Professional Documents
Culture Documents
JCDR 10 SC06
Uploaded by
YANOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JCDR 10 SC06
Uploaded by
YANCopyright:
Available Formats
DOI: 10.7860/JCDR/2016/18570.
7920
Original Article
Ventilator-Associated Pneumonia:
Paediatrics Section
Incidence, Risk Factors and
Outcome in Paediatric Intensive Care
Units at Cairo University Hospital
Yasmine S. Galal1, Meray Rene L. Youssef2, Sally K. Ibrahiem3
ABSTRACT Methicillin-resistant Staphylococcus aureus (MRSA) (14.4%).
Introduction: Ventilator-Associated Pneumonia (VAP) is a major VAP patients were significantly younger than non-VAP ones. The
cause of hospital morbidity, mortality and increased health care incidence of VAP in comatose patients and those with MOSF
costs. Although the epidemiology, pathogenesis and outcome was significantly higher. Prior antibiotic use for > 48 h before
of VAP are well described in adults; few data exist regarding MV, supine body positioning and reintubation were significantly
VAP in paediatric patients, especially in developing countries. associated with VAP. On multiple logistic regression analysis,
MOSF; prior antibiotic use > 48h; reintubation; coma; and age
Aim: To determine the incidence, risk factors and outcome of
remained independent predictors of VAP. Mortality rate among
VAP in two Paediatric Intensive Care Units (PICUs) at Cairo
the VAP group was significantly higher compared to the non-
University Hospital.
VAP one (68.2% vs. 48.5%, p<0.001). Survival curve analysis
Materials and Methods: A total of 427 patients who received showed a shorter median survival time in VAP patients.
Mechanical Ventilation (MV) were included in this prospective
Conclusion: Identification of risk factors and outcome of VAP
study during the period from September 2014 till September
in PICUs may help in reducing the incidence and improving
2015. Patients were observed daily till VAP occurrence, discharge
patients outcomes. The incidence of VAP in this study was
from the unit or death, whichever came first. Demographic,
relatively high. The most prominent risk factors for occurrence
clinical characteristics, laboratory results, radiographic and
of VAP were MOSF, prior antibiotic use for > 48 h before MV,
microbiological reports were recorded for all patients.
reintubation, coma and age. Proper use of antibiotics before
Results: Nearly 31% patients developed VAP among the entire MV in PICUs is essential. Also, adequate training of nurses and
cohort. The incidence density was 21.3 per 1000 ventilator days. strict supervision of infection control protocols are crucial. Lack
The most frequently isolated organisms from VAP patients were of a gold standard for the diagnosis of VAP and difficulty in
Pseudomonas aeruginosa (47.7%), Acinetobacter (18.2%) and sampling procedures were among the study limitations.
Keywords: Incidence density, Mechanical ventilation, Reintubation, Survival curve, Ventilator days
Introduction The risk factors responsible for VAP occurrence can be classified
Ventilator-Associated Pneumonia (VAP) refers to nosocomial into: host related, device related and personnel related. Host
pneumonia occurring 48 hours or more after initiation of related factors include associated co-morbidities such as acute
mechanical ventilation (MV) [1]. VAP is the most common Hospital- respiratory distress syndrome, cardiovascular system diseases,
Associated Infection (HAI) among adult patients in Intensive Care and central nervous system diseases; Multiple Organ System
Units (ICUs), with frequencies ranging from 15-45% [2]. Moreover, Failure (MOSF); level of consciousness; patients' body positioning;
it is the second most common HAI after blood stream infection in number of intubations; and medications including sedatives and
the paediatric age group, accounting for about 20% of all HAIs in prior antibiotic administration [10]. Device-related factors include
the paediatric intensive care units (PICUs) and has a rate of 2.9- the endotracheal tube, the ventilation circuit and the presence of
21.6 per 1000 ventilator days [3]. VAP is associated with increased a nasogastric or an orogastric tube [12]. Personnel related factors
hospital morbidity; mortality; duration of hospitalization by an include improper hand hygiene and inadequate use of personal
average of 7-9 days per patient; and health care costs [4-7]. protective equipment by the nursing staff, resulting in cross-
contamination between patients [13].
The incidence rates of VAP are higher in developing countries
with limited resources [8]. In Egypt, a study of device-associated The epidemiology and outcomes of VAP in adults were addressed
infection rates in the PICUs in a number of hospitals has showed in various studies [2,14,15]; However, fewer researches were
that the overall rate of HAIs was 24.5% and that of VAP was 31.8 conducted among paediatric patients [6,7]. To the researchers'
per 1000 ventilator days [9]. best evidence, no published data has been found regarding VAP
in the PICUs at Cairo University Hospital.
The onset of VAP can be divided into: early which occurs 48
to 96h after intubation and late which occurs more than 96h
after intubation. Early and late VAP differ in their pathogenesis, aim
microorganisms responsible, antibiotic sensitivity, outcome Hence, this study aims to determine the incidence, risk factors and
and treatment [10]. The pathogenesis of VAP involves bacterial outcome of VAP in the PICUs at Cairo University Hospital egypt.
invasion of the pulmonary parenchyma in patients receiving MV.
Inoculation of the previously sterile lower respiratory tract results Materials and Methods
from aspiration of secretions, colonization of the aerodigestive A hospital-based prospective cohort study was performed during
tract, or use of contaminated equipment or medications [11]. the period from September 2014 to September 2015 to detect
the incidence, causative organisms, risk factors, and outcomes
6 Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11
www.jcdr.net Yasmine S. Galal et al., Ventilator-associated Pneumonia in Pediatric Intensive Care Units
of VAP. The study was conducted in two separate PICUs at 132/427x100= 30.9%
the Paediatric Hospital, Cairo University; one at the emergency VAP incidence density was calculated as follows: (Number of
Department (included 24 beds and 24 ventilators) and the other at cases with VAP/Number of ventilator days) x 1000= VAP rate per
the 4th floor (included 14 beds and 14 ventilators). 1000 ventilator days [20].
All paediatric patients admitted to the selected PICUs for MV and 132/6197 x 1000= 21.3 per 1000 ventilator days.
fulfilling the inclusion criteria (n=427) were enrolled for the study.
Sepsis: Defined as suspected infection in the presence of two
Inclusion criteria: Intubation and MV for at least 48h and patients or more Systematic Inflammatory Response Syndrome (SIRS)
older than one month-up to12 years. criteria [21]. SIRS refers to a clinical response to a non-specific
Exclusion criteria: Neonates and pneumonia as admission insult, it entails 2 or more of the following: fever > 38C or < 36C,
diagnosis or detected within the first 48 hours. Patients were heart rate > 90 beats per minute, respiratory rate >20 breaths per
enrolled consecutively and were prospectively followed till VAP minute, and abnormal WBC count (>12,000/mm3 or < 4000/mm3)
diagnosis, death or discharge from the PICUs, whichever came [21]. MOSF: a progressive concurrent dysfunction of two or more
first. According to VAP occurrence, the study participants were organ systems; it is a non-specific expression of critical illness and
divided into VAP and non-VAP groups. a leading cause of death in critical care settings [21].
