Professional Documents
Culture Documents
10 1 1 473 9492 PDF
Uploaded by
arseniosilvaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1 1 473 9492 PDF
Uploaded by
arseniosilvaCopyright:
Available Formats
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Review Article
Mechanisms of Disease static plug but also secrete several mediators of wound
healing, such as platelet-derived growth factor, that
attract and activate macrophages and fibroblasts (Ta-
F R A N K L I N H . E P S T E I N , M. D. , Editor ble 1).4 However, in the absence of hemorrhage,
platelets are not essential to wound healing. Numer-
ous vasoactive mediators and chemotactic factors are
generated by the coagulation and activated-comple-
C UTANEOUS W OUND H EALING ment pathways and by injured or activated parenchy-
mal cells. These substances recruit inflammatory leu-
ADAM J. SINGER, M.D., AND RICHARD A.F. CLARK, M.D. kocytes to the site of injury.3
Infiltrating neutrophils cleanse the wounded area
of foreign particles and bacteria and are then extrud-
ed with the eschar or phagocytosed by macrophages.
T
HE primary function of the skin is to serve In response to specific chemoattractants, such as
as a protective barrier against the environ- fragments of extracellular-matrix protein, transform-
ment. Loss of the integrity of large portions ing growth factor b, and monocyte chemoattractant
of the skin as a result of injury or illness may lead to protein 1, monocytes also infiltrate the wound site and
major disability or even death. Every year in the Unit- become activated macrophages that release growth
ed States more than 1.25 million people have burns1 factors such as platelet-derived growth factor and
and 6.5 million have chronic skin ulcers caused by vascular endothelial growth factor, which initiate the
pressure, venous stasis, or diabetes mellitus.2 formation of granulation tissue. Macrophages bind
The primary goals of the treatment of wounds are to specific proteins of the extracellular matrix by their
rapid wound closure and a functional and aestheti- integrin receptors, an action that stimulates phago-
cally satisfactory scar. Recent advances in cellular and cytosis of microorganisms and fragments of extracel-
molecular biology have greatly expanded our under- lular matrix by the macrophages.5
standing of the biologic processes involved in wound Adherence to the extracellular matrix also stimu-
repair and tissue regeneration3 and have led to im- lates monocytes to undergo metamorphosis into in-
provements in wound care. We review here the biol- flammatory or reparative macrophages. Adherence
ogy of the healing of traumatic and nontraumatic induces monocytes and macrophages to express col-
wounds and discuss the use of skin substitutes and ony-stimulating factor 1, a cytokine necessary for the
growth factors to promote wound healing. survival of monocytes and macrophages; tumor ne-
crosis factor a, a potent inflammatory cytokine; and
BIOLOGY OF WOUND HEALING platelet-derived growth factor, a potent chemoat-
Wound healing is a dynamic, interactive process tractant and mitogen for fibroblasts (Table 1). Other
involving soluble mediators, blood cells, extracellular important cytokines expressed by monocytes and
matrix, and parenchymal cells (Fig. 1 and 2). Wound macrophages are transforming growth factor a, inter-
healing has three phases — inflammation, tissue for- leukin-1, transforming growth factor b, and insulin-
mation, and tissue remodeling — that overlap in time. like growth factor I.6 The monocyte- and macro-
phage-derived growth factors are almost certainly
Inflammation necessary for the initiation and propagation of new
Tissue injury causes the disruption of blood vessels tissue formation in wounds, because macrophage-
and extravasation of blood constituents. The blood depleted animals have defective wound repair.7 Thus,
clot reestablishes hemostasis and provides a provi- macrophages appear to have a pivotal role in the
sional extracellular matrix for cell migration (Fig. 1). transition between inflammation and repair.8
Platelets not only facilitate the formation of a hemo-
Epithelialization
Reepithelialization of wounds begins within hours
after injury (Fig. 3). Epidermal cells from skin ap-
From the Departments of Emergency Medicine (A.J.S.) and Dermatology pendages such as hair follicles quickly remove clotted
(R.A.F.C.), State University of New York at Stony Brook, Stony Brook. Ad- blood and damaged stroma from the wound space
dress reprint requests to Dr. Singer at the Department of Emergency Med- (Fig. 2). At the same time, the cells undergo marked
icine, University Medical Center, State University of New York at Stony
Brook, Stony Brook, NY 11794-8350. phenotypic alteration that includes retraction of in-
©1999, Massachusetts Medical Society. tracellular tonofilaments9; dissolution of most inter-
738 · S eptem b er 2 , 19 9 9
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
M EC H A NIS MS OF D IS EAS E
Inflammatory Phase (Day 3)
Fibrin clot
Macrophage
Neutrophil
Epidermis TGF-b1 TGF-a
TGF-a
Platelet# FGF
plug
VEGF
PDGF BB
TGF-b1 IGF
PDGF AB
Blood vessel
TGF-b14
KGF
PDGF TGF-b24
VEGF TGF-b3
Dermis
Neutrophil Macrophage FGF-2
FGF-2
Fibroblast TGF-b1
Fibroblast
Fat
Figure 1. A Cutaneous Wound Three Days after Injury.
Growth factors thought to be necessary for cell movement into the wound are shown. TGF-b1, TGF-b2, and TGF-b3 denote trans-
forming growth factor b1, b2, and b3, respectively; TGF-a transforming growth factor a; FGF fibroblast growth factor; VEGF vascular
endothelial growth factor; PDGF, PDGF AB, and PDGF BB platelet-derived growth factor, platelet-derived growth factor AB, and
platelet-derived growth factor BB, respectively; IGF insulin-like growth factor; and KGF keratinocyte growth factor.
cellular desmosomes, which provide physical connec- tween the collagenous dermis and the fibrin eschar,
tions between the cells; and formation of peripheral depends on the production of collagenase by epider-
cytoplasmic actin filaments, which allow cell move- mal cells,15 as well as the activation of plasmin by plas-
ment.10,11 Furthermore, epidermal and dermal cells minogen activator produced by the epidermal cells.16
no longer adhere to one another, because of the dis- Plasminogen activator also activates collagenase (ma-
solution of hemidesmosomal links between the epi- trix metalloproteinase 1)17 and therefore facilitates
dermis and the basement membrane, which allows the degradation of collagen and extracellular-matrix
the lateral movement of epidermal cells. The expres- proteins.
sion of integrin receptors on epidermal cells allows One to two days after injury, epidermal cells at the
them to interact with a variety of extracellular-matrix wound margin begin to proliferate behind the ac-
proteins (e.g., fibronectin and vitronectin) that are tively migrating cells (Fig. 3). The stimuli for the mi-
interspersed with stromal type I collagen at the mar- gration and proliferation of epidermal cells during
gin of the wound and interwoven with the fibrin reepithelialization have not been determined, but sev-
clot in the wound space.12-14 The migrating epidermal eral possibilities exist. The absence of neighbor cells
cells dissect the wound, separating desiccated eschar at the margin of the wound (the “free edge” effect)
from viable tissue. The path of dissection appears to may signal both migration and proliferation of epi-
be determined by the array of integrins that the mi- dermal cells. Local release of growth factors and in-
grating epidermal cells express on their cell mem- creased expression of growth-factor receptors may also
branes. stimulate these processes. Leading contenders in-
The degradation of the extracellular matrix, which clude epidermal growth factor, transforming growth
is required if the epidermal cells are to migrate be- factor a, and keratinocyte growth factor.18-20 As reep-
Vol ume 341 Numb e r 10 · 739
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Reepithelialization and Neovascularization (Day 5)
Fibrin clot
t-PA
u-PA
MMP-1, 2, 3, 13
MMP-1, 2, 3
Epidermis
u-PA
MMP-1, 2, 3, 13
Fibroblast
Granulation tissue Blood vessel
Dermis
Collagen
Fat
Figure 2. A Cutaneous Wound Five Days after Injury.
