Professional Documents
Culture Documents
Pi Is 1701216315302577
Uploaded by
rio rumaropenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pi Is 1701216315302577
Uploaded by
rio rumaropenCopyright:
Available Formats
CASE REPORT
Tubo-Ovarian Abscess Caused by
Candida Albicans in an Obese Patient
Valerie To, MDCM, Joshua Gurberg, MDCM, Srinivasan Krishnamurthy, MD, FRCSEd, FRCOG
Department of Obstetrics and Gynaecology, McGill University Health Centre, Montreal QC
Abstract Conclusion: Puisque lobsit morbide pourrait confrer une
immunodficience relative, les patientes obses morbides
Background: Tubo-ovarian abscess (TOA) arises in most cases pourraient contracter des infections inhabituelles, telles que des
from pelvic infection. Appropriate treatment includes use of abcs fongiques opportunistes.
antimicrobials and, especially in patients with increased BMI,
drainage of the contents.
J Obstet Gynaecol Can 2015;37(5):426429
Case: A 44-year-old morbidly obese woman (BMI 72) had a
persistent TOA despite receiving antibiotic treatment for four
months. She had no history of diabetes, and denied being INTRODUCTION
A
sexually active. Imaging demonstrated a pelvic abscess of 14.9
8.9 11.1 cm. Successful percutaneous drainage was performed pproximately 800 000 women develop pelvic
yielding purulent material which grew Candida albicans. The inflammatory disease annually in the United States,
patient recovered after drainage of the abscess and the addition of
fluconazole to her antimicrobials. She had no apparent risk factor
corresponding to approximately an incidence of 0.05%,
for acquiring such an opportunistic infection, other than her morbid which is similar to the Canadian incidence.13 Tubo-ovarian
obesity. abscess is reported to complicate 10% to 15% of cases
Conclusion: Because morbid obesity may confer a relative of PID, especially if the initial episode was inadequately
immunodeficiency, morbidly obese patients may develop unusual treated.4 Appropriate management is crucial, because there
infections such as opportunistic fungal abscesses.
are potentially severe short-term consequences (such as
abscess rupture and ensuing peritonitis and sepsis) and long
Rsum
term consequences (such as infertility, ectopic pregnancy,
Contexte: Les abcs ovario-tubaires (AOT) sont, dans la plupart and chronic abdominal/pelvic pain). Risk factors for TOA
des cas, attribuables une infection pelvienne. Parmi les development include having had a previous episode of
moyens de prise en charge adquats, on trouve le recours des
agents antimicrobiens et, particulirement chez les patientes qui
PID, having multiple sexual partners, having an intrauterine
prsentent un IMC accru, le drainage des abcs en question. device, and immunosuppression.4 PID is thought to arise
Cas: Une femme obse morbide de 44ans (IMC 72) prsentait from vaginal or cervical pathogens ascending into the
un AOT persistant malgr ladministration dune antibiothrapie sterile endometrial cavity, fallopian tubes, and peritoneal
pendant quatre mois. Elle ne prsentait pas dantcdents de cavity.5 A TOA can also result from other causes, such as
diabte et affirmait ne pas tre sexuellement active. Limagerie
a rvl la prsence dun abcs pelvien de 14,9cm sur 8,9cm diverticulitis, appendicitis, inflammatory bowel disease,
sur 11,1cm. Un drainage percutan a t men avec succs; la and gynaecologic or obstetric surgery.4 The infection is
prsence de Candida albicans a t identifie dans le matriel usually polymicrobial; microorganisms involved can include
purulent drain. La patiente a rcupr la suite du drainage de
labcs et de lajout de fluconazole ses agents antimicrobiens.
N. gonorrhoea, C. trachomatis, Bacteroides species, Peptococcus,
part son obsitmorbide, elle ne prsentait aucun facteur de Peptostreptococcus, and E. coli. 6 Nearly all causative pathogens
risque apparent de contracter une telle infection opportuniste. are bacteria, and can include rare microorganisms such as
Edwardsiella tarda and Pasteurella Multocida.7,8 TOA caused by
a fungus has been described in only three case reports to
Key Words: Female, pelvic infection, opportunistic infection,
Candida albicans, drainage, obesity, morbid date; in all three cases the causative organism was Candida
Competing Interests: None declared.
glabrata, and the patients either had an IUD or were
Received on June 3, 2014
immunocomprised.9-11 We report here a case of TOA caused
by Candida albicans, in a non-diabetic 44-year-old woman
Accepted on August 5, 2014
with no apparent risk factors except morbid obesity.
426 l MAY JOGC MAI 2015
Tubo-Ovarian Abscess Caused by Candida Albicans in an Obese Patient
THE CASE CT scan showing large gas-containing fluid collection
extending into the uterus and anterior abdominal wall
A 44-year-old woman, gravida 1 para 1, presented to
her community hospital with bilateral lower abdominal
pain, fever, and chills. Her past gynaecological history
was characterized by regular heavy menstrual flow and
dysmenorrhea, normal Papanicolaou smears, no history of
sexually transmitted infections, and no notable intrauterine
device use. Her past medical history included venous
thromboembolic events (a deep vein thrombosis and a
pulmonary embolism), urolithiasis, recurrent urinary tract
infections, chronic obstructive pulmonary disease, gout,
asthma, and morbid obesity (BMI 72). She was not diabetic.
Her surgical history included cholecystectomy, a Caesarean
section at term, and surgery for renal calculi. Her current
medications were warfarin, allopurinol, ferrous sulfate, and
fluticasone and salbutamol inhalers.
After the patient was found on CT scan to have a tubo-ovarian was 37.4C. Her hemoglobin concentration was 88g/L,
abscess measuring 12712cm, she began intravenous and white blood cell concentration was 12.2giga/L. A CT
antibiotic treatment with clindamycin, gentamicin, and scan of her abdomen and pelvis revealed a 15911cm
ampicillin. Two weeks later, she was transferred to a tertiary gas-containing fluid collection extending into the uterus
care hospital because her condition was not improving. A and anterior abdominal wall, consistent with an abscess, as
repeat CT scan showed a 161314cm multiloculated shown in the Figure.
pelvic abscess. Her white blood cell concentration was
17giga/L. She received intravenous Tazocin and oral Treatment was switched to intravenous Tazocin (4.5g at
doxycycline. After a few days of defervescence, and after 8-hour intervals). She subsequently developed C.difficile
consultation with an infectious disease specialist, this colitis and was given oral vancomycin. Concurrently, she
treatment was switched to oral metronidazole (500mg 3 developed a cutaneous fistula in her lower abdomen,
times daily) and oral levofloxacin (750mg daily). Her blood confirmed by CT scan, and this drained purulent fluid
and urine cultures were negative, as well as a gonorrhea and which was not cultured. Despite this treatment, the patient
Chlamydia PCR. An interventional radiologist attempted continued to have fever, persistent left lower quadrant
percutaneous drainage of the abscess, but was unsuccessful. rebound tenderness, and leukocytosis. Urine and blood
One week later, the abscess size had decreased to cultures showed no growth of pathogens throughout each
859cm on repeat CT. The patient felt better, and her of her hospitalizations. A vaginal culture, however, was
level of pain had decreased significantly. She was discharged positive for Candida albicans, but because the patient had
from hospital two weeks after admission (four weeks since no vaginal symptoms, no antifungal treatment was given.
her first presentation) to take oral antibiotics for three weeks. Three days after readmission to hospital, an interventional
radiologist was able to perform ultrasound-guided
At three weeks after discharge from hospital, the patient drainage of the abscess despite the patients body habitus,
presented back to her community hospital with recurrent
and inserted a pig-tail catheter for continuous drainage:
lower abdominal pain, increasing over four days, with
200mL of purulent, blood tinged fluid were drained. She
accompanying fever (up to 40C) and chills. She began
had been on antibiotics at that point for approximately
treatment with meropenem and was transferred again to
three months.
our tertiary care hospital.
Microscopy of the abscess fluid showed numerous hyphae,
On initial assessment, she had rebound tenderness in the
and culture resulted in growth of Candida albicans and
left lower quadrant of the abdomen, and her temperature
mixed enteric organisms. Treatment with oral fluconazole
(400mg daily) was added, and the patient showed rapid
clinical improvement. A repeat ultrasound examination
ABBREVIATIONS nine days after abscess drainage showed interval resolution.
PID pelvic inflammatory disease The patients level of pain improved, her white blood cell
TOA tubo-ovarian abscess count normalized, and she remained continuously afebrile.
MAY JOGC MAI 2015 l 427
Case Report
The patient was transferred to her community hospital The patient in our case did not wish to preserve her
two weeks after admission on intravenous Tazocin, oral fertility, but to assist in counselling women who do, several
fluconazole, and oral vancomycin. She continued to case series have reported on pregnancy outcomes after the
receive Tazocin and fluconazole for a total of four weeks, different modalities used in treatment of an unruptured
until a repeat CT scan showed complete resolution of the TOA. In a review by Rosen et al., only 4% to 15% of
abscess. She then stopped her antibiotic therapy and was women treated with antibiotics alone subsequently became
finally able to return home. pregnant, a rate similar to those who required a laparotomy
and antibiotics, but pregnancy rates reached 62% to 53%
following laparoscopic drainage and antibiotic therapy.17
DISCUSSION
These authors advocated for emergency laparoscopy and
In patients hospitalized with severe PID or who have medical management in all women presenting with a TOA
PID that is not responding to antibiotic therapy, tubo- who wish to conceive in the future. It is hypothesized that
ovarian abscess should be ruled out by means of imaging this management decreases the exposure of the adnexa
by ultrasonography or computed tomography. Once the to purulent material, thereby minimizing scarring and
diagnosis of TOA is made, management options include fibrosis.17 A retrospective study reported pregnancy rates
treatment with intravenous antibiotics alone, antibiotic of approximately 50% after transvaginal ultrasound-guided
therapy with imaging-assisted drainage of the abscess, drainage of TOA.18
or antibiotic therapy combined with surgery. Antibiotic We had hoped initially that a prolonged course of antibiotics
regimens include a broad spectrum beta-lactamase alone would be sufficient treatment for our patient,
agent (usually a third-generation cephalosporin) with because her high BMI and comorbidities made her a very
oral doxycycline, or clindamycin plus gentamycin. These poor candidate for surgery; percutaneous drainage of
regimens have been shown to have comparable efficacy the abscess was deemed to be almost impossible because
and response rates (defined as decreased pain, decreased of the thickness of her abdominal wall. However, weeks
white cell concentration, and loss of fever) of 63% to of antibiotic therapy did not result in resolution, and she
75%.6,12 However, a study by McNeeley et al. found that improved only with the combination of ultrasound-guided
a triple therapy regimen (using ampicillin, clindamycin, drainage (to decompress the abscess and allow identification
and gentamycin) was significantly more effective (87.5% of the causative organism) and appropriate antimicrobial
response) than cefotetan plus doxycycline (34% response) treatment (with the addition of antifungals to her therapy).
or clindamycin plus gentamicin (47% response).13 Curiously, yeast is an opportunistic microorganism and is not
Treatment failure may well be related to the size of the known to cause severe infection and form abscesses unless
abscess, as shown in a study by Reed et al., in which 60% the patient is immunocompromised9,19 or has an IUD, as in
of women with an abscess diameter of 10cm or more two other case reports.10,11 It is possible that the prolonged
required surgical intervention compared with 30% of antibiotic therapy before transfer to our hospital could have
those measuring 7 to 9cm and 15% of those measuring suppressed the detection of bacteria in culture media.
4 to 6cm.12
The patient did not have any of the known risks for immune
Patients with a TOA who fail to respond to antibiotic suppression; she was not diabetic and was presumed
treatment alone within 48 to 72 hours should be considered to be HIV-negative because she had not been sexually
for abscess drainage or surgery.14 Many patients treated active for many years (she declined testing at that time).
