q12 SGCB β-sarcoglycan Sarcolemmal-associated protein
LGMD type 2F (R6 δ-sarcoglycan-related LGMD) AR 5q33 SGCD δ-sarcoglycan Sarcolemmal-associated protein
LGMD type 2G (R7 telethonin-related LGMD) AR 17q12 TCAP Titin-cap (telethonin) Sarcomeric-associated protein (Z disc)
LGMD type 2H (R8 TRIM 32-related LGMD) AR 9q31–34 TRIM32 Tripartite motif-containing 32 (ubiquitin ligase) Sarcomeric-associated protein (Z disc)
LGMD type 2I (R9 FKRP-related LGMD) AR 19q13.3 FKRP Fukutin-related protein Putative glycosyltransferase enzymes
LGMD type 2J (R10 titin-related LGMD) AR 2q31 TTN Titin Sarcomeric protein
LGMD type 2K (R11 POMT1-related LGMD) AR 9q34.1 POMT1 Protein O-mannosyl-transferase 1 Glycosyltransferase enzymes
LGMD type 2L (R12 anoctamin 5-related LGMD) AR 11p14.3 ANO5 Anoctamin 5 Transmembrane protein (possibly
sarcoplasmic reticulum)
LGMD type 2M (R13 Fukutin-related LGMD) AR 9q31 FKTN Fukutin Putative glycosyltransferase enzymes
LGMD type 2N (R14 POMT2-related LGMD) AR 14q24.3 POMT2 Protein O-mannosyl-transferase 2 Glycosyltransferase enzymes
LGMD type 2O (R15 POMGnT1-related LGMD) AR 1p34 POMGNT1 Protein O-linked-mannose Glycosyltransferase enzymes
β-1,2-N-acetylglucosaminyltransferase 1
LGMD type 2P (R16 α-dystroglycan-related LGMD) AR 3p21 DAG1 Dystrophin-associated glycoprotein 1 Sarcolemmal-associated protein
LGMD type 2Q (R17 plectin-related LGMD) AR 8q24 PLEC1 Plectin-1 Sarcomeric-associated protein (Z disc)
LGMD type 2R (myofibrillar myopathy) AR 2q35 DES Desmin Links to sarcolemma, Z disc, nuclear
membrane
LGMD type 2S (R18 TRAPPC11-related LGMD) AR 4q35 TRAPPC11 Trafficking protein particle complex subunit 11 Endoplasmic reticulum
LGMD type 2T (R19 GMPPB-related LGMD) AR 3p21 GMPPB GDP-mannose pyrophosphorylase B Glycosyltransferase enzymes
LGMD type 2U (R20 ISPD-related LGMD) AR 7p21 ISPD Isoprenoid synthase domain-containing protein Glycosyltransferase enzymes
LGMD type 2V (Pompe disease) AR 17q25 GAA Lysosomal α-glucosidase Lysosome
LGMD type 2W (PINCH-2-related myopathy) AR 2q14 LIMS2 LIM and senescent cell antigen-like-containing domain Focal adhesion and nucleus
protein 2
LGMD type 2X (BVES-related myopathy) AR 6q21 BVES Blood vessel epicardial substance Sarcolemmal-associated protein
LGMD type 2Y (TOR1AIP1-related myopathy) AR 3q13.33 POGLUT1 Protein O-glucosyl-transferase 1 Endoplasmic reticulum
Disease names in parentheses are the recently suggested new nomenclature from the 2018 European Neuromuscular Centre workshop.12 LGMD=limb girdle muscular dystrophy. AD=autosomal dominant.
AR=autosomal recessive.
Table 2: Protein mutations associated with LGMDs
established following the finding of the inefficient repres- stable and toxic for the cell.44 In the clinically similar
sion of the transcriptional factor DUX4.43 Patients with facioscapulohumeral muscular dystrophy-2, de-repression
facioscapulohumeral muscular dystrophy-1 have a deletion of DUX4 is based on hypomethylation of the same
of integral copies of a tandemly repeated 3∙2 kb unit (D4Z4 4q35 locus, as a result of mutations in the chromosome
repeat) at the subtelomeric region 4q35. This deletion modifier SMCHD1 located on chromosome 18p11.
loosens transcriptional repression of DUX4. In addition,
for the disease to develop, the deleted 4q35 allele must Epidemiology
be associated with a specific polymorphic variant in the Duchenne muscular dystrophy represents the most
final DUX4-containing unit, in which a single nucleotide common muscular dystrophy in children, with an
polymorphism leads to a canonical polyadenylation signal annual incidence of about one in 5000 live males45
for transcripts derived from DUX4, which makes it and an estimated point prevalence of 8∙29 per
2028 www.thelancet.com Vol 394 November 30, 2019
Seminar
A B C
D E F
*
*
*
* *
G H I
J K L
Figure 2: Muscle biopsy sections stained with haematoxylin and eosin, immunostaining, immunolabelling, or immunofluorescent double-labelling,
reduced by 50% from × 250
(A) Histologically normal muscle biopsy showing a compact fascicular pattern. The fascicles are segregated by thin perimysial connective tissue and comprise
polygonal-shaped myofibres in cross-section with peripherally placed myonuclei. (B) Biopsy from a patient with Duchenne muscular dystrophy showing marked
variation in fibre size, increased rounding and hypercontraction of fibres, and clusters of basophilic regenerating fibres with internal nuclei with accompanying
fibrosis and fatty infiltration in the perimysium and endomysium. (C) These dystrophic changes are milder in the biopsy of a patient with Becker muscular
dystrophy. (D) Immunostaining with an antibody to an epitope within the rod domain of dystrophin shows uniform sarcolemmal labelling in the unaffected
individual. (E) There is a complete absence of sarcolemmal dystrophin labelling in Duchenne muscular dystrophy, except for a few strongly labelled revertant fibres
as indicated by the asteriscs. (F) In Becker muscular dystrophy, there is patchy, mild-to-moderate reduction in sarcolemmal dystrophin labelling. (G) Biopsy from a
patient with complete laminin α-2 deficient muscular dystrophy showing marked dystrophic features with striking fatty infiltration. (H) Immunolabelling for
laminin α-2 (300 kDa antibody) showing complete absence at the myofibre basal lamina, as well as in the intramuscular nerves as shown by the arrows. There is
secondary upregulation of laminin α-5 at the myofibre basal lamina as shown in the inset. (I) In partially laminin α-2 deficient muscular dystrophy, there is variable,
patchy, mild-to-moderate reduction of laminin α-2 labelling at the basal lamina of myofibres. (J) A biopsy from a patient with Ullrich muscular dystrophy shows
marked dystrophic changes with striking fatty infiltration. (K) Immunofluorescent double-labelling with an antibody to an epitope in the heterotrimeric domain of
collagen 6 (green) and perlecan (red; a myofibre basal lamina marker) showing near-total absence of collagen 6 at the basal lamina accompanied by increased
deposition in the interstitium. (L) In Becker muscular dystrophy, there is variable, patchy, partial reduction of collagen 6 at the basal lamina.
100 000 males.46 Becker muscular dystrophy has a laminin α-2 related, or collagen 6 Ullrich congenital
prevalence of 7∙29 per 100 000 males. Regarding muscular dystrophy).48,49
congenital muscular dystrophies, recent studies based Regarding limb girdle muscular dystrophies, two large
on nationwide referrals reported a point prevalence of studies using next-generation sequencing approaches
0∙563 per 100 000 in Italy.47 This finding and other identified a final diagnosis in 59% and 27% of cases,
recent studies described a similar frequency of the respectively.50,51 In both studies, autosomal recessive forms
three most common variants (dystroglycanopathies, accounted for the great majority of probands (>80%). In
www.thelancet.com Vol 394 November 30, 2019 2029
Seminar
the former study,50 limb girdle muscular dystrophy D2A birth, with reduced fetal movement and polyhydramnios;
(30% of probands) and limb girdle muscular dystrophy or in the first year of life.
D2B (23%) were the most frequent forms, followed by the LAMA2-related congenital muscular dystrophy is
sarcoglycanopathies (21%) and limb girdle muscular evident in the first few days or weeks of life with
dystrophy D2I (10%). In the latter study,51 phenocopies of generalised hypotonia, paucity of antigravity movements,
limb girdle muscular dystrophy such as the glycogen talipes, occasional hip and knee contractures, and marked
storage disorder Pompe disease accounted for about elevation of serum creatinine kinase concentration. Arm
1% of the 4656 cases studied. This finding is important in and axial weakness predominates the early clinical course,
view of the availability of enzyme replacement therapy for but lower limb weakness and progressive contractures
this metabolic disease. In the populations of northern invariably develop. Affected children typically only acquire
Europe, limb girdle muscular dystrophy D2I is one of the independent sitting, and only rarely the ability to stand
most common variants,52 with a prevalence of one per or walk. Swallowing difficulties are common and result
54 000 people and a carrier frequency of one per 116 in in inadequate ability to thrive in the first few years of
Denmark52 and the UK.46 life. Respiratory muscle weakness determines frequent
Regarding dominant disorders, facioscapulohumeral chest infections and respiratory insufficiency requiring
muscular dystrophy-1 is the most common form with nocturnal non-invasive ventilation by mid-teenage years.
an estimated prevalence of 1–1500 per 20 000.53,54 Scoliosis is common. Cognitive function is typically
preserved, although brain imaging shows white matter
Clinical manifestations and diagnosis abnormalities resembling a leukodystrophy. Focal epilepsy
The previous version of this Seminar2 and other recent occurs in about 20% of affected children, with a very small
reviews provide in-depth information about the onset proportion having neuronal migration disorder affecting
and progression of clinical signs in the different forms of the occipital lobes. Life expectancy is highly dependent on
muscular dystrophies.55–57 optimal standards of care, and currently survival in early
In order to facilitate the diagnostic pathways, an adult life can be expected in the majority of patients.