Blood vessels are seen sprouting into the fibrin clot as epidermal cells resurface the wound. Proteinases thought to be necessary
for cell movement are shown. The abbreviation u-PA denotes urokinase-type plasminogen activator; MMP-1, 2, 3, and 13 matrix
metalloproteinases 1, 2, 3, and 13 (collagenase 1, gelatinase A, stromelysin 1, and collagenase 3, respectively); and t-PA tissue plas-
minogen activator.
ithelialization ensues, basement-membrane proteins sumably stimulate fibroblasts of the tissue around
reappear in a very ordered sequence from the margin the wound to proliferate, express appropriate integrin
of the wound inward, in a zipperlike fashion.21 Epi- receptors, and migrate into the wound space. Indeed,
dermal cells revert to their normal phenotype, once platelet-derived growth factor accelerates the healing
again firmly attaching to the reestablished basement of chronic pressure sores 26 and diabetic ulcers,27 and
membrane and underlying dermis. basic fibroblast growth factor has been used with
some success to treat chronic pressure sores.28
Formation of Granulation Tissue The structural molecules of newly formed extra-
New stroma, often called granulation tissue, begins cellular matrix, termed the provisional matrix,21 con-
to invade the wound space approximately four days tribute to the formation of granulation tissue by pro-
after injury. Numerous new capillaries endow the new viding a scaffold or conduit for cell migration. These
stroma with its granular appearance. Macrophages, molecules include fibrin, fibronectin, and hyaluronic
fibroblasts, and blood vessels move into the wound acid.29,30 In fact, the appearance of fibronectin and
space at the same time.22 The macrophages provide the appropriate integrin receptors that bind fibro-
a continuing source of growth factors necessary to nectin, fibrin, or both on fibroblasts appears to be the
stimulate fibroplasia and angiogenesis; the fibroblasts rate-limiting step in the formation of granulation tis-
produce the new extracellular matrix necessary to sup- sue.25,31 The fibroblasts are responsible for the syn-
port cell ingrowth; and blood vessels carry oxygen thesis, deposition, and remodeling of the extracellular
and nutrients necessary to sustain cell metabolism. matrix. Conversely, the extracellular matrix can have
Growth factors, especially platelet-derived growth a positive or negative effect on the ability of fibro-
factor 4 and transforming growth factor b1,23 in con- blasts to synthesize, deposit, remodel, and generally
cert with the extracellular-matrix molecules,24,25 pre- interact with the extracellular matrix.25,32
740 · S ep tem b er 2 , 19 9 9
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
MEC H A NIS MS OF D IS EAS E
TABLE 1. CYTOKINES THAT AFFECT WOUND HEALING.
CYTOKINE MAJOR SOURCE TARGET CELLS AND MAJOR EFFECTS
Epidermal growth factor family Epidermal and mesenchymal regeneration
Epidermal growth factor Platelets Pleiotropic-cell motility and proliferation
Transforming growth factor a Macrophages, epidermal cells Pleiotropic-cell motility and proliferation
Heparin-binding epidermal Macrophages Pleiotropic-cell motility and proliferation
growth factor
Fibroblast growth factor family Wound vascularization
Basic fibroblast growth factor Macrophages, endothelial cells Angiogenesis and fibroblast proliferation
Acidic fibroblast growth factor Macrophages, endothelial cells Angiogenesis and fibroblast proliferation
Keratinocyte growth factor Fibroblasts Epidermal-cell motility and proliferation
Transforming growth factor b family Fibrosis and increased tensile strength
Transforming growth factors b1 Platelets, macrophages Epidermal-cell motility, chemotaxis of
and b 2 macrophages and fibroblasts, extracel-
lular-matrix synthesis and remodeling
Transforming growth factor b3 Macrophages Antiscarring effects
Other
Platelet-derived growth factor Platelets, macrophages, epi- Fibroblast proliferation and chemoattrac-
dermal cells tion, macrophage chemoattraction and
activation
Vascular endothelial growth factor Epidermal cells, macrophages Angiogenesis and increased vascular per-
meability
Tumor necrosis factor a Neutrophils Pleiotropic expression of growth factors
Interleukin-1 Neutrophils Pleiotropic expression of growth factors
Insulin-like growth factor I Fibroblasts, epidermal cells Reepithelialization and granulation-tis-
sue formation
Colony-stimulating factor 1 Multiple cells Macrophage activation and granulation-
tissue formation
Cell movement into a blood clot of cross-linked sequently, many other molecules have also been
fibrin or into tightly woven extracellular matrix may found to have angiogenic activity, including vascular
require an active proteolytic system that can cleave endothelial growth factor, transforming growth fac-
a path for cell migration. A variety of fibroblast- tor b, angiogenin, angiotropin, angiopoietin 1, and
derived enzymes, in addition to serum-derived plas- thrombospondin, to name but a few.37-39 Low oxygen
min, are potential candidates for this task, including tension40 and elevated lactic acid may also stimulate
plasminogen activator, collagenases, gelatinase A, and angiogenesis. Many of the molecules mentioned above
stromelysin.17,33 appear to induce angiogenesis by stimulating the
After migrating into wounds, fibroblasts commence production of basic fibroblast growth factor and vas-
the synthesis of extracellular matrix.32,34 The provi- cular endothelial growth factor by macrophages and
sional extracellular matrix is gradually replaced with endothelial cells. Activated epidermal cells of the
a collagenous matrix,32,34 perhaps as a result of the wound secrete large quantities of vascular endothelial-
action of transforming growth factor b1.32 cell growth factor.41 Basic fibroblast growth factor
Once an abundant collagen matrix has been depos- may set the stage for angiogenesis during the first
ited in the wound, the fibroblasts stop producing three days of wound repair, whereas vascular endo-
collagen, and the fibroblast-rich granulation tissue is thelial-cell growth factor is critical for angiogenesis
replaced by a relatively acellular scar. Cells in the during the formation of granulation tissue on days
wound undergo apoptosis35 triggered by unknown 4 through 7.42
signals. Dysregulation of these processes occurs in fi- In addition to angiogenesis factors, appropriate
brotic disorders such as keloid formation, morphea, extracellular matrix and endothelial receptors for the
and scleroderma. provisional matrix are necessary for angiogenesis.
Proliferating microvascular endothelial cells adjacent
Neovascularization to and within wounds transiently deposit increased
The formation of new blood vessels is necessary amounts of fibronectin within the vessel wall.43 Since
to sustain the newly formed granulation tissue. An- angiogenesis appears to require the expression of
giogenesis is a complex process that relies on extra- functional fibronectin receptors by endothelial cells,44
cellular matrix in the wound bed as well as migration the perivascular fibronectin may act as a conduit for
and mitogenic stimulation of endothelial cells.36 the movement of endothelial cells into the wound.
The induction of angiogenesis was initially attrib- Protease expression and activity are also necessary
uted to acidic or basic fibroblast growth factor. Sub- for angiogenesis.45
Vol ume 341 Numb e r 10 · 741
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Clot
Clot
Granulation tissue
Figure 3. Photomicrograph Demonstrating Reepithelialization
of a Cutaneous Wound in a Pig (Hematoxylin and Eosin, ¬40).
Epidermal cells (E) are seen dissecting under the fibrin clot
across the wound. The advancing edge of the epidermal cells is
shown with arrows. The white oval is an artifact of preparation.
