Professional Documents
Culture Documents
Abscess and Phlegmon PDF
Abscess and Phlegmon PDF
Uploaded by
DiannokaIhzaGanungOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abscess and Phlegmon PDF
Abscess and Phlegmon PDF
Uploaded by
DiannokaIhzaGanungCopyright:
Available Formats
ATLAS OF HEAD AND NECK PATHOLOGY ABSCESS AND PLEGMON
ABSCESS AND PHLEGMON
An abscess is a localized collection of pus often caused by bacteria such as
staphyloccus aureus. Foreign material, fibrin, and blood clot may predispose. There is
severe inflammation with masses of neutrophils, living and dead, necrotic tissue
debris, and formation of granulation tissue at the periphery to wall off the abscess.
Leukocytes gather in the infected area and produce proteases that degrade
dead tissue and convert it into pus. This process is termed liquefactive necrosis. The
pus may discharge to the surface or if resolution occurs, there is healing with scar
formation.
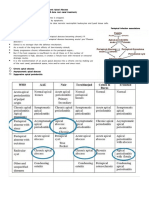
Abscess. High power shows a near pure population of
neutrophils in the central portion of this abscess.
table of contents previous next
ATLAS OF HEAD AND NECK PATHOLOGY ABSCESS AND PLEGMON
Abscess, skin. Fibrosis is present in wall (arrow) of the
abscess. Suture material was seen nearby.
Phlegmon, tongue. Muscle fibers are swollen and have
lost their striations (arrow). Nuclei are becoming indis-
tinct (triangle). There is heavy infiltrate of inflammatory
cells between muscle fibers.
table of contents previous next
ATLAS OF HEAD AND NECK PATHOLOGY ABSCESS AND PLEGMON
Abscess. Intense population of neutrophils surrounds a
liquid center containing keratinous debris. Nemerous
foreign body giant cells in periphery.
CLINCAL ASPECTS:
A common site for abscess in the head and neck area is the peritonsillar space. A periton-
sillar abscess is also known as a “quinsy.” Bacteria spread from an acute infection of the palatine
tonsil to the potential space between the tonsil and the adjacent muscle with the resultant devel-
opment of an abscess. A large abscess may literally dissect the tonsil from its bed but more
commonly the abscess is less advanced. In the healing process, a marked fibrotic reaction results
in dense scar that may make dissection difficult should the patient later undergo tonsillectomy.
Untreated, a peritonsillar abscess usually ruptures into the pharynx spontaneously, or
slowly resolves. In rare instances, an untreated patient may develop a life-threatening situation
should the peritonsillar abscess obstruct the airway, rupture with aspiration of pus, or extend into
the parapharyngeal space and superior mediastinum (carotid rupture), or travel along the carotid
sheath and reach the intracranial cavity resulting in cerebritis/meningitis.
Thyroglossal cysts and branchial cysts commonly develop intermittent infections with
abscess formation and there are a multitude of other conditions about the head and neck predis-
posing to abscess.
table of contents previous next
ATLAS OF HEAD AND NECK PATHOLOGY ABSCESS AND PLEGMON
A phlegmon results when an acute infection is not confined as in the case of
abscess. Instead the infection spreads along tissue planes and between muscle fibers.
Ludwig’s angina is a phlegmon of the neck. In that condition, infection (usually
streptococcal) comes from a mandibular tooth and produces brawny induration of the
neck that may extend from mandible to clavicle and be life-threatening.