successfully with antibiotics may still require surgery for Other conditions known to be associated with immune
recurrence in the long term.6 Alternatively, if the patient suppression include use of immunosuppressive drugs,
renal or hepatic insufficiency, certain autoimmune diseases,
is not responding to antibiotic therapy or if the abscess
malignancy and asplenia.20 It is possible however that her
is large, imaging-guided drainage can be considered and
morbid obesity contributed to a relative immunodeficiency
has been shown in several studies to be well-tolerated
state, resulting in an opportunistic fungal infection
and efficacious.15,16 It can be guided by CT scanning or by
ascending from the vagina. Obesity is a state of low-grade
ultrasound, via the transabdominal, transvaginal, transrectal,
chronic inflammation, with altered circulating levels of
and transgluteal routes. Surgical treatment is reserved for
nutrients and hormones.21
ruptured, severe, or refractory cases of TOA, and includes
laparoscopy or possibly laparotomy for drainage of an Epidemiological data have shown that obese individuals
abscess, adhesiolysis, salpingo-oophorectomy, and/or are more prone than individuals of normal weight to
hysterectomy.4 infections, including postoperative and nosocomial
428 l MAY JOGC MAI 2015
Tubo-Ovarian Abscess Caused by Candida Albicans in an Obese Patient
infections.22 Physiologically, this can be correlated with an 7. Golub V, Kim AC, Krol V. Surgical wound infection, tuboovarian abscess,
and sepsis caused by Edwardsiella tarda: case reports and literature review.
altered immune response to infection, such as impaired Infection. 2010;38(6):4879.
lymphocyte proliferation.23 However, more studies are
8. Baud D, Bizzini A, Jaton K, Achtari C, Prodhom G, Greub G. Pasteurella
required to better understand why obese people are more multocida zoonotic ascending infection: an unusual cause of tubo-ovarian
prone to infections and if and how they respond differently abscess. Vector Borne Zoonotic Dis 2012;12(1):845.
to treatment (e.g., requiring higher doses of antibiotics). 9. Mikamo H, Ninomiya M, Tamaya T. Tuboovarian abscess caused by
Candida glabrata in a febrile neutropenic patient. J Infect Chemother
2003;9(3):2579.
CONCLUSION
10. Hsu WC, Lee YH, Chang DY. Tuboovarian abscess caused by Candida
An unruptured tubo-ovarian abscess should be drained, in a woman with an intrauterine device. Gynecol Obstet Invest
2007;64(1):146.
especially if it is large or not responding well to antibiotic
11. Toy EC, Scerpella EG, Riggs JW. Tuboovarian abscess associated with
therapy, or if future fertility is a concern. Drainage can be Candida glabrata in a woman with an intrauterine device. A case report.
performed either percutaneously with imaging guidance or J Reprod Med 1995;40(3):2235.
by surgery. Both approaches can be challenging in an obese 12. Reed SD, Landers DV, Sweet RL. Antibiotic treatment of tuboovarian
patient. Draining the abscess allows antibiotics to better abscess: comparison of broad-spectrum beta-lactam agents versus
penetrate it and allows antibiotic therapy to be tailored clindamycin-containing regimens. Am J Obstet Gynecol
1991;164(6 Pt 1):155661; discussion 612.
appropriately to the organisms cultured. Causative agents
may include yeast, necessitating the use of antifungal 13. McNeeley SG, Hendrix SL, Mazzoni MM, Kmak DC, Ransom SB.
Medically sound, cost-effective treatment for pelvic inflammatory
agents. Obese individuals may have impaired immunity disease and tuboovarian abscess. Am J Obstet Gynecol
compared with lean individuals, and they may have a 1998;178(6):12728.
different response to antibiotic therapy. 14. Soper DE. Pelvic inflammatory disease. Obstet Gynecol
2010;116(2 Pt 1):41928.
ACKNOWLEDGEMENTS 15. Goharkhay N, Verma U, Maggiorotto F. Comparison of CT-
or ultrasound-guided drainage with concomitant intravenous
The woman whose story is told in this case report has antibiotics vs. intravenous antibiotics alone in the management of
tubo-ovarian abscesses. Ultrasound Obstet Gynecol 2007;29(1):659.
provided written consent for its publication.
16. Gjelland K, Ekerhovd E, Granberg S. Transvaginal ultrasound-guided
aspiration for treatment of tubo-ovarian abscess: a study of 302 cases.
REFERENCES Am J Obstet Gynecol 2005;193(4):132330.
17. Rosen M, Breitkopf D, Waud K. Tubo-ovarian abscess management
1. Sutton MY, Sternberg M, Zaidi A, St Louis ME, Markowitz LE. Trends options for women who desire fertility. Obstet Gynecol Surv
in pelvic inflammatory disease hospital discharges and ambulatory visits, 2009;64(10):6819.
United States, 19852001. Sex Transm Dis 2005;32(12):77884.
18. Gjelland K, Granberg S, Kiserud T, Wentzel-Larsen T, Ekerhovd E.
2. United States Census Bureau. Vintage 2001: population estimates. Pregnancies following ultrasound-guided drainage of tubo-ovarian
National tables. Washington (DC): U.S. Census Bureau; 2001. abscess. Fertil Steril 2012;98(1):13640.
[updated 2011]. Available at: https://www.census.gov/popest/data/
historical/2000s/vintage_2001/index.html. Accessed February 5, 2015. 19. Miceli MH, Diaz JA, Lee SA. Emerging opportunistic yeast infections.
Lancet Infect Dis 2011;11(2):14251.
3. Manitoba Health Public Health. Provincial sexually transmitted diseases
control strategy. Winnipeg (MB): Manitoba Health Public Health; 2001. 20. Pasternack MS. Approach to the adult with recurrent infections.
Available at: http://www.gov.mb.ca/health/publichealth/cdc/std_ UpToDate. May 21, 2014.
strategy.pdf. Accessed February 16, 2015. 21. Milner JJ, Beck MA. The impact of obesity on the immune response to
4. Granberg S, Gjelland K, Ekerhovd E. The management of pelvic abscess. infection. Proc Nutr Soc 2012;71(2):298306.
Best Pract Res Clin Obstet Gynaecol 2009;23(5):66778. 22. Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis
5. Lareau SM, Beigi RH. Pelvic inflammatory disease and tubo-ovarian 2006;6(7):43846.
abscess. Infect Dis Clin North Am 2008;22(4):693708, vii.
23. Nieman DC, Henson DA, Nehlsen-Cannarella SL, Ekkens M, Utter AC,
6. Landers DV, Sweet RL. Tubo-ovarian abscess: contemporary approach to Butterworth DE, et al. Influence of obesity on immune function. J Am
management. Rev Infect Dis 1983;5(5):87684. Diet Assoc 1999;99(3):2949.
MAY JOGC MAI 2015 l 429
You might also like
- Tubo-Ovarian Abscess Caused by Candida AlbicansDocument7 pagesTubo-Ovarian Abscess Caused by Candida AlbicansBagus Indra KusumaNo ratings yet
- Case - Open AccessDocument5 pagesCase - Open AccessLeonhardt RowikaNo ratings yet
- 2014 Diagnosis of Pelvic Inflammatory Disease (PID) Intra Operative Findings and ComparisonDocument7 pages2014 Diagnosis of Pelvic Inflammatory Disease (PID) Intra Operative Findings and ComparisonUrología GinecológicaNo ratings yet
- Unsafe Abortion Leads to Life-Threating SepsisDocument4 pagesUnsafe Abortion Leads to Life-Threating SepsisHoneylyn100% (1)
- Pamj 12 65Document5 pagesPamj 12 65Iwi DancelNo ratings yet
- Paper On Bact VaginosisDocument16 pagesPaper On Bact VaginosisWael GaberNo ratings yet
- Chronic Breast Abscess Due To Mycobacterium Fortuitum: A Case ReportDocument3 pagesChronic Breast Abscess Due To Mycobacterium Fortuitum: A Case ReportWiwik SundariNo ratings yet
- What Is Causing This Girl S Abdominal Pain .10Document2 pagesWhat Is Causing This Girl S Abdominal Pain .10LuisNo ratings yet
- Nejmra1315399invasive Candidiasisoct8-2015Document12 pagesNejmra1315399invasive Candidiasisoct8-2015kendyNo ratings yet
- UnknownDocument5 pagesUnknownSulaeman Andrianto SusiloNo ratings yet
- Definition-: Pelvic Inflammatory Disease (PID) Is A Sexually Transmitted Inflammatory Condition of TheDocument7 pagesDefinition-: Pelvic Inflammatory Disease (PID) Is A Sexually Transmitted Inflammatory Condition of TheanweshaNo ratings yet
- EndometritisDocument3 pagesEndometritisJazmin Venice Lasala0% (1)
- Pelvic Infections in Women: Belgian Guidelines: OutlineDocument35 pagesPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNo ratings yet
- Monografia de PelvicDocument12 pagesMonografia de PelvicTracyVillegasNo ratings yet
- 0612 OBGM Update DuffDocument6 pages0612 OBGM Update DuffcarolineNo ratings yet
- Pelvic Inflammatory Disease Diagnosis and TreatmentDocument51 pagesPelvic Inflammatory Disease Diagnosis and TreatmentNorman AjxNo ratings yet
- Pelvic Inflammatory DiseaseDocument43 pagesPelvic Inflammatory DiseaseFauzia Jamiri - Abdurasid100% (2)
- Idog 03 210Document7 pagesIdog 03 210jwmeadow2401No ratings yet
- Tuberculous Ileal Perforation in A HIV Positive Patient A Case Report and Review of LiteratureDocument4 pagesTuberculous Ileal Perforation in A HIV Positive Patient A Case Report and Review of LiteratureLeonhardt RowikaNo ratings yet
- Puerperal Sepsis: Causes, Symptoms, PreventionDocument31 pagesPuerperal Sepsis: Causes, Symptoms, PreventionRumi Maharjan100% (1)
- Caz Bun 3Document7 pagesCaz Bun 3Dumitru RadulescuNo ratings yet
- Study of Relationship Between Anemia and Urinary Tract Infection in Pregnant WomenDocument5 pagesStudy of Relationship Between Anemia and Urinary Tract Infection in Pregnant WomenIvana ThiodoraNo ratings yet
- Salmonella Tuboovarian AbscessDocument3 pagesSalmonella Tuboovarian AbscessPaul HartingNo ratings yet
- S S I L I: Eptic Hock After Ntracervical Aminaria NsertionDocument3 pagesS S I L I: Eptic Hock After Ntracervical Aminaria Nsertionari naNo ratings yet
- PID: Understanding Pelvic Inflammatory DiseaseDocument34 pagesPID: Understanding Pelvic Inflammatory Diseaseraed faisalNo ratings yet
- Jurnal Pubmed EndoDocument6 pagesJurnal Pubmed EndoSofyanNo ratings yet
- Selecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)Document7 pagesSelecting Anti-Microbial Treatment of Aerobic Vaginitis: Genitourinary Infections (J Sobel, Section Editor)eva yustianaNo ratings yet
- Jurnal - Andi Nabila A. Rusli - Infeksi Streptokokus PDFDocument6 pagesJurnal - Andi Nabila A. Rusli - Infeksi Streptokokus PDFoke boskuNo ratings yet
- Multimodal Imaging of Fibrosing Mesenteric TuberculosisDocument6 pagesMultimodal Imaging of Fibrosing Mesenteric Tuberculosisdanielito1990No ratings yet
- Classic Diseases Revisited Abdominal Tuberculosis: To OneDocument9 pagesClassic Diseases Revisited Abdominal Tuberculosis: To OneATIKA INDAH SARINo ratings yet
- Sub Diaphragmatic Abscess Leading To Empyema Thoracis in A Case of Perforated Appendix A Rare Case ReportDocument4 pagesSub Diaphragmatic Abscess Leading To Empyema Thoracis in A Case of Perforated Appendix A Rare Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2. Pelvic Inflammatory DiseaseDocument25 pages2. Pelvic Inflammatory DiseasedeepaNo ratings yet
- Clinical Teaching 4PEUPERAL SEPSISDocument5 pagesClinical Teaching 4PEUPERAL SEPSISAjit M Prasad PrasadNo ratings yet
- Diagnosis and Management of Fungal Urinary Tract InfectionDocument14 pagesDiagnosis and Management of Fungal Urinary Tract InfectionIvan SanchezNo ratings yet
- Lectie PIDDocument59 pagesLectie PIDNatalie BondariNo ratings yet
- Systematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmentDocument16 pagesSystematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmenthendraNo ratings yet
- Gill 2011Document4 pagesGill 2011qwerNo ratings yet
- 2023.07.13 - Obstetrics S2. 02 - Puerperal InfectionDocument52 pages2023.07.13 - Obstetrics S2. 02 - Puerperal InfectionVignesh ThangavelNo ratings yet
- Gastritis y SarcinaDocument5 pagesGastritis y SarcinaDayana FajardoNo ratings yet
- Tuboovarian Abscess DuetoColonicDiverticulitis in A VirginDocument4 pagesTuboovarian Abscess DuetoColonicDiverticulitis in A VirginGustavoJPereiraSNo ratings yet
- Uti - HarriDocument9 pagesUti - HarrilololoNo ratings yet
- Gyne - (Section B) PID-STI-1Document45 pagesGyne - (Section B) PID-STI-1Kailash KhatriNo ratings yet
- Infections of The Female Pelvis: Intrapartum, Postpartum, and Postabortal InfectionsDocument9 pagesInfections of The Female Pelvis: Intrapartum, Postpartum, and Postabortal Infectionsalepedro1234No ratings yet
- General Gynaecology:, Leo Francis AquilizanDocument15 pagesGeneral Gynaecology:, Leo Francis AquilizanesjayemNo ratings yet
- Pelvic Inflammatory Disease: Causes, Symptoms, Diagnosis and TreatmentDocument5 pagesPelvic Inflammatory Disease: Causes, Symptoms, Diagnosis and TreatmentGina Eliana Custodio GonzalesNo ratings yet
- Successful Management of Giant Hydrocolpos in a LiDocument3 pagesSuccessful Management of Giant Hydrocolpos in a LiVictor FernandoNo ratings yet
- A. Tunica Albuguinea: NCM 102: Assessment ExamDocument9 pagesA. Tunica Albuguinea: NCM 102: Assessment ExamdubhieNo ratings yet
- C. Difficile-7Document7 pagesC. Difficile-7Suprakkash DasNo ratings yet
- Tubo-Ovarian Abscess in A Virgin Girl: Case ReportDocument4 pagesTubo-Ovarian Abscess in A Virgin Girl: Case ReportMaria MiripNo ratings yet
- Late Puerperal Sepsis, Case Report and Literature ReviewDocument10 pagesLate Puerperal Sepsis, Case Report and Literature ReviewMuskanNo ratings yet
- A Case of Postmenopausal Pyometra Caused by Endometrial TuberculosisDocument4 pagesA Case of Postmenopausal Pyometra Caused by Endometrial TuberculosisJimmy Oi SantosoNo ratings yet
- Foul Smelling Discharge 03 - Pelvic TBDocument2 pagesFoul Smelling Discharge 03 - Pelvic TBJayricDepalobosNo ratings yet
- 3 Meses VaricelaDocument4 pages3 Meses VaricelaNatalia CruzNo ratings yet
- Bacterial Vaginosis and Its Association With Infertility, Endometritis, and Pelvic Inflammatory DiseaseDocument7 pagesBacterial Vaginosis and Its Association With Infertility, Endometritis, and Pelvic Inflammatory DiseasePraneeth PaletiNo ratings yet
- Tuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeDocument3 pagesTuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeIOSRjournalNo ratings yet
- Cervical Ectopy 2017Document3 pagesCervical Ectopy 2017Marta GasparNo ratings yet
- MANAGEMENTUL_POSTOPERATOR_IN_SINDROMUL_INTESTINULUI_SCURT_CAZ_CLINICDocument2 pagesMANAGEMENTUL_POSTOPERATOR_IN_SINDROMUL_INTESTINULUI_SCURT_CAZ_CLINICA D ANo ratings yet
- Omental Tuberculosis: A Rare Presentation of Abdominal TB: December 2019Document4 pagesOmental Tuberculosis: A Rare Presentation of Abdominal TB: December 2019Putra YdpaNo ratings yet
- Dealmeida 2020Document3 pagesDealmeida 2020sukhmaNo ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Azmi - Uji Antibakteri Daun SingkongDocument10 pagesAzmi - Uji Antibakteri Daun SingkongimaNo ratings yet
- Ascaris LumbricoidesDocument14 pagesAscaris LumbricoidesLuis MercadoNo ratings yet
- Cellulitis - Symptoms, Causes, Treatments - Medical News TodayDocument7 pagesCellulitis - Symptoms, Causes, Treatments - Medical News TodayAnonymous ceYk4p4No ratings yet
- Rheumatic Heart Disease Neglected Disease of PovertyDocument4 pagesRheumatic Heart Disease Neglected Disease of Povertyjeenath justin dossNo ratings yet
- Infection Control BrochureDocument2 pagesInfection Control BrochureTeguh Aprian Maulana GultomNo ratings yet
- Subcutaneous MycosesDocument22 pagesSubcutaneous MycosesIan MosesNo ratings yet
- Vector Borne DiseasesDocument44 pagesVector Borne DiseasesJairo Villamizar AmadorNo ratings yet
- ATYPICAL Pneumonias Caused by Legionella Pneumophila, Chlamydophila Pneumoniae and Mycoplasma Pneumonia PDFDocument8 pagesATYPICAL Pneumonias Caused by Legionella Pneumophila, Chlamydophila Pneumoniae and Mycoplasma Pneumonia PDFShelyAzradNo ratings yet
- PI Virus (Enterovirus and Rhinovirus Groups)Document34 pagesPI Virus (Enterovirus and Rhinovirus Groups)Lovryan Tadena AmilingNo ratings yet
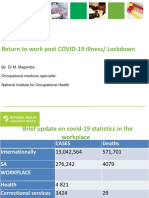
- Return to work post COVID-19 illness/ Lockdown guidelinesDocument20 pagesReturn to work post COVID-19 illness/ Lockdown guidelinesHuynh Luong Huy ThongNo ratings yet
- Contingency Plan for COVID-19 and Emerging DiseasesDocument31 pagesContingency Plan for COVID-19 and Emerging Diseasesanier joy sejatnomNo ratings yet
- A Critique On The Film Contagion - HardDocument2 pagesA Critique On The Film Contagion - HardEchoNo ratings yet
- Communicable DiseasesDocument12 pagesCommunicable Diseasesjustinejeon6No ratings yet
- Salmonella Typhi: ClassificationDocument4 pagesSalmonella Typhi: ClassificationMohammad Tahir KheridNo ratings yet
- Ebola BrochureDocument2 pagesEbola Brochureapi-386161677No ratings yet
- Candida Auris: A Fungus With Identity CrisisDocument8 pagesCandida Auris: A Fungus With Identity CrisisIsa LópezNo ratings yet
- Bio WeaponDocument27 pagesBio WeaponSimardeep SinghNo ratings yet
- Aids 8-12-2013Document6 pagesAids 8-12-2013giancarlo_luzziNo ratings yet
- What Is MeningitisDocument10 pagesWhat Is MeningitisJoshua Capa FrondaNo ratings yet
- Syphilis Symptoms, Causes, and DiagnosisDocument3 pagesSyphilis Symptoms, Causes, and DiagnosisIndra FahleviNo ratings yet
- Anthelmintic DrugsDocument35 pagesAnthelmintic DrugsRamla KashifNo ratings yet
- Bhavesh Desai-Male51 Years-8096Document2 pagesBhavesh Desai-Male51 Years-8096Prithwiraj ChakrabortyNo ratings yet
- ImmuzkcarlileDocument3 pagesImmuzkcarlileapi-242596953No ratings yet
- Lesson Plan For VirusesDocument6 pagesLesson Plan For VirusesAudrey LeonnaNo ratings yet
- Clade X Model PDFDocument5 pagesClade X Model PDFAlexandre Rocha Lima e MarcondesNo ratings yet
- Analyzing the Language of a PandemicDocument16 pagesAnalyzing the Language of a PandemicDaniela CovarrubiasNo ratings yet
- Original Research Paper: Ayurveda Key WordsDocument3 pagesOriginal Research Paper: Ayurveda Key WordsDilshad RazaNo ratings yet
- TUBERCULOSISDocument25 pagesTUBERCULOSISManuel Fatima Goncalves83% (6)
- NASKAH HIV-dikonversiDocument134 pagesNASKAH HIV-dikonversiAPRINo ratings yet
- Annual CME Program ITBPDocument7 pagesAnnual CME Program ITBPAnkit PrajapatiNo ratings yet