The series of events leading to angiogenesis may
be as follows (Fig. 2). Injury causes destruction of
tissue and hypoxia. Angiogenesis factors such as acidic
and basic fibroblast growth factor are immediately
released from macrophages after cell disruption, and
the production of vascular endothelial-cell growth Figure 4. Photomicrograph Showing Neovascularization of a
factor by epidermal cells is stimulated by hypoxia. Cutaneous Wound in a Pig (Trichrome Stain, ¬400).
Proteolytic enzymes released into the connective tis- A new blood vessel (arrowheads) is shown sprouting into the
sue degrade extracellular-matrix proteins. Fragments fibrin clot from the granulation tissue. An endothelial cell un-
of these proteins recruit peripheral-blood mono- dergoing mitosis is seen at the interface of the clot and the
granulation tissue (arrow).
cytes to the site of injury, where they become acti-
vated macrophages and release angiogenesis factors.
Certain macrophage angiogenesis factors, such as
basic fibroblast growth factor, stimulate endothelial
cells to release plasminogen activator and procolla- matrix, and cytokines. During the second week of
genase. Plasminogen activator converts plasminogen healing, fibroblasts assume a myofibroblast pheno-
to plasmin and procollagenase to active collagenase, type characterized by large bundles of actin-contain-
and in concert these two proteases digest basement ing microfilaments disposed along the cytoplasmic
membranes. The fragmentation of the basement face of the plasma membrane of the cells and by
membrane allows endothelial cells stimulated by an- cell–cell and cell–matrix linkages.34,49 The appear-
giogenesis factors to migrate and form new blood ance of the myofibroblasts corresponds to the com-
vessels at the injured site (Fig. 4). Once the wound mencement of connective-tissue compaction and the
is filled with new granulation tissue, angiogenesis contraction of the wound. The contraction probably
ceases and many of the new blood vessels disinte- requires stimulation by transforming growth factor
grate as a result of apoptosis.46 This programmed cell b1 or b 250 and platelet-derived growth factor,51 at-
death probably is regulated by a variety of matrix tachment of fibroblasts to the collagen matrix through
molecules, such as thrombospondins 1 and 2,47 and integrin receptors,52 and cross-links between individ-
antiangiogenesis factors, such as angiostatin, endosta- ual bundles of collagen.53
tin, and angiopoietin 2.48 Collagen remodeling during the transition from
granulation tissue to scar is dependent on continued
Wound Contraction and Extracellular-Matrix synthesis and catabolism of collagen at a low rate.
Reorganization The degradation of collagen in the wound is con-
Wound contraction involves a complex and su- trolled by several proteolytic enzymes termed ma-
perbly orchestrated interaction of cells, extracellular trix metalloproteinases, which are secreted by mac-
742 · S ep tem b er 2 , 19 9 9
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
MECH A NIS MS OF D IS EAS E
rophages, epidermal cells, and endothelial cells, as ing that wound repair is the result of a complex set of
well as fibroblasts.17 The various phases of wound re- interactions among soluble cytokines, formed blood
pair rely on distinct combinations of matrix metal- elements, extracellular matrix, and cells (Table 1). It
loproteinases and tissue inhibitors of metallopro- is possible that combinations of various growth fac-
teinases.54 tors given at precisely timed intervals would be more
Wounds gain only about 20 percent of their final effective in promoting healing. Indeed, synergistic
strength in the first three weeks, during which time effects on wound repair have been demonstrated for
fibrillar collagen has accumulated relatively rapidly several growth-factor combinations.65 Among these
and has been remodeled by contraction of the wound. factors, only recombinant platelet-derived growth fac-
Thereafter the rate at which wounds gain tensile tor has been approved by the Food and Drug Ad-
strength is slow, reflecting a much slower rate of ac- ministration (FDA) for the treatment of wounds.
cumulation of collagen and, more important, collagen
remodeling with the formation of larger collagen INSIGHTS FROM FETAL WOUND HEALING
bundles and an increase in the number of intermo- Fetal wounds reepithelialize rapidly. Unlike adult
lecular cross-links.55 Nevertheless, wounds never at- epidermal cells, which resurface the wound by “crawl-
tain the same breaking strength (the tension at which ing” across it, embryonic epidermal cells are pulled
skin breaks) as uninjured skin. At maximal strength, forward by the contraction of actin fibers that draw
a scar is only 70 percent as strong as normal skin.56 the wound edges together as the opening of a purse
is closed by a purse string.66 Fetal wounds also heal
ABNORMAL WOUND HEALING without scarring. One reason for this may be the small
Although a detailed discussion of the many con- amount of transforming growth factor b1, a scar-
ditions associated with abnormal wound healing is promoting cytokine, in fetal skin. The addition of
beyond the scope of this review, several examples transforming growth factor b1 to fetal wounds results
will illustrate the multifactorial nature of these con- in scarring.67 Furthermore, fetal skin is rich in me-
ditions. Diabetic ulcers are an excellent example of talloproteinases that may promote scarless healing.68
how multiple physiologic and biochemical defects can Scarring is reduced in adult rats given neutralizing
lead to impaired healing. They usually occur in pa- antibodies to transforming growth factors b1 and b2
tients who are unable to sense and relieve cutaneous and those given transforming growth factor b3, which
pressure because of neuropathy. Ischemia secondary down-regulates the other transforming growth fac-
to vascular disease impedes healing by reducing the tor b isoforms.69 This result supports the central role
supply of oxygen and other nutrients. Diabetic ul- of transforming growth factor b1 in scar formation.
cers are also prone to infection because of impaired
granulocytic function and chemotaxis.57 Other ab- SKIN SUBSTITUTES
normalities associated with diabetic ulcers include Immediate wound coverage is one of the corner-
prolonged inflammation, impaired neovascularization, stones of wound management. Acute or chronic
decreased synthesis of collagen, increased levels of wounds can usually be covered by any of a number
proteinases, and defective macrophage function.58,59 of synthetic and natural dressings. For more exten-
Keloids and hypertrophic scars that are character- sive or recalcitrant wounds, a variety of skin substi-
ized by excess accumulation of collagen within the tutes are available (Table 2). These are of three types.
wound are examples of fibroproliferative disorders. In The first type consists of grafts of cultured epidermal
these conditions, abnormalities in cell migration and cells with no dermal components. The second type
proliferation, inflammation, synthesis and secretion has only dermal components. The third type is a bi-
of extracellular-matrix proteins and cytokines, and layer containing both dermal and epidermal elements.
remodeling of the wound matrix have all been de- Most skin substitutes do not survive indefinitely.
scribed.60 Increased activity of fibrogenic cytokines Their chief effect is to promote wound healing by
(e.g., transforming growth factor b1, insulin-like stimulating the host to produce a variety of cytokines.
growth factor 1, and interleukin-1) and exaggerated These cytokines promote healing by stimulating the
responses to these cytokines have also been noted.61,62 production of components of the basement mem-
In addition, abnormal epidermal–mesenchymal in- brane, preventing dehydration, increasing inflamma-
teractions and mutations in regulatory genes (such tion, and increasing the formation of granulation
as p53) have recently been proposed to help explain tissue. Skin substitutes are attractive alternatives to
abnormal healing.63,64 autografts, especially since they do not require pain-
ful and invasive procedures and may be used in out-
CLINICAL EXPERIENCE WITH GROWTH patients.
FACTORS
The overall clinical experience with growth factors Epidermal Skin Substitutes
and other mediators to accelerate wound healing has In 1975 wound management was revolutionized
been discouraging. This is not surprising, consider- by the development of a technique that used cul-
Vol ume 341 Numb e r 10 · 743
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
TABLE 2. SKIN SUBSTITUTES.
TYPE OF SKIN SUBSTITUTE
AND BRAND NAME* COMPONENTS ADVANTAGES DISADVANTAGES
Epidermal Cultured autologous epi- Wide and permanent skin cov- 2-to-3-week delay, high cost,
dermal cells erage fragility, labor-intensive use
Cultured allogeneic epi- Ready availability, no need for Temporary superficial cover-
dermal cells biopsy age
Dermal Cryopreserved allogeneic Ready availability, use as base Need for procurement, poten-
skin for cultured epidermal cells tial disease transmission
Alloderm Decellularized allogeneic Ready availability, inert nature, Need for procurement, poten-
human skin use as base for epidermal tial disease transmission
grafts
Integra Bovine collagen with Ready availability, possible use Need to excise wounds, risk of
chondroitin 6-sulfate of thin autograft, reduced infection, high cost
scarring
Dermagraft-TC Fibroblasts on nylon mesh Ready availability, low recur- Possible need for multiple ap-
rence of ulcers plications
Combined epidermal
and dermal
Apligraf Bovine collagen, alloge- Ready availability, no need for Limited viability
neic fibroblasts, and subsequent autografting
epidermal cells
Composite Cultured Collagen matrix substrate Ready availability, no need for Limited quantity
Skin with fibroblasts and subsequent autografting
epidermal cells
*The manufacturers are as follows: Alloderm, Life Cell, Woodlands, Tex.; Integra, Integra Life Sciences, Plainsboro,
N.J.; Dermagraft-TC, Advanced Tissue Sciences, La Jolla, Calif.; Apligraf, Organogenesis, Canton, Mass.; and Composite
Cultured Skin, Ortec International, New York.
tured human epidermal cells to form sheets suitable use is mainly limited to temporary coverage of burns,
for grafting.70 This development was soon followed skin-graft donor sites, and chronic open wounds, such
by the use of autologous cultured epidermal-cell as pressure sores and venous stasis ulcers. Unlike au-
grafts for the treatment of burns as well as other tologous grafts, they are inappropriate for permanent
acute and chronic wounds, including venous ulcers coverage of full-thickness wounds.
and junctional epidermolysis bullosa.71-73 Autologous Neonatal epidermal cells, unlike adult cells, release
grafts provide permanent coverage for large areas growth factors that stimulate other epidermal cells.78
with reasonable cosmetic results. The disadvantages Allografts of cultured neonatal foreskin cells acceler-
of these grafts include the two to three weeks need- ate healing and relieve pain in patients with acute
ed to grow enough epidermal cells, the need for skin and chronic skin ulcers.79 Patients with chronic skin
biopsies to obtain autologous donor cells, and the ulcers can be treated with fresh or cryopreserved cul-
high cost. Furthermore, success is quite variable, being tured epidermal-cell allografts with equal efficacy.80
dependent on the status of the wound, the patient’s
overall health, and the experience of the physician. Dermal Skin Substitutes
Allografts of cultured epidermal cells were devel- Inclusion of a dermal component in skin substi-
oped to avoid the long time required to produce au- tutes helps prevent wound contraction and provides
tologous grafts. In 1983 burns were successfully greater mechanical stability. Allografts of cadaver skin
treated with grafts of cultured epidermal cells from containing dermis that has been chemically treated
cadavers.74 Since then there have been many reports to remove the antigenic epidermal cellular elements
of the use of cultured epidermal cells from cadavers have been used alone or in combination with cul-
and unrelated adult donors for the treatment of tured autologous epidermal cells for closure of vari-
burns,75 skin-graft donor sites,76 and chronic leg ul- ous wounds.81
cers.77 The use of cultured allogeneic epidermal cells A composite skin graft made of a collagen-based
has resulted in wound healing without any evidence dermal lattice (containing bovine collagen and chon-
of rejection, probably because cultured epidermal droitin 6-sulfate) with an outer silicon covering has
cells do not express major histocompatibility complex been used successfully to treat burns.82 The dermal
class II HLA-DR antigens74 and are not contaminat- component is slowly degraded, and several weeks
ed with Langerhans’ cells, the antigen-presenting cells later the Silastic sheet is removed and covered with
of the epidermis.76 Since cultured epidermal-cell al- an autograft. This composite graft recently received
lografts are eventually replaced by host cells, their FDA approval for the treatment of burns. A similar
744 · S ep tem b er 2 , 19 9 9
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
MECH A NIS MS OF D IS EAS E
product, in which the Silastic outer covering is re- junctions in epithelial cells and myofibroblasts during wound healing.
J Cell Biol 1978;76:561-8.
placed with human epidermal cells and the dermal 12. Clark RAF. Fibronectin matrix deposition and fibronectin receptor ex-
component includes viable fibroblasts, has also been pression in healing and normal skin. J Invest Dermatol 1990;94:Suppl:
used successfully for burns and chronic wounds.83 128S-134S.
13. Larjava H, Salo T, Haapasalmi K, Kramer RH, Heino J. Expression of
A nylon mesh in which viable human fibroblasts integrins and basement membrane components by wound keratinoctyes.
are embedded, covered with an outer Silastic layer J Clin Invest 1993;92:1425-35.
14. Clark RAF, Ashcroft GS, Spencer M-J, Larjava H, Ferguson MWJ. Re-
to limit evaporation, has been used successfully for epithelialization of normal human excisional wounds is associated with a
temporary wound coverage after excision of burn switch from avb5 to avb6 integrins. Br J Dermatol 1996;135:46-51.
wounds.84 It has recently been approved by the FDA 15. Pilcher BK, Dumin JA, Sudbeck BD, Krane SM, Welgus HG, Parks
WC. The activity of collagenase-1 is required for keratinocyte migration on
for this indication. a type I collagen matrix. J Cell Biol 1997;137:1445-57.
16. Bugge TH, Kombrinck KW, Flick MJ, Daugherty CC, Danton MJS,
Combined Dermal and Epidermal Skin Substitutes Degen JL. Loss of fibrinogen rescues mice from the pleiotropic effects of
plasminogen deficiency. Cell 1996;87:709-19.
A composite graft consisting of type I bovine col- 17. Mignatti P, Rifkin DB, Welgus HG, Parks WC. Proteinases and tissue
lagen and live allogeneic human skin fibroblasts and remodeling. In: Clark RAF, ed. The molecular and cellular biology of
epidermal cells has been developed and used success- wound repair. 2nd ed. New York: Plenum Press, 1996:427-74.
18. Nanney LB, King LE Jr. Epidermal growth factor and transforming
fully in patients with surgical wounds85 and venous growth factor-a. In: Clark RAF, ed. The molecular and cellular biology of
ulcers.86 wound repair. 2nd ed. New York: Plenum Press, 1996:171-94.
19. Werner S, Smola H, Liao X, et al. The function of KGF in morpho-
CLINICAL IMPLICATIONS genesis of epithelium and reepithelialization of wounds. Science 1994;266:
819-22.
In general, conservative and time-honored meth- 20. Abraham JA, Klagsbrun M. Modulation of wound repair by members
of the fibroblast growth factor family. In: Clark RAF, ed. The molecular
ods of wound care should be attempted first. These and cellular biology of wound repair. 2nd ed. New York: Plenum Press,
methods are successful in the majority of patients 1996:195-248.
with skin wounds and include the use of standard 21. Clark RAF, Lanigan JM, DellaPelle P, Manseau E, Dvorak HF, Colvin
RB. Fibronectin and fibrin provide a provisional matrix for epidermal cell mi-
wound dressings, remediation of underlying prob- gration during wound reepithelialization. J Invest Dermatol 1982;79:264-9.
lems such as hyperglycemia, débridement of nonvi- 22. Hunt TK, ed. Wound healing and wound infection: theory and surgi-
cal practice. New York: Appleton-Century-Crofts, 1980.
able tissue, restoration of adequate tissue perfusion, 23. Roberts AB, Sporn MB. Transforming growth factor-b. In: Clark RAF,
limitation of pressure at the wound site, and control ed. The molecular and cellular biology of wound repair. 2nd ed. New York:
of infection. Particularly large and life-threatening Plenum Press, 1996:275-308.
24. Gray AJ, Bishop JE, Reeves JT, Laurent GJ. Aa and Bb chains of fi-
skin wounds (such as extensive burns) may require brinogen stimulate proliferation of human fibroblasts. J Cell Sci 1993;104:
the use of cultured autologous epidermal-cell grafts or 409-13.
biologic skin substitutes. There are not yet enough 25. Xu J, Clark RAF. Extracellular matrix alters PDGF regulation of fibro-
blast integrins. J Cell Biol 1996;132:239-49.
clinical data to support the routine use of growth 26. Robson MC, Phillips LG, Thomason A, Robson LE, Pierce GF. Plate-
factors or other wound mediators. However, further let-derived growth factor BB for the treatment of chronic pressure ulcers.
Lancet 1992;339:23-5.
refinement and development of substances that stim- 27. Steed DL. Clinical evaluation of recombinant human platelet-derived
ulate wound healing are likely. growth factor for the treatment of lower extremity diabetic ulcers. J Vasc
Surg 1995;21:71-8.
REFERENCES 28. Robson MC, Phillips LG, Lawrence WT, et al. The safety and effect
of topically applied recombinant basic fibroblast growth factor on the heal-
1. Brigham PA, McLoughlin E. Burn incidence and medical care use in ing of chronic pressure sores. Ann Surg 1992;216:401-6.
the United States: estimate, trends, and data sources. J Burn Care Rehabil 29. Greiling D, Clark RAF. Fibronectin provides a conduit for fibroblast
1996;17:95-107. transmigration from collagenous stroma into fibrin clot provisional matrix.
2. U.S. markets for wound management products. Irvine, Calif.: Medical J Cell Sci 1997;110:861-70.
Data International, August 1997. 30. Toole BP. Proteoglycans and hyaluronan in morphogenesis and differ-
3. Clark RAF, ed. The molecular and cellular biology of wound repair. 2nd entiation. In: Hay ED, ed. Cell biology of extracellular matrix. 2nd ed.
ed. New York: Plenum Press, 1996. New York: Plenum Press, 1991:305-41.
4. Heldin C-H, Westermark B. Role of platelet-derived growth factor 31. McClain SA, Simon M, Jones E, et al. Mesenchymal cell activation is
in vivo. In: Clark RAF, ed. The molecular and cellular biology of wound the rate-limiting step of granulation tissue induction. Am J Pathol 1996;
repair. 2nd ed. New York: Plenum Press, 1996:249-73. 149:1257-70.
5. Brown EJ. Phagocytosis. Bioessays 1995;17:109-17. 32. Clark RAF, Nielsen LD, Welch MP, McPherson JM. Collagen matrices
6. Rappolee DA, Mark D, Banda MJ, Werb Z. Wound macrophages ex- attenuate the collagen-synthetic response of cultured fibroblasts to TGF-b.
press TGF-a and other growth factors in vivo: analysis by mRNA pheno- J Cell Sci 1995;108:1251-61.
typing. Science 1988;241:708-12. 33. Vaalamo M, Mattila L, Johansson N, et al. Distinct populations of
7. Leibovich SJ, Ross R. The role of the macrophage in wound repair: a stromal cells express collagenase-3 (MMP-13) and collagenase-1 (MMP-1)
study with hydrocortisone and antimacrophage serum. Am J Pathol 1975; in chronic ulcers but not in normally healing wounds. J Invest Dermatol
78:71-100. 1997;109:96-101.
8. Riches DWH. Macrophage involvement in wound repair, remodeling, 34. Welch MP, Odland GF, Clark RAF. Temporal relationships of F-actin
and fibrosis. In: Clark RAF, ed. The molecular and cellular biology of bundle formation, collagen and fibronectin matrix assembly, and fibronectin
wound repair. 2nd ed. New York: Plenum Press, 1996:95-141. receptor expression to wound contraction. J Cell Biol 1990;110:133-45.
9. Paladini RD, Takahashi K, Bravo NS, Coulombe PA. Onset of re-epithe- 35. Desmouliere A, Redard M, Darby I, Gabbiani G. Apoptosis mediates
lialization after skin injury correlates with a reorganization of keratin fila- the decrease in cellularity during the transition between granulation tissue
ments in wound edge keratinocytes: defining a potential role for keratin and scar. Am J Pathol 1995;146:56-66.
16. J Cell Biol 1996;132:381-97. 36. Madri JA, Sankar S, Romanic AM. Angiogenesis. In: Clark RAF, ed.
10. Goliger JA, Paul DL. Wounding alters epidermal connexin expression The molecular and cellular biology of wound repair. 2nd ed. New York:
and gap junction-mediated intercellular communication. Mol Biol Cell Plenum Press, 1996:355-71.
1995;6:1491-501. 37. Folkman J, D’Amore PA. Blood vessel formation: what is its molecular
11. Gabbiani G, Chaponnier C, Huttner I. Cytoplasmic filaments and gap basis? Cell 1996;87:1153-5.
Vol ume 341 Numb e r 10 · 745
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
38. Iruela-Arispe ML, Dvorak HF. Angiogenesis: a dynamic balance of I and III collagen and transforming growth factor-beta 1 mRNA and pro-
stimulators and inhibitors. Thromb Haemost 1997;78:672-7. tein in hypertrophic burn scar. J Invest Dermatol 1995;104:750-4.
39. Risau W. Mechanisms of angiogenesis. Nature 1997;386:671-4. 63. Saed GM, Ladin D, Olson J. Analysis of p53 gene mutations in keloids
40. Detmar M, Brown LF, Berse B, et al. Hypoxia regulates the expression using polymerase chain reaction-based single-strand conformational poly-
of vascular permeability factor/vascular endothelial growth factor (VPF/ morphism and DNA sequencing. Arch Dermatol 1998;134:963-7.
VEGF) and its receptors in human skin. J Invest Dermatol 1997;108:263-8. 64. Machesney M, Tidman N, Waseem A, Kirby L, Leigh I. Activated ke-
41. Brown LF, Yeo K-T, Berse B, et al. Expression of vascular permeability ratinocytes in the epidermis of hypertrophic scars. Am J Pathol 1998;152:
factor (vascular endothelial growth factor) by epidermal keratinocytes dur- 1133-41.
ing wound healing. J Exp Med 1992;176:1375-9. 65. Pierce GF, Mustoe TA. Pharmacologic enhancement of wound heal-
42. Nissen NN, Polverini PJ, Koch AE, Volin MV, Gamelli RL, DiPietro ing. Annu Rev Med 1995;46:467-81.
LA. Vascular endothelial growth factor mediates angiogenic activity during 66. Martin P, Lewis J. Actin cables and epidermal movement in embryonic
the proliferative phase of wound healing. Am J Pathol 1998;152:1445-52. wound healing. Nature 1992;360:179-83.
43. Clark RAF, Quinn JH, Winn HJ, Lanigan JM, Dellepelle P, Colvin 67. Sullivan KM, Lorenz HP, Meuli M, Lin RY, Adzick NS. A model of
RB. Fibronectin is produced by blood vessels in response to injury. J Exp scarless human fetal wound repair is deficient in transforming growth factor
Med 1982;156:646-51. beta. J Pediatr Surg 1995;30:198-203.
44. Brooks PC, Clark RAF, Cheresh DA. Requirement of vascular integrin 68. Bullard KM, Cass DL, Banda MJ, Adzick NS. Transforming growth
avb3 for angiogenesis. Science 1994;264:569-71. factor beta-1 decreases interstitial collagenase in healing human fetal skin.
45. Pintucci G, Bikfalvi A, Klein S, Rifkin DB. Angiogenesis and the fi- J Pediatr Surg 1997;32:1023-7.
brinolytic system. Semin Thromb Hemost 1996;22:517-24. 69. Shah M, Foreman DM, Ferguson MWJ. Neutralisation of TGF-b1 and
46. Ilan N, Mahooti S, Madri JA. Distinct signal transduction pathways TGF-b2 or exogenous addition of TGF-b3 to cutaneous rat wounds re-
are utilized during the tube formation and survival phases of in vitro an- duces scarring. J Cell Sci 1995;108:985-1002.
giogenesis. J Cell Sci 1998;111:3621-31. 70. Rheinwald JG, Green H. Serial cultivation of strains of human epider-
47. Guo N, Krutzsch HC, Inman JK, Roberts DD. Thrombospondin 1 mal keratinocytes: the formation of keratinizing colonies from single cells.
and type I repeat peptides of thrombospondin 1 specifically induce apop- Cell 1975;6:331-43.
tosis of endothelial cells. Cancer Res 1997;57:1735-42. 71. Grafting of burns with cultured epithelium prepared from autologous
48. Folkman J. Angiogenesis and angiogenesis inhibition: an overview. epidermal cells. Lancet 1981;1:75-8.
EXS 1997;79:1-8. 72. Hefton JM, Caldwell D, Biozes DG, Balin AK, Carter DM. Grafting
49. Desmoulière A, Gabbiani G. The role of the myofibroblast in wound of skin ulcers with cultured autologous epidermal cells. J Am Acad Derma-
healing and fibrocontractive diseases. In: Clark RAF, ed. The molecular tol 1986;14:399-405.
and cellular biology of wound repair. 2nd ed. New York: Plenum Press, 73. Rue LW III, Cioffi WG, McManus WF, Pruitt BA Jr. Wound closure
1996:391-423. and outcome in extensively burned patients treated with cultured autolo-
50. Montesano R, Orci L. Transforming growth factor-b stimulates col- gous keratinocytes. J Trauma 1993;34:662-8.
lagen-matrix contraction by fibroblasts: implications for wound healing. 74. Hefton JM, Madden MR , Finkelstein JL, Shires GT. Grafting of burn
Proc Natl Acad Sci U S A 1988;85:4894-7. patients with allografts of cultured epidermal cells. Lancet 1983;2:428-30.
51. Clark RAF, Folkvord JM, Hart CE, Murray MJ, McPherson JM. Plate- 75. Madden MR , Finkelstein JL, Staiano-Coico L, et al. Grafting of cul-
let isoforms of platelet-derived growth factor stimulate fibroblasts to con- tured allogeneic epidermis on second- and third-degree burn wounds on
tract collagen matrices. J Clin Invest 1989;84:1036-40. 26 patients. J Trauma 1986;26:955-62.
52. Schiro JA, Chan BMC, Roswit WT, et al. Integrin a2b1 (VLA-2) me- 76. Thivolet J, Faure M, Demidem A, Mauduit G. Long-term survival and
diates reorganization and contraction of collagen matrices by human cells. immunological tolerance of human epidermal allografts produced in cul-
Cell 1991;67:403-10. ture. Transplantation 1986;42:274-80.
53. Woodley DT, Yamauchi M, Wynn KC, Mechanic G, Briggaman RA. 77. Leigh IM, Purkis PE, Navsaria HA, Phillips TJ. Treatment of chronic
Collagen telopeptides (cross-linking sites) play a role in collagen gel lattice venous ulcers with sheets of cultured allogenic keratinocytes. Br J Derma-
contraction. J Invest Dermatol 1991;97:580-5. tol 1987;117:591-7.
54. Madlener M, Parks WC, Werner S. Matrix metalloproteinases (MMPs) 78. Gilchrest BA, Karassik RL, Wilkins LM, Vrabel MA, Maciag T. Auto-
and their physiological inhibitors (TIMPs) are differentially expressed dur- crine and paracrine growth stimulation of cells derived from human skin.
ing excisional skin wound repair. Exp Cell Res 1998;242:201-10. J Cell Physiol 1983;117:235-40.
55. Bailey AJ, Bazin S, Sims TJ, Le Lous M, Nicholetis C, Delaunay A. 79. Phillips TJ, Kehinde O, Green H, Gilchrest BA. Treatment of skin ulcers
Characterization of the collagen of human hypertrophic and normal scars. with cultured epidermal allografts. J Am Acad Dermatol 1989;21:191-9.
Biochim Biophys Acta 1975;405:412-21. 80. Teepe RGC, Koebrugge EJ, Ponec M, Vermeer BJ. Fresh versus cryo-
56. Levenson SM, Geever EF, Crowley LV, Oates JF III, Berard CW, Ros- preserved cultured allografts for the treatment of chronic skin ulcers. Br J
en H. The healing of rat skin wounds. Ann Surg 1965;161:293-308. Dermatol 1990;122:81-9.
57. Nolan CM, Beaty HN, Bagdade JD. Further characterization of the 81. Cuono C, Langdon R , McGuire J. Use of cultured epidermal au-
impaired bactericidal function of granulocytes in patients with poorly con- tografts and dermal allografts as skin replacement after burn injury. Lancet
trolled diabetes. Diabetes 1978;27:889-94. 1986;1:1123-4.
58. Fahey TJ III, Sadaty A, Jones WG II, Barber A, Smoller B, Shires GT. 82. Heimbach D, Luterman A, Burke J, et al. Artificial dermis for major
Diabetes impairs the late inflammatory response to wound healing. J Surg burns: a multi-center randomized clinical trial. Ann Surg 1988;208:313-20.
Res 1991;50:308-13. 83. Boyce ST, Glatter R, Kitzmiller WJ. Treatment of chronic wounds with
59. Loots MA. Differences in cellular infiltrate and extracellular matrix of cultured skin substitutes: a pilot study. Wounds 1995;7:24-9.
chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol 84. Purdue GF. Dermagraft-TC pivotal efficacy and safety study. J Burn
1998;111:850-7. Care Rehabil 1997;18:S13-S14.
60. Tredget EF, Nedelec B, Scott PG, Ghahary A. Hypertrophic scars, ke- 85. Eaglstein WH, Iriondo M, Laszlo K. A composite skin substitute
loids, and contractures: the cellular and molecular basis for therapy. Surg (graftskin) for surgical wounds: a clinical experience. Dermatol Surg 1995;
Clin North Am 1997;77:701-30. 21:839-43.
61. Babu M, Diegelmann R, Oliver N. Keloid fibroblasts exhibit an altered 86. Falanga V, Margolis D, Alvarez O, et al. Rapid healing of venous ulcers
response to TGF-beta. J Invest Dermatol 1992;99:650-5. and lack of clinical rejection with an allogeneic cultured human skin equiv-
62. Zhang K, Garner W, Cohen L, Rodriguez J, Phan S. Increased types alent. Arch Dermatol 1998;134:293-300.
746 · S ep tem b er 2 , 19 9 9
Downloaded from www.nejm.org by MARTIN BRAND MD on December 28, 2007 .