table of contents previous next
You might also like
- Dirty Texting Lenguage of LustDocument19 pagesDirty Texting Lenguage of LustValpo ValparaisoNo ratings yet
- Torts Rule StatementsDocument40 pagesTorts Rule Statementskoreanman100% (1)
- Play Based Learning PresentationDocument14 pagesPlay Based Learning PresentationNajwaCacen100% (23)
- OsteomyelitisDocument147 pagesOsteomyelitisAnkit Agur100% (1)
- Provide Housekeeping Service To The Guest: Learning Activity Sheet No. 2-3 QuarterDocument45 pagesProvide Housekeeping Service To The Guest: Learning Activity Sheet No. 2-3 Quartershirley martin100% (1)
- Thyroglossal Duct CystDocument2 pagesThyroglossal Duct CystPulkitNo ratings yet
- Cleft Lip and Palate Management: A Comprehensive AtlasFrom EverandCleft Lip and Palate Management: A Comprehensive AtlasRicardo D. BennunNo ratings yet
- Vernier CaliperDocument2 pagesVernier CaliperMechtek LabNo ratings yet
- EmpyemaDocument52 pagesEmpyemaDivara Syauta100% (3)
- Accounting For LaborDocument7 pagesAccounting For LaborKrizel Dixie ParraNo ratings yet
- GrashaDocument9 pagesGrashaLisha LiuNo ratings yet
- Pott's SpineDocument47 pagesPott's Spinesigarun67% (3)
- Extra-Cranial Complications of CSOMfinalDocument37 pagesExtra-Cranial Complications of CSOMfinalAarthi Gopal100% (2)
- A Mini-Atlas of Ear-Drum Pathology PDFDocument7 pagesA Mini-Atlas of Ear-Drum Pathology PDFalexandra_i_nitaNo ratings yet
- Hospital List For Ayushman Bharat YojnaDocument6 pagesHospital List For Ayushman Bharat Yojnadadan vishwakarma100% (1)
- Resume XerostomiaDocument1 pageResume XerostomiaGieh SyafitriNo ratings yet
- Gambar Makros Mikros RadangDocument41 pagesGambar Makros Mikros RadangBevi Ayu Kumala WardaniNo ratings yet
- Neck MassesDocument24 pagesNeck MassesIstiklal SurgeryNo ratings yet
- Kongenitalne Ciste I Fistule VrataDocument2 pagesKongenitalne Ciste I Fistule VrataRoppeNo ratings yet
- Nasolabial CystDocument7 pagesNasolabial CystathaNo ratings yet
- Acute Haematogenous Osteomyelitis (Aho)Document33 pagesAcute Haematogenous Osteomyelitis (Aho)anggi dwi puteraNo ratings yet
- Ent CsomDocument18 pagesEnt CsomtarunNo ratings yet
- Prolapso IrisDocument15 pagesProlapso IrisFelippe CorreiaNo ratings yet
- Wo MSKK Week 5Document7 pagesWo MSKK Week 5GabrielaNo ratings yet
- Neuroscience - The Brain and Spiral CordDocument4 pagesNeuroscience - The Brain and Spiral CordAnn MutisyaNo ratings yet
- Definition:: and Histiocytes. Ulceration May Finally Lead To Granulation Tissue FormationDocument11 pagesDefinition:: and Histiocytes. Ulceration May Finally Lead To Granulation Tissue FormationThomas ChapelNo ratings yet
- Kelainan Kepala Dan LeherDocument17 pagesKelainan Kepala Dan LeherSoraya HumairaNo ratings yet
- Friedberg 1940Document14 pagesFriedberg 1940YPramudiyaNo ratings yet
- Periapical PeriodontitisDocument7 pagesPeriapical Periodontitisعلي صادق جعفرNo ratings yet
- OsteomyelitisDocument32 pagesOsteomyelitisAndi Wija Indrawan PangerangNo ratings yet
- Oral Pathology: Non-Epithelialized Primary Bone CystDocument4 pagesOral Pathology: Non-Epithelialized Primary Bone Cystعلي صادق جعفرNo ratings yet
- Chronic Adhesive Otitis Media 1956Document10 pagesChronic Adhesive Otitis Media 1956Teuku Ahmad HasanyNo ratings yet
- Infecti ON: Acute, Subacute and Chronic OsteomyelitisDocument32 pagesInfecti ON: Acute, Subacute and Chronic OsteomyelitisNardine RoslanNo ratings yet
- Objective - SURGERYDocument54 pagesObjective - SURGERYlaraNo ratings yet
- Patofisiologi OsteomyelitisDocument7 pagesPatofisiologi OsteomyelitisSyahrir RusdyNo ratings yet
- Cavernous Sinus ThrombosisDocument8 pagesCavernous Sinus Thrombosisرغد القرنيNo ratings yet
- Fascial Space InfectionDocument19 pagesFascial Space Infectiondion leonardoNo ratings yet
- ENTJ 2012 07 Paranasal Sinus MucoceleDocument3 pagesENTJ 2012 07 Paranasal Sinus MucoceleTatiana DecusearăNo ratings yet
- Investigacion Complexivo InglesDocument3 pagesInvestigacion Complexivo InglesJaime Luis Guamán QuintuñaNo ratings yet
- Chronic Suppurative Otitis MediaDocument34 pagesChronic Suppurative Otitis Mediafreelancer.am1302No ratings yet