A data collection sheet was used to collect and record the following: Approval of the study protocol was obtained from the Ethical
demographic data e.g., age and sex and clinical data including Committee at the Faculty of Medicine, Cairo University. Informed
date of ICU admission; cause of admission (medical or surgical); consent was obtained directly from the legal guardian of each
associated co-morbidities; primary diagnosis (reason for initiation patient (mother, father, or other caregiver) before enrolment
of ventilation); Paediatric Risk of Mortality (PRISM) III score; level and after explaining the study objectives and importance. All
of consciousness according to the Glasgow Coma Scale (GCS); administrative permissions were obtained from the Chairman of
duration of MV; length of ICU stay; occurrence of VAP; the causative the PICUs where the study was conducted. All the procedures
organisms of VAP; duration of antibiotic use (<48h versus >48h for data collection were treated with confidentiality according to
before MV); positioning of patients (supine or semi-recumbent); Helsinki Declarations of biomedical ethics [22].
reintubation; and the patients' outcome (discharge, improvement
or death). All cases were clinically examined (respiratory rate, color, Statistical analysis
use of accessory muscles, and auscultation to detect presence of Statistical analysis of the precoded data was done using the
rales) on admission and scored according to the GCS to detect Statistical Package for Social Science Program (SPSS, version 21).
the level of consciousness [16]. The first part of the analysis examined the entire cohort of patients.
Cases were kept on broad spectrum antibiotic therapy before MV Data were summarized using the median and Interquartile Range
e.g. Tinam, Meropenam, Amikacin, Polymyxin, Ciprofloxacin and (IQR) for quantitative variables and frequency and percentage for
Vancomycin. Routine investigations were done for all patients e.g. qualitative variables. Univariate analysis was used for comparing
Complete Blood Count (CBC), blood sugar, liver function tests, variables for the outcome groups of interest (VAP versus no
kidney function tests, blood culture, arterial blood gases and VAP), and all tests of significance were two tailed. The Mann-
oxygen saturation. Baseline chest x-ray was done after intubation Whitney test was used for comparing quantitative variables,
of patients on MV. It was repeated on follow up of patients when while the x2 statistic or Fisher-exact test was used for qualitative
they developed signs of pneumonia. PRISM III score was assessed variables. The primary data analysis compared patients with VAP
for all patients to detect the risk of mortality [17]. to those without VAP, and then the results of these tests were
confirmed with a multivariate logistic regression analysis using
Symptoms and signs for patients under MV that raised suspicion
a stepwise approach. The results of logistic regression analysis
for VAP included: altered mental state with no recognized cause,
were reported as Adjusted Odds Ratios (AORs) with their 95%
new onset of purulent secretions, change in sputum character,
Confidence Intervals (CIs). Kaplan-Meier survival curve was done
new onset or worsening of cough, increased respiratory secretions
to demonstrate the predicted hospital survival in patients with and
or suctioning requirements.
without VAP. All tests were considered statistically significant at a
VAP was defined on the basis of clinical, radiologic and p-value of <0.05.
microbiological criteria. VAP was considered if it happened
after 48 h of MV and was diagnosed based on the presence of
Results
a new persistent infiltrate on chest radiograph and at least two
A total of 427 paediatric patients meeting all the inclusion criteria
of the following: 1) fever of 38C; 2) leucopenia (< 4000 white
were enrolled for the current study. Among these, VAP developed
blood cells (WBC)/mm3) or leukocytosis ( 12,000 WBC/mm3);
in 132 patients (30.9%). The median age of the studied group
3) purulent respiratory secretions; 4) worsening gas exchange
was 8 months (IQR= 5-36). The total ICU mortality was 54.6%
(PaO2/FiO2 < 240) [18]. Early onset VAP: is that which occurred
[Table/Fig-1]. The most frequently encountered organisms from
within 96 h of intubation and MV, while late onset VAP is that
endotracheal aspirate cultures were Pseudomonas (47.7%),
which occurred after 96 hour [10]. Microbiological workup was
Acinetobacter (18.2%) and Methicillin-Resistant Staphylococcus
done once VAP was clinically suspected, endotracheal aspirates
aureus (MRSA) (14.4%). The incidence density of VAP was 21.3
were performed; sputum was collected from patients from the
cases per 1000 ventilator-days.
tip of a suction catheter inserted in the endotracheal tube and
transported in sterile tubes to the Clinical Pathology Department Patients who developed VAP were significantly younger (median=6,
at Cairo University for diagnosis. Cultures were done using Blood, IQR=4-18) than those who didnt (median=12, IQR=5-42),
Chocolate and Mac-conkey agar systems, direct films were used p=0.013. A significantly higher percent of VAP patients presented
for microscopic examination with gram stain to detect gram with coma and MOSF compared to non-VAP ones (37.9% vs.
negative bacilli and gram positive cocci. VAP was established with 22.4%, p=0.001) and (60.6% vs. 23.4%, p<0.001), respectively.
a positive quantitative culture {cut-off point 106 (colony-forming The VAP and non-VAP groups differed significantly regarding the
units (CFU)/mL)} [19]. primary diagnosis [Table/Fig-2].
VAP incidence was calculated as follows: (Number of cases A significantly higher percent of patients with VAP had antibiotics
with VAP/Total number of patients who received MVx100) = VAP for more than 48 hour before MV (67.4% vs. 43.4%, p<0.001).
rate per 100 patients. Among VAP patients, 33.3% were re-intubated compared to
Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11 7
Yasmine S. Galal et al., Ventilator-associated Pneumonia in Pediatric Intensive Care Units www.jcdr.net
Variable Total (n=427) VAP p-value
Gender M/F n, (%) 235/192, (55/45) Yes (n=132) No (n=295)
Age (months) median, (IQR) 8 (5 - 36) Previous use of antibiotics > 48 h n, (%) 89 (67.4) 128 (43.4) <0.001
Cause of ICU admission medical/surgical n, (%) 400/27, (93.7/6.3) Supine position n, (%) 105 (79.5) 201 (68.1) 0.020
PRISM III on admission median, (IQR) 10 (6 - 19) Reintubation n, (%) 44 (33.3) 59 (20) 0.005
Previous use of antibiotics > 48hrs n, (%) 217 (50.8) Weaning n, (%) 44 (33.3) 138 (46.8) 0.011
Primary diagnosis n, (%) [Table/Fig-3]: Comparison between patients with and without ventilator-associated
pneumonia regarding treatment related risk factors.
Cardiovascular 82 (19.2) Data are expressed as number and %, Chi square test of significance was used for comparison
Neurologic 166 (38.9)
VAP p- value
Respiratory 120 (28.1)
Variable Yes (n=132) No (n=295)
Sepsis 31 (7.3)
Duration of MV median, (IQR) 8 (5-15) 12 (8-18) <0.001**
Neuromuscular 28 (6.6)
LOS in ICU median, (IQR) 11 (7-18.5) 17 (10-23) <0.001**
Complications of MVn, (%) 167 (39.1)
Mortality n, (%) 90 (68.2) 143 (48.5) <0.001*
VAP 132 (30.9)
[Table/Fig-4]: Comparison between patients with and without ventilator-associated
Pneumothorax 41 (9.6)
pneumonia regarding the outcome.
Atelectasis 18,(4.2) Data are expressed as number and % for qualitative variables and median with (IQR) for quantitative
variables.
