Professional Documents
Culture Documents
Effects of Respiratory Interval On Vagal Modulation of Heart Rate
Uploaded by
Guillermo Castro ContardoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effects of Respiratory Interval On Vagal Modulation of Heart Rate
Uploaded by
Guillermo Castro ContardoCopyright:
Available Formats
Effects of respiratory interval on vagal
modulation of heart rate
JUNICHIRO HAYANO, SEIJI MUKAI, MASAHITO SAKAKIBARA,
AKIYOSHI OKADA, KAZUY-UKI TAKATA, AND TAKAO FUJINAMI
Third Department of Internal Medicine, Nagoya City University Medical School,
Nagoya 467; Department of Psychology, Aichi Gakuin University, Aichi 470-01;
and Toyota College of Technology, Toyota 471, Japan
Hayano, Junichiro, Seiji Mukai, Masahito Sakaki- the HF amplitude of HRV and cardiac vagal tone in
bara, Akiyoshi Okada, Kazuyuki Takata, and Takao humans. The HF amplitude was assessedby autoregres-
Fujinami. Effects of respiratory interval on vagal modulation sive power spectral analysis, with the mean R-R interval
of heart rate. Am. J. Physiol. 267 (Heart Circ. PhysioZ. 36): of electrocardiogram (ECG) under complete P-adrener-
H33-H40, 1994.-To determine whether paced breathing gic blockade being taken as the measure of mean cardiac
(PB) and respiratory interval of PB modify the relationship
between spectral components of heart rate variability (HRV) vagal tone. Although the respiratory interval was con-
and cardiac vagal tone, we studied seven healthy young males trolled by the paced-breathing technique, this technique
under the condition of P-adrenergic blockade by intravenous has been reported to enhance cardiac vagal tone, based
propranolol(0.2 mg/kg). Compared with spontaneous breath- on the observation that paced breathing increases the
ing, PB at the same respiratory interval as that of individual relative power of the HF component to the total power of
spontaneous breathing showed no significant effect on the HRV (20, 23). Thus we also evaluated the effects of
amplitude of the high-frequency (HF) component or the mean paced breathing at the same respiratory interval as that
R-R interval in either the supine or tilt position, whereas the of individual spontaneous breathing on mean cardiac
PB decreased the amplitude of the low-frequency (LF; 0.04- vagal tone.
0.15 Hz) component in both positions (P = 0.004 and 0.042,
respectively). When the respiratory interval was increased METHODS
from 3 to 6 s, the HF amplitude showed a progressive increase
in both positions (P = 0.001 and 0.035, respectively), while the Subjects. We studied nine nonsmoking male medical stu-
LF amplitude and mean R-R interval remained unchanged. dents. All subjects were screened by careful medical history
These results indicate that the effects of PB and respiratory taking, physical examination, routine laboratory tests, chest
interval on the spectral components of HRV are not mediated X-ray, and resting and exercise ECG to ensure that they were
by the changes in mean cardiac vagal tone and support the in good health and without cardiovascular disease, pulmonary
hypothesis that increased respiratory interval amplifies the disease, diabetes mellitus, or uremia. No subject took any
respiratory-related vagal modulation of heart rate. medications during the 3-wk period before the study. Two of
the subjects were subsequently excluded from the study
heart rate variability; respiratory sinus arrhythmia; power because of development of a sign or symptom of presyncope
spectrum analysis; respiration; head-up tilt; humans during a tilt test in this study. The mean age of the remaining
seven subjects was 23 t 2 (SD) yr. All subjects gave their
written informed consent, and the procedure was performed
according to Nagoya City University Medical School’s ethical
ANALYSIS OF HEART RATE VARIABILITY (HRV) has been guidelines.
widely used as an assessment of autonomic activity, Study design. This study was designed to examine the
particularly of cardiac vagal tone (3, 5, 29), but limita- effects of paced breathing and respiratory interval under four
tions of this method in humans have also been reported different conditions, i.e., combinations among two postures
(6, 11, 19). Most of the criticism seems to focus on the (supine and 70” head-up tilt) and two drug treatments (control
influences of the respiratory parameters on the high- and propranolol). The effects of the paced breathing were
frequency (HF, > 0.15 Hz) component of HRV, which evaluated in the contrast between spontaneous breathing and
paced breathing at the same respiratory interval as that of
corresponds to respiratory sinus arrhythmia (RSA). The
individual spontaneous breathing. The paced breathing was
HF component, or RSA, has been known to result from also performed at respiratory intervals of 3, 4, 5, and 6 s. The
respiratory-related vagal modulation of heart rate (4, 5, order of the drug treatments was randomized among subjects,
7, 24-26), and the amplitude has been demonstrated to although data were collected first in the supine position in all
correlate with cardiac vagal tone (5, 8, 10, 15, 18). subjects. The spontaneous respiratory interval was deter-
However, it has also been well recognized that the mined individually in each of the four different conditions, and
amplitude decreases with respiratory frequency and therefore, data were always collected first under spontaneous
increases with tidal volume (2, 6, 8, 11, 13, 17, 22, 26, breathing followed by the paced breathing. The order of
27). Furthermore, controversy remains as to whether different respiratory intervals of the paced breathing was
randomized among subjects but was fixed within each subject.
these changes in the amplitude along with the respira-
ProtocoZ. Experiments under the two drug conditions were
tory parameters are mediated by the changes in the
performed on different days at an interval of 1 wk. For both
mean level of cardiac vagal tone or by the changes in the days, subjects were instructed not to consume food or bever-
magnitude of respiratory-related vagal modulation of ages containing caffeine or alcohol after 2100 h the previous
heart rate (11,19,20). night. Subjects were studied in an air-conditioned laboratory
This study aimed to examine whether or not the (24°C) between 1000 and 1500 h more than 3 h after a light
respiratory interval modifies the relationship between meal.
0363-6135/94 $3.00 Copyright o 1994 the American Physiological Society H33
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
H34 RESPIRATION AND VAGAL MODULATION OF HR
A SB Pe 4.7 s PB3s P04s PB 5 s PB 6 s
1200 - 0.21 Hz 0.21 Hz 0.33 Hz 0.23 Hz 0.20 Hz 0.17 Hz
YG
>
5 ;
E E 9so-
t*Iynuh,ww-mrhyIM(u
rr-
k
TOO-: , , , 1 1 1 1 1 T 1 1 1 1 T 1 1 1 1 1 1
0 5 10 15 Time (min) 20
01234501234501234501234501 2345012345
Frequency (1 QHz)
1100 - SB PB 7.7 s -3s PB 4 s PB 5 s PB 6 s
ii2 0.13 Hz 0.13 Hz 0.33 Hz 0.25 Hz 0.20 Hz 0.17 Hz
4) ‘si
z E850
w~me-w
a:-
a;:
01234501 234501234501234501 2345012345
Frequency (1 OHz)
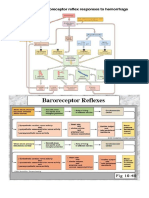
Fig. 1. Changes in R-R interval and autoregressive power spectra of R-R interval variability during spontaneous
breathing (SB) and paced breathing (PB) in a representative subject under P-adrenergic blockade caused by
propranolol (0.2 mg/kg). Paced breathing was performed at different respiratory intervals between 3 and 6 s,
including same interval as that of spontaneous breathing in supine (A) and 70” head-up tilt (B) positions. PSD, power
spectral density.
Before the experiment, subjects practiced paced breathing. Colin Electronics, Komaki, Japan) was recorded from the
We developed a computer program that generates an audio radial artery of the left arm that was supported by a side board
signal consisting of high (880 Hz)- and low (440 Hz)-pitched attached to the table.
sounds, which appeared alternatively at a programmable After 30 min of supine rest, propranolol (0.2 mg/ kg) was
interval. Subjects were instructed to breathe in when hearing injected intravenously over 5 min in the P-adrenergic blockade
the high-pitched sound (880 Hz) and to breathe out during the condition, while the same volume of saline was injected in the
low-pitched sound (440 Hz). The durations of inspiratory and control condition. After a 5min equilibrium period, data were
expiratory phases were set at an equal length (50: 50 inspiration- collected for 3 min under spontaneous breathing in the supine
to-expiration ratio). Subjects were instructed to adjust their position while subjects were resting quietly. The power spec-
tidal volume to a comfortable level according to the changes in trum of the respiratory waveform during this period was then
respiratory interval from 3 to 6 s. They continued the training immediately obtained, and the spontaneous respiratory inter-
until they were familiar with this maneuver, and all subjects val was determined from the mean respiratory frequency. The
became able to breathe comfortably in synchrony with the spectral analysis of respiratory waveform was performed by
audio signal at all of these respiratory intervals.
the same method as that used for spectral analysis of R-R
Subjects were placed on a tilt table and supported by a foot
interval described below, except that the order of autoregres-
rest. ECG (CM5 lead) and uncalibrated impedance spirogram
(AI-601G; Nihon Koden, Tokyo, Japan) were recorded continu- sive model was determined simply by Akaike’s final prediction
ously on a frequency-modulated tape recorder (MR-30; Teat, error criteria (1).
Tokyo, Japan). Transcutaneous PO, and PCO, (OKV-7101; Paced breathing sessions (4 min each) were performed at
Nihon Koden) were monitored in four subjects under both the five different respiratory intervals, the spontaneous respira-
control and P-adrenergic blockade conditions. For on-line tory interval and 3, 4, 5, and 6 s, in a randomized order. Each
measurement of spontaneous respiratory interval, the respira- session was followed by a 1-min rest period, during which
tory waveform was also supplied directly to a microcomputer subjects breathed spontaneously.
(PC9801EX; NE@, Tokyo, Japan), on which the data were Subjects were then tilted to the 70” head-up position. After 2
digitized at 2 Hz using an analog-to-digital converter (ADX- min, data were collected for spontaneous breathing session in
98E; Canopus Electronics, Kobe, Japan) and stored in memory. the head-up tilt position. The spontaneous respiratory interval
For the purpose of other studies, noninvasive continuous was determined, and paced breathing was performed in the
blood pressure by means of arterial tonometry (CBM-7000; same procedure as in the supine position.
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
RESPIRATION AND VAGAL MODULATION OF HR H35
Data analysis. The ECG data were played back from the 100
frequency-modulated tape and digitized at 1 kHz by an A
s
analog-to-digital converter (ADX-98E; Canopus Electronics) N
and analyzed on a microcomputer (PC-9801DA; NEC). The
temporal positions of all R-wave peaks were determined by a
fast peak detection algorithm. The original ECG waveform
with markers indicating the positions of detected R-wave
peaks was completely scanned on display, all ectopic beats
were checked, and any errors in R-wave detection were edited
manually. No subject presented any ectopic beats during the
experiment. All R-R intervals were measured, and the mean
R-R interval during each experimental session was calculated.
The beat-to-beat R-R intervals were then interpolated by cubic
spline function and resampled at 1 Hz, yielding an equidis- PB
tantly sampled R-R interval function.
Autoregressive power spectrum analysis was performed on 6
the R-R interval function during the last 3 min in each 4-min
session. The magnitude
frequency
and center frequency
(LF) and HF components
of the low-
of the R-R interval 1-1 SUPINE o
1
1
T
/
variability were assessed. The detail of this method has been
reported elsewhere (14- 16). Briefly, the autoregressive model
order was determined by Akaike’s final prediction error crite-
ria (l), but when the criteria provided an order of < 14, 14 was
used to obtain well-defined peaks for the LF and HF compo-
nents (9). Autoregressive coefficients were computed using the
Marple algorithm (2 1). Spectral decomposition was accom-
plished by means of an algorithm based on residual integration
(30), and the power and center frequency of individual spec-
0
trum components were determined. We defined the HF compo-
nents as the center frequency of the spectral component being SB PB SB PB
Fig. 2. Effects of paced breathing (PB) on mean R-R interval, mean
equal to the respiratory frequency corresponding to respira-
amplitude of high-frequency (HF) and low-frequency (LF) compo-
tory interval in each experimental session. The LF component nents, and LF/HF of heart rate variability in 7 young healthy male
was defined as the center frequency of the component being subjects under P-adrenergic blockade. Paced breathing was performed
between 0.04 and 0.15 Hz when the respiratory frequency was at same respiratory interval as that of individual spontaneous breath-
> 0.15 Hz, and between 0.04 Hz and the respiratory frequency ing (SB) in each of supine and head-up tilt positions.
when the respiratory frequency was 5 0.15 Hz.
In this study, the magnitudes of the LF and HF components
were expressed as the mean amplitude that was calculated by all spectra demonstrated an HF component peak at the
the following formula respiratory frequency of the paced breathing in indi-
vidual sessions and an LF component peak at a fre-
Mean amplitude (ms/Hz1/2) = J[2 x power (ms2/Hz>] (1) quency of - 0.1 Hz. The HF component appeared as
wide-based and multiple peaks during the spontaneous
We also evaluated the ratio of the mean amplitudes of the LF breathing, while it appeared as a single sharp peak
to HF components (LF/HF). during the paced breathing, and the longer the respira-
Statistical anaZysis. SAS programs (SAS Institute, Cary, tory interval, the larger the size of the HF peak in both
NC) were used for statistical analysis. The effects of paced
breathing and respiratory interval on the variables (mean R-R positions.
interval, the amplitude of the LF and HF components, and To evaluate the effects of the paced breathing, we
LF/HF) were analyzed separately for the four different condi- compared spontaneous breathing and paced breathing
tions (2 postures x 2 drug treatments). The within-subject
effects of paced breathing and respiratory interval were evalu- Table 1. Effects ofpaced breathing on center frequency
ated by paired t test and repeated-measure analysis of vari- of low-frequency component of heart rate variability
ance, respectively. Data are presented as the means 2 SE
unless otherwise noted. A P value < 0.05 was considered and transcutaneous PO, and PCO~ in healthy young
significant in all statistical analyses. male subjects under p-adrenergic blockade condition
Spontaneous Paced
RESULTS P Value
Breathing Breathing
P-Adrenergic blockade condition. Figure 1 shows rep- Low-frequency component, Hz
resentative results obtained from a subject under p-ad- Supine 0.095 + 0.004 0.082 + 0.007 NS
Tilt 0.085 + 0.005 0.077 10.007 NS
renergic blockade. In both the supine and head-up tilt
Transcutaneous POT, mmHg
positions, the mean level of the R-R interval appeared Supine 8623 8622 NS
unchanged, while its variability is clearly changed with Tilt 8125 82+5 NS
the paced breathing and with the respiratory interval of Transcutaneous PCOZ, mmHg
the paced breathing. These changes in the R-R interval Supine 3922 3624 NS
Tilt 37+4 3524 NS
variability were reflected by the changes in autoregres-
sive power spectra. In both the supine and tilt positions, Values are means + SE of 7 subiects. NS, not significant.
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
H36 RESPIRATION AND VAGAL MODULATION OF HR
Fig. 3. Effects of respiratory
mean R-R interval,
high-frequency
(LF) components,
rate variability
interval
mean amplitude
(HF) and low-frequency
and LF/HF
in 7 young healthy
subjects under p-adrenergic
on
of heart
blockade
male
of
in
*-c
PF:
<-
Qc
c N
I
5oo
,oo
L
I
1
3
i
Respiratory
4
interval (set)
3
Respiratory
4 5
interval
;r
(set)
6
supine and head-up tilt positions.
si
E n SUPINE
L
TILT
5 6 3 4 5 6
Respiratory interval (set) Respiratory interval (set)
at the same respiratory interval as that of the spontane- condition. While the mean R-R interval was unchanged
ous breathing observed under the conditions of indi- in either position, the HF amplitude in the supine and
vidual postures and drug treatment in each subject. The tilt positions increased on average 1.7 and 2.3 times,
mean R-R interval under the p-adrenergic condition respectively, when the respiratory interval was in-
decreased with the paced breathing in both the supine creased from 3 to 6 s (P = 0.001 and 0.035, respectively).
and tilt positions, but these changes did not reach the Neither the amplitude nor the frequency of the LF
significant level (Fig. 2). The HF amplitude was not component changed in either position (Table 2), but the
affected by the paced breathing in either position. LF/HF was influenced significantly by the respiratory
Although the center frequency of the LF component did interval (P = 0.049 and 0.046, respectively). No signifi-
not change significantly in either position (Table l), the cant change was observed in transcutaneous PO, or
LF amplitude showed a significant decrease with the Pco2 in either position (Table 2).
paced breathing in both the supine and tilt positions ControZ condition. The effects of paced breathing and
(P = 0.004 and 0.042, respectively). The LF/HF de- respiratory interval observed under the p-adrenergic
creased with the paced breathing, although the change blockade condition may be attributable to the effect of
was significant only for the supine position (P = 0.020). propranolol. To examine this possibility, we performed
No significant change was observed in transcutaneous the same experiments without propranolol (control con-
PO, or PCO~ in either position (Table 1). dition).
Figure 3 shows the effects of the respiratory interval As shown in Table 3, the mean R-R interval under the
of the paced breathing under the p-adrenergic blockade control condition decreased with the paced breathing in
Table 2. Effects of respiratory interval ofpaced breathing on center frequency of low-frequency component of
heart rate variability and transcutaneous PO, and PCO~in healthy young male subjects
under p-adrenergic blockade condition
Respiratory Interval, s
P Value
3 4 5 6
Low-frequency component, Hz
Supine 0.080 + 0.008 0.095+0.006 0.089 + 0.008 0.077+0.004 NS
Tilt 0.086~0.003 0.088+0.010 0.087+0.008 0.087+0.005 NS
Transcutaneous POT, mmHg
Supine 87+_3 88+3 8822 8723 NS
Tilt 81+3 8223 8323 8023 NS
Transcutaneous Pco~, mmHg
Supine 3522 34+3 3724 3624 NS
Tilt 33+2 35+4 3624 3423 NS
Values are means t SE of 7 subjects.
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
RESPIRATION AND VAGAL MODULATION OF HR H37
Table 3. Effects ofpaced breathing on heart rate and tilt positions (P = 0.019 and 0.040, respectively). No
variability in healthy young male subjects under control significant change was observed in transcutaneous PO,
(drug-free) condition or PCO~ in either position.
The effects of the respiratory interval under the
Spontaneous Paced
Breathing Breathing
P Value control condition are shown in the Table 4. The results
were basically the same as those obtained under the
R-R interval, ms P-adrenergic blockade condition. While the mean R-R
Supine 1,006 2 44 979 k 50 NS
Tilt 710 + 38 652226 0.046
interval was unchanged in either position, the HF
HF amplitude, ms/Hz1i2 amplitude in both the supine and tilt positions increased
Supine 42.4k8.2 39.1+ 7.9 NS with the respiratory interval (P = 0.002 and 0.001,
Tilt 15.2 k4.2 22.4t9.0 NS respectively). Neither the amplitude nor the center
LF amplitude, ms /Hz l/2 frequency of the LF component changed in either
Supine 23.5 23.0 19.5 + 4.3 NS
Tilt 34.0t5.1 27.1+ 2.5 0.020 position, but the LF/HF decreased with the respiratory
LF component, Hz interval (P = 0.027 and 0.046, for the supine and tilt
Supine 0.091+ 0.010 NS positions, respectively). No significant change was ob-
Tilt 0.072+0.007 NS served in transcutaneous PO, or PCO~ in either position.
LF/HF
Supine 1.0 + 0.2 0.8kO.l 0.019 DISCUSSION
Tilt 2.3kO.6 2.6+ 1.2 NS
Transcutaneous POT, mmHg In this study, we examined whether or not paced
Supine 8724 85+4 NS breathing and the respiratory interval modify the rela-
Tilt 83+2 83+4 NS
Transcutaneous Pco~, mmHg tionship between cardiac vagal tone and the spectral
Supine 36+2 3623 NS components of HRV. Contrasting between spontaneous
Tilt 3623 35k3 NS breathing and paced breathing at the same respiratory
Values are means + SE of 7 subjects. HF, high frequency; LF, low
interval as that of the individual spontaneous breathing,
frequency; LF/HF, ratio of low-frequency to high-frequency compo- we found that the paced breathing did not increase the
nent. mean R-R interval under either the P-adrenergic block-
ade or control condition. We also found that the mean
both the supine and tilt positions, but the change was R-R interval was not changed by the voluntary changes
significant only for the tilt position (P = 0.046). The HF in the respiratory interval from 3 to 6 s in either the
amplitude was not affected by the paced breathing in supine or tilt position under either the P-adrenergic
either position, while the LF amplitude showed a signifi- blockade or control condition, while the HF amplitude
cant decrease with the paced breathing in both the increased progressively with the increase in respiratory
supine and tilt positions (P = 0.018 and 0.020, respec- interval. These results indicate that the paced breath-
tively). The center frequency of the LF component did ing, at least according to the method we used in this
not change significantly in either position. The LF/HF study, does not increase the mean cardiac vagal tone and
decreased with the paced breathing in both the supine that the increase in the respiratory interval increased
Table 4. Effects of respiratory interval ofpaced breathing on heart rate variability in healthy young male subjects
under control (drug-free) condition
Respiratory Interval, s
P Value
3 4 5 6
R-R interval, ms
Supine 1,003 k 50 1,002*46 993+50 979t50 NS
Tilt 668230 651+ 18 645+17 654*16 NS
HF amplitude, ms/Hz1’2
Supine 28.825.4 50.e9.4 54.4* 11.8 79.5216.1 0.002
Tilt 9.7k2.5 14.123.7 19.5 + 4.0 32.6k5.4 0.001
LF amplitude, ms / Hz l/2
Supine 22.8t6.1 21.123.4 22.6k3.9 19.8 + 1.5 NS
Tilt 28.3 + 6.1 28.5k4.8 36.7k8.3 27.5 k2.9 NS
LF component, Hz
Supine 0.099 2 0.006 0.100 kO.004 0.092 2 0.009 0.084~0.005 NS
Tilt 0.079 2 0.007 0.085 kO.003 0.074*0.006 0.073*0.004 NS
LF/HF
Supine 1.1 t 0.2 0.62 0.1 0.72 0.1 0.5? 0.1 0.027
Tilt 3.9 + 1.2 2.0 kO.5 1.7 + 0.5 1.2 2 0.2 0.046
Transcutaneous POT, mmHg
Supine 8823 9023 88+3 8724 NS
Tilt 80+4 83+3 81+4 8223 NS
Transcutaneous Pco~, mmHg
Supine 3622 3624 3723 36+4 NS
Tilt 33k4 3224 34+4 33k4 NS
Values are means + SE of 7 subjects.
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
H38 RESPIRATION AND VAGAL MODULATION OF HR
the HF amplitude without changing the mean cardiac the RSA amplitude without changing the mean R-R
vagal tone. interval under p-adrenergic blockade, although RSA
Pagani et al. (23) reported that paced breathing and the mean R-R interval in their study were deter-
decreased the LF component, increased the HF compo- mined from a short segment of data by a nonspectral
nent, and consequently decreased the LF/HF in both method (12).
the supine and tilt positions in healthy young subjects. Our observations seem consistent with those of Tried-
Based on these observations, they concluded that during man et al. (28), who investigated the effect of hypovole-
paced breathing there is enhanced vagal tone. Despite mia induced by blood donation and postural change on
the fact that in their study the frequency of the paced the transfer magnitude of the modulation of heart rate
breathing was set at 0.33 Hz regardless of the individual by lung volume in normal subjects. They found that the
differences in the frequency of spontaneous breathing transfer magnitude in the 0.12- to O.&Hz frequency
and that the magnitudes of the LF and HF components band decreases progressively with increasing hypovole-
were expressed in normalized power (relative power to mia. However, their data also showed that at any level of
the total power of oscillating components), their find- hypovolemia, the transfer magnitude in this frequency
ings seem consistent with ours concerning the changes band decreased uniformly with increasing frequency of
in the spectral components of HRV. However, we ob- lung volume fluctuation. Thus their observations also
served that paced breathing did not increase the mean suggest that the effect of respiratory frequency on the
R-R interval under p-adrenergic blockade. Therefore, HRV in the HF band ( > 0.12 Hz in their study) is
the decrease in the LF/HF with the paced breathing is independent of the changes in autonomic tone induced
not attributable to enhanced vagal tone. by hypovolemia.
Although the effects of respiratory parameters on the Our observation that an increase in respiratory inter-
relationship between HRV and cardiac vagal tone have val enhanced the HF amplitude without changing the
been investigated in earlier studies (11, 19), in such mean cardiac vagal tone seems consistent with the
studies the HF/RSA amplitude was determined by a currently accepted hypothesis concerning the mecha-
nonspectral method, i.e., it was measured as the differ- nisms of RSA and that concerning vagal innervation of
ence between respiratory-related minimum and maxi- the sinus node. Two major physiological mechanisms
mum R-R intervals (12). Kollai and Mizsei (19) exam- have been thought to be involved in the genesis of RSA:
ined the effects of the respiratory interval on RSA 1) the phasic excitatory/inhibitory modulation of vagal
amplitude in healthy young subjects under p-adrenergic cardiomotor neurons by the central respiratory genera-
blockade and have reported that RSA amplitude invari- tor (5, 17,25) and 2) the phasic gating of vagoexcitatory
ably increased with slow breathing, but that the re- inputs in the reflex networks receiving baroreceptor and
sponse of the mean R-R interval varied among subjects; chemoreceptor afferent barrages by pulmonary stretch
it decreased, increased, or stayed at approximately the receptors (5). These mechanisms could yield maximum
same level. They determined both RSA amplitude and vagal excitation during expiration and minimal or near-
mean R-R interval during paced breathing from a short absent vagal activity during inspiration (18). The in-
segment of data (within several breath cycles, see Figs. 1 crease in tidal volume has been suggested to cause more
and 2 in Ref. 19). These measures could be confounded effective gating of vagoexcitatory input by the lung
bY nonrespiratory fluctuations of R-R interval; indeed, inflation receptors, resulting in augmented RSA through
we observed that such fluctuations resulted in the increased vagal inhibition during inspiration (5, 7). On
changes in the mean R-R interval as well as in the RSA the other hand, the response of the sinus node to direct
waveform during paced breathing (Fig. 1). However, stimulation of the cardiac vagal nerve has been reported
both the observations of their study and ours commonly to have a low-pass filter property with a decay constant
indicate that augmented RSA amplitude with slower of - 1 s, although the sinus node response to stimula-
respiration is not explained by an enhancement of tion of cardiac sympathetic nerve has a much longer
cardiac vagal tone. decay constant, specifically, > 15 s (4, 5). This property
In this study, we did not control the tidal volume of vagal action on the sinus node seems mainly respon-
during paced breathing. Because no significant change sible for the effect of the respiratory interval on the HF
was observed in transcutaneous PO, or Pco~, slower amplitude.
paced breathing was expected to be accompanied by a Figure 4 represents a simulation of this effect. If the
greater tidal volume, which could have also contributed phasic respiratory variation of the vagal outflow can be
to the changes in the HF amplitude. Although this study simulated as a step function, the R-R interval during
was not designed to examine separately the effects of expiration phase would increase from an end-inspira-
these two factors, both increased respiratory interval tory level (I) toward the upper saturation level of R-R
and increased tidal volume have been reported to in- interval (E,) that is determined by the expiratory level of
crease the HF/RSA amplitude (8, 11, 17). Our results, vagal outflow. This process can be expressed as
therefore, suggest that neither the effect of the respira-
RR(t) = E, - (E, - I)ept” (2)
tory interval nor that of the tidal volume on the HF
amplitude is mediated by the changes in the mean vagal where RR(t) is the R-R interval at time t, and 7 is the
ton& This is supported by the findings of Grossman et decay constant for the effect of vagal activation on the
al. (11) who have reported that a lengthening of the R-R interval. Similarly, the R-R interval during inspira-
respiratory interval under a fixed tidal volume increases tion phase decreases from an end-expiration level (E)
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
RESPIRATION AND VAGAL MODULATION OF HR H39
R-R
interval
Vagal
o”tf,ow _----------.._-- _______., ------~---..-----_----~ ---________ v
Respiration Expiration Inspiration Expiratiori Inspiration Expiration
Time
Fig. 4. Simulation model of respiratory sinus arrhythmia (RSA). Respiratory variation of vagal outflow is expressed
as a step function with mean level of vagal outflow (V). R-R interval increases during expiration from an
end-inspiratory level (I) toward upper saturation level (E,) that is determined by vagal outflow during expiratory
phase and decreases during inspiration from end-expiratory level (E) toward lower saturation level (I,) that is
determined by vagal outflow during inspiratory phase. These processes are expressed as RR(t) = E, - (E, - I)eytiT and
RR(t) = I, + (E - I,)eptlT’, respectively, where RR(t) is R-R interval at time t and 7 and 7’ are decay constant for effects
of vagal modulation of R-R interval. When respiratory interval (L) comprises an equal length of expiratory and
inspiratory phases, amplitude of RSA is expressed as E - I = (E, - I,)(1 - e-L/2T)/(1 + e-L/2T’).
toward the lower saturation level (I,) that is determined the pulmonary inflation reflex is most likely, which
by the inspiratory level of vagal outflow, and this process decreases I, in Eq. 6 through more effective gating of
can be expressed as vagoexcitatory input during the inspiratory phase (5).
Our finding that respiratory interval modifies the
RR(t) = I, + (E - I,)emtjT’ (3) relationship between cardiac vagal tone and the spectral
where 7’ is the decay constant for the effect of vagal components of HRV clearly indicates the importance of
withdrawal on the R-R interval. When the respiratory controlling and measuring respiration when assessing
interval is controlled to be L seconds, Eqs. 2 and 3 can be autonomic nervous activity by HRV. In both clinical and
written as basic researches, the amplitude of the HF component
and the LF/HF have been widely used as an index of
E = E, - (E, - I)eeL12’ (4) cardiac vagal tone and of sympathovagal balance, respec-
and tively (3,5,29). In this study, however, we found that an
increase in the respiratory interval augments the HF
I = I, + (E - I,)e-Li2$’ (5) amplitude and decreases the LF/HF without changing
If we assume that 7 = 7’ = 1 s as reported, Eqs. 4 and 5 the mean R-R interv .a1 under both the control and
would yield p-adrenergic blockade conditions. These observations
indicate that the increase in the HF amplitude and the
E - I = (E, - I,)(1 - eeLj2)/(1 + emLi2) (6) decrease in the LF/HF with the increasing respiratory
In Eq. 6, E - I represents the HF amplitude and E, - I, interval do not reflect either an increase in cardiac vagal
is thought to be determined by the difference in cardiac tone or a decrease in sympathovagal balance. Thus, in
vagal outflow between the inspiration and expiration the assessment of autonomic activity by HRV, it is
phases. Thus, when the vagal outflow during the inspira- important to compare both between individuals and
tory phase could be assumed to be approximately zero, within individuals with similar respiratory frequency
the E, - I, would be equal to two times mean cardiac contents.
vagal control, and thus, proportional to the mean vagal Conclusion. We investigated the effects of paced
outflow. According to Eq. 6, the HF amplitudes at a breathing and respiratory interval on the relationship
respiratory interval (L) of 3, 4, 5, and 6 s are calculated between the spectral components of HRV and the mean
as 64, 76,85, and 91% of E, - I,, respectively. Therefore, cardiac vagal tone. Under both the control and p-adren-
the increase in the HF amplitude with the increase in ergic blockade conditions, we found that paced breath-
the respiratory interval from 3 to 6 s is estimated as 1.43 ing decreased the LF/HF without an increase in the
times. This value appears to be smaller than those mean R-R interval and that an increase in the respira-
actually observed in this study (1.7 and 2.3 times in the tory interval augmented the HF amplitude without
supine and tilt positions, respectively), suggesting pos- changing the mean R-R interval. The results of this
sible underestimation of the 7 value, or the involvement study suggest that neither the increase in the LF/HF
of other factors in the increase in the HF amplitude, with paced breathing nor the increase in the HF ampli-
among which the effect of the increasing tidal volume on tude with the increasing respiratory interval is mediated
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
H40 RESPIRATION AND VAGAL MODULATION OF HR
by an increase in the mean cardiac vagal tone. Our 15 Hayano, J., Y. Sakakibara, A. Yamada, M. Yamada,
findings support the hypothesis that an increase in the S. Mukai, T. Fujinami, K. Yokoyama, Y. Watanabe, and
K. Takata. Accuracy of assessment of cardiac vagal tone by heart
respiratory interval amplifies the respiratory-related
rate variability in normal subjects. Am. J. CardioZ. 67: 199-204,
vagal modulation of heart rate. 1991.
This work was supported in part by a grant (1993) from T. Nanba 16. Hayano, J., J. A. Taylor, A. Yamada, S. Mukai, R. Hori,
Memorial Health Care Foundation, by the Research Grant 5A-8 for T. Asakawa, K. Yokoyama, Y. Watanabe, K. Takata, and
Nervous and Mental Disorders from the Japanese Ministry of Health T. Fujinami. Continuous assessment of hemodynamic control by
and Welfare, and by the Research Grant (1993) for Aging and Health complex demodulation of cardiovascular variability. Am. J. PhysioZ.
from the Japanese Ministry of Health and Welfare to the first author 264 (Heart Circ. Physiol. 33): H1229-H1238, 1993.
(J. Hayano). 17. Hirsch, J. A., and B. Bishop. Respiratory sinus arrhythmia in
Address for reprint requests: J. Hayano, The Third Department of humans: how breathing pattern modulates heart rate. Am. J.
Internal Medicine, Nagoya City University Medical School, Kawa- Physiol. 241 (Heart Circ. Physiol. 10): H620-H629, 1981.
sumi, Mizuho-cho, Mizuho-ku, Nagoya 467, Japan. 18. Katona, P. G., and F. Jih. Respiratory sinus arrhythmia:
Received 28 June 1993; accepted in final form 29 January 1994. noninvasive measure of parasympathetic cardiac control. J. AppZ.
Physiol. 39: 801-805, 1975.
REFERENCES 19. Kollai, M., and G. Mizsei. Respiratory sinus arrhythmia is a
1. Akaike, H. Fitting autoregressive models for prediction. Ann. limited measure of cardiac parasympathetic control in man. J.
Inst. Stat. Math. 21: 234-247, 1969. Physiol. Lond. 424: 329-342, 1990.
2. Angelone, A., and N. A. Coulter. Respiratory sinus arrhyth- 20. Malliani, A., M. Pagani, F. Lombardi, and S. Cerutti.
mia: a frequency dependent phenomenon. J. AppZ. Physiol. 19: Cardiovascular neural regulation explored in the frequency do-
479-482,1964. main. Circulation 84: 482-492, 1991.
3. Appel, M. L., R. D. Berger, J. P. Saul, J. M. Smith, and R. J. 21. Marple, L. A new autoregressive spectrum analysis algorithm.
Cohen. Beat to beat variability in cardiovascular variables: noise IEEE Trans. Acoust. Speech Signal Processing ASSP-28: 441-
or music? J. Am. CoZZ. Cardiol. 14: 1139-1148, 1989. 455,198O.
4. Berger, R. D., J. P. Saul, and R. J. Cohen. Transfer function 22. Novak, V., P. Novak, J. De Champlain, A. R. Le Blanc,
analysis of autonomic regulation. I. Canine atria1 rate response. R. Martin, and R. Nadeau. Influence of respiration on heart
Am. J. Physiol. 256 (Heart Circ. Physiol. 25): H142-H152, 1989. rate and blood pressure fluctuations. J. AppZ. PhysioZ. 74: 617-
5. Berntson, G. G., J. T. Cacioppo, and K. S. Quigley. Respira- 626,1993.
tory sinus arrhythmia: autonomic origins, physiological mecha- 23. Pagani, M., F. Lombardi, S. Guzzetti, 0. Rimoldi, R. Furlan,
nisms, and psychophysiological implications. Psychophysiology P. Pizzinelli, G. Sandrone, G. Malfatto, S. Dell’Orto, E.
30: 183-196,1993. Piccaluga, M. Turiel, G. Baselli, S. Cerutti, and A. Malli-
6. Brown, T. E., L. A. Beightol, J. Koh, and D. L. Eckberg. ani. Power spectral analysis of heart rate and arterial pressure
Important influence of respiration on human R-R interval power
variabilities as a marker of sympatho-vagal interaction in man
spectra is largely ignored. J. AppZ. PhysioZ. 75: 2310-2317, 1993.
and conscious dog. Circ. Res. 59: 178-193, 1986.
7. Daly, M. de B. Interactions between respiration and circulation.
24. Pomeranz, B., R. J. B. Macaulay, M. A. Caudill, I. Kutz,
In: Handbook of Physiology. The Respiratory System. ControZ of
Breathing. Bethesda, MD: Am. Physiol. Sot., 1985, sect. 3, vol. II, D. Adam, D. Gordon, K. M. Kilborn, A. C. Barger, D. C.
pt. 2, chapt. 16, p. 529-594. Shannon, R. J. Cohen, and H. Benson. Assessment of auto-
8. Eckberg, D. L. Human sinus arrhythmia as an index of vagal nomic function in humans by heart rate spectral analysis. Am. J.
cardiac outflow. J. AppZ. Physiol. 54: 961-966, 1983. Physiol. 248 (Heart Circ. Physiol. 17): H151-H153, 1985.
9. Fallen, E. L., M. V. Kamath, and D. N. Ghista. Power 25. Richter, D. W., and K. M. Spyer. Cardiorespiratory control. In:
spectrum of heart rate variability: a noninvasive test of integrated CentraZ Regulation of Autonomic Function, edited by A. D. Loewy
neurocardiac function. CZin. Invest. Med. 11: 331-340, 1991. and K. M. Spyer. New York: Oxford Univ. Press, 1990, p.
10. Fouad, F. M., R. C. Tarazi, C. M. Ferrario, S. Fighaly, and 189-207.
C. Alicandri. Assessment, of parasympathetic control of heart, 26. Saul, J. P., R. D. Berger, P. Albrecht, S. P. Stein, M. H.
rate by a noninvasive method. Am. J. Physiol. 246 (Heart Circ. Chen, and R. J. Cohen. Transfer function analysis of the
Physiol. 15): H838-H842, 1984. circulation: unique insights into cardiovascular regulation. Am. J.
11. Grossman, P., J. Karemaker, and W. Wieling. Prediction of Physiol. 261 (Heart Circ. Physiol. 30): H1231-H1245, 1991.
tonic parasympathetic cardiac control using respiratory sinus 27. Saul, J. P., R. D. Berger, M. H. Chen, and R. J. Cohen.
arrhythmia: the need for respiratory control. PsychophysioLogy Transfer function analysis of autonomic regulation. II. Respira-
28: 201-216,199l. tory sinus arrhythmia. Am. J. Physiol. 256 (Heart Circ. Physiol.
12. Grossman, P., and S. Svebak. Respiratory sinus arrhythmia as
25): H153-H161,1992.
an index of parasympathetic control during active coping. Psycho-
28. Triedman, J. K., R. J. Cohen, and J. P. Saul. Mild hypovole-
physiology 24: 228-235, 1987.
mic stress alters autonomic modulation of heart rate. Hyperten-
13. Hayano, J. Quantitative assessment of autonomic function by
sion DaZZas 21: 236-247, 1993.
autoregressive spectral analysis of heart rate variability: effect of
posture, respiratory frequency, and age. Jiritsusinkei 25: 334- 29. Van Ravenswaaij-Arts, C. M. A., L. A. A. Kolle, J. C. W.
344,1988. Hopman, G. B. A. Stoelinga, and H. P. Van Geijn. Heart rate
14. Hayano, J., Y. Sakakibara, M. Yamada, T. Kamiya, variability. Ann. Intern. Med. 118: 436-447, 1993.
T. Fujinami, K. Yokoyama, Y. Watanabe, and K. Takata. 30. Zetterberg, L. H. Estimation of parameters for a linear differ-
Diurnal variations in vagal and sympathetic cardiac control. ence equation with application to EEG analysis. Math. Biosci. 5:
Am. J. Physiol. 258 (Heart Circ. PhysioZ. 27): H642-H646, 1990. 227-275,1969.
Downloaded from www.physiology.org/journal/ajpheart by ${individualUser.givenNames} ${individualUser.surname} (146.155.210.231) on December 21, 2018.
You might also like
- Respiration and EmotionFrom EverandRespiration and EmotionY. HarukiNo ratings yet
- The Relationship Between Resting Heart Rate Variability and Heart Rate RecoveryDocument6 pagesThe Relationship Between Resting Heart Rate Variability and Heart Rate RecoveryAndrés MenesesNo ratings yet
- Acute Effects of Resonance Frequency Breathing On Cardiovascular RegulationDocument10 pagesAcute Effects of Resonance Frequency Breathing On Cardiovascular RegulationLezard DomiNo ratings yet
- Zazen and Cardiac VariabilityDocument10 pagesZazen and Cardiac VariabilitySoulyogaNo ratings yet
- Rsspiratory Rate VariabilityDocument9 pagesRsspiratory Rate VariabilitynarykNo ratings yet
- Pulse Rate Variability Is Not A Surrogate For Heart Rate VariabilityDocument7 pagesPulse Rate Variability Is Not A Surrogate For Heart Rate VariabilityFiras ZakNo ratings yet
- Slow Frequency Anuloma Viloma Pranayama Modulates Cardiac and Neural Oscillations in Yoga Practitioners - PubMedDocument1 pageSlow Frequency Anuloma Viloma Pranayama Modulates Cardiac and Neural Oscillations in Yoga Practitioners - PubMedIndian Journal of Yoga Exercise & Sport Science and Physical EducationNo ratings yet
- Postexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State CyclingDocument10 pagesPostexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State Cyclingnuttela ismeNo ratings yet
- Relation Between Respiratory Rate and HeDocument4 pagesRelation Between Respiratory Rate and HeMuhammad Naufal NoorrachmanNo ratings yet
- Heart Rate Variability Biofeedback Improves Emotional and PhysicalDocument21 pagesHeart Rate Variability Biofeedback Improves Emotional and Physicaljuan miguel GregoriNo ratings yet
- Fphys 09 00621Document9 pagesFphys 09 00621SIVAMATHIVANAN P 22MTL129No ratings yet
- Apnea: A Specific and Potent Pressor Effect of Hypoxia in Patients With SleepDocument6 pagesApnea: A Specific and Potent Pressor Effect of Hypoxia in Patients With SleepDiego SolaqueNo ratings yet
- Cardiac Sympathovagal Balance During Sleep Apnea Episodes: Vanninen, A. Tuunainen, M. Kansanen,? Uusitupas and LansimiesDocument8 pagesCardiac Sympathovagal Balance During Sleep Apnea Episodes: Vanninen, A. Tuunainen, M. Kansanen,? Uusitupas and LansimiesaudiNo ratings yet
- 445Document8 pages445teodoraNo ratings yet
- 19 03 PDFDocument6 pages19 03 PDFT h o r y n R a m o sNo ratings yet
- Banner 1995Document7 pagesBanner 1995Ariel Badillo BustamanteNo ratings yet
- Chronic Cholinergic Stimulation Promotes Changes in CardiovascularDocument7 pagesChronic Cholinergic Stimulation Promotes Changes in CardiovascularAndré RibeiroNo ratings yet
- JTCM 1 51Document6 pagesJTCM 1 51soylahijadeunvampiroNo ratings yet
- 08 Chapter 2Document10 pages08 Chapter 2surbhi pareekNo ratings yet
- Experimental Biology and MedicineDocument9 pagesExperimental Biology and Medicineiri_balNo ratings yet
- Reference Values For Lung Function Tests. I. Static VolumesDocument15 pagesReference Values For Lung Function Tests. I. Static VolumesLucho1234No ratings yet
- A Study of Efficiency of Breathing Exercises To Improve Pulmonary FX in SCi PtsDocument6 pagesA Study of Efficiency of Breathing Exercises To Improve Pulmonary FX in SCi PtsMarion AtienzaNo ratings yet
- Breath Holding Index in The Evaluation of Cerebral VasoreactivityDocument5 pagesBreath Holding Index in The Evaluation of Cerebral Vasoreactivityydhapratama11No ratings yet
- Heart Rate Variability (HRV) BiofeedbackDocument9 pagesHeart Rate Variability (HRV) BiofeedbackLUCIENE CRISTALDO ALBUQUERQUENo ratings yet
- Hynynen 2009 PDFDocument5 pagesHynynen 2009 PDFigmartgmNo ratings yet
- MainDocument11 pagesMainDhonz R AdiwaramanNo ratings yet
- New Physiological Approach To Control Essenti HypertensionDocument9 pagesNew Physiological Approach To Control Essenti HypertensionsandeepNo ratings yet
- Pi Is 0007091217435811Document6 pagesPi Is 0007091217435811Julio AltamiranoNo ratings yet
- Effect of Muslim Prayer (Salat) on α Electroencephalography and Its Relationship with Autonomic Nervous Syst...Document6 pagesEffect of Muslim Prayer (Salat) on α Electroencephalography and Its Relationship with Autonomic Nervous Syst...edi_wsNo ratings yet
- Heart Rate Variability: A Diagnostic and Prognostic Tool in Anesthesia and Intensive CareDocument15 pagesHeart Rate Variability: A Diagnostic and Prognostic Tool in Anesthesia and Intensive CarenrlaprilianiNo ratings yet
- IamDocument9 pagesIamPame Neculpan ArangoNo ratings yet
- HEARTRATEVARIABILITYDocument8 pagesHEARTRATEVARIABILITYdenta aeNo ratings yet
- Acute Effect of Kapalbhati Yoga On Cardiac AutonomDocument7 pagesAcute Effect of Kapalbhati Yoga On Cardiac AutonomAkarat SivaphongthongchaiNo ratings yet
- Achilles Reflex Time and Sympathetic ToneDocument5 pagesAchilles Reflex Time and Sympathetic ToneBudi AthAnza SuhartonoNo ratings yet
- Prognostic Value of Desaturation During A 6-Minute Walk Test in Idiopathic Interstitial PneumoniaDocument7 pagesPrognostic Value of Desaturation During A 6-Minute Walk Test in Idiopathic Interstitial PneumoniaVh TRNo ratings yet
- Effect of Volume-Oriented Versus Flow-Oriented Incentive Spirometry On Chest Wall Volumes, Inspiratory Muscle Activity, and Thoracoabdominal Synchrony in The ElderlyDocument7 pagesEffect of Volume-Oriented Versus Flow-Oriented Incentive Spirometry On Chest Wall Volumes, Inspiratory Muscle Activity, and Thoracoabdominal Synchrony in The ElderlyErina SeptianaNo ratings yet
- 1 s2.0 S0167876000000854 Main PDFDocument13 pages1 s2.0 S0167876000000854 Main PDFmehdi.chlif4374No ratings yet
- Jurnal YaahDocument9 pagesJurnal YaahTatiex 'logat' NoerhayatiNo ratings yet
- 10 1111@psyp 13712Document16 pages10 1111@psyp 13712naya RiveraNo ratings yet
- Fan 2013Document9 pagesFan 2013Anonymous qwH3D0KrpNo ratings yet
- Physiological Measures of Right Nostril Breathing Shirley Telles, Nagarathna R., and Nagendra, H.RDocument6 pagesPhysiological Measures of Right Nostril Breathing Shirley Telles, Nagarathna R., and Nagendra, H.RRitam SenguptaNo ratings yet
- New Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Document5 pagesNew Evidence in Home Mechanical Ventilation: Thematic Poster Session Hall 2-4 - 12:50-14:40Shirley CoelhoNo ratings yet
- Mortalidad y Mecanica en Sdra Driving PressureDocument8 pagesMortalidad y Mecanica en Sdra Driving PressureWillian Palma GómezNo ratings yet
- Heart Rate Variability in An Ageing PopulationDocument9 pagesHeart Rate Variability in An Ageing PopulationBasharat BhatNo ratings yet
- AJP Heart 2008Document8 pagesAJP Heart 2008Rezza FahlevhyNo ratings yet
- Casanova ChestDocument9 pagesCasanova ChestguidepNo ratings yet
- Shoemaker Et Al 2020 Disparity in The Effect of Morphine On Eupnea and Gasping in Anesthetized Spontaneously BreathingDocument15 pagesShoemaker Et Al 2020 Disparity in The Effect of Morphine On Eupnea and Gasping in Anesthetized Spontaneously Breathingoliwia.be92No ratings yet
- Aust JPhysiotherv 48 I 4 ChangDocument6 pagesAust JPhysiotherv 48 I 4 Changprosenjit_patra_1No ratings yet
- Camarena 2000Document10 pagesCamarena 2000Veronica JanethNo ratings yet
- ChangDocument3 pagesChangZULKIFLI POMALANGONo ratings yet
- ContentServer Asp4Document7 pagesContentServer Asp4ganda gandaNo ratings yet
- 1414 431X BJMBR 51 11 E7704Document8 pages1414 431X BJMBR 51 11 E7704Gede AdiNo ratings yet
- Lehrer2000 Article ResonantFrequencyBiofeedbackTrDocument15 pagesLehrer2000 Article ResonantFrequencyBiofeedbackTrAderilson OliveiraNo ratings yet
- Autonomic Testing, Methods and TechniquesDocument15 pagesAutonomic Testing, Methods and TechniquesYanina Pérez de VillarrealNo ratings yet
- Paper Valenti Et Al 1Document5 pagesPaper Valenti Et Al 1Érica Engrácia ValentiNo ratings yet
- Slow Deep BreathingDocument17 pagesSlow Deep BreathingpluigiaNo ratings yet
- WongDocument5 pagesWongtalleresccorporal5No ratings yet
- Respiratory Physiology & Neurobiology: Henrik Fox, Susanne Witzel, Thomas Bitter, Dieter Horstkotte, Olaf OldenburgDocument6 pagesRespiratory Physiology & Neurobiology: Henrik Fox, Susanne Witzel, Thomas Bitter, Dieter Horstkotte, Olaf OldenburgTedy Buana PutraNo ratings yet
- Sheu 2003Document7 pagesSheu 2003CORO CORPSNo ratings yet
- Net Notes CardioDocument9 pagesNet Notes CardioJess PeltraNo ratings yet
- Dr. Kodilkar Jitendra V.Document2 pagesDr. Kodilkar Jitendra V.Jatin PrajapatNo ratings yet
- Angina PostprandialDocument10 pagesAngina PostprandialJoaquín SosaNo ratings yet
- 1-Cardiac AnatomyDocument5 pages1-Cardiac AnatomyZintan HospitalNo ratings yet
- Lawson Jepson 2021 Feline Comorbidities The Intermingled Relationship Between Chronic Kidney Disease and HypertensionDocument11 pagesLawson Jepson 2021 Feline Comorbidities The Intermingled Relationship Between Chronic Kidney Disease and HypertensionNallis RodhdezNo ratings yet
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNDocument34 pagesArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212No ratings yet
- Patho Physio 51 To 100qDocument67 pagesPatho Physio 51 To 100qRaquel BencosmeNo ratings yet
- ECG Interpretation Essentials (Updated) PDFDocument44 pagesECG Interpretation Essentials (Updated) PDFShobana RaveendranNo ratings yet
- ALSDocument35 pagesALSZainal ArifinNo ratings yet
- Hypertension Management RecommendationDocument32 pagesHypertension Management RecommendationSomnath Das GuptaNo ratings yet
- Diastolic Murmurs Valvular Diseases ChartDocument2 pagesDiastolic Murmurs Valvular Diseases ChartNaman KanakiyaNo ratings yet
- AV Fistula ExamDocument4 pagesAV Fistula ExamKay BristolNo ratings yet
- 1 s2.0 S0735109716332739 MainDocument11 pages1 s2.0 S0735109716332739 MainBhagya Narayan PanditNo ratings yet
- Blalock Taussig Shunt PDFDocument4 pagesBlalock Taussig Shunt PDFzuraini_mdnoorNo ratings yet
- 2012 Resistant HypertensionDocument9 pages2012 Resistant HypertensionBarry Tumpal Wouter NapitupuluNo ratings yet
- Welly@unissula - Ac.id: Welly Anggarani, Sandy Christiono, Prima AgusmawantiDocument6 pagesWelly@unissula - Ac.id: Welly Anggarani, Sandy Christiono, Prima Agusmawantinabilah syahirahNo ratings yet
- MI-I Pulse Oximeter PPDocument10 pagesMI-I Pulse Oximeter PPYonatan SolomonNo ratings yet
- Apex BeatDocument22 pagesApex BeatdanielNo ratings yet
- 1 s2.0 S2666084923005089 MainDocument6 pages1 s2.0 S2666084923005089 MainGabriel JoséNo ratings yet
- Animal Physiology From Genes To Organisms 2nd Edition Sherwood Test Bank DownloadDocument9 pagesAnimal Physiology From Genes To Organisms 2nd Edition Sherwood Test Bank DownloadDonna Lee100% (29)
- Ehs Web2Document28 pagesEhs Web2Ahmed KhafagyNo ratings yet
- Physiological Adaptation of Cardiovascular System To High AltitudeDocument11 pagesPhysiological Adaptation of Cardiovascular System To High AltitudeNicholas Matthew SantosoNo ratings yet
- WBI11 01 Que 20220108Document28 pagesWBI11 01 Que 20220108Hammodshan 7No ratings yet
- ArrhythmiaDocument55 pagesArrhythmiaDonjeta AbaziNo ratings yet
- Summative Test in Science 6 (Circulatory)Document3 pagesSummative Test in Science 6 (Circulatory)ronaldodigma97% (33)
- ECG - Systematic-ApproachDocument12 pagesECG - Systematic-ApproachMicael MendesNo ratings yet
- Unstable Angina With Underlying DyslipidaemiaDocument9 pagesUnstable Angina With Underlying DyslipidaemiaAiman ArifinNo ratings yet
- Introduction To Vital SignsDocument17 pagesIntroduction To Vital SignsEvello Mercano100% (1)
- 10.1007@s11886 019 1213 XDocument13 pages10.1007@s11886 019 1213 XИлија РадосављевићNo ratings yet
- Terapi Pasien HMS 2020Document108 pagesTerapi Pasien HMS 2020alvindwi lufikaNo ratings yet
- Junaid Kalia CVDocument9 pagesJunaid Kalia CVJunaid KaliaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (38)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (255)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet