0% found this document useful (0 votes)
658 views28 pagesSystemic Mycosis and Candidiasis Overview
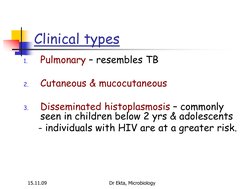
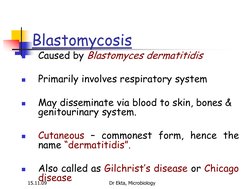
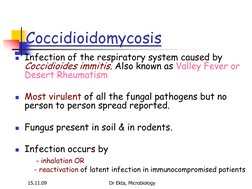
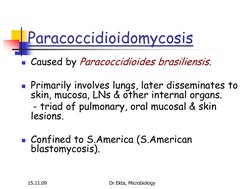
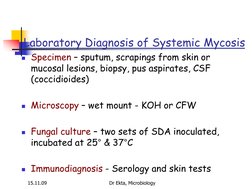
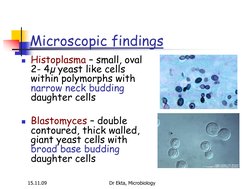
This document discusses systemic mycosis, which are fungal infections that spread throughout the internal organs. The most common types are histoplasmosis, blastomycosis, coccidioidomycosis, and paracoccidioidomycosis. They are caused by dimorphic fungi that can infect both healthy and immunocompromised individuals. Laboratory diagnosis involves examining samples microscopically for fungal structures, culturing samples, and performing serological tests. Treatment depends on the severity and location of infection, and may include antifungal drugs like amphotericin B or azoles.
Uploaded by
adiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
658 views28 pagesSystemic Mycosis and Candidiasis Overview
This document discusses systemic mycosis, which are fungal infections that spread throughout the internal organs. The most common types are histoplasmosis, blastomycosis, coccidioidomycosis, and paracoccidioidomycosis. They are caused by dimorphic fungi that can infect both healthy and immunocompromised individuals. Laboratory diagnosis involves examining samples microscopically for fungal structures, culturing samples, and performing serological tests. Treatment depends on the severity and location of infection, and may include antifungal drugs like amphotericin B or azoles.
Uploaded by
adiCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd