Professional Documents
Culture Documents
Trophoblast To Placenta EOR 163163 284 18220
Uploaded by
Fellita Ratri AOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Trophoblast To Placenta EOR 163163 284 18220
Uploaded by
Fellita Ratri ACopyright:
Available Formats
From Trophoblast to Human Placenta
(from The Encyclopedia of Reproduction)
Harvey J. Kliman, M.D., Ph.D.
Yale University School of Medicine
I. Introduction
II. Formation of the placenta
III. Structure and function of the placenta
IV. Complications of pregnancy related to trophoblasts and the placenta
Glossary
amnion the inner layer of the external membranes in direct contact with the
amnionic fluid.
chorion the outer layer of the external membranes composed of trophoblasts and
extracellular matrix in direct contact with the uterus.
chorionic plate the connective tissue that separates the amnionic fluid from the maternal
blood on the fetal surface of the placenta.
chorionic villous the final ramification of the fetal circulation within the placenta.
cytotrophoblast a mononuclear cell which is the precursor cell of all other trophoblasts.
decidua the transformed endometrium of pregnancy
intervillous space the space in between the chorionic villi where the maternal blood
circulates within the placenta
invasive trophoblast the population of trophoblasts that leave the placenta, infiltrates the
endo– and myometrium and penetrates the maternal spiral arteries,
transforming them into low capacitance blood channels.
Sunday, October 29, 2006 Page 1 of 19
From Trophoblasts to Human Placenta Harvey Kliman
junctional trophoblast the specialized trophoblast that keep the placenta and external
membranes attached to the uterus.
spiral arteries the maternal arteries that travel through the myo– and endometrium
which deliver blood to the placenta.
syncytiotrophoblast the multinucleated trophoblast that forms the outer layer of the chorionic
villi responsible for nutrient exchange and hormone production.
I. Introduction
The precursor cells of the human placenta—the trophoblasts—first appear four days after
fertilization as the outer layer of cells of the blastocyst. These early blastocyst trophoblasts
differentiate into all the other cell types found in the human placenta. When fully developed, the
placenta serves as the interface between the mother and the developing fetus. The placental
trophoblasts are critical for a successful pregnancy by mediating such critical steps as
implantation, pregnancy hormone production, immune protection of the fetus, increase in
maternal vascular blood flow into the placenta, and delivery.
II. Formation of the placenta
As early as three days after fertilization, the trophoblasts—the major cell type of the
placenta—begin to make human chorionic gonadotropin (hCG), a hormone which insures that
the endometrium will be receptive to the implanting embryo. Over the next few days, these same
trophoblasts attach to and invade into the uterine lining, beginning the process of pregnancy
(Figure 1). Over the next few weeks the placenta begins to make hormones which control the
basic physiology of the mother in such a way that the fetus is supplied with the necessary
nutrients and oxygen needed for successful growth. The placenta also protects the fetus from
immune attack by the mother, removes waste products from the fetus, induces the mother to
bring more blood to the placenta, and near the time of delivery, produces hormones that matures
the fetal organs in preparation for life outside of the uterus.
Sunday, October 29, 2006 Page 2 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 1. From ovulation to implantation. Ovulation occurs around day 14 of the menstrual cycle,
followed by fertilization within 24 hours. The first three days of development occur within the fallopian
tube. Upon arrival within the uterus the conceptus has developed into a blastocyst (see figure 2) and has
already begun to make mRNA for human chorionic gonadotropin, the first hormone signal from the early
embryo. By day 6 after fertilization the blastocyst has initiated implantation into the maternal
endometrium. (Modified from Sadler TW, Langman’s Medical Embryology, 5th edition, Williams &
Wilkins, 1985, with permission.)
A. Early Development
Within a few days of fertilization the embryo develops into a blastocyst, a spherical structure
composed on the outside of trophoblasts and on the inside of a group of cells called the inner cell
mass (Figure 2). The inner cell mass will develop into the fetus and ultimately, the baby. In
addition to making hCG, the trophoblasts mediate the implantation process by attaching to, and
eventually invading into the endometrium (Figure 3).
Sunday, October 29, 2006 Page 3 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 2. Blastocyst. By 4-5 days after fertilization
the embryo has differentiated into two distinct cell
types: inner cell mass (lighter cells)—which will
develop into the fetus and eventually become the
newborn and trophoblasts (darker cells)—which
will develop into the placenta and external
membranes. Even by this stage the trophoblasts
have begun to make their hallmark hormone:
human chorionic gonadotropin (hCG)—the
hormone of pregnancy-test fame. (Modified from
Sadler TW, Langman’s Medical Embryology, 5th
edition, Williams & Wilkins, 1985, with
permission.)
Figure 3. Implantation. The most difficult hurdle for
the floating blastocyst is to become attached to the
uterine lining (endometrium). Like trying to dock a
tanker coming into port, the blastocyst is first slowed
down by long molecules that extend from the
endometrium (mucins), followed by a cascade of
molecules that bring the trophoblasts into closer and
closer contact with the endometrium. Once intimate
contact is made the trophoblasts begin to invade into
the endometrium, beginning the process of
placentation. (Modified from Sadler TW, Langman’s
Medical Embryology, 5th edition, Williams & Wilkins,
1985, with permission.)
Implantation is regulated by a complex interplay between trophoblasts and endometrium. On
the one hand trophoblasts have a potent invasive capacity and if allowed to invade unchecked,
would spread throughout the uterus. The endometrium, on the other hand, controls trophoblast
invasion by secreting locally acting factors (cytokines and protease inhibitors), which modulate
Sunday, October 29, 2006 Page 4 of 19
From Trophoblasts to Human Placenta Harvey Kliman
trophoblast invasion. Ultimately, normal implantation and placentation is a balance between
regulatory gradients created by both the trophoblasts and endometrium (Figure 4).
Figure 4. Regulation of trophoblast invasion by
hCG
gradient
an hCG gradient. Within the placenta the
hCG
hCG
syncytiotrophoblasts generate high levels of hCG
which shifts cytotrophoblast differentiation towards
hCG, EGF
a non-invasive hormone secreting villous-type
GnRH, Activin,
TGFα, Inhibin
trophoblast. The closer the trophoblasts are to the
EGF hCG
endometrium the less hCG is made, allowing the
trophoblasts to differentiate into anchoring type
TUN cells which make the placental glue protein
TGFß
trophouteronectin. Trophoblasts that leave the
LIF TGFß placenta and migrate within the endo and
myometrium are induced to make proteases and
Urokinase PAI-1
Collagenases TIMP protease inhibitors, presumably to facilitate
LRP
trophoblast invasion into the maternal tissues.
CSF-1
B. Formation of the early placenta
Once firmly attached to the endometrium the developing conceptus grows and continues to
expand into the endometrium. One of the basic paradigms which is established even within the
first week of gestation is that the embryonic/fetal cells are always separated from maternal
tissues and blood by a layer of cytotrophoblasts (mononuclear trophoblasts) and
syncytiotrophoblasts (multinucleated trophoblasts) (Figure 5). This is critical not only for
nutrient exchange, but to protect the developing fetus from maternal immunologic attack.