Weaning n, (%) 182 (42.6) *Chi square with Fisher exact
**Mann-Whitney test
Reintubation n, (%) 103 (24.1)
Supine position n, (%) 306 (71.7) VAP onset
Coma n, (%) 116 (27.2) Mortality Early (n=65) Late (n=67) p-value
MOSF n, (%) 149 (34.9) N % N %
ICU Mortality n, (%) 233 (54.6) Yes 38 58.5 52 77.6 0.025
Duration of MV (days) median, (IQR) 11 (5 - 17) No 27 41.5 15 22.4
Length of ICU stay (days) median, (IQR) 16 (8 - 22) [Table/Fig-5]: Comparison between the onset of ventilator-associated pneumonia
and mortality.
[Table/Fig-1]: Characteristics of 427 mechanically ventilated patients at the
paediatric intensive care units, Cairo University Hospital.
Data are expressed as number and % for qualitative variables and median with interquartile range respectively). Mortality rate among VAP patients was significantly
(IQR) for quantitative variables.
MOSF: Multi-Organ System Failure higher compared to non-VAP patients (68.2% vs. 48.5%, P<0.001).
[Table/Fig-5] shows that late onset VAP (>96 h) was significantly
VAP p-value associated with higher mortality rate (77.6% vs. 58.5%, P=0.025)
Yes (n=132) No (n=295)
than early onset VAP (<96h).
Gender n, (%) A backward stepwise logistic regression model was conducted
to explore the significant predictors of VAP [Table/Fig-6]. Variables
Male 58 (43.9) 177 (60) 0.002*
entered on 1st step were: gender, age in months, coma, MOSF,
Female 74 (56.1) 118 (40)
CVS disorders and sepsis (as an indication for MV), previous
Age (months) median, (IQR) 6 (4-18) 12 (5-42) 0.013** use of antibiotics > 48h, reintubation, and supine position. The
Coma n, (%) 50 (37.9) 66 (22.4) 0.001* last step revealed that only MOSF (OR=4.619, 95% CI 2.903-
MOSF n, (%) 80 (60.6) 69 (23.4) <0.001* 7.347, p<0.001), previous use of antibiotics > 48 h (OR=2.259,
PRISM III on admission median, (IQR) 12 (6-24) 10 (6-15) 0.052**
95% CI 1.412-3.616, p=0.001), re-intubation (OR=1.794, 95% CI
1.076-2.991, p=0.025), coma (OR=1.733, 95% CI 1.051-2.856,
Primary diagnosis n, (%)
p=0.031), and age in months (OR=0.990, 95% CI 0.983-0.998,
CVS 37 (28) 45 (15.3) 0.003*
p=0.013) were the significant predictors of VAP.
CNS 52 (39.4) 114 (38.6) 0.915*
Kaplan-Meier survival analysis revealed that the median survival
Respiratory 25 (18.9) 95 (32.2) 0.005* time for VAP patients (12, 95% CI 9.6-14.4) was significantly
Sepsis 15 (11.4) 16 (5.4) 0.042* shorter (log rank, p<0.001) compared to non-VAP patients (30,
Neuromuscular 3 (2.3) 25 (8.5) 0.019* 95% CI 23.7-36.3) [Table/Fig-7].
Cause of ICU admission n, (%) [Table/Fig-8] showed normal chest X ray for patient on MV in its
Medical 121 (91.7) 279 (94.6) 0.284* 1st two hours then he developed by lateral lung infiltration on day
three on MV.
Surgical 11 (8.3) 16 (5.4)
[Table/Fig-2]: Comparison between patients with and without ventilator-associated
pneumonia regarding demographic and clinical risk factors. Discussion
Data are expressed as number and % for qualitative variables and median with (IQR) for quantitative Although MV is an essential component of modern ICU care, it is
variables.
*Chi square with Fisher exact associated with a considerable risk of VAP [23]. Proper recognition
**Mann-Whitney test
Variables 95% CI OR p-value
20% among the non-VAP ones, p=0.005. Regarding positioning
of patients, 79.5% of the VAP group was in the supine position MOSF 2.903 - 7.347 4.619 <0.001
compared to 68.1% of the non-VAP group, p=0.02 [Table/Fig-3]. Previous use of antibiotics > 48hrs 1.412 - 3.616 2.259 0.001
The outcome of both study groups was shown in [Table/Fig-4]. Reintubation 1.076 - 2.991 1.794 0.025
The total duration of MV and that of ICU stay among patients Coma 1.051 - 2.856 1.733 0.031
with VAP (median=8, IQR=5-15 and median=11, IQR=7-18.5, Age in months 0.983 - 0.998 0.990 0.013
respectively) was significantly shorter (p<0.001) compared to non- [Table/Fig-6]: Logistic regression analysis of risk factors associated with ventilator-
VAP patients (median=12, IQR=8-18 and median=17, IQR=10-23, associated pneumonia among patients in the paediatric intensive care units.
8 Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11
www.jcdr.net Yasmine S. Galal et al., Ventilator-associated Pneumonia in Pediatric Intensive Care Units
factors of VAP after paediatric cardiac surgery, Pseudomonas
aeruginosa and MRSA were the most common pathogens isolated
from the endotracheal aspirate [3]. In a study conducted by Aelami
et al., publications addressing VAP in any inpatient paediatric
population were analyzed, it was found that Pseudomonas
aeruginosa, Acinetobacter and Enterobacteriaceae were the most
common causative agents of VAP [30].
In this study, coma and MOSF were among the patient-related risk
factors for development of VAP. Similarly, in a study conducted
in the United States, patients with VAP had a greater incidence
of coma (p=0.007) compared to those without [14]. Patients with
VAP had a higher PRISM III score on admission compared to those
without VAP, but no significant difference was observed (p=0.052).
Roeleveld et al., found that VAP patients were more likely to have
an admission PRISM III score of 10 (p=0.033) [31].
In this study, there was a significant association between the
primary diagnosis of patients namely sepsis (p=0.042) and CVS
disorders including congenital heart diseases (p=0.003) and the
increased risk of VAP. However, in a study conducted in India,
[Table/Fig-7]: Kaplan-Meier survival analysis of patients relative to ventilator- the primary diagnosis of patients enrolled (septicaemia, cardiac,
associated pneumonia. neurologic and cancer) was similar in those who developed or did
not develop VAP [32].
Treatment with antibiotics may affect the ecology of colonization
by suppressing the normal flora and consequently increasing
the risk of acquiring a nosocomial infection that is more likely
to be drug-resistant [26]. Although prior antibiotic therapy has
been recognized as a risk factor for VAP in previous studies of
adults [33,34], it was rarely mentioned in studies of paediatric
patients [26,35]. In this study, antibiotic use for >48h before MV
was associated with a significantly higher risk of VAP (p<0.001).
Similarly, Almuneef et al., found that prior antibiotic therapy was
significantly associated with increased risk of VAP (p=0.005) [26].
[Table/Fig-8]: Chest X Ray of patient on MV 1st hour and after 3 days.