Copyright © 1999 Massachusetts Medical Society. All rights reserved.
You might also like
- Abd 91 05 0614Document7 pagesAbd 91 05 0614Selvy Anriani GasperszNo ratings yet
- Tissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDDocument10 pagesTissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDAmith HadhimaneNo ratings yet
- Manejo de HeridasDocument17 pagesManejo de HeridassaortizpNo ratings yet
- A Practical Guide To Wound Healing: Learning ObjectivesDocument15 pagesA Practical Guide To Wound Healing: Learning ObjectivesVanessaGGSNo ratings yet
- Cellular Human Tissue-Engineered Skin Substitutes Investigated For Deep and Dif Ficult To Heal InjuriesDocument23 pagesCellular Human Tissue-Engineered Skin Substitutes Investigated For Deep and Dif Ficult To Heal InjuriesNovelas, Series y PelículasNo ratings yet
- Review Article: Nanotechnology-Based Therapies For Skin Wound RegenerationDocument12 pagesReview Article: Nanotechnology-Based Therapies For Skin Wound RegenerationDina Arwina DalimuntheNo ratings yet
- Wound HealingDocument2 pagesWound HealingChoon Jin NgNo ratings yet
- Growth Factors and Cytokines in Wound HealingDocument17 pagesGrowth Factors and Cytokines in Wound HealingCitra AryantiNo ratings yet
- Wound Healing and Perioperative Care Vol 18 Issue 1 Feb 2006 Omfs PDFDocument7 pagesWound Healing and Perioperative Care Vol 18 Issue 1 Feb 2006 Omfs PDFR KNo ratings yet
- Principles of Wound HealingDocument28 pagesPrinciples of Wound HealingRafael BagusNo ratings yet
- Pathophysiology of Hypertrophic ScarsDocument15 pagesPathophysiology of Hypertrophic ScarsLarashati Putri WijayaNo ratings yet
- Rebuilding Human Ability To Regenerate Cells Inhibiting Anatomical Growth During Early Embryonic StageDocument8 pagesRebuilding Human Ability To Regenerate Cells Inhibiting Anatomical Growth During Early Embryonic StageInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 3a. Wound HealingDocument37 pages3a. Wound HealingOlivia Avriyanti HanafiahNo ratings yet
- Mucosal wound repair role of immune-epithelial interactionsDocument10 pagesMucosal wound repair role of immune-epithelial interactionsBrilliantNo ratings yet
- Leoni 2015Document10 pagesLeoni 2015Yunita SaharawatiNo ratings yet
- Wound HealingDocument15 pagesWound HealingfgrehNo ratings yet
- Relation Between Hypothermia and SSIDocument7 pagesRelation Between Hypothermia and SSIRekkiNo ratings yet
- Chronic WoundsDocument7 pagesChronic WoundstaniaNo ratings yet
- Wound Healing: Ziv Peled, M.DDocument8 pagesWound Healing: Ziv Peled, M.Dapi-26007957No ratings yet
- Wound Healing and Its Impairment in The Diabetic Foot: ReviewDocument9 pagesWound Healing and Its Impairment in The Diabetic Foot: ReviewJoey TsaiNo ratings yet
- Wound Healing in The Oral Mucosa: Patricio C. Smith and Constanza MartínezDocument14 pagesWound Healing in The Oral Mucosa: Patricio C. Smith and Constanza MartínezNadira NurinNo ratings yet
- Wound Healing and Dental Therapies Repair and RegenerationDocument44 pagesWound Healing and Dental Therapies Repair and RegenerationAthenaeum Scientific PublishersNo ratings yet
- The Basic Science of Wound Healing: SummaryDocument23 pagesThe Basic Science of Wound Healing: SummaryKevin AdrianNo ratings yet
- 0003IADDocument12 pages0003IADRika AzyenelaNo ratings yet
- Normal and Diabetic Wound Healing Macrophage-Mediated Inflammation inDocument9 pagesNormal and Diabetic Wound Healing Macrophage-Mediated Inflammation inNanang Miftah FajariNo ratings yet
- Management of Ocular Adnexal TraumaDocument21 pagesManagement of Ocular Adnexal TraumamariaNo ratings yet
- Wound Healing, or Wound Repair, Is An Intricate Process in Which The Skin (OrDocument20 pagesWound Healing, or Wound Repair, Is An Intricate Process in Which The Skin (OrDeepak AhujaNo ratings yet
- Stem CellDocument14 pagesStem CellsattwikaNo ratings yet
- Kumar - What Is The New Wound HealingDocument14 pagesKumar - What Is The New Wound HealingDiana CerveraNo ratings yet
- 0003iad PDFDocument12 pages0003iad PDFASTY AZZAHRANo ratings yet
- Wound Healing )Document14 pagesWound Healing )miftahuldursinaNo ratings yet
- Factors Affecting Wound HealingDocument11 pagesFactors Affecting Wound HealingFredy Rodeardo MaringgaNo ratings yet
- NIH Public Access: Inflammation and Wound Healing: The Role of The MacrophageDocument14 pagesNIH Public Access: Inflammation and Wound Healing: The Role of The MacrophageSigit Harya HutamaNo ratings yet
- Martin Paul PDFDocument8 pagesMartin Paul PDFSteven NoriegaNo ratings yet
- The Practice and Science of Wound Healing History and Physiology of Wound HealingDocument5 pagesThe Practice and Science of Wound Healing History and Physiology of Wound HealingscrewdriverNo ratings yet
- wrr.12952Document14 pageswrr.12952randomaeiou7273No ratings yet
- The L PRF MembraneDocument11 pagesThe L PRF Membraneanh le ducNo ratings yet
- Stechmiller JK. Understanding The Role of Nutrition and Wound Healing. Nutr Clin PractDocument8 pagesStechmiller JK. Understanding The Role of Nutrition and Wound Healing. Nutr Clin PractOctavianus KevinNo ratings yet
- WOUND HEALING: A COMPLEX PROCESSDocument35 pagesWOUND HEALING: A COMPLEX PROCESSGayathri MaigandanNo ratings yet
- 7ads4663 74663 IJPapprovedDocument13 pages7ads4663 74663 IJPapprovedIndra HedarNo ratings yet
- Wound Healing Phases and ProcessesDocument24 pagesWound Healing Phases and ProcessesSrishti SrivastavaNo ratings yet
- International Immunopharmacology: SciencedirectDocument10 pagesInternational Immunopharmacology: SciencedirectRohadatul AisyNo ratings yet
- Wounds Biology Pathology and ManagementDocument13 pagesWounds Biology Pathology and ManagementChilo PrimaNo ratings yet
- Healing and Repair Flash PointsDocument3 pagesHealing and Repair Flash PointsHassan AhmadNo ratings yet
- Biomaterials in Wound Healing PDFDocument11 pagesBiomaterials in Wound Healing PDFshubhamNo ratings yet
- Cardio CuracionDocument11 pagesCardio Curacionapi-613248156No ratings yet
- Cellular and Molecular Mechanisms of FibrosisDocument20 pagesCellular and Molecular Mechanisms of FibrosisJason KothNo ratings yet