Sunday, October 29, 2006 Page 5 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 5. Day 9 implantation site. By nine days the
embryo is surrounded by two layers of trophoblasts: the
inner mononuclear cytotrophoblasts and the outer
multinucleated syncytiotrophoblast layer. This
arrangement of embryo, trophoblasts and maternal
tissue remains the paradigm throughout gestation. This
trophoblast interface not only serves as the means to
extract nutrients from the mother, but protects the
embryo and fetus from maternal immunologic attack.
(Modified from Sadler TW, Langman’s Medical
Embryology, 5th edition, Williams & Wilkins, 1985,
with permission.)
Within the first 2 weeks of development, the invading front of trophoblasts has penetrated the
endometrial blood vessels, forming intertrophoblastic maternal blood filled sinuses (Figure 6).
The trophoblastic shell continues to grow and develop until by 3 weeks after fertilization the
earliest evidence of fetal circulation can be identified, and with that, the earliest evidence of the
chorionic villi formation (Figure 7).
Figure 6. Day 12 implantation site. The invading
trophoblasts have penetrated the maternal vessels,
forming pools of maternal blood which surround
the growing trophoblasts. (Modified from Sadler
TW, Langman’s Medical Embryology, 5th edition,
Williams & Wilkins, 1985, with permission.)
Sunday, October 29, 2006 Page 6 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 7. 3 weeks implantation site. Still barely
perceptible to the naked eye, the embryo has
already begun to make an early circulatory system.
Again, embryonic tissue and maternal blood are
separated by a layer of cytotrophoblasts and
syncytiotrophoblasts. (Modified from Sadler TW,
Langman’s Medical Embryology, 5th edition,
Williams & Wilkins, 1985, with permission.)
In spite of the fact that the entire conceptus is less than 2 cm in diameter at four weeks, the
basic structure of the mature placenta has been laid out: a fetal circulation that terminates in
capillary loops within chorionic villi which penetrate a maternal blood-filled intervillous space
which is supplied by spiral arteries and drained by uterine veins (Figure 8).
Figure 8. 4 weeks implantation site. The basic
structure of the placenta has been formed with
maternal blood being delivered to the forming
placenta via spiral arteries while being drained
away via uterine veins. Like the roots of a tree, the
developing chorionic villi remain immersed in a
space filled with the nutrient rich maternal blood.
(Modified from Sadler TW, Langman’s Medical
Embryology, 5th edition, Williams & Wilkins,
1985, with permission.)
The chorionic villi closest to the maternal blood supply will continue to develop and expand
into a mass of chorionic tissue which we identify as the placenta. The chorionic villi farthest
Sunday, October 29, 2006 Page 7 of 19
From Trophoblasts to Human Placenta Harvey Kliman
away from the maternal blood supply are slowly pushed into the uterine cavity by the expanding
amnionic sac which surrounds the embryo. These villi eventually degenerate and form the
chorionic layer of the external membranes. At around 20 weeks of gestation the combined
amnion–chorion membrane makes contact with the opposite side of the uterus, where it fuses
with the decidualized maternal endometrium, forming the complete external membrane
consisting of amnion, chorion and decidua layers.
III. Structure and function of the placenta
A. Basic structure
The placenta is the fetus’ extension into the mother, where it functions as the interface
between the two. Like the radiator of a car—which is a heat exchanger—the placenta is a
nutrient and waste exchanger. The fetal circulation enters the placenta much like the water of an
automobile engine enters the radiator—via the umbilical arteries embedded within the umbilical
cord. Once in the placenta, the fetal circulation branches into units called cotyledons, structures
similar to inverted trees (Figure 9). The finest branches of the fetal circulation are made up of
capillary loops within the chorionic villi (Figure 10). Once nutrients have been absorbed and
waste products released, the fetal blood ultimately collects into the umbilical vein, where it
returns to the fetus via the umbilical cord.
Figure 9. Maternal and fetal circulations within
the placenta. Maternal blood is fountained into the
placenta through the uterine spiral arteries where it
circulates around the chorionic villi—much like
ocean water circulating around sea anemone. The
fetus pumps blood into the placenta via two
umbilical arteries that branch over the fetal surface
of the placenta. The fetal arteries then dive into the
placental mass, continuously branching until the
blood reaches the capillary loops of the chorionic
villi—much like a branching tree with leaves.
(Modified from Moore KL,The developing human,
Sunday, October 29, 2006 Page 8 of 19
From Trophoblasts to Human Placenta Harvey Kliman
5th edition, WB Saunders, 1993, with permission.)
Figure 10. Terminal chorionic villous. The fetal
circulation branches until it reaches the capillaries
of the chorionic villi (Latin for leaf) where
exchange of nutrients takes place between the
mother and fetus. Like a growing branch, new
villous branches bud off of the larger villi to
increase the mass and exchange surface area of the
placenta. (Modified from Sadler TW, Langman’s
Medical Embryology, 5th edition, Williams &
Wilkins, 1985, with permission.)
If the fetal circulation is analogous to the circulating water in an engine, the maternal
circulation is analogous to the cool air rushing by the fine fins of the radiator. The maternal
blood enters the placenta via the spiral arteries of the uterus. At the point were the spiral arteries
make contact with the placenta, they end in open channels, fountaining maternal blood into the
intervillous space (Figure 9). The intervillous blood is returned to the maternal circulation via
drain-like uterine veins. In order to support the developing fetus, especially at term, up to 35% of
the maternal blood flow courses through the intervillous space.
The finger-like chorionic villi are the main functional units of the placenta (Figure 10)—
mediating nutrient absorption, waste elimination and generating the bulk of the hormones
produced by the placenta during pregnancy. Cross sectioning a chorionic villous reveals the basic
components of this part of the placenta (Figure 11). Towards the end of the first trimester a cross
section of a chorionic villous reveals a central mesenchymal core with embedded fetal capillaries
surrounded by a layer of cytotrophoblasts and syncytiotrophoblasts (Figure 11A). At term a
chorionic villous cross section reveals the same basic structure with some noteworthy differences
(Figure 11B). A term chorionic villous exhibits increased numbers of fetal capillaries, some of
which are very close to the outer edge of the villous to facilitate nutrient exchange. The
syncytiotrophoblast layer, a flat multinucleated cell sheet for most of pregnancy, develops grape-
Sunday, October 29, 2006 Page 9 of 19
From Trophoblasts to Human Placenta Harvey Kliman
like nucleated clusters within its cytoplasm called syncytial knots near term. Although there are
fewer cytotrophoblasts visible at term, they are still present, as they have been throughout
gestation, functioning as the precursor cells for all the other trophoblast types.