In an effort to reduce the incidence of VAP in our PICU, rotation
and appropriate use of antibiotics will be considered.
of high risk patients and of potential modifiable risk factors may Many studies highlighted the role of aspiration in the pathogenesis
outline preventive measures and institutional strategies to reduce of VAP [6,35]. Reintubation frequently implicates aspiration of
the infection [2]. gastric or oropharyngeal contents that are contaminated with
The incidence of VAP differs according to the studied population, colonizing flora. In the current study, reintubation was found to
type of ICU and the country income level [24,25]. In this study, be a risk factor of VAP (p=0.005). Similar findings were reported
the incidence of VAP was nearly 31%, which is relatively high by Srinivasan et al., Patria et al., and Chiru et al., [7,27,35]. In
compared to other figures in the literature. However, a lower figure contrast Elward et al., and Gautam et al., did not find a higher VAP
was detected in another study conducted in Egypt to identify the risk with reintubation [6,28].
rate of device-associated infections, where the incidence of VAP Supine positioning may also facilitate aspiration leading to an
was 12.6% in the PICUs [9]. Thus, a considerable within-country increased risk of VAP [36]. In the present study, patients in the
variation can also exist which could be attributed to variations in supine position had an increased risk of VAP compared to those
VAP definitions, study methods, as well as the extent of application in the semi-recumbent position. Measures to prevent aspiration
of infection control programs for preventing nosocomial infections. in adults, including elevation of the head to 30- 45, continuous
In a 30-month prospective study in a PICU in Saudi Arabia, the subglottic suctioning and continuous lateral rotation of the bed
VAP incidence was 10.3% [26]. Moreover, Patria et al., estimated to improve drainage of lower airway secretions, are expected to
a VAP incidence of only 6.6% in the PICU at a University Hospital
be effective in children too [4,26]. Smulders et al., concluded that
in Milan, Italy [27].
subglottic secretion drainage was associated with a relative risk
The incidence density of VAP in this study was 21.3 cases per reduction of VAP [37].
1000 ventilator days. In another study conducted in Egypt, the
Several studies have showed that prolonged duration of MV and
VAP rate in the PICUs was 31.8 per 1000 ventilator days [9]. In
PICU stay were associated with increased VAP risk [3,32,35].
contrast, lower rates were reported in a 1-year prospective study
in Australia, where the incidence density of VAP in a tertiary PICU Surprisingly, in the current study, different findings were observed
was 7.02 per 1000 ventilation days [28]. Moreover, OBrien et al., where the duration of MV and the LOS in PICU were significantly
in the United States found a mean VAP rate of 1.33 per 1000 shorter in VAP patients compared to non-VAP ones. This finding
ventilator days [29]. could be attributed to decreased median survival time in the
VAP group subjecting them to earlier mortality compared to the
The results of sputum cultures in the current study revealed that
gram-negative bacteria were isolated from the majority of VAP non-VAP one as shown by the Kaplan-Meier survival analysis. In
patients (75.7%), with Pseudomonas aeruginosa and Acinetobacter contrast, Rello et al., stated that patients with and without VAP
predominance, while Methicillin-Resistant Staphylococcus aureus had similar in-hospital survival as shown by Kaplan-Meier curves,
(MRSA) accounted for the majority of the gram-positive infections. although the mortality rate was higher for patients without VAP
Similarly, in a study conducted in Taiwan to determine the risk during the first 30 hospital days [14].
Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11 9
Yasmine S. Galal et al., Ventilator-associated Pneumonia in Pediatric Intensive Care Units www.jcdr.net
In the present study, mortality rate in the VAP group was significantly [2] Jaimes F, De La Rosa G, Gomez E, Munera P, Ramirez J, Castrillon S. Incidence
and risk factors for ventilator-associated pneumonia in a developing country:
higher compared to the non-VAP one. Similarly, patients with VAP
where is the difference? Resp Med. 2007;101(4):762-67. Doi: 10.1016/j.
had a higher mortality rate (p=0.04) in a study conducted in a PICU rmed.2006.08. 008.
in Italy [27]. Ramya et al., and Alexis et al., also reported similar [3] Tang CW, Liu PY, Huang YF, Pan JY, Lee SS, Hsieh KS, et al. Ventilator-
results [38,39]. In contrast, Huang et al., found that mortality rates associated pneumonia after paediatric cardiac surgery in southern Taiwan. J
Microbiol Immunol Infect. 2009;42(5):413-19.
of the VAP and non-VAP groups were similar in a PICU in Taiwan [4] Urrea M, Pons M, Serra M, Latorre C, Palomeque A. Prospective incidence study
[40]. In the current study, distinction between early and late onset of nosocomial infections in a paediatric intensive care unit. Paediatr Infect Dis J.
VAP was done in relation to the mortality rate, where patients with 2003;22:490-93.
[5] Stover BH, Shulman ST, Bratcher DF, Brady MT, Levine GL, Jarvis WR.
late onset VAP had a significantly higher mortality rate (P=0.025)
Nosocomial infection rates in US childrens hospitals neonatal and paediatric
than those with an early onset. However, differentiation between intensive care units. Am J Infect Control. 2001;29:152-57.
the two types is also important with regards to the causative [6] Elward AM, Warren DK, Fraser VJ. Ventilator-associated pneumonia in
organisms and thus the required treatment [14]. paediatric intensive care unit patients: risk factors and outcome. Paediatrics.
2002;109:75864.
In the current study, significant variables on univariate analysis [7] Srinivasan R, Asselin J, Gildengorin G, Wiener-Kronish J, Flori HR. A
(p<0.05) were entered in a multivariate logistic regression model; prospective study of ventilator-associated pneumonia in children. Paediatrics.
only MOSF, prior antibiotic use >48h, reintubation, coma and 2009;123(4):1108-15. Doi: 10.1542/peds.2008-1211.
[8] Raza MW, Kazi BM, Mustafa M, Gould FK. Developing countries have their own
age in months remained significant. In study conducted in the characteristic problems with infection control. J Hosp Infect. 2004;57(4):294-
Netherlands, univariate analysis showed that risk factors for VAP 99.
in paediatric patients after cardiac surgery were: a PRISM score [9] Rasslan O, Seliem ZS, Ghazi IA, Abd El Sabour M, El Kholy AA, Sadeq FM.
Device-associated infection rates in adult and paediatric intensive care units
of 10 on admission, receiving fresh frozen plasma transfusions
of hospitals in Egypt. International Nosocomial Infection Control Consortium
and a longer aortic cross-clamp time [31]. Only a PRISM score (INICC) findings. J Infect Public Health. 2012;5(6):394-402. Doi: 10.1016/j.
of 10 remained significant after a multiple logistic regression jiph.2012.07.002.
analysis. In another study conducted in Saudi Arabia, significant [10] Fathy A, Abdelhafeez R, El-Gilany A, AbdElhafez SA. Analysis of ventilator
associated pneumonaia (VAP) studies in Egyptian University Hospitals. Egypt J
variables for VAP after multiple logistic regressions were only prior Chest Dis Tuberc. 2013;62(1):17-25. Doi: 10.1016/j.ejcdt.2013.04.008.
antibiotic therapy, continuous enteral feeding and bronchoscopy [11] Abdel-Gawad TA, El-Hodhod MA, Ibrahim HM, Michael YW. Gastroesophageal
[26]. Chiru et al., found previous use of one or more antibiotics, reflux in mechanically ventilated paediatric patients and its relation to ventilator-
associated pneumonia. Crit Care. 2009;13:R164. Doi: 10.1186/cc8134.
antifungal drugs and reintubation to be positively associated with
[12] Ferrer R, Artigas A. Clinical review: Non-antibiotic strategies for preventing
the development of VAP in children after a multivariate analysis ventilator-associated pneumonia. Crit Care. 2001;6(1):45-51.