- Petrous Apex LesionsDocument2 pagesPetrous Apex LesionsPulkitNo ratings yet
- Histology: Diagnosis and Treatment of Chronic Apical AbscessDocument3 pagesHistology: Diagnosis and Treatment of Chronic Apical AbscessPrince AmiryNo ratings yet
- Edited - Very Very FinalDocument31 pagesEdited - Very Very FinalRm LavariasNo ratings yet
- Absceso Cerebral 99Document7 pagesAbsceso Cerebral 99shen_siiNo ratings yet
- Case of The Week: Professor Yasser MetwallyDocument9 pagesCase of The Week: Professor Yasser MetwallyNinaNo ratings yet
- Manish Deo Roll No..10 Bds 3rd YrDocument27 pagesManish Deo Roll No..10 Bds 3rd YrKim Duyen DoNo ratings yet
- 28-Clin Head & NeckDocument42 pages28-Clin Head & NeckKHAIRUN NISA MOHD ZAIDANNo ratings yet
- Empyema (Pyothorax) : Week 1 Dr. Kazzara RaeburnDocument4 pagesEmpyema (Pyothorax) : Week 1 Dr. Kazzara Raeburnpvs5155No ratings yet
- Exposicion FinishDocument13 pagesExposicion FinishFernanda ChNo ratings yet
- 14 Review ArticleDocument3 pages14 Review ArticleShriya ShahuNo ratings yet
- CystDocument6 pagesCystmustafaNo ratings yet
- Abscess 2Document4 pagesAbscess 2SANDEEP SINGHNo ratings yet
- Fissural CystsDocument17 pagesFissural CystssailalithaNo ratings yet
- Nose and Paranasal Sinuses According To New Reference 2Document121 pagesNose and Paranasal Sinuses According To New Reference 2Victor EnachiNo ratings yet
- Dangerous Area of FaceDocument1 pageDangerous Area of FaceDianPresarioNo ratings yet
- Histologically, The Chancre Is Characterised byDocument6 pagesHistologically, The Chancre Is Characterised byIsak ShatikaNo ratings yet
- Ijohns 2015081714003574Document4 pagesIjohns 2015081714003574lukyNo ratings yet
- 34 OsteomyelitisDocument3 pages34 OsteomyelitisDurga VoraNo ratings yet
- Auntminnie SignsDocument56 pagesAuntminnie SignsHey ReelNo ratings yet
- Head and Neck Space Infections: Parotid AbscessDocument7 pagesHead and Neck Space Infections: Parotid AbscessFara Nindya MaharaniNo ratings yet
- Occur Largely in The Newborn and in Children Younger Than 5 Years, and Rarely in Older IndividualsDocument6 pagesOccur Largely in The Newborn and in Children Younger Than 5 Years, and Rarely in Older IndividualsElle ReyesNo ratings yet
- LP Abses SerebriDocument29 pagesLP Abses SerebriMarinaLestariNo ratings yet
- Spread of InflamationDocument14 pagesSpread of InflamationShadeeBreijiehNo ratings yet
- Dr. K Tarun Rao PG in Dept of Orthopedics Caims, KarimnagarDocument163 pagesDr. K Tarun Rao PG in Dept of Orthopedics Caims, KarimnagarShravani ShagapuramNo ratings yet
- 1st Shift CA Sources (Snell)Document6 pages1st Shift CA Sources (Snell)ernignacioNo ratings yet
- Tuberculosis Urogenital: Urología Dr. Francisco Cruz López Universidad Veracruzana Javier Evaristo Hernández OrdazDocument80 pagesTuberculosis Urogenital: Urología Dr. Francisco Cruz López Universidad Veracruzana Javier Evaristo Hernández OrdazJavier EvaristoNo ratings yet
- Abscess, Lud Wig AnginaDocument64 pagesAbscess, Lud Wig Anginafahim ahamedNo ratings yet
- 1 s2.0 S1658361218300246 Main PDFDocument8 pages1 s2.0 S1658361218300246 Main PDFDanis Diba Sabatillah YaminNo ratings yet
- Tooth Autotransplantation. What's The Limit of Our Possibilities in Conservative Treatments?Document6 pagesTooth Autotransplantation. What's The Limit of Our Possibilities in Conservative Treatments?Danis Diba Sabatillah YaminNo ratings yet
- Influence of Platelet Rich Fibrin On Post-Extraction Socket Healing: A Clinical and Radiographic StudyDocument7 pagesInfluence of Platelet Rich Fibrin On Post-Extraction Socket Healing: A Clinical and Radiographic StudyDanis Diba Sabatillah YaminNo ratings yet
- 1 s2.0 S1013905218305467 Main PDFDocument7 pages1 s2.0 S1013905218305467 Main PDFDanis Diba Sabatillah YaminNo ratings yet
- 1 s2.0 S0002817714622935 Main PDFDocument8 pages1 s2.0 S0002817714622935 Main PDFDanis Diba Sabatillah YaminNo ratings yet
- Ectopic Third Molar Associated With A Cyst in The Sigmoid NotchDocument3 pagesEctopic Third Molar Associated With A Cyst in The Sigmoid NotchDanis Diba Sabatillah YaminNo ratings yet