Figure 11. Diagrammatic cross sections of first (A) and third (B) trimester chorionic villi. The
villous core of villi from all gestational ages beyond 5 weeks of gestation contains fetal capillaries
embedded in a loose matrix which contains fibroblasts and macrophages (also called Hofbauer cells). In
the first trimester a villous cross section (A) reveals two distinct trophoblast layers, the outer
syncytiotrophoblast layer which is in direct contact with maternal blood and the inner cytotrophoblast
layer, the source of new trophoblasts. A cross section of a third trimester villous still exhibits a distinct
syncytiotrophoblast layer, but fewer cytotrophoblasts can be identified, although they persist throughout
pregnancy. (See also figures 13 and 14). (Modified from Sadler TW, Langman’s Medical Embryology,
5th edition, Williams & Wilkins, 1985, with permission.)
B. Trophoblast differentiation pathways
Concomitant with the overall development of placental architecture is the differentiation of
three distinct trophoblast types. Depending on their subsequent function in vivo, undifferentiated
cytotrophoblasts can develop into 1) hormonally active villous syncytiotrophoblasts, 2)
extravillous anchoring trophoblastic cell columns, or 3) invasive intermediate trophoblasts
(Figure 12). Within the villi of the human placenta—at all gestational ages—there always exists
a population of cytotrophoblasts which remain undifferentiated and available for differentiation
as necessary.
Cytotrophoblast
cAMP Phorbol
hCG Esters
TGFß LIF
Sunday, October 29, 2006 Page 10 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 12. Pathways of trophoblast differentiation. Just as the undifferentiated basal layer of the
skin gives rise to differentiated keratinocytes, the cytotrophoblast—the stem cell of the placenta—gives
rise to the differentiated forms of trophoblasts. Left) Within the chorionic villi, cytotrophoblasts fuse to
form the overlying syncytiotrophoblast. The villous syncytiotrophoblast makes the majority of the
placental hormones, the most studied being hCG. Cyclic AMP and its analogs, and more recently hCG
itself, have been shown to direct cytotrophoblast differentiation towards a hormonally active
syncytiotrophoblast phenotype. Center) At the point where chorionic villi make contact with external
extracellular matrix (decidual stromal ECM in the case of intrauterine pregnancies), a population of
trophoblasts proliferates from the cytotrophoblast layer to form the second type of trophoblast—the
junctional trophoblast. The junctional trophoblasts make a unique fibronectin—trophouteronectin
(TUN)—that appears to mediate the attachment of the placenta to the uterus. TGFß, and more recently,
leukemia inhibitory factor (LIF), have been shown to downregulate hCG synthesis and upregulate TUN
secretion. Right) Finally, a third type of trophoblast differentiates towards an invasive phenotype and
leaves the placenta entirely—the invasive intermediate trophoblast. In addition to making human
placental lactogen, these cells also make urokinase-type plasminogen activator (u-PA) and type 1
plasminogen activator inhibitor (PAI-1). Phorbol esters have been shown to increase trophoblast
invasiveness in in vitro model systems and to upregulate PAI-1 in cultured trophoblasts.
1. Villous syncytiotrophoblast
Within the chorionic villi, cytotrophoblasts fuse to form the overlying syncytiotrophoblast.
The villous syncytiotrophoblast makes the majority of the placental hormones, the most studied
being human chorionic gonadotropin. Human chorionic gonadotropin (hCG) (Figure 13) is
critical to pregnancy since it rescues the corpus luteum from involution, thus maintaining
progesterone secretion by the ovarian granulosa cells. Its usefulness as a diagnostic marker of
pregnancy stems from the fact that it may be one of the earliest secreted product of the
conceptus. Researchers have demonstrated by in situ hybridization that ß-hCG transcripts are
present in human blastocyst trophoblasts prior to implantation. Placental production of hCG
peaks during the tenth to the twelfth week of gestation, and tends to plateau at a lower level for
the remainder of pregnancy.
Sunday, October 29, 2006 Page 11 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 13. Immunohistochemical identification
of hCG in first trimester chorionic villi. The
villous core (V) is covered by two layers of
trophoblasts. The intensely stained
syncytiotrophoblast layer (S) is in direct contact
with the intervillous space (I) which contains the
maternal blood. Underlying the syncytiotrophoblast
layer is a continuous layer of cytotrophoblasts
(arrows), the proliferative cell type of the placenta.
Human placental lactogen (hPL) is a potent glycoprotein made throughout gestation,
increasing progressively until the 36th week, where it can be found in the maternal serum at a
concentration of 5-15 µg/ml, the highest concentration of any known protein hormone. The
major source of hPL appears to be the villous syncytiotrophoblasts, where it is made at a
constant level throughout gestation. In addition to the villous syncytiotrophoblast, hPL has been
identified in invasive trophoblasts during the first trimester. hPL appears to regulate the lipid and
carbohydrate metabolism of the mother (Figure 14). Placental researchers have also
demonstrated by immunohistochemical studies that villous syncytiotrophoblasts contain
prolactin, relaxin and chorionic adrenocorticotropin, an ACTH-like protein. The physiological
role of placental ACTH is unclear, but as with other placental hormones, all of these hormones
may represent a shift from maternal to placental control.
Figure 14. Immunohistochemical identification
of hPL in third trimester chorionic villi. The
villous cores (V) are surrounded by a continuous
layer of syncytiotrophoblasts (*) which are in direct
contact with the intervillous space. Underlying the
syncytiotrophoblasts are scattered cytotrophoblasts
(arrows). Although fewer in number during the
third trimester, cytotrophoblasts are still easily
identified, especially when the overlying syncytium
Sunday, October 29, 2006 Page 12 of 19
From Trophoblasts to Human Placenta Harvey Kliman
is stained so as to highlight the less differentiated,
hormonally negative cytotrophoblasts.
The significance of placental elaboration of progesterone was revealed when it was
demonstrated that bilateral oophorectomy between 7 and 10 weeks of gestation had little impact
on the conceptus or urinary pregnanediol levels. More recently, researchers have been able to
directly demonstrate progesterone secretion by cultured term trophoblasts. The placenta does not
have all the necessary enzymes to make estrogens from cholesterol, or even progesterone.
Human trophoblasts lack 17α-hydroxylase and therefore can not convert C21-steroids to C19-
steroids, the immediate precursors of estrogen. To bypass this deficit, dehydroisandrosterone
sulfate from fetal adrenal is converted to estradiol-17ß by trophoblasts. Not surprisingly,
trophoblasts contain the necessary enzymes to make this conversion, namely sulphatase,
3ß-hydroxysteroid dehydrogenase/∆5→4-isomerase (3ßHSD), and aromatase.
The placenta also appears to produce a number of hypothalamic-pituitary hormones,
including GnRH and CRH. GnRH was first identified within villous cytotrophoblasts by
immunochemical staining of intact placentae. Corticotropin releasing hormone (CRH) is also
made and secreted by cultured trophoblasts and that glucocorticoids stimulate this secretion. In
addition to the hypothalamic factors GnRH and CRH, pituitary growth hormone is synthesized
and secreted by first and third trimester cultured trophoblasts. It appears from these studies that
the placenta, in addition to replacing much of the women’s pituitary function during pregnancy,
also replaces critical hypothalamic functions so as to maintain control and feedback loop
mechanisms close to the conceptus.
2. Anchoring trophoblasts
At the point where chorionic villi make contact with the uterus, a population of trophoblasts
proliferates from the cytotrophoblast layer to form the second type of trophoblast—the junctional
trophoblast. Like the pylons of a bridge that attach to a river bed, these cells form the anchoring
cell columns that can be seen at the junction of the placenta and endometrium throughout
gestation (Figure 15). Similar trophoblasts can be seen at the junction of the chorion layer of the
external membranes and the decidua (Figure 16). The junctional trophoblasts make a unique
fibronectin—trophouteronectin (TUN)—that appears to mediate the attachment of the placenta to
Sunday, October 29, 2006 Page 13 of 19
From Trophoblasts to Human Placenta Harvey Kliman
the uterus. Transforming growth factor beta (TGFß), and more recently, leukemia inhibitory
factor (LIF), have been shown to downregulate hCG synthesis and upregulate TUN secretion.
The premature loss of attachment of the developing conceptus or placenta to the uterus can
terminate the gestation. Therefore, the anchoring trophoblast cell columns and the extracellular
matrix proteins that promote this attachment are critical to the developing pregnancy.
Figure 15. Trophouteronectin (pregnancy glue)
expression by the junctional trophoblasts (T) that
mediate the attachment of the placenta (P) to the
uterus (U).
Figure 16. Trophouteronectin (pregnancy glue)
expression by membrane trophoblasts (T). The
external membranes consist of two layers: amnion
epithelium and its underlying connective tissue (A)
and chorion trophoblasts (C). Where the chorionic
trophoblasts make contact with the maternal
decidua (D), a layer of trophouteronectin can be
identified (T). Amnionic cavity (AC).
3. Invading trophoblasts
Finally, a third type of trophoblast differentiates towards an invasive phenotype and leaves
the placenta entirely—the invasive intermediate trophoblast. Studies using human specimens
three to four weeks after implantation show that as gestation progresses, these invasive
populations of extravillous trophoblasts attach to and interdigitate through the extracellular
spaces of the endo- and myometrium. The endpoint for this invasive behavior is penetration of
maternal spiral arteries within the uterus. Histologically, trophoblast invasion of maternal blood
Sunday, October 29, 2006 Page 14 of 19
From Trophoblasts to Human Placenta Harvey Kliman
vessels results in disruption of extracellular matrix components and development of dilated
capacitance vessels within the uteroplacental vasculature (Figure 17). Biologically, trophoblast-
mediated vascular remodeling within the placental bed allows for marked distensibility of the
uteroplacental vessels, thus accommodating the increased blood flow needed during gestation.
Abnormalities in this invasive process have been correlated with early and mid-trimester
pregnancy loss, preeclampsia and eclampsia, and intrauterine growth retardation.
Figure 17. Invasive trophoblasts. Uterine spiral
artery (V) containing maternal blood (M) from a
four week pregnancy. The maternal endometrium
(D) has become decidualized, meaning that the
stromal cells have been transformed into large, pale
cells (*). Infiltrating between these decidual cells
are the invasive trophoblasts (some examples are
highlighted by arrows) which have begun to
modify the vessel wall (≈).
IV. Complications of pregnancy related to trophoblasts and the placenta
As in any complicated system, problems can arise. It is not possible to discuss all of these
pathologic states of the placenta, but the three most important complications of pregnancy related
to the placenta will be outlined below.
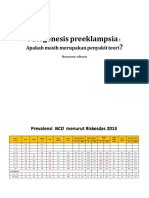
A. Diseases of trophoblast invasion: preeclampsia and gestational trophoblastic neoplasia
Preeclampsia, the clinical state prior to full blown eclampsia (seizures), is one of the
‘toxemias’ of pregnancy. The basic clinical definition is a “pregnancy-specific condition of
increased blood pressure accompanied by proteinuria, edema, or both.” In spite of the simplicity
of this description of these clinical signs and symptoms, the etiology of the disease has remained
elusive. In fact, a seal over the University of Chicago Lying-in-Hospital remains blank awaiting
the name of the person(s) who elucidate the cause of this disease. Many phenomena have been
investigated, but the recurring theme appears to be an abnormally low blood flow into the
Sunday, October 29, 2006 Page 15 of 19
From Trophoblasts to Human Placenta Harvey Kliman
placenta. One of the difficulties has been to distinguish between primary cause and secondary
effects. Part of this difficulty may be attributable to the fact that the common end result of low
uteroplacental blood flow may be caused by many primary defects. Possibly, therefore,
preeclampsia/eclampsia is not a disease, but a syndrome with many causes. Significantly, one of
the most frequent findings in preeclampsia is decreased or absent trophoblast invasion of the
maternal spiral arteries.
Decreased or absent trophoblast invasion may be a consequence of primary defects in the
invasive trophoblasts or in the environment that the trophoblasts are attempting to invade.
Studies have shown that in some cases of preeclampsia there are abnormalities in trophoblast
function, including, but not limited to: integrin expression, glycogen metabolism, and decreased
galactose alpha 1-3 galactose expression. In addition, preeclampsia has been associated with
trisomy 13, the chromosome that carries the gene for type IV collagen. Placental bed biopsy in a
case of preeclampsia in a multiparous woman carrying a trisomy 13 fetus showed lack of
trophoblast invasion of maternal spiral arteries. These trophoblasts may have had difficulty
invading through the maternal ECM because of increased type IV collagen production. In
addition to primary trophoblast defects, many cases of preeclampsia appear to be related to
maternal immunologic reaction against the invading trophoblasts. A common clinical finding in
these cases is that the invasive trophoblasts have reached the vicinity of the spiral arteries, but
have not penetrated them. In addition, the unconverted arteries are often surrounded by
lymphocytes, presumably attacking the foreign-appearing invasive trophoblasts. As can be seen
from a placental bed biopsy in a typical case of preeclampsia, the invasive trophoblasts have
invaded through the endo– and myometrium, but have failed to complete their journey into the
spiral arteries (Fig. 18). Failure to convert the maternal spiral arteries into low-resistance
channels can induce the placenta to secrete vasoactive substances that leads to maternal
hypertension. If the maternal blood pressure rises significantly, the spiral arteries can be
damaged and may even become occluded, leading to placental infarction.
Sunday, October 29, 2006 Page 16 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Figure 18. Failure of invasive trophoblasts to
penetrate the maternal spiral arteries. Normally
the invasive trophoblasts (T) infiltrate through the
endo- and myometrium, reach the spiral arteries (*)
and convert their muscular walls into pliant
channels. In cases of preeclampsia, the trophoblasts
often do not complete the final arterial penetration,
possibly due to the maternal lymphocytes that often
surround the spiral arteries. Compensatory maternal
hypertension can lead to spiral artery damage or
even occlusion. Maternal uterine vein (V).