[35]. [13] Kollef MH. Prevention of hospital-associated pneumonia and ventilator-
associated pneumonia. Crit Care Med. 2004;32:1396-405.
[14] Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R, et al.
limitations Epidemiology and outcomes of Ventilator-associated pneumonia in a large US
Among the study limitations, there was the lack of a gold standard database. Chest. 2002;122: 2115-21.
for diagnosis, which may have limited the accuracy of the [15] Mokhless NA, El-Mofty MF, Hanafi NF, Fayed AM, Asser SL. Atypical bacteria in
ventilator associated pneumonia; an Egyptian university hospital experience. J
correlation with the risk factors and outcomes. Also, there was
Am Sci. 2010;6(12):1074-79.
a difficulty in sampling procedures to obtain the microbiological [16] Fischer M, Ruegg S, Czaplinski A, Strohmeier M, LehmannA, Tschan F, et al.
specimens from the small respiratory tract of children. Invasive Inter-rater reliability of the full outline of Unresponsiveness score and the Glasgow
techniques to differentiate between infection and colonization Coma Scale in critically ill patients: a prospective observational study. Crit Care.
2010;14:R64.
such as Broncho Alveolar Lavage (BAL) could not be used as they [17] Ponce-Pone De Leon AL, Romero-Gutierrez G, Valenzuela CA, Gonzalez Bravo
were not practical and could be harmful in small infants. FE. Simplified PRISM III score and outcome in the paediatric intensive care unit.
Paediatr Int. 2005;47(1):80-83. Doi: 1111/j.1442-200x.2004.01997.x.
Conclusion [18] Calandra T, Cohen J. International Sepsis Forum Definition of Infection in
the ICU Consensus Conference. The international sepsis forum consensus
The incidence of VAP in this study was relatively high which conference on definitions of infection in the intensive care unit. Crit Care Med.
necessitates the need for possible improvements in the PICUs. 2005;33(7):153848.
The most prominent risk factors for VAP occurrence were MOSF, [19] Rocha Lde A, Vilela CA, Cezario RC, Almeida AB, GontijoFilho P. Ventilator-
associated pneumonia in an adult clinical-surgical intensive care unit of a Brazilian
prior antibiotic use for >48h before MV, reintubation, coma university hospital: Incidence, risk factors, etiology, and antibiotic resistance. Braz
and age. Late onset VAP was associated with poor prognosis. J Infect Dis. 2008;12(1):80-85. Doi: 10.1590/S1413-86702008000/00017.
Awareness about the different risk factors will help in reducing VAP [20] Khattab AA, El-Lahony DM, Fathy W. Ventilator associated pneumonia in a
neonatal intensive care unit. J Am Sci. 2013;9(11):251-58.
morbidity and mortality. Therefore, we recommend proper use of
[21] Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Kanus WA, et al. Definitions
antibiotics before MV in PICUs to avoid the development of drug- for sepsis and organ failure and guidelines for the use of innovative therapies
resistant pathogens. Also, adequate training of nurses and strict in sepsis. The ACCP/SCCM Consensus Conference Committee. American
supervision of infection control protocols are crucial. Measures College of chest physicians/ Society of Critical Care Medicine, 1992. Chest.
2009;136:28.
to prevent aspiration resulting from reintubation are needed e.g. [22] Carlson VR, Boyd KM, Webb DJ. The revision of the Declaration of Helsinki:
continuous subglottic suctioning. Further studies are warranted to past, present and future. Br J Clin Pharmacol. 2004;57(6). Doi: 10.1111/j.1365-
evaluate the effect of these interventions in reducing VAP incidence 2125.2004.02103.x.
[23] Arora SC, Mudaliar YM, Lee C, Mitchell D, Iredell J, Lazarus R. Non-bronchoscopic
in children.
broncho alveolar lavage in the microbiological diagnosis of pneumonia in mechanically
ventilated patients. Anaesth Intensive Care Med. 2002;30(1):11-20.
Acknowledgments [24] Epps B, Edwards JR, Sohn AH, Horan TC, Gaynes RP. Improving benchmarks
The authors are thankful to the Chairman of the PICUs and Clinical for surveillance by defining types of paediatric intensive care units. Am J Infect
Control. 2002;30:68-70.
Pathology Departments at Cairo University Hospitals for conducting [25] Rosenthal VD, Jarvis WR, Jamulitrat S, Silva CP, Ramachandran B, Duenas L, et
this study. The authors also thank all the nursing staff in the PICUs al. Socioeconomic impact on device-associated infections in paediatric intensive
who helped the researchers during the data collection process. care units of 16 limited-resource countries: international Nosocomial Infection
Control Consortium findings. PaediatrCrit Care Med. 2012;13:339-406.
The research team also thanks all the patient's relatives.
[26] Almuneef M, Memish ZA, Balkhy HH, Alalem H, Abutaleb A. Ventilator-associated
pneumonia in a paediatric intensive care unit in Saudi Arabia: a 30-month
References prospective surveillance. Infect Control Hosp Epidemiol. 2004;25(9):753-58. Doi:
[1] Liu B, Li SQ, Zhang SM, Xu P, Zhang X, Zhang YH, et al. Risk factors of ventilator- 10.1086/502472.
associated pneumonia in a paediatric intensive care unit: a systematic review [27] Patria MF, Chidini G, Ughi L, Montani C, Prandi E, Galeone C, et al. Ventilator-
and meta-analysis. J Thorac Dis. 2013; 5(4):525-31. Doi: 10.3978/j.issn.2072- associated pneumonia in an Italian paediatric intensive care unit: a prospective
1439.2013.08.31. study. World J Paediatr. 2013;9(4):365-68. Doi: 10.1007/s12519-013-0444-y.
10 Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11
www.jcdr.net Yasmine S. Galal et al., Ventilator-associated Pneumonia in Pediatric Intensive Care Units
[28] Gautam A, Ganu SS, Tegg OJ, Andresen DN, Wilkins BH, Schell DN. Ventilator- [34] Bonten MJ, Weinstein RA. Infection control in intensive care units and prevention
associated pneumonia in a tertiary paediatric intensive care unit: a 1-year of ventilator-associated pneumonia. Semin Respir Infect. 2000;15:327-35.
prospective observational study. Crit Care Resusc. 2012;14(4):283-89. [35] Chiru D, Craciun A, Tepeneu NF, Sipos C, Bizerea T, Grecu A, et al. Incidence,
[29] OBrien JE, Iovanna D, Dumas HM, Burke S, Maher A, Ladenheim B. Ventilator- risk factors, and nosocomial germs for ventilator-associated pneumonia in
associated pneumonia and paediatric post-acute care. J Clin Outcomes Manage. children. Jurnalul Paediatrului. 2013;16(64):3-6.
2013;20(6):256-62. [36] Bonten MJ, Kollef MH, Hall JB. Risk factors for ventilator-associated pneumonia:
[30] Aelami MH, Lotfi M, Zingg W. Ventilator-associated pneumonia in neonates, infants from epidemiology to patient management. Clin Infect Dis. 2004;38(8):1141-49.
and children. Antimicrob Resist Infect Control. 2014;3:30. Doi: 10.1186/2047- Doi: 10.1086/383039.
2994-3-30. [37] Smulders K, van der HH, Weers-Pothoff I, Vandenbroucke-Grauls C. A
[31] Roeleveld PP, Guijt D, Kuijper EJ, Hazekamp MG, de Wilde RBP, de Jonge randomized clinical trial of intermittent subglottic secretion drainage in patients
E. Ventilator-associated pneumonia in children after cardiac surgery in the receiving mechanical ventilation. Chest. 2002;121:858-62.
Netherlands. Intensive Care Med. 2011;37:1656-63. Doi: 10.1007/s00134-011- [38] Ramya S, Jeanette A, Ginny G, Wiener-Kronish J, Flori HR. A prospective study
2349-43. of ventilator-associated pneumonia in children. Paediatrics. 2009;123:1108-15.
[32] Awasthi S, Tahazzul M, Ambast A, Govil YC, Jain A. Longer duration of mechanical [39] Alexis ME, David KW, Victoria JF. Ventilator-associated pneumonia in
ventilation was found to be associated with ventilator-associated pneumonia in paediatric intensive care unit patients: risk factors and outcomes. Paediatrics.
children aged 1 month to 12 years in India. J Clin Epidemiol. 2013;66(1):62-66. 2002;109:758-64.
Doi: 10.1016/j. jclinepi.2012.06.006. [40] Huang WY, Lee MS, Lee CH, Tsao LY, Chiu HY. Risk factors and outcomes of
[33] Bauer TT, Ferrer R, Angrill J, Schultze-Werninghaus G, Torres A. Ventilator- ventilator-associated pneumonia in children without pneumonia on admission. J
associated pneumonia: incidence, risk factors, and microbiology. Semin Respir Paediatr Resp Dis. 2012;8:78-84.
Infect. 2000;15:272-79.
PARTICULARS OF CONTRIBUTORS:
1. Faculty of Medicine, Departments of Public Health and Community Medicine, Cairo University, Egypt.
2. Faculty of Medicine, Departments of Pediatrics, Cairo University, Egypt.
3. Faculty of Medicine, Departments of Pediatrics, Cairo University, Egypt.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Meray Rene Labib. Youssef,
Date of Submission: Dec 31, 2015
Faculty of Medicine, Departments of Pediatrics, Cairo University, Egypt.
E-mail: anargislabib@yahoo.com Date of Peer Review: Jan 14, 2016
Date of Acceptance: Feb 05, 2016
Financial OR OTHER COMPETING INTERESTS: None. Date of Publishing: Jun 01, 2016
Journal of Clinical and Diagnostic Research. 2016 Jun, Vol-10(6): SC06-SC11 11
You might also like
- NCP On Preterm LaborDocument2 pagesNCP On Preterm Laborinah krizia lagueNo ratings yet
- VAP in ICU ReviewDocument8 pagesVAP in ICU ReviewAdam KurniaNo ratings yet
- Neonatal PneumoniaDocument8 pagesNeonatal PneumoniaAde Gustina SiahaanNo ratings yet
- Impact Vap Bundle 2017Document6 pagesImpact Vap Bundle 2017Elisya KharuniawatiNo ratings yet
- Criteria of ProfessionDocument5 pagesCriteria of Professionmadhurima kundu55% (11)
- Pneumonia Nosokomial Pedoman Diagnosis Dan Penatalaksanaan Di IndonesiaDocument17 pagesPneumonia Nosokomial Pedoman Diagnosis Dan Penatalaksanaan Di IndonesiaOkta Adinanto P100% (1)
- Nursing Care Plan-1idealDocument30 pagesNursing Care Plan-1idealSheila Mae PanisNo ratings yet
- Mobilisasi Dan Fisioterapi-Vap PDFDocument9 pagesMobilisasi Dan Fisioterapi-Vap PDFYANNo ratings yet
- School Shootings EssayDocument3 pagesSchool Shootings Essayapi-2848250550% (2)
- Ventilator-Associated Pneumonia in Paediatric InteDocument7 pagesVentilator-Associated Pneumonia in Paediatric InteDr tahera noorNo ratings yet
- Ventilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreDocument5 pagesVentilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreJoaquín SosaNo ratings yet
- The Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimDocument3 pagesThe Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimAquardoleo ValentinoNo ratings yet
- Insiden dan Risk Faktor VAP 2013Document5 pagesInsiden dan Risk Faktor VAP 2013Yudi Jaya CahyanaNo ratings yet
- 3 DC 3Document8 pages3 DC 3astutikNo ratings yet
- Epidemiology of ICU Acqired PnemoniaDocument7 pagesEpidemiology of ICU Acqired PnemoniaRicardo ZúñigaNo ratings yet
- Hospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionDocument7 pagesHospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionadhitiaNo ratings yet
- Minor Diagnostic Factors in Ventilator Associated Pneumonia in ChildrenDocument9 pagesMinor Diagnostic Factors in Ventilator Associated Pneumonia in ChildrenmariskaNo ratings yet
- Acinetobacter Baumannii in Ventilator-Associated PneumoniaDocument8 pagesAcinetobacter Baumannii in Ventilator-Associated PneumoniaMahmoudAboAlSamenNo ratings yet
- outDocument8 pagesoutAnjar EnggoNo ratings yet
- Antimicrobial Susceptibility Among Pathogens Isolated in Early-Versus Late-Onset Ventilator-Associated PneumoniaDocument10 pagesAntimicrobial Susceptibility Among Pathogens Isolated in Early-Versus Late-Onset Ventilator-Associated PneumoniaJeremy CNo ratings yet
- New Paradigm for VAP in Critically Ill ChildrenDocument18 pagesNew Paradigm for VAP in Critically Ill ChildrenAndry Wahyudi AgusNo ratings yet
- Ventilator AssociatedDocument10 pagesVentilator Associatedtoothfairy2780No ratings yet
- VAP Reviw XDocument19 pagesVAP Reviw XCroitoru CosminNo ratings yet
- Ventilator-Associated Pneumonia in Adults in Developing Countries: A Systematic ReviewDocument8 pagesVentilator-Associated Pneumonia in Adults in Developing Countries: A Systematic Reviewfrisca susdiNo ratings yet
- Ventilator Associated Pneumonia in ChildrenDocument7 pagesVentilator Associated Pneumonia in ChildrendarlingcarvajalduqueNo ratings yet
- VAP Incidence, Risk Factors and Bacteria in PICUDocument6 pagesVAP Incidence, Risk Factors and Bacteria in PICURabiatul 'raney' AdawiyahNo ratings yet
- The Clinical Impact and Preventability of Ventilator-Associated Conditions in Critically Ill Patients Who Are Mechanically Ventilated - Muscedere2013Document8 pagesThe Clinical Impact and Preventability of Ventilator-Associated Conditions in Critically Ill Patients Who Are Mechanically Ventilated - Muscedere2013Maxi BoniniNo ratings yet
- COVID Plasma ConvalescenteDocument11 pagesCOVID Plasma ConvalescenteBreno Bertozo SilvaNo ratings yet
- Incidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorDocument6 pagesIncidence and Risk Factors For Ventilator Associated Pneumon 2007 RespiratorTomasNo ratings yet
- Diagnosing and Treating Hospital-Acquired PneumoniaDocument7 pagesDiagnosing and Treating Hospital-Acquired PneumoniatinatobingNo ratings yet
- Accuracy of The Clinical Pulmonary Infection Score To Differentiate Ventilator-Associated Tracheobronchitis From Ventilator-Associated PneumoniaDocument10 pagesAccuracy of The Clinical Pulmonary Infection Score To Differentiate Ventilator-Associated Tracheobronchitis From Ventilator-Associated PneumoniaOkki KardianNo ratings yet
- Combes 2007Document9 pagesCombes 2007RaffaharianggaraNo ratings yet
- Hospital-Acquired andDocument7 pagesHospital-Acquired andadhitiaNo ratings yet
- Risk Factors For Ventilator-Associated Events - Liu 2019Document6 pagesRisk Factors For Ventilator-Associated Events - Liu 2019Maxi BoniniNo ratings yet
- IndianJMedRes1396814-2632712 071847Document8 pagesIndianJMedRes1396814-2632712 071847christian hansNo ratings yet
- Jurnal Kritis ICU Bundle Vap PneumoniaDocument6 pagesJurnal Kritis ICU Bundle Vap PneumoniaAdzkia PintaNo ratings yet
- 990 Full PDFDocument18 pages990 Full PDFAkbar Adrian RamadhanNo ratings yet
- New Guidelines For NeumoniaDocument7 pagesNew Guidelines For NeumoniacarlosNo ratings yet
- Risk Factors of Ventilator-Associated Pneumonia in Critically III PatientsDocument7 pagesRisk Factors of Ventilator-Associated Pneumonia in Critically III PatientsGladysNo ratings yet
- antibiotics-10-00608Document10 pagesantibiotics-10-00608Marketable StudioNo ratings yet
- Cambridge University Press, The Society For Healthcare Epidemiology of America Infection Control and Hospital EpidemiologyDocument23 pagesCambridge University Press, The Society For Healthcare Epidemiology of America Infection Control and Hospital EpidemiologyChaesar Abdil BarNo ratings yet
- Epidemiology of ICU-Acquired Pneumonia Review 2018Document9 pagesEpidemiology of ICU-Acquired Pneumonia Review 2018Andhika Marthsyal PratamaNo ratings yet
- BJSTR MS Id 006919Document22 pagesBJSTR MS Id 006919Anz JoyNo ratings yet
- Risk Factors For Healthcare-Associated Infection Caused by Carbapenem-Resistant Pseudomonas AeruginosaDocument8 pagesRisk Factors For Healthcare-Associated Infection Caused by Carbapenem-Resistant Pseudomonas AeruginosaUjjwal kumarNo ratings yet
- Hospital-Acquired Infection in Public Hospital Buildings in The Philippines: Is The Type of Ventilation Increasing The Risk?Document7 pagesHospital-Acquired Infection in Public Hospital Buildings in The Philippines: Is The Type of Ventilation Increasing The Risk?Khim Joshua MagtibayNo ratings yet
- A Study On Ventilator Associated Pneumonia inDocument4 pagesA Study On Ventilator Associated Pneumonia inAl MuzakkiNo ratings yet
- Strategies To Prevent Ventilator-Associated Pneumonia in Acute Care Hospitals: 2014 UpdateDocument22 pagesStrategies To Prevent Ventilator-Associated Pneumonia in Acute Care Hospitals: 2014 UpdatePPINo ratings yet
- البحث السادس PDFDocument32 pagesالبحث السادس PDFايمان عمرانNo ratings yet
- The University of Chicago Press The Society For Healthcare Epidemiology of AmericaDocument11 pagesThe University of Chicago Press The Society For Healthcare Epidemiology of Americaزينب محمد عبدNo ratings yet
- Aerosolized Antibiotics and Ventilator-Associated Tracheobronchitis in The Intensive Care UnitDocument6 pagesAerosolized Antibiotics and Ventilator-Associated Tracheobronchitis in The Intensive Care UnitMASIEL AMELIA BARRANTES ARCENo ratings yet
- The Clinical Impact of Ventilator-Associated Events - Zhu2015Document8 pagesThe Clinical Impact of Ventilator-Associated Events - Zhu2015Maxi BoniniNo ratings yet
- Multiplex PCR Severe PneumoniaDocument13 pagesMultiplex PCR Severe PneumoniaSrinivas PingaliNo ratings yet
- Hunter - VAP - Postgrad Med J-2006 (Bakteri Penyebab VAP Terbanyak)Document8 pagesHunter - VAP - Postgrad Med J-2006 (Bakteri Penyebab VAP Terbanyak)Irfany Nurul HamidNo ratings yet
- Outcome of Ventilator-Associated Pneumonia: Impact of Antibiotic Therapy and Other FactorsDocument6 pagesOutcome of Ventilator-Associated Pneumonia: Impact of Antibiotic Therapy and Other FactorsAnonymous r3ql4y9No ratings yet
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoNo ratings yet
- Shea Vap 2014Document22 pagesShea Vap 2014Sally Mohy El-DinNo ratings yet
- Sépsis em Pacientes Neurovascular Focus On Infection and Sepsis in Intensive Care PatientsDocument3 pagesSépsis em Pacientes Neurovascular Focus On Infection and Sepsis in Intensive Care PatientsEdson MarquesNo ratings yet
- Comparison of Viral Infection in Healthcare-Associated Pneumonia (HCAP) and Community-Acquired Pneumonia (CAP)Document16 pagesComparison of Viral Infection in Healthcare-Associated Pneumonia (HCAP) and Community-Acquired Pneumonia (CAP)MutianbllNo ratings yet
- Characteristics and Treatment of Hospitalized Pregnant Women With COVID-19Document11 pagesCharacteristics and Treatment of Hospitalized Pregnant Women With COVID-19Diana MontoyaNo ratings yet
- Zapalenie Pluc EN 15-20Document6 pagesZapalenie Pluc EN 15-20endahNo ratings yet
- Alaiyan 2017Document5 pagesAlaiyan 2017adiNo ratings yet
- En 13Document8 pagesEn 13Bruna CarvalhoNo ratings yet
- Sepsis in Icu GreeceDocument9 pagesSepsis in Icu GreeceChrysiida DelimitrouNo ratings yet
- Comparison of Methicillin-Resistant Community-Acquired and Healthcare-Associated PneumoniaDocument8 pagesComparison of Methicillin-Resistant Community-Acquired and Healthcare-Associated PneumoniaSuarniNo ratings yet
- Effect of Nurses Training on VAP Prevention BundleDocument7 pagesEffect of Nurses Training on VAP Prevention BundlemochkurniawanNo ratings yet
- Living on the Frontline of COVID-19 in MCO And CMCOFrom EverandLiving on the Frontline of COVID-19 in MCO And CMCONo ratings yet
- References 1Document3 pagesReferences 1YANNo ratings yet
- Ips ViiDocument1 pageIps ViiYANNo ratings yet
- No Mode T FIO TV IPL Peep RR I:E 1 VC 2 PC 3 Simv 4 Simv+Ps 5 PS 6 CpapDocument1 pageNo Mode T FIO TV IPL Peep RR I:E 1 VC 2 PC 3 Simv 4 Simv+Ps 5 PS 6 CpapYANNo ratings yet
- Patient Safety Environment: Perception of Health Care Professionals Dora Maria Ricardo Fonseca Saraiva & Anabela Antunes de AlmeidaDocument8 pagesPatient Safety Environment: Perception of Health Care Professionals Dora Maria Ricardo Fonseca Saraiva & Anabela Antunes de AlmeidaYANNo ratings yet
- Safe Di ICUDocument1 pageSafe Di ICUYANNo ratings yet
- Emergency Department Navigator Role: 1. Key FunctionsDocument3 pagesEmergency Department Navigator Role: 1. Key FunctionsYANNo ratings yet
- Literature ReviewDocument4 pagesLiterature ReviewDeepa SaxenaNo ratings yet
- Safe Di ICUDocument1 pageSafe Di ICUYANNo ratings yet
- Adverse Events in Skilled NursingDocument101 pagesAdverse Events in Skilled NursingYANNo ratings yet
- LS 1134 Rev A Early Mobility and Walking Program PDFDocument10 pagesLS 1134 Rev A Early Mobility and Walking Program PDFYANNo ratings yet
- From: Effectiveness of Acute Medical Units in Hospitals: A Systematic ReviewDocument1 pageFrom: Effectiveness of Acute Medical Units in Hospitals: A Systematic ReviewYANNo ratings yet
- Making Health Care Safer.2Document9 pagesMaking Health Care Safer.2YANNo ratings yet
- BH09Document22 pagesBH09YANNo ratings yet
- Pelod ScoreDocument7 pagesPelod ScoreAgus SarjonoNo ratings yet
- Early Mobilization in The Intensive Care UnitDocument10 pagesEarly Mobilization in The Intensive Care UnitYANNo ratings yet
- Emergency 1Document14 pagesEmergency 1YANNo ratings yet
- IncidenceDocument7 pagesIncidenceYANNo ratings yet
- Mobilisasi Dini Pasien Kritis 3Document12 pagesMobilisasi Dini Pasien Kritis 3YANNo ratings yet
- ICU study finds high mortality from ventilator pneumoniaDocument4 pagesICU study finds high mortality from ventilator pneumoniaYANNo ratings yet
- CPT in VAPDocument7 pagesCPT in VAPLisa Im The Queen Of Universe KoNo ratings yet
- VAP Tagged PDFDocument1 pageVAP Tagged PDFYANNo ratings yet
- IncidenceDocument7 pagesIncidenceYANNo ratings yet
- 466 400 1 SMDocument8 pages466 400 1 SMYANNo ratings yet
- ICU study finds high mortality from ventilator pneumoniaDocument4 pagesICU study finds high mortality from ventilator pneumoniaYANNo ratings yet
- Chest P 1Document8 pagesChest P 1YANNo ratings yet
- Mobilisasi Dini Pasien Kritis 6 PDFDocument11 pagesMobilisasi Dini Pasien Kritis 6 PDFYANNo ratings yet
- 1 s2.0 S0195670113003824 MainDocument10 pages1 s2.0 S0195670113003824 MainYANNo ratings yet
- Family Counselling Enhances Environmental Control of Allergic PatientsDocument6 pagesFamily Counselling Enhances Environmental Control of Allergic PatientsNinuk KurniawatiNo ratings yet
- Hubungan Pemberian Obat Terhadap HB, Zat Besi ProteinDocument10 pagesHubungan Pemberian Obat Terhadap HB, Zat Besi ProteinFanny Aulia PratamaNo ratings yet
- Student's PortfolioDocument6 pagesStudent's PortfolioApril Joy de LimaNo ratings yet
- Science4 - Q2 - Mod2 - Causes and Treatment of Diseases of The Major Organs - Version3Document50 pagesScience4 - Q2 - Mod2 - Causes and Treatment of Diseases of The Major Organs - Version3Liezel BinsolNo ratings yet
- Right Brain, Left BrainDocument2 pagesRight Brain, Left BrainCamelia TuguiNo ratings yet
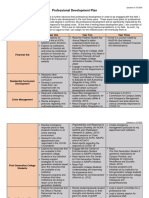
- Professional Development PlanDocument5 pagesProfessional Development Planapi-506915607No ratings yet
- Covid19 PPT Template-GryffindorDocument32 pagesCovid19 PPT Template-GryffindorAngelika NievaNo ratings yet
- Shell Advance 4T Ultra 10W-40Document2 pagesShell Advance 4T Ultra 10W-40Anonymous oAbjbl4HNo ratings yet
- Gender Differences in Exercise Habits and Quality of Life Reports - Assessing The Moderating Effects of Reasons For ExerciseDocument15 pagesGender Differences in Exercise Habits and Quality of Life Reports - Assessing The Moderating Effects of Reasons For ExerciseArischo MardiansyahNo ratings yet
- Assignment # 01: Morton's NeuromaDocument5 pagesAssignment # 01: Morton's Neuromazoha hassanNo ratings yet
- Siemens Mammomat Nova 3000 ProspektDocument8 pagesSiemens Mammomat Nova 3000 Prospektbancodesangre688No ratings yet
- Elder Justice Roadmap SnapshotDocument3 pagesElder Justice Roadmap SnapshotWGMENo ratings yet
- Strategic Management CIA - 3: Assignment On Company AnalysisDocument8 pagesStrategic Management CIA - 3: Assignment On Company AnalysisThanish Sujaudeen 2027716100% (1)
- Disaster Preparedness in the Philippines: Local Governance and Policy EvaluationDocument18 pagesDisaster Preparedness in the Philippines: Local Governance and Policy EvaluationCamille SantosNo ratings yet
- MSDS STOPRUST - NewDocument2 pagesMSDS STOPRUST - NewAnurag JainNo ratings yet
- DLL - Heath and Safety Protocols S.Y. 2023 2024Document2 pagesDLL - Heath and Safety Protocols S.Y. 2023 2024ETHELVNo ratings yet
- Drug Education 2Document11 pagesDrug Education 2Erick Tesoro AgarcioNo ratings yet
- Alcholism ResearchDocument68 pagesAlcholism ResearchYasith WeerasingheNo ratings yet
- Healthy EatingDocument6 pagesHealthy EatingGabriela Elena StanciuNo ratings yet
- Martinplus Silo Solutions: Storage Vessel Cleaning Service and ProductsDocument8 pagesMartinplus Silo Solutions: Storage Vessel Cleaning Service and ProductstacosanchezbrayanNo ratings yet
- What Is Post-Acute Withdrawal Syndrome (PAWS) ?Document2 pagesWhat Is Post-Acute Withdrawal Syndrome (PAWS) ?DeAn WhiteNo ratings yet
- Social Stratification ApproachesDocument12 pagesSocial Stratification ApproachesEdgar PeninsulaNo ratings yet
- Pengaruh Pemberian Buah Pepaya Terhadap Nafsu Makan Anak Berumur 2-5 Tahun Di Wilayah Kerja Puskesmas KuranjiDocument16 pagesPengaruh Pemberian Buah Pepaya Terhadap Nafsu Makan Anak Berumur 2-5 Tahun Di Wilayah Kerja Puskesmas KuranjiRiza IrmasariNo ratings yet
- DopamineDocument4 pagesDopamineHassan KhiljiNo ratings yet
- Oligodontia Case Report and Review of LiteratureDocument2 pagesOligodontia Case Report and Review of LiteratureWindaNo ratings yet
- Abnormality data analysis and clinical questionsDocument2 pagesAbnormality data analysis and clinical questionsHeldasari SianturiNo ratings yet