- Angio GenesisDocument8 pagesAngio GenesisSamarTharwatNo ratings yet
- Macrophages - A Review of Their Role in Wound Healing and Their Therapeutic UseDocument17 pagesMacrophages - A Review of Their Role in Wound Healing and Their Therapeutic UseklaumrdNo ratings yet
- Balsa 2015Document17 pagesBalsa 2015Pipe VodNo ratings yet
- Molecular Aspects of Medicine: Ralf Weiskirchen, Sabine Weiskirchen, Frank TackeDocument14 pagesMolecular Aspects of Medicine: Ralf Weiskirchen, Sabine Weiskirchen, Frank TackeEvy YuliantiNo ratings yet
- The Roles of in Ammation in Keloid and Hypertrophic ScarsDocument10 pagesThe Roles of in Ammation in Keloid and Hypertrophic ScarsireneardianiNo ratings yet
- Wound Healing and Its Impairment in The Diabetic Foot: ReviewDocument8 pagesWound Healing and Its Impairment in The Diabetic Foot: ReviewSuzana PoloncaNo ratings yet
- Referencia 3Document10 pagesReferencia 3Ulises MattoNo ratings yet
- Basic Science of Wound HealingDocument4 pagesBasic Science of Wound HealingMarnia SulfianaNo ratings yet
- GROUP6Document22 pagesGROUP6AYUSHI PATELNo ratings yet
- Chronic Wound Evaluation and Differential DiagnosisDocument17 pagesChronic Wound Evaluation and Differential DiagnosisVar AndaNo ratings yet
- Page 1 of 12: Surgery A Wound Healing Phases of Wound HealingDocument12 pagesPage 1 of 12: Surgery A Wound Healing Phases of Wound Healingrjh1895No ratings yet
- The Role of Phytochemicals in The Inflammatory Phase of Wound HealingDocument17 pagesThe Role of Phytochemicals in The Inflammatory Phase of Wound Healingfahira septianiNo ratings yet
- TRIX-8: Multi-Use Temperature LoggerDocument2 pagesTRIX-8: Multi-Use Temperature LoggerarseniosilvaNo ratings yet
- Neurips 2019Document70 pagesNeurips 2019arseniosilvaNo ratings yet
- Icml 2019Document87 pagesIcml 2019arseniosilvaNo ratings yet
- Icml 2019Document87 pagesIcml 2019arseniosilvaNo ratings yet
- Gold 2020 Report Ver1.0wmsDocument141 pagesGold 2020 Report Ver1.0wmsRoxana GonzalezNo ratings yet
- Prevention Guidelines Made SimpleDocument17 pagesPrevention Guidelines Made SimplearseniosilvaNo ratings yet
- 10 1 1 473 9492 PDFDocument9 pages10 1 1 473 9492 PDFarseniosilvaNo ratings yet
- 03 Brain BasicsDocument25 pages03 Brain BasicsarseniosilvaNo ratings yet
- Neonatal Stomach Volume and Physiology Suggest Feeding at 1-h IntervalsDocument5 pagesNeonatal Stomach Volume and Physiology Suggest Feeding at 1-h IntervalsarseniosilvaNo ratings yet
- Phrasalverbs 160428081515 PDFDocument42 pagesPhrasalverbs 160428081515 PDFarseniosilvaNo ratings yet
- Chapter 11 Lung Cancer PDFDocument12 pagesChapter 11 Lung Cancer PDFFirah Triple'sNo ratings yet
- Phrasal verbs and templatesDocument38 pagesPhrasal verbs and templatesAlina AlinaNo ratings yet
- Basic Phrasal Verbs With Pictures and SynonymsDocument42 pagesBasic Phrasal Verbs With Pictures and SynonymsarseniosilvaNo ratings yet
- Conciliar Post Reference GuideDocument9 pagesConciliar Post Reference GuideBenjamin WinterNo ratings yet
- TELENGANA BUSINESS DIRECTORY PENEL D-PanelDocument65 pagesTELENGANA BUSINESS DIRECTORY PENEL D-Panelamandeep100% (4)
- CS 401 Artificial Intelligence: Zain - Iqbal@nu - Edu.pkDocument40 pagesCS 401 Artificial Intelligence: Zain - Iqbal@nu - Edu.pkHassan RazaNo ratings yet
- FisikaDocument46 pagesFisikaNurol Hifzi Putri RizkiNo ratings yet
- Cyber Crime and Law ClassDocument99 pagesCyber Crime and Law ClassMohd ShifanNo ratings yet
- Kundalini Reiki Manual: Paul CrickDocument17 pagesKundalini Reiki Manual: Paul CrickKkkk100% (1)
- Human Rights EducationDocument149 pagesHuman Rights EducationLeonard MamergaNo ratings yet
- Juice in PakistanDocument9 pagesJuice in Pakistanrize1159100% (1)
- Report For Court, Sale of Dowling College Brookhaven CampusDocument26 pagesReport For Court, Sale of Dowling College Brookhaven CampusRiverheadLOCALNo ratings yet
- Ch01 Standard Methods and PractisesDocument44 pagesCh01 Standard Methods and PractisesUsman FarooqNo ratings yet
- Linear Programming Evaluation of Feeds pH and AcidityDocument5 pagesLinear Programming Evaluation of Feeds pH and AcidityAugust Ridlof RiwuNo ratings yet
- Access 2013 Beginner Level 1 Adc PDFDocument99 pagesAccess 2013 Beginner Level 1 Adc PDFsanjanNo ratings yet
- 1562229628974192Document33 pages1562229628974192Phuong NgocNo ratings yet
- Hubspot Architecture Practicum Workbook: ObjectiveDocument4 pagesHubspot Architecture Practicum Workbook: Objectivecamilo.salazarNo ratings yet
- Micro-Finance: 16 Principles of Grameen BankDocument5 pagesMicro-Finance: 16 Principles of Grameen BankHomiyar TalatiNo ratings yet
- Swift Group Technical HandbookDocument8 pagesSwift Group Technical HandbookLukasz WilkNo ratings yet
- (RHSA 124) : Monitoring and Managing Linux ProcessesDocument56 pages(RHSA 124) : Monitoring and Managing Linux ProcessesRomeo SincereNo ratings yet
- Human, AGV or AIV? An Integrated Framework For Material Handling System Selection With Real-World Application in An Injection Molding FacilityDocument10 pagesHuman, AGV or AIV? An Integrated Framework For Material Handling System Selection With Real-World Application in An Injection Molding FacilitymertikNo ratings yet
- Women in PoliticsDocument13 pagesWomen in PoliticsMusa M. KamaraNo ratings yet
- Videoteca - Daniel Haddad (March 2019)Document8 pagesVideoteca - Daniel Haddad (March 2019)Daniel HaddadNo ratings yet
- Types of EquityDocument2 pagesTypes of EquityPrasanthNo ratings yet
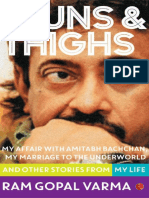
- Guns and Thighs by Ram Gopal Verma PDFDocument100 pagesGuns and Thighs by Ram Gopal Verma PDFSoma ShekharNo ratings yet
- Is 5312 1 2004Document13 pagesIs 5312 1 2004kprasad_56900No ratings yet
- JPT Jan 2013Document119 pagesJPT Jan 2013Maryam IslamNo ratings yet
- 9331 DCCBDocument5 pages9331 DCCBgopimodalavalasaNo ratings yet
- Three Days To SeeDocument2 pagesThree Days To SeeMae MejaresNo ratings yet
- Techniques To Prevent Food SpoilageDocument30 pagesTechniques To Prevent Food SpoilageCourtney GrahamNo ratings yet
- 411 PS1 2018 AnsDocument3 pages411 PS1 2018 AnsAlbertus MuheuaNo ratings yet
- June 10Document16 pagesJune 10rogeliodmngNo ratings yet