In contrast to the clinical syndrome of decreased trophoblast invasion, gestational
trophoblastic disease (GTD) represents increased and uncontrolled trophoblast invasion.
Expanded trophoblast invasion ranges from an exaggerated placental site with increased numbers
of benign intermediate trophoblasts, to placental site trophoblastic tumors, to invasive moles, to
frank choriocarcinoma. Morphologic distinction between these forms of trophoblast proliferation
can be difficult, but it appears that the normal mechanisms that stop trophoblast invasion are
defective in choriocarcinoma cell lines. Normal cytotrophoblast differentiation can be shifted
towards a villous syncytiotrophoblast and away from an invasive trophoblast phenotype by
cAMP analogues, while this treatment does not affect choriocarcinoma invasiveness, suggesting
a primary defect in differentiation-signalling in the malignantly invasive trophoblast.
B. Infection
More than a third of all preterm births are associated with labor initiated by acute
chorioamnionitis (inflammatory infiltrates in the chorionic plate and chorion and amnion layers
of the external membranes). Not only does chorioamnionitis have severe consequences for the
fetus through the initiation of preterm delivery, but chorioamnionitis increases the risk for
cerebral palsy by a factor of at least four. Elucidation of the role of cytokines in controlling the
inflammatory process during pregnancy has facilitated the development of diagnostic tests which
Sunday, October 29, 2006 Page 17 of 19
From Trophoblasts to Human Placenta Harvey Kliman
can detect the earliest phases of chorioamnionitis as well as pointing the way towards effective
treatment modalities for this disease process.
The Collaborative Perinatal Study (CPS) of the National Institute of Neurological and
Communicative Disorders and Stroke followed the course of over 56,000 pregnancies in the
United States between 1959 and 1966. In the CPS, more than a third of all preterm births were
associated with labor initiated by acute chorioamnionitis. This study also revealed that acute
chorioamnionitis was the most frequent cause of stillbirth and neonatal death. Chorioamnionitis
does not only have severe consequences for the fetus through the initiation of preterm delivery
but may—through the initiation of the inflammatory cascade in the placenta and decidua—have
direct deleterious effects on the fetus. The CPS showed clearly that acute chorioamnionitis was
followed by a 20% greater-than-expected frequency of neurologic abnormalities at 7 years of
age.
Infections of the amniotic fluid arise by a variety of routes—including from the abdominal
cavity through the fallopian tube, via the maternal blood stream through the placenta, or
iatrogenically following amniocentesis or funipuncture—but the most common route is an
ascending infection through the cervix. It is not surprising, therefore, that the most common
organisms cultured from amnionic fluid are commonly found in the vagina. There are clinical
reports, however, of a wide variety of organisms found to cause intrauterine infections,
including: Group B streptococci, Listeria monocytogenes, Morganella morganii, Ureaplasma
urealyticum, Herpes simplex virus, parvovirus, Chlamydia species, Capnocytophaga, adeno-
associated virus, and human immunodeficiency virus.
Once bacteria enter the amniotic fluid, they quickly multiply. Within 30 hours of the
initiation of the infection, maternal neutrophils begin to be chemoattracted from the maternal
circulation towards the amniotic cavity to fight off the bacterial infection. The extent to which
these maternal neutrophils migrate towards the amniotic fluid has been used to estimate the
severity and timing of intraamniotic infections.
The basic paradigm for inflammation induced cytokine release and leukocytic
chemoattraction has been elucidated in a number of organs, and is being actively studied in the
placenta. Breakdown products of the growing bacteria—especially the lipopolysaccharides (LPS)
of the bacterial cell walls (endotoxin)—appear to play an important role in the initiation of this
process. LPS initiates the inflammatory response by triggering the release of a cascade of
Sunday, October 29, 2006 Page 18 of 19
From Trophoblasts to Human Placenta Harvey Kliman
cytokines from a variety of cell types which mediate the physiological process of inflammation.
Components of this process include the chemotaxis and activation of inflammatory cells—like
the neutrophil—and the leaking of fluid from vascular spaces into the extracellular space—
possibly in response to tumor necrosis factor alpha (TNFα). In experimental models, peak TNFα
production occurs within 1 h of LPS treatment. TNFα then induces the prolonged production of
IL-8, a neutrophil chemoattractant and activator. In addition to chemoattracting leukocytes to the
focus of inflammation, this cytokine cascade—as is succinctly described in Celsus’s first century
phrase rubor, tumor, calor, dolor—also results in swelling due to edema. In the placenta this
swelling is manifested by villous edema—fluid accumulation within the mesenchymal cores of
chorionic villi of the placenta. It has been hypothesized that villous edema makes the fetus
hypoxic by compressing fetal blood vessels inside the villi and by increasing the diffusion barrier
for oxygen between the maternal and fetal circulations (Fig. 19). These effects make villous
edema the most frequent cause of stillbirth, neonatal death and neonatal morbidity, especially
cerebral palsy, in children born before 28 weeks.
Figure 19. Severe villous edema following
induction of intrauterine inflammation. Cross
section of a markedly edematous chorionic villous
16 hours after the initiation of an intrauterine
infection. Note the very pale, fluid filled villous
core (V). The edema fluid has compressed the fetal
vessels (arrows) so severely that only a one or two
erythrocyte cross sections can be seen in each
capillary. Intervillous space (I).
C. Immunologic rejection
In spite of the fact that the placenta and fetus are ‘foreign’ to the mother, most pregnancies
show no evidence of ‘immunologic rejection.’ When immunologic reactions do occur, they can
be against any of the components of the gestation (placenta and fetus). These reactions can occur
at all stages of pregnancy, and can occur repeatedly, pregnancy after pregnancy.
Sunday, October 29, 2006 Page 19 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Examination of hematoxylin and eosin stained histologic sections of placental, abortion or
dilation and curettage material can often reveal evidence of immune damage. However, more
specialized techniques are needed to reveal the specific immune cells involved in these reactions.
Immunohistochemistry of formalin-fixed, paraffin-embedded tissues can be used to identify
specific cell types involved in immunologic reactions of pregnancy.
In approximately 1-2% of all gestations, mononuclear cells can be seen infiltrating into the
chorionic villi of the placenta. Until the work of Redline and Patterson, however, the origin of
these cells had been controversial, some arguing for a fetal origin, some for a maternal origin.
Since immunochemistry alone could not answer this question they utilized in situ hybridization
for Y and X markers in male gestations to demonstrate that the lymphocytes present in cases of
chronic villitis are maternally derived, allowing us to focus on the causes of this apparent
maternal immunologic reaction against trophoblast and/or villous antigens.
Immunohistochemistry of such cases has shown that the cells within the villous core are T-cells
and macrophages.
Occasionally placentas manifest an intervillous space that is filled with mononuclear cells.
When immunohistochemically stained, these cells are revealed to be monocytic/macrophage in
origin. This monocytic intervillositis has been associated with IUGR, preeclampsia, recurrent
pregnancy loss and intrauterine fetal demise.
Dizygotic twins offer a unique opportunity to examine maternal immunologic reactions
against the placenta and fetus. Examination of dizygotic twins can sometimes reveal discordant
chronic villitis between the two placentas, with concomitant discrepancies in fetal growth.
Detailed analysis of each of such twins’ HLA expression and cytokine expression may help to
elucidate the causes of these immunologic reactions.
Although most cases of first trimester pregnancy loss are the result of genetic defects in the
fetus and/or placenta, some patients have recurrent pregnancy loss due to repeated maternal
immunologic reactions. These reactions can be directed against villous core antigens, against
antigens of the syncytiotrophoblast surface—manifested as an intervillositis, or against invasive
intermediate trophoblasts. Some have suggested a variety of therapies for these conditions,
including treatment with intravenous immunoglobulins, immunization with paternal or allogenic
leukocytes, or exposure to semen through vaginal or rectal suppositories. However, the scientific
Sunday, October 29, 2006 Page 20 of 19
From Trophoblasts to Human Placenta Harvey Kliman
basis of many of these approaches remains controversial and the efficacy of the therapies
proposed have been questioned.
Sunday, October 29, 2006 Page 21 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Further Reading
Benirschke K, Kaufmann P. (1995) Pathology of the human placenta. Third edition. Springer-
Verlag, New York.
Boyd JD, Hamilton WJ. (1970) The human placenta. W Heffer & Sons, Cambridge, England.
Feinberg R, Kliman H, Lockwood C. (1991) Oncofetal fibronectin: A trophoblast “glue” for
human implantation? American Journal of Pathology 138:537-543
Feinberg RF, Kliman HJ, Cohen AW. (1991) Preeclampsia, trisomy 13, and the placental bed.
Obstet Gynecol 78:505-8
Kliman H. (1994) Trophoblast infiltration. Reproductive Medicine Review 3:137-157
Kliman H. (1994) Placental hormones. Infertility and Reproductive Medicine Clinics of North
America 5:591-610
Kliman H, Nestler J, Sermasi E, Sanger J, Strauss J. (1986) Purification and in vitro
differentiation of cytotrophoblasts from human term placentae. Endocrinology 118:1567-82
Kliman HJ. (1993) The Placenta Revealed. Amer J Pathol 143:332-336
Kliman HJ, Feinberg RF. (1990) Human Trophoblast-Extracellular Matrix (ECM) Interactions
Invitro - ECM Thickness Modulates Morphology and Proteolytic Activity. Proceedings Of
the National Academy Of Scien 87:3057-3061
Kurman RJ, Main CS, Chen HC. (1984) Intermediate trophoblast: a distinctive form of
trophoblast with specific morphological, biochemical and functional features. Placenta
5:349-69
Moore KL. (1993) The developing human. Fifth edition. WB Saunders, Philadelphia.
Naeye RL. (1992) Disorders of the placenta, fetus, and neonate: Diagnosis and clinical
significance. Mosby Year Book, St. Louis.
Sunday, October 29, 2006 Page 22 of 19
From Trophoblasts to Human Placenta Harvey Kliman
Redline RW, Patterson P. (1993) Villitis of unknown etiology is associated with major
infiltration of fetal tissue by maternal inflammatory cells. Am J Pathol 143:473-9
Sadler TW. (1990 Langman’s medical embryology. Sixth edition. Williams & Wilkins,
Baltimore.
Sunday, October 29, 2006 Page 23 of 19
You might also like
- The Skincare Bible PDFDocument156 pagesThe Skincare Bible PDFLacramioara Valentina100% (12)
- Placenta 4 2 15Document52 pagesPlacenta 4 2 15Fellita Ratri A100% (1)
- Fertilization: The Beginning of PregnancyDocument389 pagesFertilization: The Beginning of PregnancyAngel Gabriel Fornillos100% (1)
- Elephant - Biology, Medicine and SurgeryDocument596 pagesElephant - Biology, Medicine and Surgerymada_superhero100% (2)
- Embryology: The Development of an Embryo in the First 3 WeeksDocument86 pagesEmbryology: The Development of an Embryo in the First 3 Weeksravindra sharma100% (1)
- Last Minute Embryology: Human embryology made easy and digestible for medical and nursing studentsFrom EverandLast Minute Embryology: Human embryology made easy and digestible for medical and nursing studentsNo ratings yet
- Embryology Made Ridiculously Simple Presentation (1) Updated (1) AgainDocument100 pagesEmbryology Made Ridiculously Simple Presentation (1) Updated (1) AgainAya Sobhi100% (4)
- Infection ControlDocument18 pagesInfection Controlannien_5No ratings yet
- 101-Normal Skin MCQsDocument25 pages101-Normal Skin MCQsHybat ElsheikhNo ratings yet
- Unit 2 - Fertilization, Impantation, Development of Placenta and Its Function, AbnormalityDocument62 pagesUnit 2 - Fertilization, Impantation, Development of Placenta and Its Function, AbnormalityN. Siva100% (1)
- ImplantationDocument20 pagesImplantationABc abcNo ratings yet
- Conception to Implantation: A Guide to the Early StagesDocument97 pagesConception to Implantation: A Guide to the Early StagesXo Yem100% (1)
- Microbiology and Parasitology Exam ReviewDocument157 pagesMicrobiology and Parasitology Exam ReviewJhasmin SalipotNo ratings yet
- Maternal and Child Health Nursing: Implantation and Fetal DevelopmentDocument7 pagesMaternal and Child Health Nursing: Implantation and Fetal DevelopmentJustine FloresNo ratings yet
- Module 2 - Process of Conception and Stage of Fetal DevelopmentDocument25 pagesModule 2 - Process of Conception and Stage of Fetal DevelopmentKatie HolmesNo ratings yet
- Pathophysiology of NSVDDocument2 pagesPathophysiology of NSVDLenjun83% (6)
- Anatomy of Normal PlacentaDocument8 pagesAnatomy of Normal Placentaareejk_94No ratings yet
- Fetal Development from Embryonic to Fetal Period Week by WeekDocument71 pagesFetal Development from Embryonic to Fetal Period Week by WeeklisafelixNo ratings yet
- Prenatal GrowthDocument56 pagesPrenatal GrowthnavjotsinghjassalNo ratings yet
- Fetal Heart Rate Monitoring PDFDocument279 pagesFetal Heart Rate Monitoring PDFFellita Ratri A100% (3)
- Ponciano IH PDFDocument69 pagesPonciano IH PDFCaressa Marie EstradaNo ratings yet
- DBT BET Question Paper 2009 With Answer KeyDocument22 pagesDBT BET Question Paper 2009 With Answer KeyAbhay Kumar100% (3)
- Pregnancy Conception and Early DevelopmentDocument10 pagesPregnancy Conception and Early DevelopmentErin SaavedraNo ratings yet
- Normal PregnancyDocument6 pagesNormal PregnancyCruz, Donna Angela M.No ratings yet
- MCH 314 Part ADocument5 pagesMCH 314 Part AAnifowose samsonNo ratings yet
- 8. Postimplantation Development in mammalianDocument52 pages8. Postimplantation Development in mammalianBiology BảoNo ratings yet
- Embryological and Fetal Development:-Fertilization - It Is The Process of Fusion of Spermatozoon With The Mature Ovum. ItDocument19 pagesEmbryological and Fetal Development:-Fertilization - It Is The Process of Fusion of Spermatozoon With The Mature Ovum. ItRaman SamraoNo ratings yet
- The Fundamentals of Embryology: Fertilization & Implantation and TwinningDocument15 pagesThe Fundamentals of Embryology: Fertilization & Implantation and TwinningElisa NNo ratings yet
- Anatomy of Normal PlacentaDocument8 pagesAnatomy of Normal PlacentaMaharani KartikaNo ratings yet
- MCN Lec - Chapter 3Document18 pagesMCN Lec - Chapter 3David LomentigarNo ratings yet
- Embryology Part 1Document34 pagesEmbryology Part 1Aira CorderoNo ratings yet
- Role of Cytotrophoblast in Placenta FormationDocument2 pagesRole of Cytotrophoblast in Placenta FormationJoe ThesecondmonthNo ratings yet
- Maternal and Child (Healthy Pregnancy)Document37 pagesMaternal and Child (Healthy Pregnancy)Lenny SucalditoNo ratings yet
- Human Embryonic DevelopmentDocument16 pagesHuman Embryonic DevelopmentsivaNo ratings yet
- SAQ EmbryologyDocument9 pagesSAQ EmbryologyShilpa DuttaNo ratings yet
- Human Physiology-25 (DR Sachin Kapur)Document42 pagesHuman Physiology-25 (DR Sachin Kapur)AmitNo ratings yet
- fertlizationDocument5 pagesfertlizationgallardo.bettinarose.iNo ratings yet
- Methotrexate for Ectopic Pregnancy is ImmoralDocument21 pagesMethotrexate for Ectopic Pregnancy is ImmoralelainemenezNo ratings yet
- Chapt17 Placenta PDFDocument12 pagesChapt17 Placenta PDFAnonymous 7resQ9No ratings yet
- Menstrual Cycle and Implantation)Document19 pagesMenstrual Cycle and Implantation)Ragdha MehdawiNo ratings yet
- Fetal DevelopmentDocument32 pagesFetal DevelopmentSavita HanamsagarNo ratings yet
- 3rd LecDocument8 pages3rd Lecنشط عقلكNo ratings yet
- 2008 - Huppertz - The Anatomy of The Normal PlacentaDocument8 pages2008 - Huppertz - The Anatomy of The Normal Placentaиick LooяNo ratings yet
- Stages of Fetal DevelopmentDocument42 pagesStages of Fetal DevelopmentKara Ashleigh0% (1)
- 6th Lecture Embryogenesis 2nd Week-8thDocument28 pages6th Lecture Embryogenesis 2nd Week-8thHussein Al Saedi100% (1)
- 1.5.3.1 - Perkembangan Janin Intrauterin Dan Gangguan Yang Mungkin TimbulDocument54 pages1.5.3.1 - Perkembangan Janin Intrauterin Dan Gangguan Yang Mungkin TimbulMuhammad Fatkhi100% (1)
- Reproduction Part 2Document12 pagesReproduction Part 2Yuh moddaNo ratings yet
- Conception and Diagnosis of Early PregnancyDocument48 pagesConception and Diagnosis of Early PregnancyjerrydanfordfxNo ratings yet
- The Placenta and Fetal MembranesDocument69 pagesThe Placenta and Fetal MembranesAnu ChauhanNo ratings yet
- Early Embryonic DevelopmentDocument48 pagesEarly Embryonic DevelopmentYeyen MusainiNo ratings yet
- 1-4 Fertilization & Fetal DevelopmentDocument9 pages1-4 Fertilization & Fetal DevelopmentElla DionedaNo ratings yet
- Nur 214 HandoutsDocument6 pagesNur 214 HandoutsCharlz ZipaganNo ratings yet
- Obstetrics: The Normal Menstrual CycleDocument4 pagesObstetrics: The Normal Menstrual Cycleapi-3829364No ratings yet
- CVM Pres - IIDocument152 pagesCVM Pres - IIseraphim8No ratings yet
- Embryonic Adaptations and Formation of Fetal Membranes Placentations and DeciduaeDocument69 pagesEmbryonic Adaptations and Formation of Fetal Membranes Placentations and DeciduaeApril MarieNo ratings yet
- Dkp1 Imam Agus Faisal 1.A. Stage or Phase Embriogenesis and OrganogenesisDocument3 pagesDkp1 Imam Agus Faisal 1.A. Stage or Phase Embriogenesis and OrganogenesisImam Agus FaisalNo ratings yet
- Biology ProjectDocument21 pagesBiology ProjectsivaNo ratings yet
- Fertilization to Childbirth: Stages of Human ReproductionDocument6 pagesFertilization to Childbirth: Stages of Human ReproductionAshok KumarNo ratings yet
- Abnormal ImplantationDocument3 pagesAbnormal ImplantationMuhammet Fatih CantepeNo ratings yet
- Fertilization - ImplantationDocument4 pagesFertilization - ImplantationEzeoke ChristabelNo ratings yet
- Phytotherapy For ReproductionDocument26 pagesPhytotherapy For ReproductionHusna JuliaNo ratings yet
- 7 - Week 1+2 - EmbryologyDocument6 pages7 - Week 1+2 - EmbryologyHajar ObeidatNo ratings yet
- Mitosis and Meiosis Objectives ExplainedDocument7 pagesMitosis and Meiosis Objectives ExplainedImranMohiuddinNo ratings yet
- Lecture - 2 - 3 - Goal - Fertilization - Placentation - LactationDocument4 pagesLecture - 2 - 3 - Goal - Fertilization - Placentation - LactationAPOORVA SHANDILYANo ratings yet
- The Biological Problem of To-day: Preformation Or Epigenesis?: The Basis of a Theory of Organic DevelopmentFrom EverandThe Biological Problem of To-day: Preformation Or Epigenesis?: The Basis of a Theory of Organic DevelopmentNo ratings yet
- COVID-19 Reinfection: Myth or TruthDocument4 pagesCOVID-19 Reinfection: Myth or TruthFellita Ratri ANo ratings yet
- L12. Medical Mycology 2 Ed DEDocument50 pagesL12. Medical Mycology 2 Ed DEFellita Ratri ANo ratings yet
- L10. Basic MycologyDocument45 pagesL10. Basic MycologyFellita Ratri ANo ratings yet
- Patogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFDocument49 pagesPatogenesis Preeklampsia - Apakah Masih Merupakan Penyakit Teori PDFFellita Ratri ANo ratings yet
- EclampsiaMidwiferyManagement-Jennie MagorDocument24 pagesEclampsiaMidwiferyManagement-Jennie MagorFellita Ratri ANo ratings yet
- EARLY AND LATE ONSET PREECLAMPSIA: KEY DIFFERENCESDocument35 pagesEARLY AND LATE ONSET PREECLAMPSIA: KEY DIFFERENCESFellita Ratri ANo ratings yet
- EclampsiaMidwiferyManagement-Jennie MagorDocument24 pagesEclampsiaMidwiferyManagement-Jennie MagorFellita Ratri ANo ratings yet
- Acceleration Program Reduction in Maternal Mortality Dr. Adhi Pribadi, SP - OG-KDocument6 pagesAcceleration Program Reduction in Maternal Mortality Dr. Adhi Pribadi, SP - OG-KFellita Ratri ANo ratings yet
- Statin in PE - MalangDocument33 pagesStatin in PE - MalangFellita Ratri ANo ratings yet
- Placenta Accreta Index Predicts Invasive PlacentationDocument7 pagesPlacenta Accreta Index Predicts Invasive PlacentationGregorius Juan GunawanNo ratings yet
- Endometriosis LirDocument32 pagesEndometriosis LirFellita Ratri ANo ratings yet
- Antihypertensive in Preeclampsia - Prof. SarmaDocument34 pagesAntihypertensive in Preeclampsia - Prof. SarmaFellita Ratri ANo ratings yet
- AubDocument16 pagesAubFellita Ratri ANo ratings yet
- EclampsiaMidwiferyManagement-Jennie MagorDocument24 pagesEclampsiaMidwiferyManagement-Jennie MagorFellita Ratri ANo ratings yet
- Placenta Accreta Index Predicts Invasive PlacentationDocument7 pagesPlacenta Accreta Index Predicts Invasive PlacentationGregorius Juan GunawanNo ratings yet
- Ovarian Life Cycle: Jimmy Yanuar AnnasDocument55 pagesOvarian Life Cycle: Jimmy Yanuar AnnasFellita Ratri ANo ratings yet
- Kondori - Final Physiology of Fetal Circulation - BWDocument34 pagesKondori - Final Physiology of Fetal Circulation - BWSudipta GhoshNo ratings yet
- 4 WHO Pathology Female Genital Organs - 2014Document308 pages4 WHO Pathology Female Genital Organs - 2014Fellita Ratri ANo ratings yet
- CPC RIK 5 Jurnal EngDocument6 pagesCPC RIK 5 Jurnal EngFellita Ratri ANo ratings yet
- An Update On Gestational Trophoblastic DiseaseDocument9 pagesAn Update On Gestational Trophoblastic DiseaseFellita Ratri ANo ratings yet
- FIGO 2012 Pathology of CancerDocument14 pagesFIGO 2012 Pathology of CancerFellita Ratri ANo ratings yet
- Pathophysiology of Ovarial CystDocument9 pagesPathophysiology of Ovarial CystFellita Ratri ANo ratings yet
- Pathophysiology of Ovarial CystDocument9 pagesPathophysiology of Ovarial CystFellita Ratri ANo ratings yet
- Animal Experimentation: A Look Into Ethics, Welfare and Alternative MethodsDocument6 pagesAnimal Experimentation: A Look Into Ethics, Welfare and Alternative MethodsBENSLIMANEOTHMANENo ratings yet
- Board of Intermediate & Secondary Education Saidu Sharif SwatDocument2 pagesBoard of Intermediate & Secondary Education Saidu Sharif SwatMUSHTAQ AHMADNo ratings yet
- Six Kingdoms of LifeDocument48 pagesSix Kingdoms of LifesagiNo ratings yet
- Questions On Transport and Storage in PlantsDocument10 pagesQuestions On Transport and Storage in PlantsNathan mwapeNo ratings yet
- A First Case Report of Feline Infectious Peritonitis in A Domestic Cat in PakistanDocument6 pagesA First Case Report of Feline Infectious Peritonitis in A Domestic Cat in PakistanRizki Ainun NajibNo ratings yet
- Sustainable Liquid Biofuels From Biomass: The Writing's On The WallsDocument13 pagesSustainable Liquid Biofuels From Biomass: The Writing's On The WallsLextito HarnadiNo ratings yet
- Practicas Microbiologicas EstandarDocument2 pagesPracticas Microbiologicas EstandarWendy JNo ratings yet
- First Year B.Sc. Nursing Question Paper 2004Document17 pagesFirst Year B.Sc. Nursing Question Paper 2004Biju Antony100% (1)
- Loeffler 1986Document11 pagesLoeffler 1986Dicson Sánchez AbadNo ratings yet
- Activity No. 4 Amino Acids and ProteinsDocument6 pagesActivity No. 4 Amino Acids and ProteinsAngel EspanolNo ratings yet
- ISC Class 12 Biology Question Paper 01 (2018) : Material Downloaded From - 1 / 5Document5 pagesISC Class 12 Biology Question Paper 01 (2018) : Material Downloaded From - 1 / 5HemantNo ratings yet
- Aries 28: A Large Disappointed AudienceDocument2 pagesAries 28: A Large Disappointed AudienceStarlingNo ratings yet
- GPB-366-ALL-OBJECTIVE-QU.Document56 pagesGPB-366-ALL-OBJECTIVE-QU.durgeshhire710No ratings yet
- Novel Delivery Technology For Probiotic BacteriaDocument3 pagesNovel Delivery Technology For Probiotic BacteriaArup NagNo ratings yet
- Understanding Stated and Unstated Information in A Text1Document12 pagesUnderstanding Stated and Unstated Information in A Text1Bella AzisNo ratings yet
- Environmental Biotech UsesDocument40 pagesEnvironmental Biotech Usesalfi alfathanaNo ratings yet
- Class-3 Army School Holiday HomeworkDocument33 pagesClass-3 Army School Holiday HomeworkRAVINDRA SINGH SAHABNo ratings yet
- Thesis Bone Tissue EngineeringDocument6 pagesThesis Bone Tissue Engineeringsarahturnerdesmoines100% (2)
- Sulci & Gyri - Doaa 2021Document23 pagesSulci & Gyri - Doaa 2021Mohamed AbouzaidNo ratings yet
- Ability Uber ListDocument80 pagesAbility Uber Listorinnightshade100% (1)
- VentussaDocument7 pagesVentussaDianne ManingdingNo ratings yet
- DPP - Daily Practice Problems - BIOLOGYDocument6 pagesDPP - Daily Practice Problems - BIOLOGYmansoorbariNo ratings yet
- HermanYeung DSE Bio CH 3E Temp NoteDocument5 pagesHermanYeung DSE Bio CH 3E Temp NoteliNo ratings yet