integrated approach combining clinical signs, age of onset, Clinically overt cardiac involvement is exceptional. The
distribution of muscle weakness, and cardiac involvement diagnosis is suggested by the severely reduced or absent
with laboratory results (serum creatine kinase concen- protein expression in muscle (figure 2) or in skin, and
trations, which are typically and markedly elevated in requires genetic confirmation.58
muscular dystrophies), muscle biopsy (figure 2), and Ullrich COL6-related congenital muscular dystrophy
muscle imaging (figure 3) is useful. For some subtypes of might also be present at birth, with typical skeletal
congenital muscular dystrophies, brain imaging can also deformities including kyphoscoliosis, contractures of
be useful. Diagnostic guidelines are available50,58–60 and a the larger joints, and a striking hyperlaxity of hands and
For the limb girdle muscular comprehensive e-tool developed by one of the limb girdle feet, which is often associated with torticollis and hip
dystrophy diagnostic assistant muscular dystrophy advocacy groups provides helpful dysplasia. Serum creatine kinase concentration is nor-
e-tool see https://www.jain-
foundation.org/lgmd-subtyping-
information about how to approach the diagnosis of such mal or mildly elevated. Nearly 50% of patients acquire
diagnosis-tool diseases. independent ambulation, which is however lost by their
early teens as a result of progressive muscle weakness
Congenital muscular dystrophies and of joint contractures with rigidity of the spine.
Congenital muscular dystrophies typically describe Inadequate ability to thrive commonly develops requiring
children symptomatic at birth; sometimes also before gastrostomy; respiratory insufficiency sets in early and is
Becker muscular dystrophy LGMD2A LGMD2B/MM LGMD2D Facioscapulohumeral
muscular dystrophy
Figure 3: Muscle MRI (T1 images) of the thigh and calf muscles
The upper panels show the thigh muscles and the lower panels show the calf muscles. Muscle MRI shows distinct pattern of selective muscle involvement in the
different muscular dystrophies. LGMD=limb girdle muscular dystrophy. LGMD2A=calpain-related LGMD. LGMD2B/MM=dysferlin-related LGMD/Miyoshi myopathy.
LGMD2D=α sarcoglycan deficient LGMD.
2030 www.thelancet.com Vol 394 November 30, 2019
Seminar
fully manifested by the early teens requiring nocturnal leading to loss of independent ambulation by the age of
respiratory support.61,62 Cognitive and cardiac function 12 years (mean age of 9∙5 years), followed by scoliosis,
are spared. The diagnosis is made by observation of loss of upper limb function, respiratory insufficiency,
absence or more frequently reduction in collagen 6 and cardiomyopathy. These complications led to a mean
expression at the basal lamina of muscle fibres or in age of survival in the late teens. With the recently revised
dermal skin fibroblasts in addition to the severe standards of respiratory and cardiac management,
pathological dystrophic changes (figure 2). Muscle MRI the implementation of multidisciplinary care, and the
shows a distinctive pattern of muscle involvement highly use of corticosteroids,66–68 ambulation is now maintained
suggestive of a collagen 6 involvement (figure 3). The until a mean age of 13–14 years and the mean age of
genetic analysis of COL6A1, COL6A2, and COL6A3 survival has increased to the late twenties.69 Cardiac
completes the diagnostic pathway with the identification death due to progressive dilated cardiomyopathy is now
of either recessive mutations, or de-novo dominant a leading cause of mortality in the older patients.62,70
mutations. Recently a deep-intronic de-novo dominant Recent data suggest a beneficial effect of eplerenone, an
mutation in COL6A1 was identified by transcriptomic anti-mineralocorticoid of the spironolactone group, in
analysis and represents one of the most common single addition to β blocker or angiotensin converting enzyme
mutations in this condition.63,64 inhibitors.71 There is still no consensus on whether
pharmacological cardiac protection therapies should be
Dystroglycanopathies started at a young age (<10 years), as a preventive
This is an extremely heterogeneous group of conditions. measure; data from a limited cohort supports this view,72
Clinically, the variable severity is dependent on the effect while the outcome of larger randomised studies are
of the individual recessive mutations on the level of awaited (EudraCT 2007-005932-10).
dystroglycan glycosylation. The increasing depletion of Unlike the progressive skeletal and cardiac muscle
dystroglycan glycosylation affects, in a hierarchical way, degeneration, brain involvement is not progressive in
skeletal and cardiac muscles first. More severe deficiency Duchenne muscular dystrophy. Although muscle only
of glycosylation leads to CNS involvement, ranging from produces one isoform, in the brain there are multiple
intellectual disability in absence of structural involvement dystrophin isoforms. The site of the DMD gene mutation
and thus suggestive of synaptic involvement, to severe determines how many brain dystrophin isoforms are
cortical dysplasia of the cobblestone type, a form of affected, providing an explanation for the variability in
polymicrogyria with neuronal over migration. Structural brain involvement observed.65,73
eye defects are common in severe cases. The conditions The advent of clinical trials has highlighted the need
with severe structural brain involvement are muscle eye for validated outcome measures and longitudinal, long-
brain disease and Fukuyama congenital muscular term natural history studies. The 6-min walk test
dystrophy, often complicated by epilepsy, and Walker- (6MWT) has been used as a primary outcome measure in
Warburg syndrome (the extreme end of the severe most clinical trials; disease-specific functional measures,
lissencephaly spectrum); all of these conditions have such as the North Star Ambulatory assessment or the
structural eye involvement. The diagnosis of these Performance of Upper Limb test or timed items have
conditions is suggested by the markedly elevated serum also been increasingly used. Natural history studies have
creatine kinase concentration, the dystrophic muscle shown that Duchenne muscular dystrophy progression
biopsy findings, and the reduction of glycosylated is not linear and that there is a huge variability in the
α-dystroglycan at the sarcolemma. The diagnosis needs progression even within 12 months.74–76 The combination
to be confirmed by the analysis of the genes responsible of functional assessments (eg, 6MWT with timed
for this group of conditions (table 1). function tests) and imaging assessment (MRI) further
enhances the possibility to identify patients with different
Duchenne muscular dystrophy disease progression. A more accurate categorisation of
Boys with Duchenne muscular dystrophy are typically trajectories in Duchenne muscular dystrophy progres-
symptomatic after the first years of life, often after mildly sion have recently been achieved using a statistical
delayed acquisition of ambulation. Early complaints are approach that allows the identification of how multiple
frequent falls, inability to run and to climb stairs, and variables (eg, age, timed function tests, height, weight,
difficulty to get up from the floor, requiring the help body-mass index) help in defining the trajectory of
of the hands to push on the knees and provide suffi- progression of affected boys (figure 4).77,78
cient momentum to get upright (Gowers’ manoeuvre).
Delayed acquisition of speech is common (50%). In Limb girdle muscular dystrophies
addition, intellectual disability, autistic spectrum disor- The clinical and genetic heterogeneity of the limb girdle
der, and attention deficit disorder are comorbidities muscular dystrophies, and similar clinical features of
present in about 30% of patients.65 The muscular conditions that are not typically considered within this
dystrophy remains relatively stable until the age of about pathological categorisation complicates their diagnostic
7 years, when more rapid progression becomes apparent, approach.79,80 Common to all forms is an onset after the
www.thelancet.com Vol 394 November 30, 2019 2031
Seminar
next-generation sequencing has been particularly
A
impactful in this situation and these tools are now
800
increasingly used as first-line investigations.49,81.82
A recent European Neuromuscular Centre workshop
suggested a new classification for limb girdle muscle
600
dystrophies (table 2).12
Distance walked (m)
400
Emery–Dreifuss muscular dystrophy
The classical phenotype of Emery–Dreifuss muscular
dystrophy is that of a slowly progressive muscle weakness
200
and wasting, affecting predominantly the biceps and calves.
Contractures affecting the elbows, the Achilles tendons,
and the neck and spine are common. The onset is typically
0
in the early teenage years; an invariable complication is the
5 10 15 20 associated atrial and cardiac system conduction disease
Age (years) and, in a proportion of cases, ventricular arrhythmias and
B
dilated cardiomyopathy that often determine the long-term
800 survival. Standards of care recommend the implantation of
a defibrillator, as pacemakers only have a modest effect on
survival. Compared with the X-linked emerin mutation-
600
Distance walked (m)
related Emery–Dreifuss muscular dystrophy, dominantly
acting LMNA mutation-related Emery–Dreifuss muscular
400 dystrophy overall has earlier onset, in some children
resembling a form of congenital muscular dystrophy
200 (LMNA-related congenital muscular dystrophy). These
children might never acquire the ability to walk, or if they
0 do, they lose this ability in the first decade of life; the
severity of their muscle weakness is paralleled by a more
800
severe respiratory and cardiac progression. Serum
creatinine kinase is typically moderately elevated and
600 muscle MRI shows a typical pattern of selective
Distance walked (m)
involvement. The clinical diagnosis requires genetic
400 confirmation—ie, the analysis of the genes associated with
this phenotype (table 1).
200
Facioscapulohumeral muscular dystrophy
0
The hallmark of facioscapulohumeral muscular dys-
5 10 15 20 5 10 15 20 trophy is the progressive, frequently asymmetrical
Age (years) Age (years) weakness involving the face, scapular muscles, and
proximal limb and peroneal muscles, often with foot
Figure 4: Categorisation of trajectories in Duchenne muscular dystrophy progression using the 6MWT and
multiple variables drop. Marked, progressive winging and typical elevation
Each blue line and dot represents an individual progression trajectory for a patient with Duchenne muscular of the scapulae associated with facial weakness is very
dystrophy. (A) A longitudinal distance walked by a group of boys with Duchenne muscular dystrophy, assessed common. Cardiorespiratory function is usually normal,
using the 6MWT, shows major heterogeneity in disease progression. (B) Different disease trajectories can be
and the progression of weakness is variable, with the
identified taking into account variables other than age to help reduce variability. The black line is the median
progression trajectory. 6MWT=6-min walk test. majority of patients retaining the ability to walk in adult
life. Patients who have onset of symptoms in the first
few years of life are rare (infantile facioscapulohumeral
acquisition of walking (ie, not congenital), a predomi- muscular dystrophy); this subgroup has more severe
nantly proximal pattern of muscle weakness at onset weakness with loss of independent ambulation by
with sparing of facial and extraocular muscles, and the early teens.83 Additional features of facioscapulohu-
dystrophic changes in the muscle biopsy. The assessment meral muscular dystrophy that correlate with clinical
of a panel of relevant proteins on muscle biopsy (figure 2) severity are a retinal vasculopathy with telangiectasia and
and suggestive patterns on muscle imaging (figure 3) microaneurysms (Coats’ disease), and high-frequency
can help guide the diagnostic process. There are sensorineural hearing loss. Serum creatinine kinase
important subtype-specific differences as respiratory concentrations are normal or mildly elevated. The
and cardiac involvement are concerned, highlighting the diagnosis requires the appropriate genetic analysis at the
importance of a specific genetic diagnosis. The advent of chromosomal locus 4q35 or at the FSHD2 locus.
2032 www.thelancet.com Vol 394 November 30, 2019
Seminar
Therapeutic approaches in current clinical trials The approaches focus on either improving structural
Duchenne muscular dystrophy integrity of the muscle fibres by restoring dystrophin
The past decade has seen an exponential increase in production, or on the secondary consequences of dystro-
experimental therapeutic approaches for Duchenne phin deficiency—ie, the inflammatory process, fibrosis,
muscular dystrophy, with two drugs having received muscle regeneration, and muscle mass (table 3). For more on the current trials in
conditional approval in 2016, one in the USA and one in The strategies used for restoring dystrophin expression Duchenne muscular dystrophy
see http://www.treat-nmd.eu/
Europe. There are currently more than 20 active clinical at the sarcolemma range from small molecules or
research/clinical-research/
trials for Duchenne muscular dystrophy, ranging from antisense oligonucleotides, to adeno-associated virus overview-current-trials-dmd/
phase 1 to more advanced studies. (AAV) gene therapy approaches. current-trials/
Mechanism of action Phase Drug route ClinicalTrials.gov number Sponsor
Antisense oligonucleotides
Eteplirsen Morpholino antisense (exon 51 skipping) 2 Intravenous NCT02420379 Sarepta
SRP-4045 Morpholino antisense (exon 45 skipping) 1 Intravenous NCT02530905 Sarepta
SRP-4053 Morpholino antisense (exon 53 skipping) 1/2 Intravenous NCT02310906 Sarepta
DS-5141b 2 ENA antisense (exon 45 skipping) 1/2 Intravenous NCT02667483 Daiichi Sankyo
NS-065/NCNP-01 Morpholino antisense (exon 51 skipping) 2 Intravenous NCT03167255 NS Pharma
SRP-5051 Peptide conjugated morpholino antisense 1 Intravenous NCT03375255 Sarepta
Gene therapy
rAAVrh74.MHCK7 AAV9 gene therapy 1 Intravenous NCT03375164 Nationwide Children’s Hospital
SGT-001 AAV9 gene therapy 1 Intravenous NCT03368742 Solid Bioscience
PF-06939926 AAV9 gene therapy 1 Intravenous NCT03362502 Pfizer
Nonsense readthrough
Ataluren Readthrough strategy of nonsense mutations 2 Oral NCT02819557 PTC Therapeutics
NPC-14 arbekacin sulphate Readthrough strategy of nonsense mutations 2 Oral NCT01918384 Kobe University
Utrophin upregulation
C1100 ezutromid Upregulation of utrophin 2 Oral NCT02858362 Summit
Myostatin inhibition
BMS-986089 Myostatin signalling block 2/3 Subcutaneous NCT03039686 Hoffmann-La Roche
PF-06252616 Myostatin signalling block 2 Intravenous NCT02907619 Pfizer
Corticosteroids
Prednisone vs deflazacort Corticosteroid 3 Oral NCT01603407 University of Rochester
Defazacort Corticosteroid Open label Oral NCT02592941 PTC Therapeutics
Vamorolone Dissociative steroid 2 Oral NCT03038399 ReveraGen BioPharma
Anti-inflammatory
Edasalonexent Inhibition of activated NF-κB 2 Oral NCT02439216 Catabasis Pharmaceuticals
Givinostat Histone deacetylase inhibitor 3 Oral NCT02851797 Italfarmaco
TAS-205 Prostaglandin D synthase inhibitor 2 Oral NCT02752048 Taiho Pharmaceutical
Anti-fibrotic
Pamrevlumab (FG-3019) Tissue growth factor MAB 2 Intravenous NCT02606136 FibroGen
Reduction of muscle damage
Epicatechin Antioxidant 1/2 Oral NCT02964377 Cardero Therapeutics
Tamoxifen Reduced muscle damage 3 Oral NCT03354039 University Hospital, Basel
Idebenone Reduction of mitochondrial damage 3 Oral NCT02814019 Santhera
Sunphenon epigallocatechin-gallate Protection of muscle damage 3 Oral NCT01183767 Charité University
Rimeporide Sodium-hydron exchanger 1/2 Oral NCT02710591 Esperare
Improved mitochondrial function
Idebenone Increased mitochondrial function 3 Oral NCT02814019 Santhera
Cardiac protection
Spironolactone vs eplerenone Preservation in cardiopulmonary function 3 Oral NCT02354352 Ohio State University
Epicatechin Preservation of cardiac function 2 Oral NCT02964377 Cardero Therapeutics
Nebivolol β blocker 2 Oral NCT01648634 Assistance Publique–Hôpitaux de Paris
Data compiled from ClinicalTrials.gov. AAV=adeno-associated virus. MAB=monoclonal antibodies.
Table 3: Interventional clinical trials in Duchenne muscular dystrophy as of January, 2018
www.thelancet.com Vol 394 November 30, 2019 2033
Seminar
Another therapeutic approach is the targeting of the USA despite criticisms due to the small patient
nonsense mutations. Ataluren, an orally bioavailable population treated, the small amount of dystrophin
small molecule, induces readthrough of nonsense produced,92 and the absence of a placebo group. Recent
mutations at the ribosome and partially restores dys- additional data for the long-term preservation of
trophin production. Two randomised, double-blind, respiratory function in the boys with Duchenne muscular
placebo-controlled trials showed a trend in therapeutic dystrophy studied over the course of 5 years were pub-
efficacy as measured by changes in the 6MWT, although lished.93 Currently, confirmatory studies (NCT02310906;
both studies did not achieve the 48-week primary NCT02255552; NCT03218995; NCT02500381) are
endpoint.84 The study design might have had a role on targeting exon 51, but also exons 45 and 53 (table 3).
this outcome, as both studies recruited a high proportion Next-generation antisense oligonucleotides are also
of boys with Duchenne muscular dystrophy in the stable now in phase 1 studies: a peptide-conjugated morpho-
phase, reducing the possibility to appreciate a treatment lino antisense oligonucleotide for improved muscle
effect. When considering only the boys in ambulatory targeting; and a novel stereochemical modification of
decline (a prespecified endpoint in the phase 3 study), a the 2’OMe backbone, which is expected to improve
statistical difference between the treated children and the efficacy, should result in reduced dosage and adverse
placebo group was detected.85 On the basis of this finding events.94,95
and a favourable safety profile, the European Medicines AAV gene therapy is also being considered as a
Agency granted a conditional approval, while the com- therapeutic option for Duchenne muscular dystrophy.
pany is running further trials. The large size of the DMD gene precludes packaging of
Antisense oligonucleotides for out-of-frame deletions the full cDNA in AAV vectors. However, considerably
is an alternative treatment strategy. This strategy uses shortened microdystrophin versions, originally inspired
antisense oligonucleotides, which need to be admin- by some patients with large intragenic deletions and yet
istered systemically each week, to manipulate the pre- a Becker muscular dystrophy phenotype, have been
mRNA splicing in patients with eligible out-of-frame developed that can be accommodated in AAV vectors.
deletions and generate an in-frame message by removing As viral delivery to muscle is associated with an immune
For more on frame restoring one exon adjacent to the deletion breakpoint (ie, frame response to the AAV that precludes repeated adminis-
exon skipping see https://www. restoring exon skipping. This approach is mutation trations with the same serotype, it is essential to develop
musculardystrophyuk.org/
progress-in-research/
specific and facilitated by clustering of deletions in efficient strategies with a realistic perspective of
background-information/what- specific hotspots: skipping exon 51 for example is producing a therapeutic benefit for the patients to mini-
is-exon-skipping-and-how-does- applicable to about 13% of all the boys with deletions. mise the need for a repeat treatment. Recent preclinical
it-work/ Two different antisense oligonucleotide chemical modi- studies have shown the potential of AAV8 and AAV9 to
fications, the morpholino and the 2ʹOMe have been used target muscles, with histological and clinical improve-
in trials of Duchenne muscular dystrophy. Both antisense ments.93,96–101 Several academic groups and industrial
oligonucleotides induce frame-restored dystrophin pro- partners have initiated phase 1 clinical trials, in which
duction when administered following a single intra- escalating doses of AAV9 and AAVrh74 are being
muscular injection to boys with Duchenne muscular administered systemically to boys with Duchenne
dystrophy.86,87 In two subsequent phase 2 studies, the muscular dystrophy.
2ʹOMe antisense oligonucleotide drisapersen met the
clinical endpoint.84 However, a larger phase 3 study did Dealing with secondary consequences of dystrophin
not show a clinical benefit. The inclusion criteria might deficiency
have had a role; a recent post-hoc analysis suggested Numerous clinical phase 1–3 trials are underway to
a significant improvement in 6MWT in favour of assess safety and efficacy of targeting the NF-κB
drisapersen in boys in moderate decline compared inflammatory pathway (Catabasis Pharmaceuticals): a
with patients receiving the placebo.88 Nevertheless, the dissociative steroidal drug, which aims to retain the
inadequate clinical efficacy combined with the un- corticosteroid efficacy but reduce their chronic side-effect
favourable safety profile led BioMarin to abandon the profile (ReveraGen BioPharma); downregulation of the
development of the 2ʹOMe antisense oligonucleotide myostatin pathway, which in animal models induces
platform for Duchenne muscular dystrophy. improved regeneration and increases muscle mass
The morpholino antisense oligonucleotide designed (Pfizer; Roche); compounds with an effect on fibrosis
to skip exon 51 (eteplirsen) also induced dystrophin and muscle regeneration (Italfarmaco); or improved
restoration in a dose escalation intravenous phase 2 mitochondrial bioenergetics (Santhera). Table 3 provides
study.89,90 Subsequent studies confirmed the production a list of the ongoing clinical trials of Duchenne muscular
of dystrophin in most of the treated patients,91 and a dystrophy.
divergence of the clinical course between the treated
children and a concomitant natural history study based COL6-related congenital muscular dystrophy
on the 6MWT.92 These data led the US Food and Drug In this condition, myofibre degeneration is at least
Administration to conditionally approve eteplirsen in partially due to mitochondrial mediated muscle fibre
2034 www.thelancet.com Vol 394 November 30, 2019
Seminar
apoptosis, driven by inappropriate opening of the explored preclinically includes upregulation of the glyco-
mitochondrial permeability transition pore.102,103 Pharma- syltransferase LARGE, involved in adding an important
cological interference with this mechanism can be glycoepitope that confers the binding activity to laminin.
achieved using cyclosporine A, exploiting its inhibition This approach might be able to compensate for a variety
of cyclophilin D.104 A small uncontrolled trial of cyclo- of defects more upstream.110 However, there might be
sporine A in patients with COL6-related muscular dystro- risks in upregulating this glycosyltransferase too much
phy apparently improved mitochondrial permeability that still need to be explored.
transition pore dysfunction on pathology; however, Gene transfer strategies are also being explored for the
the study was not designed to detect functional sarcoglycanopathies as well as for calpainopathy and
improvement.105 Other studies have suggested that the anoctaminopathy in relevant preclinical models. Phase 1
muscle autophagic machinery is underperforming in studies of local intramuscular delivery of γ, α and β
COL6-related muscular dystrophy, causing backed up sarcoglycans have been done in the corresponding limb
clearance of the abnormal mitochondria. Autophagy can girdle muscular dystrophy variants. The next stage of
be induced by protein restriction, leading to a small systemic delivery of some of these transgenes has recently
uncontrolled trial of protein restriction in patients with been initiated with the delivery of β-sarcoglycan using the
COL6-related muscular dystrophy. Although it was pos- same AAVrh74 used for dystrophin (NCT03652259).
sible to suggest an induction of autophagy in the patients, Pharmacological approaches aimed at intervening in
the study design did not allow the detection of clinical secondary disease driving processes are also being pur-
efficacy.106,107 The anti-apoptotic compound omigapil has sued preclinically in dysferlinopathy and calpainopathy.
recently been studied in a phase 1 pharmacokinetic study These approaches include the upregulation or even
at the National Institutes of Health in children with both the systemic administration of proteins that collaborate
COL6-related and LAMA2-related congenital muscular with dysferlin in the resealing process, such as
dystrophy. mitsugumin 53,111–113 and the identification of the targets
responsible for progressive muscle damage in
LAMA2-related congenital muscular dystrophy calpainopathy.
Preclinical work has identified inappropriate premature
apoptosis of myofibres as one potential disease driver. Emery–Dreifuss muscular dystrophy disorders
Omigapil is a glyceraldehyde 3-phosphate dehydroge- Genetic therapeutic approaches for the Emery–Dreifuss
nase (GAPDH) interactor and interferes with the muscular dystrophy disorders are only at the preclinical
GAPDH/Siah1-mediated apoptosis pathway. Preclinical stage. Gene replacement is conceivable in emerin defi-
studies in mouse models of the disease have suggested ciency since the gene product can be packaged into AAV.
disease modifying potential for this compound. A phase 1 However the same therapeutic approach would not be
pharmacokinetic study of omigapil in children with appropriate for LMNA mutations, where the mutations
LAMA2-related congenital muscular dystrophy as well as act in a dominant negative way, but haploinsufficiency
COL6-related muscular dystrophy has recently been also leads to disease (cardiomyopathy), making even a
done. Pharmacological approaches to other potential mutation-specific silencing approach a challenge.
mechanisms for this disease (overactive autophagy and
underactive proteasome, TGFβ-mediated fibrosis,108 and Conclusions
inflammation) have been studied preclinically but not yet In the past few years, the genetic diversity of muscular
in clinical trials. Functional replacement of laminin α-2 dystrophies has been further elucidated, mainly because
(which is too large for AAV-mediated delivery) has of the powerful genetic diagnostic tools, which now—
been achieved preclinically using two ingenious linker along with excellent clinical sorting and improvement on
molecules in combination, mini-agrin and mini- muscle pathology and imaging—achieves individual
nidogen,109 which could be delivered using AAV. genetic diagnosis in the majority of patients.
Therapeutic developments have also seen a
Limb girdle muscular dystrophies substantial expansion of efforts, initially with mutation
The translational research in these conditions is mostly and gene-directed approaches, which led to drugs
focused on preclinical models. In the dystroglyca- targeting specific Duchenne muscular dystrophy
nopathies, gene transfer approaches are being explored mutations being commercially available. The second-
since these conditions are based on loss of function generation drugs of some of these approaches are now
and most of the cDNAs are small enough to be packaged in early clinical trials. At the same time, approaches
into AAVs. Relevant animal models, most importantly that are potentially applicable to patients irrespective of
the more common FKRP, are being studied. For the the mutations are also being developed. Over the past
subtypes that are also involved in the CNS, it will be few years, increasing confidence in AAV gene therapy
important to target the brain as well, although the effect is leading to multi-partner efforts to take these viral
of postnatal correction of the primary defect in the brain vectors to clinical trials for the treatment of Duchenne
remains to be explored. Another approach that has been muscular dystrophy. These efforts, if effective, will pave
www.thelancet.com Vol 394 November 30, 2019 2035
Seminar
the way for other forms of dystrophies in which this 8 Muntoni F, Torelli S, Wells DJ, Brown SC. Muscular dystrophies
approach is feasible. due to glycosylation defects: diagnosis and therapeutic strategies.
Curr Opin Neurol 2010; 24: 437–42.
Although mechanisms and pathways might be disease 9 Nigro V, Aurino S, Piluso G. Limb girdle muscular dystrophies:
specific, in some instances they might also be valid update on genetic diagnosis and therapeutic approaches.
across different diseases with opportunities for use Curr Opin Neurol 2011; 24: 429–36.
10 Kaplan JC, Hamroun D. Corrigendum to “The 2016 version of the
across entities. It is also feasible that in the future we will gene table of monogenic neuromuscular disorders (nuclear
see the development of combinatorial therapies for a genome)”. Neuromuscul Disord 2016; 26: 330.
number of these approaches. 11 Kaplan JC, Hamroun D. The 2016 version of the gene table of
monogenic neuromuscular disorders (nuclear genome).
Although there is tangible excitement in this field for Neuromuscul Disord 2015; 25: 991–1020.
these efforts, it is nevertheless essential not to lose sight 12 Straub V, Murphy A, Udd B, LGMD workshop study group.
of the fact that the ultimate cure for muscular dystro- 229th ENMC international workshop: limb girdle muscular
phies will be very challenging, these being degenerative dystrophies—nomenclature and reformed classification, Naarden,
the Netherlands, 17–19 March 2017. Neuromuscul Disord 2018;
disorders of muscle. Substantial obstacles to overcome 28: 702–10.
are, in congenital muscular dystrophies, the timing of 13 Urciuolo A, Quarta M, Morbidoni V, et al. Collagen VI regulates
onset of pathology; in Duchenne muscular dystrophy satellite cell self-renewal and muscle regeneration. Nat Commun
2013; 4: 1964.
and limb girdle muscular dystrophies, the abundance of 14 Camacho Vanegas O, Bertini E, Zhang RZ, et al. Ullrich scleroatonic
the muscle tissue to target, together with the fact that muscular dystrophy is caused by recessive mutations in collagen
symptomatic patients already have lost a considerable type VI. Proc Natl Acad Sci USA 2001; 98: 7516–21.
15 Demir E, Sabatelli P, Allamand V, et al. Mutations in COL6A3 cause
amount of muscle tissue that is not replaceable with severe and mild phenotypes of Ullrich congenital muscular
current technology. dystrophy. Am J Hum Genet 2002; 70: 1446–58.
Therefore implementation of optimal medical man- 16 Baker NL, Morgelin M, Peat R, et al. Dominant collagen VI
mutations are a common cause of Ullrich congenital muscular
agement on the basis of standards of care remains as dystrophy. Hum Mol Genet 2005; 14: 279–93.
important as ever, because management can still be 17 Helbling-Leclerc A, Zhang X, Topaloglu H, et al. Mutations in the
improved, remains often inconsistent between centres laminin alpha 2-chain gene (LAMA2) cause merosin-deficient
and countries, and needs to be optimal as a baseline on congenital muscular dystrophy. Nat Genet 1995; 11: 216–18.
18 Kubota A, Ishiura H, Mitsui J, et al. A homozygous LAMA2 mutation
which to test additional experimental approaches. of c.818G>A caused partial merosin deficiency in a Japanese patient.
Contributors Intern Med 2018; 57: 877–82.
FM wrote the first draft, which was reviewed and completed by EM and 19 Han R. Muscle membrane repair and inflammatory attack in
CGB. All authors reviewed the literature, contributed to the writing of dysferlinopathy. Skelet Muscle 2011; 1: 10.
subsequent drafts, and reviewed the final manuscript. 20 Sharma A, Yu C, Leung C, et al. A new role for the muscle repair
protein dysferlin in endothelial cell adhesion and angiogenesis.
Declaration of interests Arterioscler Thromb Vasc Biol 2010; 30: 2196–204.
EM reports receiving grants and personal fees from Sarepta and PTC; 21 Han R, Campbell KP. Dysferlin and muscle membrane repair.
grants from EU FP7 (SKIP-nmd grant); and personal fees from Pfizer Curr Opin Cell Biol 2007; 19: 409–16.
and Roche, during the conduct of this Seminar. CGB reports receiving 22 Bolduc V, Marlow G, Boycott KM, et al. Recessive mutations in the
institutional clinical trial support from Audentes Therapeutics; putative calcium-activated chloride channel anoctamin 5 cause
and non-compensated advisory activity from SOLID, Abeona, and proximal LGMD2L and distal MMD3 muscular dystrophies.
Sarepta, during the conduct of this Seminar. FM reports receiving grants Am J Hum Genet 2010; 86: 213–21.
and personal fees from Sarepta, Pfizer, and PTC; grants from EU FP7 23 Hicks D, Sarkozy A, Muelas N, et al. A founder mutation in
(SKIP-nmd grant) and Wave; and personal fees from Roche, during the Anoctamin 5 is a major cause of limb-girdle muscular dystrophy.
conduct of this Seminar. Brain 2011; 134: 171–82.
24 Griffin DA, Johnson RW, Whitlock JM, et al. Defective membrane
Acknowledgments
fusion and repair in anoctamin-5-deficient muscular dystrophy.
We thank the patients and their families for the continuous inspiration Hum Mol Genet 2016; 25: 1900–11.
they provide us. We also thank Caroline A Sewry and Rahul Phadke 25 de Haan W. Lipodystrophy and muscular dystrophy caused by PTRF
(Dubowitz Neuromuscular Centre, Neuropathology Department, Institute mutations. Clin Genet 2010; 77: 436–37.
of Neurology, London, UK) for providing figure 2 of this manuscript and 26 Hayashi YK, Matsuda C, Ogawa M, et al. Human PTRF mutations
Susan J Ward, James Edward Signorovitch, and the collaborative cause secondary deficiency of caveolins resulting in muscular
Trajectory Analysis Project for providing figure 4 of this manuscript. dystrophy with generalized lipodystrophy. J Clin Invest 2009;
References 119: 2623–33.
1 Emery AE. The muscular dystrophies. Lancet 2002; 359: 687–95. 27 Muntoni F, Brockington M, Blake DJ, Torelli S, Brown SC.
2 Mercuri E, Muntoni F. Muscular dystrophies. Lancet 2013; Defective glycosylation in muscular dystrophy. Lancet 2002;
381: 845–60. 360: 1419–21.
3 Guglieri M, Straub V, Bushby K, Lochmuller H. Limb-girdle 28 Taniguchi-Ikeda M, Morioka I, Iijima K, Toda T. Mechanistic
muscular dystrophies. Curr Opin Neurol 2008; 21: 576–84. aspects of the formation of α-dystroglycan and therapeutic research
for the treatment of α-dystroglycanopathy: a review. Mol Aspects Med
4 Mercuri E, Muntoni F. The ever-expanding spectrum of congenital 2016; 51: 115–24.
muscular dystrophies. Ann Neurol 2012; 72: 9–17.
29 Godfrey C, Clement E, Mein R, et al. Refining genotype phenotype
5 Mendell JR, Rodino-Klapac L, Sahenk Z, et al. Gene therapy for correlations in muscular dystrophies with defective glycosylation of
muscular dystrophy: lessons learned and path forward. Neurosci Lett dystroglycan. Brain 2007; 130: 2725–35.
2012; 527: 90–99.
30 Godfrey C, Foley AR, Clement E, Muntoni F. Dystroglycanopathies:
6 Sahenk Z, Mendell JR. The muscular dystrophies: distinct pathogenic coming into focus. Curr Opin Genet Dev 2011; 21: 278–85.
mechanisms invite novel therapeutic approaches. Curr Rheumatol Rep
2011; 13: 199–207. 31 Mercuri E, Messina S, Bruno C, et al. Congenital muscular
dystrophies with defective glycosylation of dystroglycan: a population
7 Goyenvalle A, Seto JT, Davies KE, Chamberlain J. Therapeutic study. Neurology 2009; 72: 1802–09.
approaches to muscular dystrophy. Hum Mol Genet 2011; 20: R69–78.
2036 www.thelancet.com Vol 394 November 30, 2019
Seminar
32 Jimenez-Mallebrera C, Torelli S, Feng L, et al. A comparative study 55 Nadeau A, Kinali M, Main M, et al. Natural history of Ullrich
of α-dystroglycan glycosylation in dystroglycanopathies suggests congenital muscular dystrophy. Neurology 2009; 73: 25–31.
that the hypoglycosylation of α-dystroglycan does not consistently 56 Scoto M, Cirak S, Mein R, et al. SEPN1-related myopathies:
correlate with clinical severity. Brain Pathol 2009; 19: 596–611. clinical course in a large cohort of patients. Neurology 2011;
33 Bonne G, Di Barletta MR, Varnous S, et al. Mutations in the gene 76: 2073–78.
encoding lamin A/C cause autosomal dominant Emery–Dreifuss 57 Geranmayeh F, Clement E, Feng LH, et al. Genotype-phenotype
muscular dystrophy. Nat Genet 1999; 21: 285–88. correlation in a large population of muscular dystrophy patients
34 Bonne G, Mercuri E, Muchir A, et al. Clinical and molecular genetic with LAMA2 mutations. Neuromuscul Disord 2010; 20: 241–50.
spectrum of autosomal dominant Emery–Dreifuss muscular 58 Bonnemann CG, Wang CH, Quijano-Roy S, et al. Diagnostic
dystrophy due to mutations of the lamin A/C gene. Ann Neurol approach to the congenital muscular dystrophies. Neuromuscul Disord
2000; 48: 170–80. 2014; 24: 289–311.
35 Foley AR, Hu Y, Zou Y, et al. Large genomic deletions: a novel cause 59 Kang PB, Morrison L, Iannaccone ST, et al. Evidence-based guideline
of Ullrich congenital muscular dystrophy. Ann Neurol 2011; summary: evaluation, diagnosis, and management of congenital
69: 206–11. muscular dystrophy: report of the Guideline Development
36 Bertrand AT, Chikhaoui K, Yaou RB, Bonne G. Clinical and genetic Subcommittee of the American Academy of Neurology and the
heterogeneity in laminopathies. Biochem Soc Trans 2010; Practice Issues Review Panel of the American Association of
39: 1687–92. Neuromuscular and Electrodiagnostic Medicine. Neurology 2015;
37 Udd B. Distal myopathies—new genetic entities expand diagnostic 84: 1369–78.
challenge. Neuromuscul Disord 2012; 22: 5–12. 60 Narayanaswami P, Weiss M, Selcen D, et al. Evidence-based guideline
38 Udd B. Distal muscular dystrophies. Handb Clin Neurol 2011; summary: diagnosis and treatment of limb-girdle and distal
101: 239–62. dystrophies: report of the Guideline Development Subcommittee of
39 Yoskovitz G, Peled Y, Gramlich M, et al. A novel titin mutation in the American Academy of Neurology and the Practice Issues Review
adult-onset familial dilated cardiomyopathy. Am J Cardiol 2012; Panel of the American Association of Neuromuscular and
109: 1644–50. Electrodiagnostic Medicine. Neurology 2014; 83: 1453–63.
40 Bogershausen N, Shahrzad N, Chong JX, et al. Recessive TRAPPC11 61 Foley AR, Quijano-Roy S, Collins J, et al. Natural history of
mutations cause a disease spectrum of limb girdle muscular pulmonary function in collagen VI-related myopathies. Brain 2013;
dystrophy and myopathy with movement disorder and intellectual 136: 3625–33.
disability. Am J Hum Genet 2013; 93: 181–90. 62 Yonekawa T, Nishino I. Ullrich congenital muscular dystrophy:
41 Liang WC, Zhu W, Mitsuhashi S, et al. Congenital muscular clinicopathological features, natural history and pathomechanism(s).
dystrophy with fatty liver and infantile-onset cataract caused by J Neurol Neurosurg Psychiatry 2015; 86: 280–87.
TRAPPC11 mutations: broadening of the phenotype. Skelet Muscle 63 Cummings BB, Marshall JL, Tukiainen T, et al. Improving genetic
2015; 5: 29. diagnosis in mendelian disease with transcriptome sequencing.
42 Schindler RF, Scotton C, Zhang J, et al. POPDC1(S201F) causes Sci Transl Med 2017; 9: eaal5209.
muscular dystrophy and arrhythmia by affecting protein trafficking. 64 Bolduc V, Foley AR, Solomon-Degefa H, et al. A recurrent
J Clin Invest 2016; 126: 239–53. COL6A1 pseudoexon insertion causes muscular dystrophy and is
43 Lemmers RJ, van der Vliet PJ, Klooster R, et al. A unifying genetic effectively targeted by splice-correction therapies. JCI Insight 2019;
model for facioscapulohumeral muscular dystrophy. Science 2010; 4: 124403.
329: 1650–53. 65 Ricotti V, Mandy WP, Scoto M, et al. Neurodevelopmental, emotional,
44 Wallace LM, Liu J, Domire JS, et al. RNA interference inhibits and behavioural problems in Duchenne muscular dystrophy in
DUX4-induced muscle toxicity in vivo: implications for a targeted relation to underlying dystrophin gene mutations.
FSHD therapy. Mol Ther 2012; 20: 1417–23. Dev Med Child Neurol 2016; 58: 77–84.
45 Ellis JA, Vroom E, Muntoni F. 195th ENMC International 66 Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and
Workshop: newborn screening for Duchenne muscular dystrophy management of Duchenne muscular dystrophy, part 2: respiratory,
14–16th December, 2012, Naarden, the Netherlands. cardiac, bone health, and orthopaedic management. Lancet Neurol
Neuromuscul Disord 2013; 23: 682–89. 2018; 17: 347–61.
46 Norwood FL, Harling C, Chinnery PF, Eagle M, Bushby K, 67 Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and
Straub V. Prevalence of genetic muscle disease in northern management of Duchenne muscular dystrophy, part 1: diagnosis,
England: in-depth analysis of a muscle clinic population. Brain and neuromuscular, rehabilitation, endocrine, and gastrointestinal
2009; 132: 3175–86. and nutritional management. Lancet Neurol 2018; 17: 251–67.
47 Graziano A, Bianco F, D’Amico A, et al. Prevalence of congenital 68 Birnkrant DJ, Bushby K, Bann CM, et al. Diagnosis and
muscular dystrophy in Italy: a population study. Neurology 2015; management of Duchenne muscular dystrophy, part 3: primary care,
84: 904–11. emergency management, psychosocial care, and transitions of care
across the lifespan. Lancet Neurol 2018; 17: 445–55.
48 Sframeli M, Sarkozy A, Bertoli M, et al. Congenital muscular
dystrophies in the UK population: clinical and molecular spectrum 69 Passamano L, Taglia A, Palladino A, et al. Improvement of survival
of a large cohort diagnosed over a 12-year period. Neuromuscul Disord in Duchenne muscular dystrophy: retrospective analysis of
2017; 27: 793–803. 835 patients. Acta Myol 2012; 31: 121–25.
49 O’Grady GL, Lek M, Lamande SR, et al. Diagnosis and etiology of 70 Cheeran D, Khan S, Khera R, et al. Predictors of death in adults
congenital muscular dystrophy: we are halfway there. Ann Neurol with Duchenne muscular dystrophy-associated cardiomyopathy.
2016; 80: 101–11. J Am Heart Assoc 2017; 6: e006340.
50 Magri F, Nigro V, Angelini C, et al. The Italian limb girdle muscular 71 Raman SV, Hor KN, Mazur W, et al. Eplerenone for early
dystrophy registry: relative frequency, clinical features, and cardiomyopathy in Duchenne muscular dystrophy: a randomised,
differential diagnosis. Muscle Nerve 2017; 55: 55–68. double-blind, placebo-controlled trial. Lancet Neurol 2015; 14: 153–61.
51 Nallamilli BRR, Chakravorty S, Kesari A, et al. Genetic landscape 72 Duboc D, Meune C, Pierre B, et al. Perindopril preventive treatment
and novel disease mechanisms from a large LGMD cohort of on mortality in Duchenne muscular dystrophy: 10 years’ follow-up.
4656 patients. Ann Clin Transl Neurol 2018; 5: 1574–87. Am Heart J 2007; 154: 596–602.
52 Stensland E, Lindal S, Jonsrud C, et al. Prevalence, mutation 73 Battini R, Chieffo D, Bulgheroni S, et al. Cognitive profile in
spectrum and phenotypic variability in Norwegian patients with limb Duchenne muscular dystrophy boys without intellectual disability:
girdle muscular dystrophy 2I. Neuromuscul Disord 2011; 21: 41–46. the role of executive functions. Neuromuscul Disord 2018;
28: 122–28.
53 Tawil R, van der Maarel S, Padberg GW, van Engelen BG. 171st ENMC
international workshop: standards of care and management of 74 Henricson E, Abresch R, Han JJ, et al. The 6-Minute Walk Test and
facioscapulohumeral muscular dystrophy. Neuromuscul Disord 2010; person-reported outcomes in boys with Duchenne muscular
20: 471–75. dystrophy and typically developing controls: longitudinal
comparisons and clinically-meaningful changes over one year.
54 Tawil R, van der Maarel SM. Facioscapulohumeral muscular
PLoS Curr 2013; 5: 5.
dystrophy. Muscle Nerve 2006; 34: 1–15.
www.thelancet.com Vol 394 November 30, 2019 2037
Seminar
75 Goemans N, Klingels K, van den Hauwe M, et al. Six-Minute Walk 94 Gait MJ, Arzumanov AA, McClorey G, et al. Cell-penetrating
Test: reference values and prediction equation in healthy boys peptide conjugates of steric blocking oligonucleotides as
aged 5 to 12 years. PLoS One 2013; 8: e84120. therapeutics for neuromuscular diseases from a historical
76 Pane M, Mazzone ES, Sivo S, et al. Long term natural history perspective to current prospects of treatment. Nucleic Acid Ther
data in ambulant boys with Duchenne muscular dystrophy: 2019; 29: 1–12.
36-month changes. PLoS One 2014; 9: e108205. 95 Iwamoto N, Butler DCD, Svrzikapa N, et al. Control of
77 Mercuri E, Signorovitch JE, Swallow E, et al. Categorizing natural phosphorothioate stereochemistry substantially increases the
history trajectories of ambulatory function measured by the efficacy of antisense oligonucleotides. Nat Biotechnol 2017;
6-minute walk distance in patients with Duchenne muscular 35: 845–51.
dystrophy. Neuromuscul Disord 2016; 26: 576–83. 96 Wang JZ, Wu P, Shi ZM, Xu YL, Liu ZJ. The AAV-mediated and
78 Goemans N, Vanden Hauwe M, Signorovitch J, Swallow E, RNA-guided CRISPR/Cas9 system for gene therapy of DMD and
Song J, Collaborative Trajectory Analysis Project (cTAP). BMD. Brain Dev 2017; 39: 547–56.
Individualized prediction of changes in 6-minute walk distance for 97 Heller KN, Mendell JT, Mendell JR, Rodino-Klapac LR.
patients with Duchenne muscular dystrophy. PLoS One 2016; MicroRNA-29 overexpression by adeno-associated virus suppresses
11: e0164684. fibrosis and restores muscle function in combination with
79 Murphy AP, Straub V. The classification, natural history and micro-dystrophin. JCI Insight 2017; 2: 93309.
treatment of the limb girdle muscular dystrophies. J Neuromuscul Dis 98 Chamberlain JR, Chamberlain JS. Progress toward gene therapy for
2015; 2: S7–19. Duchenne muscular dystrophy. Mol Ther 2017; 25: 1125–31.
80 Fayssoil A, Ogna A, Chaffaut C, et al. Natural history of cardiac and 99 Ramos J, Chamberlain JS. Gene therapy for Duchenne muscular
respiratory involvement, prognosis and predictive factors for dystrophy. Expert Opin Orphan Drugs 2015; 3: 1255–66.
long-term survival in adult patients with limb girdle muscular 100 Nance ME, Duan D. Perspective on adeno-associated virus capsid
dystrophies type 2C and 2D. PLoS One 2016; 11: e0153095. modification for Duchenne muscular dystrophy gene therapy.
81 Savarese M, Di Fruscio G, Tasca G, et al. Next generation Hum Gene Ther 2015; 26: 786–800.
sequencing on patients with LGMD and nonspecific myopathies: 101 Le Guiner C, Servais L, Montus M, Larcher T. Long-term
findings associated with ANO5 mutations. Neuromuscul Disord microdystrophin gene therapy is effective in a canine model of
2015; 25: 533–41. Duchenne muscular dystrophy. Nat Commun 2017; 8: 16105.
82 Savarese M, Di Fruscio G, Torella A, et al. The genetic basis of 102 Angelin A, Tiepolo T, Sabatelli P, et al. Mitochondrial dysfunction
undiagnosed muscular dystrophies and myopathies: results from in the pathogenesis of Ullrich congenital muscular dystrophy and
504 patients. Neurology 2016; 87: 71–76. prospective therapy with cyclosporins. Proc Natl Acad Sci USA 2007;
83 Goselink RJ, Schreuder TH, Mul K, et al. Facioscapulohumeral 104: 991–96.
dystrophy in children: design of a prospective, observational study 103 Irwin WA, Bergamin N, Sabatelli P, et al. Mitochondrial dysfunction
on natural history, predictors and clinical impact (iFocus FSHD). and apoptosis in myopathic mice with collagen VI deficiency.
BMC Neurol 2016; 16: 138. Nat Genet 2003; 35: 367–71.
84 Voit T, Topaloglu H, Straub V, et al. Safety and efficacy of 104 Tiepolo T, Angelin A, Palma E, et al. The cyclophilin inhibitor
drisapersen for the treatment of Duchenne muscular dystrophy Debio 025 normalizes mitochondrial function, muscle apoptosis
(DEMAND II): an exploratory, randomised, placebo-controlled and ultrastructural defects in Col6a1-/- myopathic mice.
phase 2 study. Lancet Neurol 2014; 13: 987–96. Br J Pharmacol 2009; 157: 1045–52.
85 Bushby K, Finkel R, Wong B, et al. Ataluren treatment of patients 105 Merlini L, Angelin A, Tiepolo T, et al. Cyclosporin A corrects
with nonsense mutation dystrophinopathy. Muscle Nerve 2014; mitochondrial dysfunction and muscle apoptosis in patients with
50: 477–87. collagen VI myopathies. Proc Natl Acad Sci USA 2008;
86 Kinali M, Arechavala-Gomeza V, Feng L, et al. Local restoration of 105: 5225–29.
dystrophin expression with the morpholino oligomer AVI-4658 in 106 Grumati P, Coletto L, Sabatelli P, et al. Autophagy is defective in
Duchenne muscular dystrophy: a single-blind, placebo-controlled, collagen VI muscular dystrophies, and its reactivation rescues
dose-escalation, proof-of-concept study. Lancet Neurol 2009; 8: 918–28. myofiber degeneration. Nat Med 2010; 16: 1313–20.
87 van Deutekom JC, Janson AA, Ginjaar IB, et al. Local dystrophin 107 Grumati P, Coletto L, Sandri M, Bonaldo P. Autophagy induction
restoration with antisense oligonucleotide PRO051. N Engl J Med rescues muscular dystrophy. Autophagy 2011; 7: 426–28.
2007; 357: 2677–86. 108 Erb M, Meinen S, Barzaghi P, et al. Omigapil ameliorates the
88 Goemans NM, Tulinius M, van den Hauwe M, et al. Long-term pathology of muscle dystrophy caused by laminin-alpha2 deficiency.
efficacy, safety, and pharmacokinetics of drisapersen in Duchenne J Pharmacol Exp Ther 2009; 331: 787–95.
muscular dystrophy: results from an open-label extension study. 109 Reinhard JR, Lin S, McKee KK, et al. Linker proteins restore
PLoS One 2016; 11: e0161955. basement membrane and correct LAMA2-related muscular
89 Cirak S, Feng L, Anthony K, et al. Restoration of the dystrophin- dystrophy in mice. Sci Transl Med 2017; 9: eaal4649.
associated glycoprotein complex after exon skipping therapy in 110 Brockington M, Torelli S, Sharp PS, et al. Transgenic overexpression
Duchenne muscular dystrophy. Mol Ther 2012; 20: 462–67. of LARGE induces α-dystroglycan hyperglycosylation in skeletal and
90 Anthony K, Feng L, Arechavala-Gomeza V, et al. Exon skipping cardiac muscle. PLoS One 2010; 5: e14434.
quantification by quantitative reverse-transcription polymerase 111 Weisleder N, Takizawa N, Lin P, et al. Recombinant MG53 protein
chain reaction in Duchenne muscular dystrophy patients treated modulates therapeutic cell membrane repair in treatment of
with the antisense oligomer eteplirsen. Hum Gene Ther Methods muscular dystrophy. Sci Transl Med 2012; 4: 139ra85.
2012; 23: 336–45.
112 Weisleder N, Takeshima H, Ma J. Mitsugumin 53 (MG53) facilitates
91 Mendell JR, Rodino-Klapac LR, Sahenk Z, et al. Eteplirsen for the vesicle trafficking in striated muscle to contribute to cell membrane
treatment of Duchenne muscular dystrophy. Ann Neurol 2013; repair. Commun Integr Biol 2009; 2: 225–26.
74: 637–47.
113 Cai C, Weisleder N, Ko JK, et al. Membrane repair defects in
92 Mendell JR, Goemans N, Lowes LP, et al. Longitudinal effect of muscular dystrophy are linked to altered interaction between
eteplirsen versus historical control on ambulation in Duchenne MG53, caveolin-3, and dysferlin. J Biol Chem 2009; 284: 15894–902.
muscular dystrophy. Ann Neurol 2016; 79: 257–71.
93 Kodippili K, Hakim CH, Pan X, et al. Dual AAV gene therapy for © 2019 Elsevier Ltd. All rights reserved.
Duchenne muscular dystrophy with a 7-kb mini-dystrophin gene in
the canine model. Hum Gene Ther 2018; 29: 299–311.
2038 www.thelancet.com Vol 394 November 30, 2019
You might also like
- Mental Health Awareness and PFA Training ReportDocument4 pagesMental Health Awareness and PFA Training ReportSHEILA MAE PERTIMOS100% (14)
- Patrick Meyer Reliability Understanding Statistics 2010Document160 pagesPatrick Meyer Reliability Understanding Statistics 2010jcgueinj100% (1)
- Past Simple Past ContinuousDocument2 pagesPast Simple Past ContinuousEsmeralda Gonzalez80% (5)
- Demolition and excavation worksDocument30 pagesDemolition and excavation worksHafizan Hanafiah100% (3)
- Sample Final Exam Larkin AnswersDocument18 pagesSample Final Exam Larkin AnswersLovejot SinghNo ratings yet
- Week 1-12 strength and conditioning programDocument6 pagesWeek 1-12 strength and conditioning programBrian Michael CarrollNo ratings yet
- Skeletal MuscleDocument11 pagesSkeletal MuscleStefania CristinaNo ratings yet
- Recent Advances in Nemaline Myopathy: Jenni Laitila, Carina Wallgren-PetterssonDocument13 pagesRecent Advances in Nemaline Myopathy: Jenni Laitila, Carina Wallgren-PetterssonSuzie Simone Mardones SilvaNo ratings yet
- Clearance of Defective Muscle Stem Cells by Senolytics Restores Myogenesis in Myotonic Dystrophy Type 1Document17 pagesClearance of Defective Muscle Stem Cells by Senolytics Restores Myogenesis in Myotonic Dystrophy Type 1wohoso4679No ratings yet
- Neurogenic Arthrogryposis and The Power of Phenoty - 2021 - Neuromuscular DisordDocument8 pagesNeurogenic Arthrogryposis and The Power of Phenoty - 2021 - Neuromuscular DisordSuzie Simone Mardones SilvaNo ratings yet
- Neurogenic Arthrogryposis and The Power of Phenoty 2021 Neuromuscular DisordDocument8 pagesNeurogenic Arthrogryposis and The Power of Phenoty 2021 Neuromuscular DisordSuzie Simone Mardones SilvaNo ratings yet
- Approach To The Diagnosis of Congenital Myopathies PIIS0960896613009942Document20 pagesApproach To The Diagnosis of Congenital Myopathies PIIS0960896613009942ElcklymNo ratings yet
- Frohman 2006Document11 pagesFrohman 2006Alfredo Enrique Marin AliagaNo ratings yet
- Multiple Sclerosis Lancet 2018Document15 pagesMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoNo ratings yet
- Lamperti 2010Document10 pagesLamperti 2010Marina GomesNo ratings yet
- Primary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersDocument10 pagesPrimary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Mechanobiology and Diseases of Mechanotransduction by IngberDocument14 pagesMechanobiology and Diseases of Mechanotransduction by IngberTensegrity Wiki100% (1)
- Congenital Muscular Dystrophies and Congenital.8 PDFDocument26 pagesCongenital Muscular Dystrophies and Congenital.8 PDFlithium2203No ratings yet
- Vocal Cord Paralysis and Feeding Difficulties As Early Diagnostic Clues of Congenital Myasthenic Syndrome With Neonatal Onset - A Case Report and Review of LiteratureDocument20 pagesVocal Cord Paralysis and Feeding Difficulties As Early Diagnostic Clues of Congenital Myasthenic Syndrome With Neonatal Onset - A Case Report and Review of LiteratureRA Tri Retno WulanNo ratings yet
- Neuromuscular Diseases PDFDocument205 pagesNeuromuscular Diseases PDFsalmazzNo ratings yet
- Cellular Regulation of Amyloid Formation in Aging and DiseaseDocument17 pagesCellular Regulation of Amyloid Formation in Aging and DiseasedianawilcoxNo ratings yet
- Muscular Dystrophies Seminar ReviewDocument16 pagesMuscular Dystrophies Seminar ReviewAli KhaqaanNo ratings yet
- Intensive Care Unit-Acquired WeaknessDocument13 pagesIntensive Care Unit-Acquired WeaknessAnonymous 3VkEwIsXRNo ratings yet
- Review: Mitochondrial Diseases: Hope For The FutureDocument21 pagesReview: Mitochondrial Diseases: Hope For The Futureluqui guzmanNo ratings yet
- Multiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkDocument11 pagesMultiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkasasakopNo ratings yet
- Complexity of Skeletal Muscle Degeneration Multi Systems Pathophysiology and Organ Crosstalk in DystrophinopathyDocument27 pagesComplexity of Skeletal Muscle Degeneration Multi Systems Pathophysiology and Organ Crosstalk in Dystrophinopathybose21No ratings yet
- Enfrentamiento General ContinuumDocument28 pagesEnfrentamiento General Continuummaria palaciosNo ratings yet
- Rehabilitation interventions may help muscle strength in multi-organ injuryDocument8 pagesRehabilitation interventions may help muscle strength in multi-organ injurysari murnaniNo ratings yet
- Acute Spinal Cord Injury: Pathophysiology and Pharmacological Intervention (Review)Document18 pagesAcute Spinal Cord Injury: Pathophysiology and Pharmacological Intervention (Review)Jasper CubiasNo ratings yet
- Utilisation of Exome Sequencing For Muscular Disorders in Thai Paediatric Patients: Diagnostic Yield and Mutational SpectrumDocument7 pagesUtilisation of Exome Sequencing For Muscular Disorders in Thai Paediatric Patients: Diagnostic Yield and Mutational SpectrumVeciGugiNo ratings yet
- Mechanobiology and Diseases of Mechanotransduction: Donald E IngberDocument14 pagesMechanobiology and Diseases of Mechanotransduction: Donald E IngberTezar AndreanNo ratings yet
- OCT Reveals Mechanisms of Neurodegeneration in Multiple SclerosisDocument12 pagesOCT Reveals Mechanisms of Neurodegeneration in Multiple SclerosisSara BkrNo ratings yet
- Neuromuscular Disorders I To 12Document280 pagesNeuromuscular Disorders I To 12Mário MachadoNo ratings yet
- Systemic Use of Corticosteroids in Neurological Disorders: Review ArticleDocument3 pagesSystemic Use of Corticosteroids in Neurological Disorders: Review ArticleDrscottmccallNo ratings yet
- Artigos Cel Tronco 0014Document7 pagesArtigos Cel Tronco 0014Gabriel Teske RiosNo ratings yet
- 149 FullDocument7 pages149 FullTolu TanimowoNo ratings yet
- Narrowing the Differential for "Floppy ChildDocument3 pagesNarrowing the Differential for "Floppy ChildMateen ShukriNo ratings yet
- Case Report of Intrafamilial Variability in Autosomal Recessive Centronuclear Myopathy Associated To A Novel BIN1 Stop MutationDocument6 pagesCase Report of Intrafamilial Variability in Autosomal Recessive Centronuclear Myopathy Associated To A Novel BIN1 Stop Mutationyael1991No ratings yet
- SeminarDocument20 pagesSeminarricardojosesotofontalvoNo ratings yet
- Neuromuscular Disorders - A. Zaher (Intech, 2012) WW PDFDocument280 pagesNeuromuscular Disorders - A. Zaher (Intech, 2012) WW PDFDaianaNo ratings yet
- Occurrence of Tendon Pathologies in MetabolicDocument10 pagesOccurrence of Tendon Pathologies in MetabolicSebastián Jiménez GaticaNo ratings yet
- Johnson 2019Document14 pagesJohnson 2019Mariel González.No ratings yet
- DMD PDFDocument14 pagesDMD PDFJefryan SofyanNo ratings yet
- Spinal Muscular Atrophy From Rags To Riches 2021 Neuromuscular DisordersDocument6 pagesSpinal Muscular Atrophy From Rags To Riches 2021 Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Daluiski 2001Document15 pagesDaluiski 2001Marcelo CortesNo ratings yet
- Insights Into The Molecular Regulatory Network of Pathomechanisms in OsteochondromaDocument8 pagesInsights Into The Molecular Regulatory Network of Pathomechanisms in OsteochondromaEga AihenaNo ratings yet
- Enfermedad MitocondrialDocument12 pagesEnfermedad MitocondrialOsvaldo CortésNo ratings yet
- Brainstem LesionsDocument7 pagesBrainstem LesionsErnesto Ochoa MonroyNo ratings yet
- Agm2 2 147 PDFDocument10 pagesAgm2 2 147 PDFAntonioNo ratings yet
- Newborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersDocument11 pagesNewborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersSuzie Simone Mardones SilvaNo ratings yet
- Congenital Myopathies: Clinical Phenotypes and New Diagnostic ToolsDocument16 pagesCongenital Myopathies: Clinical Phenotypes and New Diagnostic ToolsRizki Nandasari SulbahriNo ratings yet
- Eisenberg Et Al 2007Document7 pagesEisenberg Et Al 2007Dário Talita SantanaNo ratings yet
- Apoptosis - An Introduction For The Endodontist PDFDocument9 pagesApoptosis - An Introduction For The Endodontist PDFRamona MateiNo ratings yet
- Therapeutic Developments in Spinal Muscular Atrophy: Douglas M. Sproule and Petra KaufmannDocument13 pagesTherapeutic Developments in Spinal Muscular Atrophy: Douglas M. Sproule and Petra KaufmannNoniqTobingNo ratings yet
- ATROFIA MUSCULAR ESPINAL Lancet 2008Document14 pagesATROFIA MUSCULAR ESPINAL Lancet 2008Sebastián Silva SotoNo ratings yet
- Seminar: Mitchell R Lunn, Ching H WangDocument14 pagesSeminar: Mitchell R Lunn, Ching H WangCatalina AlzogarayNo ratings yet
- Transverse Myelitis: Clinical PracticeDocument9 pagesTransverse Myelitis: Clinical PracticearnabNo ratings yet
- Romero 2013Document16 pagesRomero 2013Rizki Nandasari SulbahriNo ratings yet
- Debilidad Neuromuscular Adquirida y Movilizacion Temprana en UTIDocument14 pagesDebilidad Neuromuscular Adquirida y Movilizacion Temprana en UTILucho FelicevichNo ratings yet
- Mcanism B NeurodegenerativeDocument13 pagesMcanism B NeurodegenerativeAlin CiubotaruNo ratings yet
- Traumatic Brain Injury 1: SeriesDocument13 pagesTraumatic Brain Injury 1: SeriesIntan HaddadNo ratings yet
- Seminar: Anthony H V SchapiraDocument10 pagesSeminar: Anthony H V Schapiramompou88No ratings yet
- Cerebral PalsyDocument5 pagesCerebral PalsyAnggie Pradetya MaharaniNo ratings yet
- The Floppy Infant Contribution of Genetic and MetaDocument21 pagesThe Floppy Infant Contribution of Genetic and MetaMagdaLena02No ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Kma 252 Exam 18 NewstyleDocument19 pagesKma 252 Exam 18 NewstyleSebin GeorgeNo ratings yet
- Envi. Data AcquisitionDocument10 pagesEnvi. Data AcquisitionDexter John Gomez JomocNo ratings yet
- Procedure For Design and DevelopmentDocument8 pagesProcedure For Design and DevelopmentISO SRCASNo ratings yet
- Y10 ICT End of TermDocument7 pagesY10 ICT End of TermIvy Atuhairwe BisoborwaNo ratings yet
- 4 McdonaldizationDocument17 pages4 McdonaldizationAngelica AlejandroNo ratings yet
- Implementing Cisco Application Centric Infrastructure: (Dcaci)Document2 pagesImplementing Cisco Application Centric Infrastructure: (Dcaci)radsssssNo ratings yet
- LMV Tyre SafetyDocument19 pagesLMV Tyre SafetykarvadNo ratings yet
- Summer Training Report at B H E L BhopalDocument66 pagesSummer Training Report at B H E L BhopalshantanuNo ratings yet
- Treatment: Animated Text Onstage:: Topic: Learning Objective: WMS Packages Module Introduction Display 1Document8 pagesTreatment: Animated Text Onstage:: Topic: Learning Objective: WMS Packages Module Introduction Display 1hikikNo ratings yet
- Nitrogen CycleDocument15 pagesNitrogen CycleKenji AlbellarNo ratings yet
- Multiple PDP Contexts User Guide Rev1Document16 pagesMultiple PDP Contexts User Guide Rev1ajit_balyan2003No ratings yet
- EnrollNOLA Daily Seat Availability ReportDocument2 pagesEnrollNOLA Daily Seat Availability ReportAdvocateOnlineNo ratings yet
- 2-Stress-Test Your Strategy The 7 Questions To AskDocument9 pages2-Stress-Test Your Strategy The 7 Questions To AskMalaika KhanNo ratings yet
- Wilkinson 2001Document44 pagesWilkinson 2001Toño Gaspar MuñozNo ratings yet
- Lucky TextileDocument5 pagesLucky TextileSaim Bin RashidNo ratings yet
- MAKING THINGS SIMPLER Review of Related LiteratureDocument72 pagesMAKING THINGS SIMPLER Review of Related Literaturejuju_batugal100% (1)
- I. VHF CommunicationsDocument12 pagesI. VHF CommunicationsSamuel OyelowoNo ratings yet
- Understanding Heavy Lifting Operations and Vessel StabilityDocument15 pagesUnderstanding Heavy Lifting Operations and Vessel StabilitygeorgesagunaNo ratings yet
- TCS L6 ActsDocument7 pagesTCS L6 ActsBhebz Erin MaeNo ratings yet
- X1jet MX Manual PDFDocument97 pagesX1jet MX Manual PDFrithik srivastavaNo ratings yet
- Thesis Based On Digital Image ProcessingDocument7 pagesThesis Based On Digital Image Processingkristenwilsonpeoria100% (1)
- Catalogue TecoDocument8 pagesCatalogue TecopriyantohonggonoNo ratings yet
- Macalloy Corporate Brochure September 2018 LR PDFDocument12 pagesMacalloy Corporate Brochure September 2018 LR PDFsampathkumarNo ratings yet
- BIG-IP Access Policy Manager CustomizationDocument118 pagesBIG-IP Access Policy Manager CustomizationDhananjai SinghNo ratings yet