- What Are The Risk Factors For External Root Resorption of Second Molars Associated With Impacted Third Molars? A Cone-Beam Computed Tomography StudyDocument7 pagesWhat Are The Risk Factors For External Root Resorption of Second Molars Associated With Impacted Third Molars? A Cone-Beam Computed Tomography StudyDanis Diba Sabatillah YaminNo ratings yet
- Immediate Bonding Properties of Universal Adhesives To DentineDocument8 pagesImmediate Bonding Properties of Universal Adhesives To DentineDanis Diba Sabatillah YaminNo ratings yet
- NSK Varios Tip Book PDFDocument28 pagesNSK Varios Tip Book PDFDanis Diba Sabatillah YaminNo ratings yet
- 2016 Vol 62 No - 2 - April May 2016 PDFDocument56 pages2016 Vol 62 No - 2 - April May 2016 PDFDanis Diba Sabatillah YaminNo ratings yet
- 100 103 PDFDocument4 pages100 103 PDFDanis Diba Sabatillah YaminNo ratings yet
- 100 103 PDFDocument4 pages100 103 PDFDanis Diba Sabatillah YaminNo ratings yet
- 1999 WHO/ISH Statement On Management of HypertensionDocument10 pages1999 WHO/ISH Statement On Management of HypertensionDenisa NugrahitaNo ratings yet
- ClarkClassIIDentToday PDFDocument3 pagesClarkClassIIDentToday PDFDanis Diba Sabatillah YaminNo ratings yet
- Microleakage in Combined Amalgam/composite Resin Restorations in MOD CavitiesDocument5 pagesMicroleakage in Combined Amalgam/composite Resin Restorations in MOD CavitiesDanis Diba Sabatillah YaminNo ratings yet
- 5657764908aeafc2aac101b1 PDFDocument102 pages5657764908aeafc2aac101b1 PDFDanis Diba Sabatillah YaminNo ratings yet
- Improvement of Palliative Care in Cancer Patients inDocument20 pagesImprovement of Palliative Care in Cancer Patients inLeaLunaNo ratings yet
- Importing Mining Chemicals From ChinaDocument6 pagesImporting Mining Chemicals From Chinacalisto_rNo ratings yet
- Fuel Production Cost Estimates and Assumptions.: This Is Part of Zero-Emission Vessels: Transition PathwaysDocument44 pagesFuel Production Cost Estimates and Assumptions.: This Is Part of Zero-Emission Vessels: Transition PathwaysPanchadcharam PushparubanNo ratings yet
- Center List Above 1.5 Crore AssamDocument115 pagesCenter List Above 1.5 Crore AssamRahul BhagatNo ratings yet
- Ingles UPCDocument5 pagesIngles UPCHector TineoNo ratings yet
- Ca3 Therapeutic Modality Grp.3Document15 pagesCa3 Therapeutic Modality Grp.3Valjim PacatangNo ratings yet
- Safety Valves For Industrial ApplicationDocument164 pagesSafety Valves For Industrial ApplicationJOHNNo ratings yet
- Series 622: Operating, Maintenance & Parts ManualDocument12 pagesSeries 622: Operating, Maintenance & Parts ManualMARTIN FLORESNo ratings yet
- This Study Resource Was: Ak - Ic - Mock Exam Set ADocument9 pagesThis Study Resource Was: Ak - Ic - Mock Exam Set AArvinALNo ratings yet
- Beauty CosmeticsDocument27 pagesBeauty CosmeticsMark OlsenNo ratings yet
- History of NarraDocument4 pagesHistory of NarraArmand Caleb Delos ReyesNo ratings yet
- 9990 Scheme of Work (For Examination From 2020)Document96 pages9990 Scheme of Work (For Examination From 2020)AyaNo ratings yet
- The Effect of Probiotic Biscuit On Faecal Microbiota in Malnourished ChildrenDocument11 pagesThe Effect of Probiotic Biscuit On Faecal Microbiota in Malnourished ChildrenAhmad DexNo ratings yet
- Scope2 PDFDocument2 pagesScope2 PDFGregorNo ratings yet
- Lightnin Plenty BrochureDocument28 pagesLightnin Plenty BrochureHenry Garavito RamirezNo ratings yet
- Prevalence and Underlying Factors of MobileDocument10 pagesPrevalence and Underlying Factors of MobileJoan CedyNo ratings yet
- Myasthenia GDocument7 pagesMyasthenia GAcbel RnucoNo ratings yet
- Ertad SVX01F E4Document84 pagesErtad SVX01F E4sachin JoshiNo ratings yet
- Create The ValueDocument6 pagesCreate The ValueMegan PurdyNo ratings yet
- Mattoc 160mm, Main Spring 40 Psi, IRT Pressure ComparisonDocument1 pageMattoc 160mm, Main Spring 40 Psi, IRT Pressure ComparisonFandy SugiartoNo ratings yet
- Analytical Framework: This Guide Provides You With Explanations To Help You Work With The Analytical Framework TemplateDocument4 pagesAnalytical Framework: This Guide Provides You With Explanations To Help You Work With The Analytical Framework Templatemohammed mahfoudhNo ratings yet
- NewsRecord14 01 29Document14 pagesNewsRecord14 01 29Kristina HicksNo ratings yet